Abstract
Objective:
The present study utilized a prospective, longitudinal design to examine the role of temperament and maltreatment in predicting the emergence of borderline (BPD) and antisocial (ASPD) personality disorder symptoms during adolescence.
Method:
Two hundred and forty-five children aged between 11 and 13 years were recruited from primary schools in Melbourne, Australia. Participants completed temperament, maltreatment, BPD and ASPD symptom measures, and approximately two years later, 206 participants were again assessed for BPD and ASPD symptoms.
Results:
The findings indicate that childhood neglect is a significant predictor of an increase in BPD symptoms, while childhood abuse is a significant predictor of an increase in ASPD symptoms. Moreover, abuse and neglect acted as moderators of the relationship between temperament dimensions and increase in BPD and ASPD symptoms, respectively. Abuse was associated with an increase in BPD symptoms for children with low Affiliation, while neglect was associated with an increase in ASPD symptoms for children with low Effortful Control.
Conclusions:
The current study contributes much needed prospective, longitudinal information on the early development of symptoms of BPD and ASPD, and supports importance of both temperamental and environmental factors in predicting the emergence of these mental health problems early in life.
Keywords: personality, temperament, neglect, abuse, adolescence
Résumé
Objectif:
La présente étude a utilisé une méthode prospective longitudinale pour examiner le rôle du tempérament et de la maltraitance dans la prédiction de l’émergence des symptômes d’un trouble de la personnalité limite (TPL) et d’un trouble de la personnalité antisociale (TPA) durant l’adolescence.
Méthode:
Deux cent quarante-cinq enfants de 11 à 13 ans ont été recrutés dans des écoles primaires de Melbourne, en Australie. Les participants ont répondu à des mesures des symptômes du tempérament, de maltraitance, du TPL et du TPA, et environ deux ans plus tard, 206 participants ont de nouveau été évalués pour les symptômes du TPL et du TPA.
Résultats:
Les résultats indiquent que la négligence dans l’enfance est un prédicteur significatif d’une augmentation des symptômes de TPL, alors que l’abus dans l’enfance est un prédicteur significatif d’une augmentation des symptômes de TPA. En outre, l’abus et la négligence servaient de modérateurs à la relation entre les dimensions du tempérament et l’augmentation des symptômes de TPL et TPA, respectivement. L’abus était associé à une augmentation des symptômes de TPL pour les enfants ayant une faible affiliation, tandis que la négligence était associée à une augmentation des symptômes de TPA pour les enfants ayant un faible contrôle volontaire.
Conclusions:
La présente étude apporte une information prospective et longitudinale très nécessaire sur le développement précoce des symptômes de TPL et de TPA, et confirme l’importance des facteurs du tempérament et de l’environnement pour prédire l’émergence de ces problèmes de santé mentale en début de vie.
Keywords: personnalité, tempérament, négligence, abus, adolescent
Introduction
Little is known about the childhood antecedents of most personality disorders (PDs) (Cohen & Crawford, 2005). The Children in the Community (CIC) study remains the only prospective, longitudinal, community-based study to examine PD symptoms from childhood through to adulthood (Cohen, Crawford, Johnson, & Kasen, 2005) but this study did not measure antisocial features until participants were aged 18 years (Cohen & Crawford, 2005). Even so, the CIC findings suggest that mean levels of non-antisocial PD traits peak during early adolescence (9–12 years) and follow a linear decline through to 25–28 years of age (Johnson et al., 2000a). This is consistent with a normative pattern whereby the transition from adolescence to adulthood is characterized by decreases in negative affectivity and behavioural disinhibition (Roberts, Caspi, & Moffitt, 2001; Robins, Fraley, Roberts, & Trzesniewski, 2001). Many individuals, however, exhibit no change from adolescent levels or may change in a direction opposing the overall population trend (Johnson, Hicks, McGue, & Iacono, 2007). Indeed, 21% of the CIC sample exhibited an increase in PD symptoms over a decade of follow-up assessments (Johnson et al., 2000b), becoming more deviant relative to their age peers (Crawford et al., 2005). Thus, as the tide of ‘normative’ PD traits recedes, in part due to maturational or socialization processes (Cohen et al., 2005), a group is revealed that perhaps conforms more to descriptions of ‘adult’ PD and is more familiar to practitioners and researchers in adult mental health settings (Chanen & McCutcheon, 2008).
Temperament is one individual difference variable that might be a good candidate for predicting such an ‘at risk’ developmental trajectory. Temperament is generally defined as constitutionally based differences in reactivity and regulation that are observable from early in life and have strong biological origins (Goldsmith et al., 1987). It has been implicated in the emergence of a broad range of adolescent mental health problems (Sanson, Letcher, & Smart, 2008). Previous research commonly reports four broad temperament dimensions (Putnam, Ellis, & Rothbart, 2001). Surgency (SUR) refers to a tendency to seek out and enjoy intense experiences, together with a lack of shyness and fear, and is positively associated with the personality factor of extroversion (Putnam et al., 2001). Negative Affect (NA) refers to expressed and felt irritability, sadness and frustration in response to limitations, and is associated with the personality dimension of neuroticism (Rothbart & Ahadi, 1994). Affiliation (AF) relates to a desire for, and pleasure in, warmth and closeness with others and is aligned with the personality factor of agreeableness. Effortful Control (EC) refers to the ability to inhibit a dominant response in order to produce a more socially appropriate and/or goal-directed, non-dominant response (Rothbart, Ahadi, & Evans, 2000), and maps reasonably well onto the adult personality dimension of conscientiousness (Putnam et al., 2001).
Understanding the childhood antecedents of borderline personality disorder (BPD) and antisocial personality disorder (ASPD) is of particular importance because they are both associated with severe functional impairments and have disproportionate effects upon the health and justice systems (Coid et al., 2009; Lenzenweger, Lane, Loranger, & Kessler, 2007). It is generally agreed that these disorders emerge during adolescence or early adulthood (APA, 2000) and contribute to serious psychosocial consequences both during adolescence and in later in life (APA, 2000; Chanen, Jovev, & Jackson, 2007; Winograd, Cohen, & Chen, 2008). Moreover, their temporal stability, functional impairments, and related characteristics are similar to those observed in adult populations (Chanen et al., 2004; Chanen et al., 2007; Chanen, Jovev, McCutcheon, Jackson, & McGorry, 2008).
Research has robustly associated high negative affect, and low effortful control, agreeableness and conscientiousness with BPD (Joyce et al., 2003; Paris, 2005; Saulsman & Page, 2004). Although similar traits have been associated with ASPD, this disorder also appears to be uniquely associated with low negative affectivity (Liest & Dadds, 2009). While temperamental extremes have been considered among the best candidates for developmental antecedents of adult PDs (Mervielde, De Clercq, De Fruyt, & Van Leeuwen, 2005), no studies have prospectively assessed the role of early adolescent temperament in the etiology of PD symptoms or disorders. Adolescent temperament extremes are likely to confer vulnerability for later personality pathology, at least in part, via their interaction with other etiological factors. Aversive life experiences represent an obvious candidate for such a moderating influence.
Childhood abuse and neglect are specific adverse life experiences that have a robust empirical association with the development of adult psychopathology in general (Fergusson, Horwood, & Lynskey, 1996; Mullen, Martin, Anderson, Romans, & Herbison, 1993), with some evidence supporting the idea that this relationship is causal (Kendler et al., 2000). Furthermore, childhood abuse or neglect are both risk factors for both adolescent and adult PD (Cohen et al., 2005). Children with documented childhood abuse or neglect have an increased risk for a range of PDs, including ASPD and BPD, after controlling for offspring age, parental education, and parental psychiatric disorders and symptoms of other PDs (Johnson, Cohen, Brown, Smailes, & Berstein, 1999a). Childhood physical abuse, sexual abuse, and neglect might be differentially associated with PDs, and suggest that it is important to investigate specific etiologic models for each of the PDs. With regard to ASPD and BPD, after symptoms of other PDs were accounted for, documented physical abuse was associated with elevated ASPD symptoms, sexual abuse was associated with elevated BPD symptoms, and neglect was associated with elevated symptoms of ASPD and BPD.
The present study utilized a community-based, prospective, longitudinal assessment of both PD symptoms and temperament features beginning early in adolescence. The study specifically focused upon BPD and ASPD symptoms, with the primary aim being to examine the influence of early maltreatment and temperamental antecedents in predicting the emergence of these PD symptoms. Particularly, the degree to which four dimensions of temperament (NA, SUR, AFL and EC) predict emerging symptoms of ASPD and BPD during early adolescence was examined. It was hypothesized that low AFL, low EC and high SUR would be significant predictors of increases in both BPD and ASPD symptoms, while high NA would be a predictor of increased BPD symptoms only. It was further hypothesized that the levels of abuse and neglect would moderate the relationship between temperament and change in ASPD and BPD symptoms, such that the presence of early abuse or neglect would increase the strength of the relationships between temperament and change in symptoms. Consistent with the findings of the CIC study, it was expected that across the sample, measures of BPD and ASPD symptoms would decrease from baseline to follow-up two years later.
Method
Participants: Sampling and Recruitment
Study participants were drawn from a larger study (see Yap et al., 2008a for details). Children were originally recruited from a random sample of government, independent and Catholic primary schools across metropolitan Melbourne. A large group of children (N=2453), between 10–12 years of age, were screened using the Early Adolescent Temperament Questionnaire (EATQ; see below) in order to: (a) select a smaller sample of children for more intensive assessment that represented the full range of temperament scores; and, (b) to maximize the inclusion of children with temperaments associated with both high and low risk of later affect-regulation problems, including PDs. Participants scoring at both extremes of each temperament dimension during the school-based screening were over-sampled for selection into the baseline cohort (N=415).
Of the children selected and asked to participate in the more intensive assessments, 59% (N=245) consented to participate and completed the baseline assessments. At baseline, the participants were 11–13 (M=12.5, SD=0.5) years of age, with 121 (49%) male participants. At follow-up (approximately two years after baseline (M = 2.56 years, SD = 0.25 years, range = 1.74 – 3.39 years)), participants were 14–16 years of age (M = 14.57, SD = 0.53). Two hundred and fourteen participants (87%) consented to the follow-up assessment, but not all completed the assessment. The final sample consisted of 205 individuals who had usable follow-up data. Written informed consent was obtained in accordance with the guidelines of the Human Research Ethics Committee of the University of Melbourne, Australia.
Father’s education was utilized as an index of general family socioeconomic status. Of our sample, 0.5% of fathers were primary school educated only, 40.1% were high school educated, 18.1% received vocational training (TAFE: Training And Further Education) and 41.2% were university educated. In regard to ethnicity, 87.3% of the sample self-identified as Australian, 6.9% as Australian-European, 3.7% as Australian-Asian, 1.6% as Australian-American and 0.5% as Australian-Middle Eastern.
Measures
The Early Adolescent Temperament Questionnaire-Revised (EATQ-R: Ellis & Rothbart, 2001) was used to examine adolescent temperament child self-report forms. The EATQ-R consists of ten subscales (Activation Control, Affiliation, Attention, Fear, Frustration, High Intensity Pleasure, Inhibitory Control, Pleasure Sensitivity, Perceptual Sensitivity and Shyness) loading onto four higher-order temperamental dimensions: Negative Affect (NA), Surgency (SUR), Affiliation (AFL) and Effortful Control (EC). The EATQ-R has good internal consistency, test-retest reliability and validity data (Capaldi & Rothbart, 1992; Ellis & Rothbart, 2001).
The BPD and ASPD subscales of the Children in the Community Self Report Scale (CIC-SR) were used to dimensionally assess BPD and ASPD symptoms in the sample. The CIC-SR was developed as an age-appropriate measure of PDs for the CIC sample (mean age=13 years). The CIC study’s original assessment of PDs took place in 1983 and the scale has been modified on subsequent occasions to reflect the most recent DSM system revisions. The development of the CIC-SR, is described in detail by Crawford and colleagues (Crawford et al., 2005), and it has been repeatedly validated in longitudinal analyses (Bernstein, Cohen, Skodol, Bezirganian, & Brook, 1996; Bernstein et al., 1993; Crawford, Cohen, & Brook, 2001; Johnson et al., 1999a; Johnson et al., 1999b; Kasen et al., 2001).
The BPD scale (26 items) and the ASPD scale (31 items) were utilized in the present study, and the subscales were used to dimensionally assess BPD and ASPD symptoms rather than for diagnostic purposes. The BPD and ASPD scores ranged from 1 to 3.92 (mean=1.72, SD=0.56) and 1.01 to 2.96 (mean=1.27, SD=0.27), respectively. This is comparable to the data reported in the CIC study for BPD (mean=1.7, SD=1.5); however, ASPD data was not collected until 1992 when participants were 22 years of age (Johnson, Smailes, Cohen, Brown, & Bernstein, 2000c). Both scales had excellent internal consistency (BPD Cronbach’s alpha = 0.94; ASPD Cronbach’s alpha = 0.86) and have appropriate convergence with other self-report instruments in the present sample.
The Childhood Trauma Questionnaire (CTQ: Bernstein, Ahluvalia, Pogge, & Handelsman, 1997), a 28-item self-report inventory suitable for use with adolescents, was used to screen for a history of abuse and/or neglect. The CTQ consists of items measuring physical, sexual, and emotional abuse (‘Abuse’ scale), and items measuring physical and emotional neglect (‘Neglect’ scale). The CTQ is quick to administer, and has been shown to have acceptable psychometric properties for use in both clinical and community based samples (Bernstein et al., 1997; Scher, Stein, Asmundson, McCreary, & Forde, 2001).
Procedure
Interviewers met with the adolescent in their home for administration of baseline and follow-up assessments. Assessments were conducted as part of a larger Adolescent Development Study (Yap, Allen, & Ladouceur, 2008b). CIC-SR was administered at both baseline and follow-up. EATQ-R was also administered at both baseline and follow-up assessments, however; only baseline data was utilized, as it was closest to the baseline CIC-SR assessment. CTQ was completed at follow-up, and thus measures abuse and neglect that might have occurred between baseline and follow-up assessments.
Data Analysis
Data were analyzed using separate hierarchical regressions for each of the maltreatment (abuse and neglect) scores separately. The dependent variable in each regression model was follow-up PD score; with separate analyses conducted for BPD and ASPD scores. Baseline higher-order temperament scores and one of the maltreatment scores were entered into the second block of predictors, after first controlling for the effects of gender, baseline PD score, and SES (father’s highest level of education) in the first block. All two-way interactions involving second block predictors were entered into the third block. All continuous independent variables were mean-centred before forming any interaction terms (Aiken & West, 1991). Significant temperament by trauma interactions were probed using Stata Version 11 (StataCorp., 2009). An alpha level of 0.05 was used to classify findings as significant for all statistical tests.
Two participants were missing temperament data and five were missing baseline CIC-SR data. All missing observations were imputed using the EM approach in the SPSS Missing Values procedure. In addition to the variables of interest, the imputation model contained all centered variables and two-way interactions. After imputation of missing data, all continuous independent variables were again mean-centered and interaction terms were re-calculated.
Results
Preliminary Analyses
Summary statistics for temperament, maltreatment and PD symptoms are presented in Table 1. The pattern of stability and change of PD symptoms across the study period was examined. Paired samples t-tests revealed that mean ASPD symptoms significantly increased over the observed period (t(204) = −3.01, p =0.003) while mean BPD symptoms significantly decreased (t(204) = 4.48, p<0.001). Hierarchical regression analyses were conducted to examine temperament variables as predictors of change in BPD and ASPD symptoms, with separate analysis for each PD. Low EC was a significant predictor of increase in both BPD (Beta=−0.18, t(197)= −2.32, p=0.002) and ASPD symptoms (Beta=−0.30, t(197)= −3.81, p<0.001), while high SUR was a significant predictor of increase in ASPD symptoms (Beta=0.19, t(197)=2.73, p<0.001).
Table 1.
Summary statistics for temperament, maltreatment and personality disorder symptoms
| Minimum | Maximum | Mean | SD | |
|---|---|---|---|---|
| EC (Baseline) | 18 | 68 | 47.27 | 10.04 |
| NA (Baseline) | 8 | 35 | 23.10 | 6.46 |
| SUR (Baseline) | 22 | 70 | 46.93 | 11.10 |
| AFL (Baseline) | 22 | 64 | 44.25 | 8.60 |
| Neglect (Baseline) | 10 | 35 | 14.73 | 5.06 |
| Abuse (Baseline) | 15 | 43 | 18.38 | 4.92 |
| ASPD (Baseline) | 1 | 2.66 | 1.25 | 0.24 |
| BPD (Baseline) | 1 | 3.92 | 1.67 | 0.53 |
| ASPD (Follow-up) | 1 | 3.00 | 1.52 | 0.40 |
| BPD (Follow-up) | 1 | 2.19 | 1.30 | 0.26 |
SUR = surgency; AFL = affiliation; NA = negative affect; EC = effortful control; ASPD = antisocial personality disorder; BPD = borderline personality disorder
Four separate regression analyses were conducted to examine abuse and neglect as moderator variables in predicting ASPD and BPD symptoms at follow up. Main effects were firstly examined followed by interactions.
Childhood Maltreatment as a Moderator in Prediction of Antisocial PD Symptoms at Follow-up
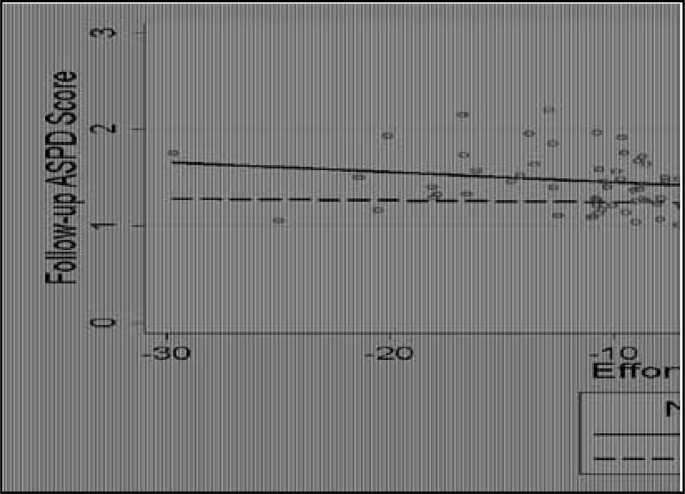
Analyses indicated that CTQ abuse score had a significant main effect on the increase in ASPD symptoms at follow-up, such that higher abuse scores were associated with more symptoms. CTQ neglect score was a significant moderator of the relationship between temperament and ASPD symptoms at follow-up (see Table 2). Figure 1 shows that in high neglect environments, EC was negatively associated with follow-up ASPD symptoms, such that low EC was associated with increased ASPD symptoms at follow-up (Beta=−4.95, p<0.001). For adolescents in low neglect environment, their EC score had no effect on ASPD symptoms at follow-up (Beta=−0.83, p=0.40).
Table 2.
Summary of hierarchical, linear regressions predicting ASPD symptoms at Time 2 from temperament and childhood maltreatment variables
| Abuse | Neglect | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Beta | t | Sig. | Beta | t | Sig. | |
| Sex | −0.07 | −1.11 | 0.27 | −0.07 | −1.11 | 0.27 |
| Father’s Ed | −0.07 | −1.12 | 0.27 | −0.07 | −1.12 | 0.27 |
| Time 1 ASPD | 0.40 | 6.03 | <0.01** | 0.40 | 6.03 | <0.01** |
|
| ||||||
| EC | −0.28 | −3.64 | <0.001** | −0.26 | −3.45 | <0.01** |
| NA | <0.01 | 0.05 | 0.96 | 0.05 | 0.64 | 0.52 |
| AFL | −0.11 | −1.74 | 0.08 | −0.06 | −0.91 | 0.36 |
| SUR | 0.16 | 2.40 | 0.02* | 0.19 | 2.88 | <0.01** |
| CMV | 0.27 | 4.43 | <0.01** | 0.26 | 4.27 | <0.01** |
|
| ||||||
| ECxCMV | −0.10 | −1.42 | 0.16 | −0.32 | −3.76 | <0.01** |
| NAxCMV | −0.02 | −0.17 | 0.86 | −0.16 | −1.69 | 0.09 |
| AFLxCMV | −0.12 | −1.34 | 0.18 | −0.05 | −0.62 | 0.53 |
| SURxCMV | <0.01 | 0.03 | 0.97 | 0.06 | 0.96 | 0.34 |
SUR = surgency; AFL = affiliation; NA = negative affect; EC = effortful control; CMV = childhood maltreatment variable; Ed = education; ASPD = antisocial personality disorder
p <0.05.
p<0.01.
^Additional 2-way interactions between temperament variables were computed as part of the regression model. These were not shown in the table as they do not relate to the proposed hypotheses but are an artifact of the regression model.
Figure 1.
Relationship between temperament and childhood neglect in predicting an increase in ASPD symptoms
Prediction of Borderline PD Symptoms at Follow-up
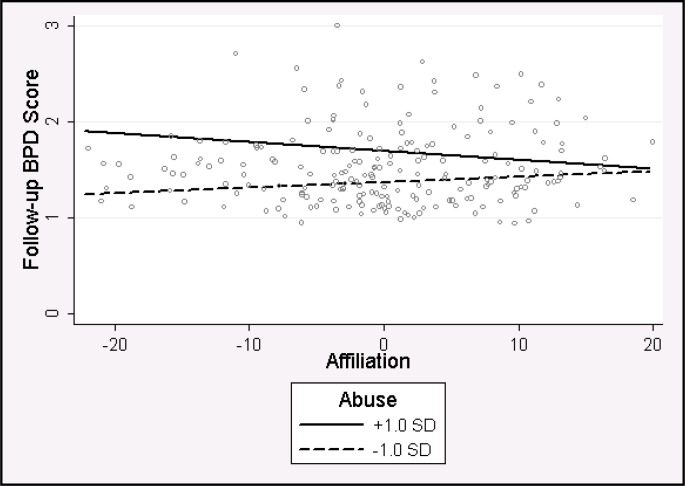
Two separate regression analyses were conducted to examine abuse and neglect as moderator variables in predicting BPD symptoms at follow-up. Analyses indicated that CTQ neglect score had a significant main effect on the increase in BPD symptoms at follow-up, such that higher neglect scores were associated with more symptoms. Regression analyses suggested that CTQ abuse score acted as a moderator in the relationship between temperament and BPD symptoms at follow-up. There was a significant 2-way interaction observed between abuse and AFL, but no significant 2-way interactions between temperament scales and CTQ neglect scores (see Table 3) in predicting BPD scores at Time 2. Figure 2 shows the interactive effects of childhood abuse and AFL on BPD symptoms. In the presence of high abuse, adolescents low in AFL had higher follow-up BPD symptoms (Beta=−2.61, p=0.01). For adolescents in low abuse environment, their AFL score has no effect on BPD symptoms at follow-up (Beta=1.57, p=0.115).
Table 3.
Summary of Hierarchical, Linear Regressions Predicting BPD Symptoms at Time 2 from temperament and childhood maltreatment variables
| Abuse | Neglect | |||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Beta | t | Sig. | Beta | t | Sig. | |
| Gender | 0.13 | 2.08 | 0.04* | 0.13 | 2.08 | 0.04* |
| Father’s Ed | −0.09 | −1.42 | 0.16 | −0.09 | −1.42 | 0.16 |
| Time 1 BPD | 0.49 | 7.94 | <0.01** | 0.49 | 7.94 | <0.01** |
|
| ||||||
| EC | −0.15 | −2.05 | 0.04* | −0.15 | −1.91 | 0.06 |
| NA | −0.04 | −0.53 | 0.60 | 0.01 | 0.06 | 0.95 |
| AFL | −0.02 | −0.31 | 0.76 | 0.03 | 0.50 | 0.66 |
| SUR | −0.10 | −1.56 | 0.12 | −0.06 | −0.86 | 0.39 |
| CMV | 0.33 | 5.54 | <0.01** | 0.22 | 3.64 | <0.01** |
|
| ||||||
| ECxCMV | 0.07 | 1.07 | 0.29 | <0.01 | <0.01 | 1.00 |
| NAxCMV | −0.01 | −0.08 | 0.94 | −0.01 | −0.08 | 0.94 |
| AFLxCMV | −0.22 | −2.67 | 0.01** | −0.05 | −0.61 | 0.55 |
| SURxCMV | −0.05 | −0.79 | 0.43 | 0.02 | 0.25 | 0.80 |
SUR = surgency; AFL = affiliation; NA = negative affect; EC = effortful control; CMV = childhood maltreatment variable; Ed = education; BPD = borderline personality disorder
p <0.05.
p<0.01.
^Additional 2-way interactions between temperament variables were computed as part of the regression model. These were not shown in the table as they do not relate to the proposed hypotheses but are an artifact of the regression model.
Figure 2.
Relationship between temperament and childhood abuse in predicting an increase in BPD symptoms
Discussion
The findings of this study suggest that early adolescent temperament and parental maltreatment contribute to the prospective prediction of changes in BPD and ASPD symptoms across early to middle adolescence. The main findings were that low EC was a predictor in increases in both BPD and ASPD symptoms. Also, neglect and abuse scores were independent predictors of increased BPD and ASPD symptoms, respectively. Furthermore, the effect of parental abuse and neglect was moderated by particular temperamental factors. Specifically, childhood neglect appears to have an effect upon the increase in ASPD symptoms for children with low EC, while childhood abuse appears to have an effect upon the increase in BPD symptoms for children with low AFL.
These findings are consistent with a range of research showing that general maltreatment (Luntz & Widom, 1994) and more specifically aspects of emotional abuse and neglect, including supervision neglect (Johnson et al., 2000b) and verbal abuse (Johnson et al., 2001), are associated with increased PD symptoms (Watson, Chilton, Fairchild, & Whewell, 2006), symptom severity (Bierer et al., 2003) and clinical diagnoses (Gratz, Tull, Baruch, Bornovalova, & Lejuez, 2008). Longitudinal research has also indicated that, after symptoms of other PDs were accounted for, documented physical abuse was associated with elevated ASPD symptoms, sexual abuse was associated with elevated BPD symptoms, and neglect was associated with elevated ASPD and BPD symptoms during early adulthood (Johnson et al., 1999a). While BPD has been associated specifically with sexual abuse, we were not able to investigate sexual abuse in isolation from other types of abuse due to low reported rates in our sample. In the current study, participants were informed in advance of the criteria for mandatory reporting to statutory authorities, which might have influenced their responses.
The effects of parental neglect and abuse also appear to be moderated by particular temperament factors. The finding implicating low EC as a prospective predictor of changes in ASPD symptoms corresponds with previous cross-sectional research showing associations between adolescent impulsivity and antisocial symptoms and diagnoses (Lynam et al., 2000; White, Bates, & Buyske, 2001) or low agreeableness and conscientiousness (Saulsman & Page, 2004). The interaction with childhood neglect, however, indicates a more complex relationship that also implicates the role of family environment in the development of ASPD symptoms. The current findings suggest that familial environments high in neglect are particularly predictive of later elevated ASPD in those adolescents that show a low capacity for regulation of attention and behavior. Parental warmth and support are associated with low levels of antisocial and behavioral problems in children (Caspi et al., 2004; Eisenberg et al., 2005), while children with temperaments low in self-regulatory ability (low EC) are in particular need of high quality parenting in order to develop adequate self-regulation skills and avert the increased risk of developing behavioral problems association with poor self-control (Loeber, Burke, & Lahey, 2002).
By contrast, parental abuse (but not neglect) had a moderating role on the increase of BPD symptoms in the presence of low AFL. The finding implicating low AFL (antagonism) is consistent with previous research showing an association between low AFL and BPD symptoms (Joyce et al., 2003; Paris, 2005; Saulsman & Page, 2004), and reflects the high prevalence of interpersonal difficulties associated with the disorder (Chanen et al., 2007; Jovev & Jackson, 2006; Skodol, Johnson, Cohen, Sneed, & Crawford, 2007). The interaction with childhood abuse, not only points to the role of family environment, but more broadly highlights the question about the effect of environment on temperament development. In particular, it is unclear whether the observed low AFL is a result of living in an abusive childhood environment, or whether low AFL and abusive environment are independent of one another. There is general consensus that temperamental dimensions are observed in infancy, are genetically influenced, and are modestly but significantly preserved across the lifespan. Nevertheless, prospective longitudinal studies, starting in infancy, are needed to answer questions regarding the effect of early childhood environments upon temperament characteristics.
Interestingly, high NA was not found to be a vulnerability for longitudinal increase in BPD symptoms, which is somewhat inconsistent with cross-sectional research associating high neuroticism, negative affectivity, and emotional distress with BPD diagnoses and symptoms (Gratz et al., 2008; Saulsman & Page, 2004). Although a moderate cross-sectional relationship between NA and BPD symptoms (r=0.46, p<0.01) was observed, this temperament dimension did not predict longitudinal changes in these symptoms, suggesting that high levels of NA might covary with BPD symptoms across time rather than being a prospective risk factor per se.
While the current study explored two important putative risk factors in the development of PDs symptoms (temperament and early maltreatment), it also identified possible protective factors. High EC and high AFL were associated with lower ASPD and BPD symptoms, respectively, at follow-up – even in the presence of childhood maltreatment. These findings suggest that children with high capacity for self-regulation and interpersonal affiliation might be protected from developing future psychopathology in the presence of adverse childhood environment. Current theories conceptualize the development of psychopathological outcomes as due to the summative effects of risk and protective factors (Rutter, 2006) or individual sensitivity to positive and negative environmental influence (Ellis, Essex, & Boyce, 2005), such that sufficiently positive factors might ameliorate or even counterbalance aversive ones. Outcome measures of elevated PD symptoms in adolescence might also be more accurately and comprehensively understood when considering early abuse and neglect in combination with other protective factors, such as secure attachment, supportive interpersonal relationships and positive parenting skills.
Stability and change in PD ratings were also examined in this study. Consistent with the CIC study findings (Johnson et al., 2007), adolescents reported that BPD symptoms declined over the study follow-up period. This contrasts with findings from a slightly older clinical sample (Chanen et al., 2004) in which no such decrease was observed. The increase in group-level ASPD ratings is consistent with findings from Chanen and colleagues (2004), and suggests that mean group-level ASPD symptoms might peak at a slightly later age. Indeed, personality traits of aggression, alienation and reactivity to stress, began their developmental decline from later adolescence (approx 17 years) (Johnson et al., 2007). A substantial body of research has provided support for the period from late adolescence to young adulthood being the period of greatest developmental change in mean levels of personality traits, with traits changing more in young adulthood than in any other age bracket, including adolescence (Roberts, Walton, & Viechtbauer, 2006).
The present study has a number of strengths, including the assessment of PD traits prospectively in early adolescence, assessment of PD using an adolescent-specific measure, and the use of a longitudinal design to investigate the prevalence and change in PD symptoms across a well-documented ‘at-risk’ developmental period for the emergence of psychopathology. Additionally, we measured abuse and neglect whilst participants were still in middle adolescence, thus minimizing any recall biases associated with retrospective recall of maltreatment (Cohen et al., 2005; Maughan & Rutter, 1997). There are also several limitations, including the use of questionnaires (rather than clinical interviews) to assess BPD and ASPD symptoms (rather than disorder), as well as the overlap between ASPD and BPD symptoms (r= 0.58) in the sample. Although the current findings indicate that developmental pathways might be different for the two disorders, there is some expected overlap between the disorders and the risk factors identified might not necessarily apply to the development of ‘case-level’ disorder. Furthermore, a fuller understanding of temperamental and environmental risk and protective factors requires consideration of a wider range of factors, including better quantification of putative factors (e.g., intensity, frequency and duration), examination of co-occurring Axis I diagnoses, and extension of the inquiry across the full breadth of PD categories.
Despite its limitations, the current study contributes much needed prospective, longitudinal information on the development of PD symptoms in early adolescence, using a community-based sample. The findings suggest that early adolescent temperament extremes and experiences of mal-treatment do, in part, predict the trajectory of PD symptoms towards middle adolescence, both independently and in interaction. This lends support to an interactional model between temperament and environment in the development of PDs.
Acknowledgments/Conflicts of Interest
This research was supported by grants from the Colonial Foundation, the National Health and Medical Research Council (NHMRC; Australia; Program Grant 350241) and the Australian Research Council (Discovery Grant DP0878136). Dr. Jovev is supported by a NHMRC Training Fellowship. Dr. Whittle is supported by an Australian Research Council Postdoctoral Fellowship. The authors would like to thank the families who participated in the study.
References
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. London: Sage Publications; 1991. [Google Scholar]
- APA . Diagnostic and statistical manual of mental disorders. 4th TR (text revision) ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- Bernstein DP, Ahluvalia T, Pogge D, Handelsman L. Validity of the childhood trauma questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36:340–348. doi: 10.1097/00004583-199703000-00012. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Cohen P, Skodol AE, Bezirganian S, Brook J. Childhood antecedents of adolescent personality disorders. American Journal of Psychiatry. 1996;153(7):907–913. doi: 10.1176/ajp.153.7.907. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Cohen P, Velez CN, Schwab-Stone M, Siever LJ, Shinsato L. Prevalence and stability of the DSM-III--R personality disorders in a community-based survey of adolescents. American Journal of Psychiatry. 1993;150(8):1237–1243. doi: 10.1176/ajp.150.8.1237. [DOI] [PubMed] [Google Scholar]
- Bierer L, Yehuda R, Schmeidler J, Mitropoulou V, New A, Silverman J, Siever L. Abuse and neglect in childhood: Relationship to personality disorder diagnoses. CNS Spectrum. 2003;8(10):737–740. 749–754. doi: 10.1017/s1092852900019118. [DOI] [PubMed] [Google Scholar]
- Capaldi D, Rothbart M. Development and validation of an early adolescent temperament measure. Journal of Early Adolescence. 1992;12(2):153–171. [Google Scholar]
- Caspi A, Moffitt T, Morgan J, Rutter M, Taylor A, Arseneault L, Polo-Tomas M. Maternal expressed emotion predicts children’s antisocial behavior problems: Using monozygotic-twin differences to identify environmental effects on behavioral development. Developemental Psychology. 2004;40(2):149–161. doi: 10.1037/0012-1649.40.2.149. [DOI] [PubMed] [Google Scholar]
- Chanen AM, Jackson HJ, McGorry PD, Allot KA, Clarkson V, Yuen HP. Two-year stability of personality disorder in older adolescent outpatients. Journal of Personality Disorders. 2004;18(6):526–541. doi: 10.1521/pedi.18.6.526.54798. [DOI] [PubMed] [Google Scholar]
- Chanen AM, Jovev M, Jackson HJ. Adaptive functioning and psychiatric symptoms in adolescents with borderline personality disorder. Journal of Clinical Psychiatry. 2007;68(2):297–306. doi: 10.4088/jcp.v68n0217. [DOI] [PubMed] [Google Scholar]
- Chanen AM, Jovev M, McCutcheon LK, Jackson HJ, McGorry PD. Borderline personality disorder in young people and the prospects for prevention and early intervention. Current Psychiatry Reviews. 2008;4:48–57. [Google Scholar]
- Chanen AM, McCutcheon LK. Personality disorder in adolescence: The diagnosis that dare not speak its name. Personal Mental Health. 2008;2:35–41. [Google Scholar]
- Cohen P, Crawford TN. Developmental issues. In: Bender DS, Oldham JM, Skodol AE, editors. The American Psychiatric Publishing textbook of personality disorders. Washington, DC: American Psychiatric Publishing; 2005. pp. 171–185. [Google Scholar]
- Cohen P, Crawford TN, Johnson JG, Kasen S. The children in the community study of developmental course of personality disorder. Journal of Personality Disorders. 2005;19(5):466–486. doi: 10.1521/pedi.2005.19.5.466. [DOI] [PubMed] [Google Scholar]
- Coid J, Yang M, Bebbington P, Moran P, Brugha T, Jenkins R, Ullrich S. Borderline personality disorder: Health service use and social functioning among a national household population. Psychological Medicine. 2009;39:1721–1731. doi: 10.1017/S0033291708004911. [DOI] [PubMed] [Google Scholar]
- Crawford TN, Cohen P, Brook J. Dramatic-erratic personality disorder symptoms: I. Continuity from early adolescence into adulthood. Journal of Personality Disorders. 2001;15(4):319–335. doi: 10.1521/pedi.15.4.319.19182. [DOI] [PubMed] [Google Scholar]
- Crawford TN, Cohen P, Johnson JG, Kasen S, First MB, Gordon K, Brook JS. Self-reported personality disorder in the children in the community sample: Convergent and prospective validity in late adolescence and adulthood. Journal of Personality Disorders. 2005;19(1):30–52. doi: 10.1521/pedi.19.1.30.62179. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Zhou Q, Spinrad TL, Valiente C, Fabes RA, Liew J. Relations among positive parenting, children’s effortful control, and externalizing problems: A three-wave longitudinal study. Child Development. 2005;76(5):1055–1071. doi: 10.1111/j.1467-8624.2005.00897.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis B, Essex M, Boyce W. Biological sensitivity to context: II. Empirical explorations of an evolutionary-developmental theory. Development and Psychopathology. 2005;17:303–328. doi: 10.1017/s0954579405050157. [DOI] [PubMed] [Google Scholar]
- Ellis L, Rothbart M. Revision of the Early Adolescent Temperament Questionnaire. 2001. Manuscript in progress.
- Fergusson D, Horwood J, Lynskey M. Childhood sexual abuse and psychiatric disorder in young adulthood: II. Psychiatric outcomes of childhood sexual abuse. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(10):1365–1374. doi: 10.1097/00004583-199610000-00024. [DOI] [PubMed] [Google Scholar]
- Goldsmith H, Buss A, Plomin R, Rothbart M, Thomas A, Chess S, et al. Roundtable: What is temperament? Four approaches. Child Development. 1987;58:505–529. [PubMed] [Google Scholar]
- Gratz K, Tull M, Baruch M, Bornovalova M, Lejuez C. Factors associated with co-occurring borderline personaility disorder among inner-city substance users: The roles of childhood maltreatment, negative affect intensity/reactivity and emotion dysregulation. Comprehensive Psychiatry. 2008;19:603–615. doi: 10.1016/j.comppsych.2008.04.005. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen D, Brown J, Smailes E, Berstein D. Childhood Maltreatment Increases Risk for Personality Disorders During Early Adulthood. Archives of General Psychiatry. 1999a;56(7):600–606. doi: 10.1001/archpsyc.56.7.600. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Kasen S, Skodol AE, Hamagami F, Brook JS. Age-related change in personality disorder trait levels between early adolescence and adulthood: A community-based longitudinal investigation. Acta Psychiatrica Scandinavica. 2000a;102(4):265–275. doi: 10.1034/j.1600-0447.2000.102004265.x. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Skodol AE, Oldham JM, Kasen S, Brook JS. Personality disorders in adolescence and risk of major mental disorders and suicidality during adulthood. Archives of General Psychiatry. 1999b;56(9):805–811. doi: 10.1001/archpsyc.56.9.805. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Smailes E, Kasen S, Oldham J, Skodol A. Adolescent personality disorders associated with violence and criminal behaviour during adolecence and early adulthood: findings of a community-based longitudinal study. American Journal of Psychiatry. 2000b;157:1406–1412. doi: 10.1176/appi.ajp.157.9.1406. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Smailes E, Skodol A, Brown J, Oldham J. Childhood verbal abuse and risk for personality disorders during adolescence and early adulthood. Comprehensive Psychiatry. 2001;42(1):16–23. doi: 10.1053/comp.2001.19755. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Smailes EM, Cohen P, Brown J, Bernstein DP. Associations between four types of childhood neglect and personality disorder symptoms during adolescence and early adulthood: Findings of a community-based longitudinal study. Journal of Personality Disorders. 2000c;14(2):171–187. doi: 10.1521/pedi.2000.14.2.171. [DOI] [PubMed] [Google Scholar]
- Johnson W, Hicks B, McGue M, Iacono W. Most of the girls are alright, but some aren’t: Personality trajectory groups from ages 14–24 and some associations with outcomes. Journal of Personality and Social Psychology. 2007;93(2):266–284. doi: 10.1037/0022-3514.93.2.266. [DOI] [PubMed] [Google Scholar]
- Jovev M, Jackson HJ. The relationship of borderline personality disorder, life events and functioning in an Australian psychiatric sample. Journal of Personality Disorders. 2006;20(3):205–217. doi: 10.1521/pedi.2006.20.3.205. [DOI] [PubMed] [Google Scholar]
- Joyce P, McKenzie J, Luty S, Mulder R, Carter J, Sullivan P, Cloninger R. Temperament, childhood environment and psychopathology as risk factors for avoidant and borderline personality disorders. Australian and New Zealand Journal of Psychiatry. 2003;37:756–764. doi: 10.1080/j.1440-1614.2003.01263.x. [DOI] [PubMed] [Google Scholar]
- Kasen S, Cohen P, Skodol AE, Johnson JG, Smailes E, Brook JS. Alternative pathways of continuity: Childhood depression and adultpersonality disorder. Archives of General Psychiatry. 2001;58:231–236. doi: 10.1001/archpsyc.58.3.231. [DOI] [PubMed] [Google Scholar]
- Kendler K, Bulik C, Silberg J, Hettema J, Myers J, Prescott C. Childhood sexul abuse and adult psychiatiric and substance use disorders in women. Archives of General Psychiatry. 2000;57:953–959. doi: 10.1001/archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- Lenzenweger M, Lane M, Loranger A, Kessler R. DSM-IV personality disorders in the national comorbidity survey replication. Biological Psychiatry. 2007;62(6):553–564. doi: 10.1016/j.biopsych.2006.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liest T, Dadds MR. Adolescents’ ability to read different emotional faces relates to their history of maltreatment and type of psychopathology. Clinical Child Psychology and Psychiatry. 2009;14(2):237–250. doi: 10.1177/1359104508100887. [DOI] [PubMed] [Google Scholar]
- Loeber R, Burke J, Lahey B. What are adolescent antecedents to antisocial personality disorder? Criminal Behaviour and Mental Health. 2002;12:24–36. doi: 10.1002/cbm.484. [DOI] [PubMed] [Google Scholar]
- Luntz B, Widom C. Antisocial personality disorder in abused and neglected children grown up. American Journal of Psychiatry. 1994;151:670–674. doi: 10.1176/ajp.151.5.670. [DOI] [PubMed] [Google Scholar]
- Lynam D, Caspi A, Moffitt T, Wisktrom P, Loeber R, Novak S. The interaction between impulsivity and neighbourhood context on offending: The effects of impulsivity are stronger in poorer neighbourhoods. Journal of Abnormal Psychology. 2000;109:563–574. doi: 10.1037//0021-843x.109.4.563. [DOI] [PubMed] [Google Scholar]
- Maughan B, Rutter M. Retrospective reporting of childhood adversity: Assessing long-term recall. Journal of Personality Disorders Special Issue: Trauma and personality disorders. 1997;11(1):19–33. doi: 10.1521/pedi.1997.11.1.19. [DOI] [PubMed] [Google Scholar]
- Mervielde I, De Clercq B, De Fruyt F, Van Leeuwen K. Temperament, personality and developmental psychopathology as childhood antecedents of personality disorders. Journal of Personality Disorders. 2005;19(2):171–201. doi: 10.1521/pedi.19.2.171.62627. [DOI] [PubMed] [Google Scholar]
- Mullen P, Martin J, Anderson J, Romans S, Herbison P. Childhood sexual abuse and mental health in adult life. British Journal of Psychiatry. 1993;163:721–732. doi: 10.1192/bjp.163.6.721. [DOI] [PubMed] [Google Scholar]
- Paris J. The development of impulsivity and suicidality in borderline personality disorder. Development and Psychopathology. 2005;17:1091–1104. doi: 10.1017/s0954579405050510. [DOI] [PubMed] [Google Scholar]
- Putnam S, Ellis L, Rothbart M. The structure of temperament from infancy through adolescence. In: Eliasz A, Angleitner A, editors. Advances in Research on Temperament. Lengerich: Pabst Science Publishers; 2001. [Google Scholar]
- Roberts B, Caspi A, Moffitt T. The kids are alright: Growth and stability in personality development from adolescence to adulthood. Journal of Personality and Social Psychology. 2001;81:670–683. [PubMed] [Google Scholar]
- Roberts B, Walton K, Viechtbauer W. Patterns of mean-level change in personaltiy traits across the life course: A meta-analysis of longitudinal studies. Psychological Bulletin. 2006;132:1–25. doi: 10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
- Robins R, Fraley R, Roberts B, Trzesniewski K. A longitudinal study of personality change in young adulthood. Journal of Personality. 2001;69:617–640. doi: 10.1111/1467-6494.694157. [DOI] [PubMed] [Google Scholar]
- Rothbart M, Ahadi S. Temperament and the development of personality. Journal of Abnormal Psychology. 1994;103(1):55–66. doi: 10.1037//0021-843x.103.1.55. [DOI] [PubMed] [Google Scholar]
- Rothbart M, Ahadi S, Evans D. Temperament and personality: Origins and outcomes. Journal of Personality and Social Psychology. 2000;78(1):122–135. doi: 10.1037//0022-3514.78.1.122. [DOI] [PubMed] [Google Scholar]
- Rutter M. Implications of resilience concepts for scientific understanding. Annals of the New York Academy of Sciences. 2006;1094:1–12. doi: 10.1196/annals.1376.002. [DOI] [PubMed] [Google Scholar]
- Sanson A, Letcher P, Smart D. Temperament in early adolescence. In: Allen N, Sheeber L, editors. Adolescent emotional development and the emergence of depressive disorders. New York, NY: Cambridge University Press; 2008. [Google Scholar]
- Saulsman L, Page A. The five-factor model and personality disorder empirical literature: A meta-analytic review. Clinical Psychology Review. 2004;23:1055–1085. doi: 10.1016/j.cpr.2002.09.001. [DOI] [PubMed] [Google Scholar]
- Scher C, Stein M, Asmundson G, McCreary D, Forde D. The childhood trauma questionnaire in a community sample: Psychometric properties and normative data. Journal of Traumatic Stress. 2001;14(4):843–857. doi: 10.1023/A:1013058625719. [DOI] [PubMed] [Google Scholar]
- Skodol A, Johnson J, Cohen P, Sneed J, Crawford T. Personality disorder and imparied functioning from adolescence to adulthood. British Journal of Psychiatry. 2007;190:415–420. doi: 10.1192/bjp.bp.105.019364. [DOI] [PubMed] [Google Scholar]
- StataCorp . Stata Statistical Software: Release 11.0. College Station, TX: StataCorp LP; 2009. [Google Scholar]
- Watson S, Chilton R, Fairchild H, Whewell P. Association between childhood trauma and dissociation amoung patients with borderline personality disorder. Australian and New Zealand Journal of Psychiatry. 2006;40:478–481. doi: 10.1080/j.1440-1614.2006.01825.x. [DOI] [PubMed] [Google Scholar]
- White H, Bates M, Buyske S. Adolescence-limited versus persistent deliquency: Extending Moffitt’s hypothesis into adulthood. Journal of Abnormal Psychology. 2001;110:600–609. doi: 10.1037//0021-843x.110.4.600. [DOI] [PubMed] [Google Scholar]
- Winograd G, Cohen P, Chen H. Adolescent borderline symptoms in the community: Prognosis for functioning over 20 years. The Journal of Child Psychology and Psychiatry. 2008;49(9):933–941. doi: 10.1111/j.1469-7610.2008.01930.x. [DOI] [PubMed] [Google Scholar]
- Yap MBH, Whittle S, Yucel M, Sheeber L, Pantelis C, Simmons J, Allen N. Interaction of parenting experiences and brain structure in the predicition of depressive symptoms in adolescents. Archives of General Psychiatry. 2008a;65(12):1377–1385. doi: 10.1001/archpsyc.65.12.1377. [DOI] [PubMed] [Google Scholar]
- Yap MBH, Allen NB, Ladouceur CD. Maternal socialization of positive affect: The impact of invalidation on adolescent emotion regulation and depressive symptomatology. Child Development. 2008b;79(5):1415–1431. doi: 10.1111/j.1467-8624.2008.01196.x. [DOI] [PubMed] [Google Scholar]