Abstract
Background
Torsade de pointes is a rare, but potentially fatal arrhythmia. More than 40 cases of perioperative torsade de pointes have been reported in the literature; however, the current evidence regarding this complication is very limited. To improve our understanding we performed a systematic review and meta-analysis of all published case reports of perioperative torsade de pointes.
Methods
MEDLINE was systematically searched for cases of perioperative torsade de pointes. We included patients of all age groups, and cases that occurred from the immediate preoperative period to the third postoperative day. Patient and case characteristics as well as QT interval data were extracted.
Results
Forty-six cases of perioperative torsade de pointes were identified; 29 occurred in women (67%) and two episodes were fatal (case fatality rate: 4%). Craniotomies and cardiac surgery accounted for 40% of all cases. Preceding events identified by the authors were hypokalemia (12/46, 26%; 99%CI 9% – 43%) and bradycardia (7/46, 15%; 99%CI 2% – 28%). Drugs were implicated in approximately one-third of the events (14/46, 30%; 99% CI 13% – 48%). The mean QTc at baseline was 457 ± 67ms (min. 320ms; max. 647ms; data available in 27/46 patients). At the time of the event, the mean QTc increased to 575 ± 77ms (min. 413ms; max. 766ms; data available in 33/46 patients). On average, QTc increased by +118ms (99% CI 70 – 166 ms; p< 0.001) between baseline and after the torsade de pointes event. All patients, except for two, had a substantial prolongation of their QTc interval at the time of the event.
Conclusions
This systematic review identified several common risk factors for perioperative torsade de pointes. Given the nearly uniform presence of a substantial QTc interval prolongation at the time of a torsade de pointes episode, increased vigilance for perioperative QTc interval prolongation may be warranted.
Introduction
Torsade de pointes is a rare, but potentially fatal polymorphic ventricular tachycardia.1 This arrhythmia characterized by a typical twisting of the QRS complex morphology2 has several unique features among ventricular tachyarrhythmias.3 First, the ventricular rate in torsade de pointes is often less than 200 beats per minute and it frequently terminates spontaneously, although it can degenerate into ventricular fibrillation and cardiac arrest. Second, torsade de pointes most frequently occurs when the heart rate-corrected QT (QTc) interval is prolonged >500ms and the electrocardiogram shows a characteristic QT-U wave deformity. Furthermore, torsade de pointes occurs nearly always in patients with an abnormal QT interval which is commonly referred to as long QT syndrome, a condition of abnormal cardiac repolarization.2,4 The long QT syndrome can be congenital or acquired, or a combination thereof. Acquired long QT syndrome is commonly the result of QT interval-prolonging drugs.5,6 There is a strong correlation between QTc prolongation and the risk for torsade de pointes, but there is no absolute QTc threshold above which torsade de pointes routinely occurs. Several drugs that are routinely administered in the perioperative setting, such as antibiotics, sevoflurane,7–10 or ondansetron11–13 have been shown to cause QTc interval prolongation. Furthermore, in a recent study we found that the 80% of patients undergoing noncardiac surgery under general anesthesia developed postoperative QTc prolongation with a median increase of 23ms.14
Since the 1970s more than 40 case reports of torsade de pointes occurring in the perioperative setting have been published. However, there has been no systematic review of this subject on the clinical features, precipitating events, and treatments of the potentially fatal arrhythmia occurring in the perioperative setting. The aim of this study was to perform a systematic review and analysis of all published case reports of perioperative torsade de pointes.
Methods
Search Strategy
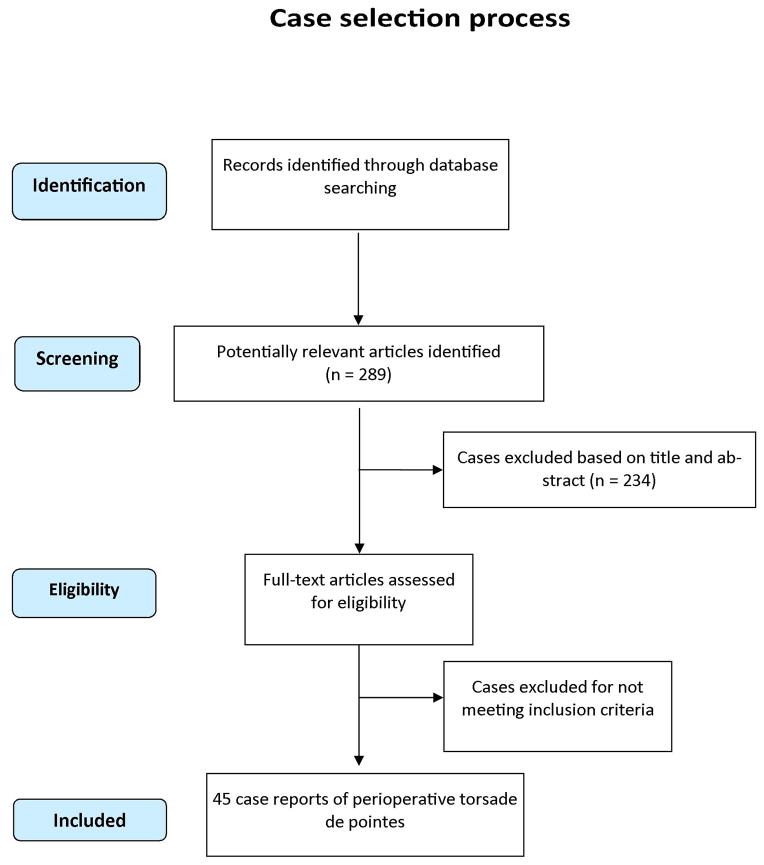
The MOOSE (Meta-analysis Of Observational Studies in Epidemiology)15 and PRISMA (Preferred Reporting Items for Systematic reviews and Meta-Analyses)16 guidelines were followed in our systematic review. In December 2011, we performed a systematic search on MEDLINE for the following search terms: “Surgery AND Torsades de pointes,” “Surgery AND Torsade de pointes,” “Anesthesia AND Torsades de pointes,” “Anesthesia AND Torsade de pointes,” “Perioperative AND Torsades de pointes,” “Perioperative AND Torsade de pointes,” “Intraoperative AND Torsades de pointes,” “Intraoperative AND Torsade de pointes,” “Postoperative AND Torsades de pointes,” “Postoperative AND Torsade de pointes.” This search resulted in 289 hits (Figure 1).
Figure 1.
Study selection process.
Case report selection
Case reports were eligible for inclusion when they reported episodes of torsade de pointes occurring in close temporal relationship to a surgical procedure either under general or regional anesthesia or sedation in human patients. The torsade de pointes event must have occurred between the immediate preoperative phase and the third postoperative day. We did not exclude any age group. Cases were considered from all languages and a particular emphasis was put on including reports from non-English sources. If the publication could not be accessed electronically or in print, we attempted to contact authors by email. The search and case report selection was primarily conducted by one author (JJ) with the help of a second (SP) under supervision by PN. Selection of cases was typically straightforward and any initial disagreement resolved by consensus.
Data Extraction
If available, the following variables were extracted from the case reports: patient characteristics (e.g., age, sex), timing of the torsade de pointes event, heart rates at baseline and at the event, electrolytes, administered drugs, pre- and postevent QT interval duration administered treatments such as defibrillation and magnesium, and outcome (fatal/nonfatal).
Statistical Analysis
Correction for heart rate of the QT interval (QTc) is reported using Bazett’s formula (QTcB = QT/√RR). Pooled categorical and nominal variables are summarized by frequencies and percentages in a fixed-effects meta-analysis. We compared QTc interval duration before the torsade de pointes event with QTc during or after the event using an unpaired two-sided t-test. The D’Agostino and Pearson omnibus normality test was used to determine if QTc measurements were normally distributed before hypothesis testing (QTc values at baseline: p= 0.0606; QTc values at or after torsade de pointes: p= 0.5064). GraphPad 6.01 was used for graphing and statistical analysis (GraphPad Software Inc., LaJolla, CA).
Results
The comprehensive search strategy identified 46 case reports of perioperative torsade de pointes.17–60 These reports were published between 1978 and 2011. Of the 46 cases, 29 occurred in female patients (67%), 14 in male patients (33%) and 2 were of unknown sex. Five patients had a diagnosis of congenital long QT syndrome. The median age among patients with congenital long QT syndrome who developed torsade de pointes was 11 years (range: 8 to 32 years); among patients without congenital long QT syndrome the median age was 56 years (range: 6 weeks to 80 years).
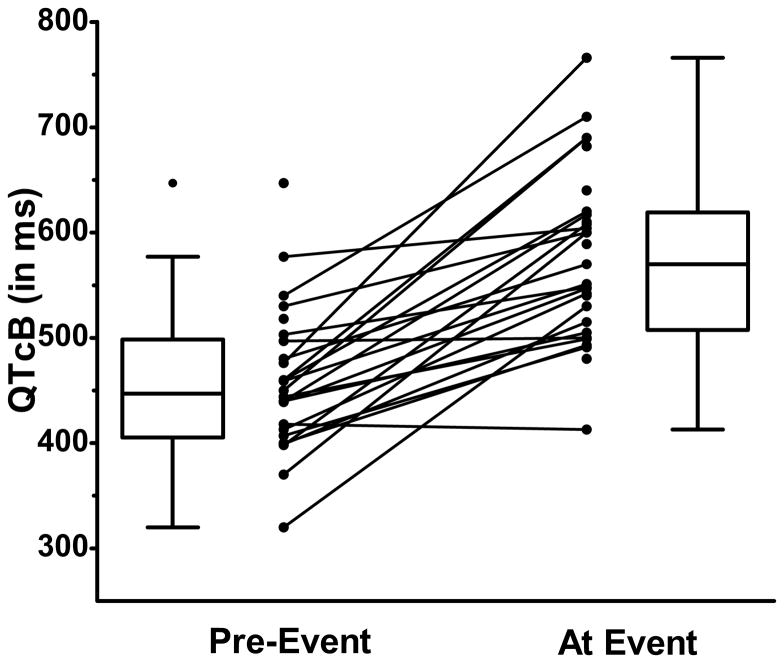
The mean duration of the baseline QTc interval (available in 27 of 46 cases) was 457 ± 67ms (min. 320ms; max. 647ms). At the time of the event, or shortly thereafter, the mean QTc increased to 575 ± 77ms (min. 413ms; max. 766ms; data available for 33 of 46 patients) as shown in Figure 2. At the time of the event, the median heart rate was 62/min (minimum 40 – maximum 105/min; data available for 15 of 46 patients). In 24 patients, QTc interval duration was available before and after the event. These results showed that the QTc increased by +118ms (99% CI 70 – 166 ms; p< 0.001; Figure 2). Two patients had only a minor change in their respective QTc (less than ± 10ms); all others had a substantial prolongation of the QTc interval at the time of the event. Before the torsade de pointes episode, 14 of 27 patients (52%; 99% CI 27% – 77%) had a QTc >440ms and 6 of 27 >500ms (22%); after the event, 32 of 33 (97%; 99% CI 89% – 100%) had a QTc >440ms and 26/33 (79%; 99% CI 61% – 97%) >500ms.
Figure 2.
Dispersion of QTc interval duration before, during, or after the perioperative torsade de pointes event (n=45). QTcB = heart-rate corrected QT interval using Bazett’s formula. Box plots indicate the 25th and 75th percentile; the whiskers reflects the median and the error bars indicate the Tukey’s distance (1.5 times the interquartile distance).
The systematic review and meta-analysis identified several characteristics associated with perioperative torsade de pointes (summarized in tables): Table 1 reports the time point and Table 2 lists all surgical procedures during which torsade de pointes events occurred. Preceding events identified by the authors of the individual case reports are shown in Table 3. In nine cases (20%), the combination of several factors such as hypokalemia or congenital long QT syndrome and QT interval-prolonging drug was identified as trigger for the torsade de pointes event. Table 4 lists all implicated drugs. Two episodes of perioperative torsade de pointes were fatal (case fatality rate: 4%); 40% were treated with magnesium and more than one in four patients required defibrillation. Table 5 lists all commonly used treatment strategies.
Table 1.
Time Point of Torsade de Pointes Episode
| Time Point of Torsade de Pointes Event | Frequency n (%) |
|---|---|
| Preoperative | 2 (4) |
| Induction | 3 (7) |
| Maintenance | 22 (49) |
| Emergence | 1 (2) |
| Postoperative | 19 (42) |
Some events occurred more than once. Percentages do not add to 100%.
Table 2.
Procedures where Torsade de Pointes Episodes Occurred
| Procedures | Frequency n (%) |
|---|---|
| Cardiac | 12 (27) |
| CABG | 3 (7) |
| Cardiac surgery, non-CABG | 3 (7) |
| Radiofrequency Ablation | 4 (9) |
| AICD | 2 (4) |
| Craniotomy | 6 (13) |
| Cerebral Aneurysm Clipping | 4 (9) |
| Meningioma Resection | 2 (4) |
| Liver Transplant | 3 (7) |
| Adrenalectomy | 3 (7) |
| Colon Resection | 2 (4) |
| Others (all 1 case only) | 19 (42) |
|
| |
| Total | 46 (100) |
CABG – coronary artery bypass graft; AICD – automated implantable cardioverter-defibrillator
Table 3.
Preceeding Events for Torsade de Pointes Episodes Identified by the Authors of the Case Reports
| Preceeding Events | Frequency n (%) |
|---|---|
| Hypokalemia | 12 (28) |
| Hypomagnesemia | 4 (9) |
| Hypocalcemia | 2 (5) |
| Bradycardia | 7 (16) |
| Drugs | 13 (30) |
| Congenital Long QT Syndrome | 5 (12) |
More than one factor could be present in an episode of torsade de pointes.
Table 4.
Drugs Implicated in Torsade de Pointes Episodes.
| Drugs |
|---|
| Procainamide |
| Mannitol and subsequent hypokalemia |
| Sevoflurane, Disopyramide, Lidocaine |
| Cyclobenzaprine |
| Haloperidol |
| Halothane |
| Sevoflurane |
| Dolasetron |
| Flecainide |
| Sotalol |
| Erythromycin, Amiodarone, Ciprofloxacin |
| Tacrolimus |
| Papaverine |
Drugs are listed as reported in the published case reports. Several episodes of torsade de pointes occurred as a result of drug-drug interactions.
Table 5.
Treatment used for Torsade de Pointes Events
| Treatment | Frequency n (%) |
|---|---|
| Magnesium | 18 (40) |
| Lidocaine | 14 (31) |
| Defibrillation | 12 (28) |
| Potassium | 5 (11) |
| Overdrive pacing | 5 (11) |
| Isoproterenol | 3 (7) |
| Amiodarone | 1 (2) |
More than one treatment may have been necessary to treat the torsade de pointes event
Discussion
In what we believe is the first systematic analysis of perioperative torsade de pointes, we were able to identify 46 case reports. There are several pertinent findings resulting from the pooling of the available evidence from these case reports. First, nearly all episodes of perioperative torsade de pointes occurred when the QTc interval was substantially prolonged. Our data show an increase of > 100ms at the time of the event compared to baseline in the majority of patients while only two patients had no significant increase in QTc. It therefore appears that QTc interval prolongation is nearly always required to develop perioperative torsade de pointes, but in itself is not sufficient to trigger actual episodes. As in other settings, perioperative torsade de pointes appears to be triggered by a simultaneous occurrence of several factors in the presence of QTc prolongation, such as hypokalemia, bradycardia, or drug-drug interactions. In a recent prospective study we found that among 469 patients undergoing noncardiac surgery under general anesthesia, more than 80% developed postoperative QTc prolongation and one patient developed torsade de pointes (incidence rate of 0.4%).14 As in this report, many of these patients received several drugs within a short period of time that likely contributed to QTc prolongation. Consistent with previous evidence, perioperative torsade de pointes appears to be more prevalent in women than men.61,62 Patients with diagnosed congenital long QT syndrome had episodes of perioperative torsade de pointes at a much earlier age (median age 11 years)63 compared to patients without this diagnosis (median age 56 years).
It is noteworthy that several drugs were implicated in the case reports of perioperative torsade de pointes, but not droperidol for which the Food and Drug Administration issued a “black box” warning regarding the QTc prolongation risk.12,13,64 Many other perioperatively administered drugs such as ondansetron65 and metoclopramide66 also prolong the QTc interval.
Among the 46 identified cases of perioperative torsade de pointes, procedures and conditions, such as cerebral aneurysm rupture, cardiac surgery, and pheochromocytoma, appear to be over-represented. We do not have a clear explanation for this observation and it may represent random chance, but perhaps it is related to elevated catecholamine levels. Catecholamine release and stress have been previously shown to trigger episodes of torsade de pointes67,68 so these surgical procedures and conditions may be associated with a higher risk for perioperative torsade de pointes. It is noteworthy that only 4% of perioperative torsade de pointes cases were fatal. However one in four patients required defibrillation but the majority of events responded to magnesium, lidocaine or were self-terminated.5
Evidence regarding even the most basic facts about perioperative torsade de pointes is largely missing. Since most episodes are unreported, there is little evidence regarding the precise incidence or prevalence of this condition. Nonsurgical hospitalized patients are at higher risk for torsade de pointes3 and the perioperative period may also be a period of increased risk due to the potential exposure to multiple drugs that can affect myocardial repolarization.14 Forty-six case reports over 40 years may indicate a very low, negligible prevalence of perioperative torsade de pointes. Reporting bias, the tendency to under-report less desirable findings, was clearly a major limitation of our study. Neither numerator nor denominator are known to accurately estimate the prevalence of torsade de pointes in surgical patients and only large-scale epidemiological studies will be able to provide this evidence. Recently the American Heart Association and the American College of Cardiology Foundation published guidelines on the “Prevention of Torsade de Pointes in Hospital Settings” with the goal to raise awareness about this potentially fatal arrhythmia and its prevention.3 The authors of this statement argue that hospitalized patients are often at higher risk for torsade de pointes as they have other risk factors for proarrhythmic response and are often exposed to multiple QT-prolonging drugs.
This study had several limitations. First, the quality of any systematic review is dependent on the available studies and published case reports. Case reports of perioperative torsade de pointes did not follow a uniform reporting standard, so missing data were a substantial limitation. Important variables such as medical risk factors, drugs, and level of electrolytes were not uniformly captured. Furthermore, it is to be expected that there are many more cases of perioperative torsade de pointes than represented by the 46 reports we identified. Second, cases that occurred in the 1970s and 1980s may have become less relevant for modern medical practice as several of the drugs implicated in perioperative torsade de pointes or are no longer widely used (e.g., halothane, droperidol, flecainide or sotalol). As mentioned above, reporting bias is without a doubt the most significant limitation of this study. Nevertheless, we believe that even given these severe limitations, our study provides novel and potentially important insights into perioperative torsade de pointes.
In conclusion, this systematic review identified several common characteristics among 46 case reports of perioperative torsade de pointes. Nearly all episodes were preceded by a substantial QTc prolongation that was commonly the result of several QTc-prolonging factors. Given the common exposure to drugs and physiologic stressors with potential effects on myocardial repolarization, increased vigilance for perioperative QTc interval prolongation and the potential for torsade de pointes may be warranted.
Acknowledgments
Funding: The study was supported, in parts, by grants from the National Institutes of Health, Bethesda, MD (NIHK23 GM087534 to PN and UL1RR024992 to Washington University Institute of Clinical and Translational Sciences) and the American Heart Association (9CRP2240001).
Footnotes
See Disclosures at end of article for Author Conflicts of Interest.
Reprints will not be available from the authors.
DISCLOSURES:
Name: Joshua Johnston, MD
Contribution: This author helped conduct the study, analyze the data, and write the manuscript
Attestation: Joshua Johnston has seen the original study data, reviewed the analysis of the data, and approved the final manuscript
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Swatilika Pal, MBBS, MS
Contribution: This author helped conduct the study, analyze the data, and write the manuscript
Attestation: Swatilika Pal has seen the original study data, reviewed the analysis of the data, and approved the final manuscript
Conflicts of Interest: The author has no conflicts of interest to declare.
Name: Peter Nagele, MD, MSc
Contribution: This author helped design the study, conduct the study, analyze the data, and write the manuscript
Attestation: Peter Nagele has seen the original study data, reviewed the analysis of the data, approved the final manuscript, and is the author responsible for archiving the study files
Conflicts of Interest: Peter Nagele received research funding from Roche Diagnostics Roche provides research support for PI-initiated studies.
Contributor Information
Joshua Johnston, Division of Clinical and Translational Research, Department of Anesthesiology, Washington University School of Medicine, St. Louis, Missouri.
Swatilika Pal, Division of Clinical and Translational Research, Department of Anesthesiology, Washington University School of Medicine, St. Louis, Missouri.
Peter Nagele, Division of Clinical and Translational Research, Department of Anesthesiology, Washington University School of Medicine, St. Louis, Missouri.
References
- 1.El-Sherif NMD, Turitto GMD. Torsade de pointes. Curr Opin Cardiol. 2003;18:6–13. doi: 10.1097/00001573-200301000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Roden DM. Long-QT Syndrome. N Engl J Med. 2008;358:169–76. doi: 10.1056/NEJMcp0706513. [DOI] [PubMed] [Google Scholar]
- 3.Drew BJ, Ackerman MJ, Funk M, Gibler WB, Kligfield P, Menon V, Philippides GJ, Roden DM, Zareba W. Prevention of Torsade de Pointes in Hospital Settings: A Scientific Statement From the American Heart Association and the American College of Cardiology Foundation Endorsed by the American Association of Critical-Care Nurses and the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2010;55:934–47. doi: 10.1016/j.jacc.2010.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moss AJ, Schwartz PJ, Crampton RS, Tzivoni D, Locati EH, MacCluer J, Hall WJ, Weitkamp L, Vincent GM, Garson A., Jr The long QT syndrome. Prospective longitudinal study of 328 families. Circulation. 1991;84:1136–44. doi: 10.1161/01.cir.84.3.1136. [DOI] [PubMed] [Google Scholar]
- 5.Roden DM. Drug-Induced Prolongation of the QT Interval. N Engl J Med. 2004;350:1013–22. doi: 10.1056/NEJMra032426. [DOI] [PubMed] [Google Scholar]
- 6.Heist EK, Ruskin JN. Drug-Induced Arrhythmia. Circulation. 2010;122:1426–35. doi: 10.1161/CIRCULATIONAHA.109.894725. [DOI] [PubMed] [Google Scholar]
- 7.Nakao S, Hatano K, Sumi C, Masuzawa M, Sakamoto S, Ikeda S, Shingu K. Sevoflurane causes greater QTc interval prolongation in elderly patients than in younger patients. Anesth Analg. 2010;110:775–9. doi: 10.1213/ANE.0b013e3181cde713. [DOI] [PubMed] [Google Scholar]
- 8.Han DW, Park K, Jang SB, Kern SE. Modeling the effect of sevoflurane on corrected QT prolongation: a pharmacodynamic analysis. Anesthesiology. 2010;113:806–11. doi: 10.1097/ALN.0b013e3181f26d34. [DOI] [PubMed] [Google Scholar]
- 9.Loeckinger A, Kleinsasser A, Maier S, Furtner B, Keller C, Kuehbacher G, Lindner KH. Sustained prolongation of the QTc interval after anesthesia with sevoflurane in infants during the first 6 months of life. Anesthesiology. 2003;98:639–42. doi: 10.1097/00000542-200303000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Scuderi PE. Sevoflurane and QTc Prolongation: An Interesting Observation, or a Clinically Significant Finding? Anesthesiology. 2010;113:772–5. doi: 10.1097/ALN.0b013e3181f2b088. [DOI] [PubMed] [Google Scholar]
- 11.Chan MT, Choi KC, Gin T, Chui PT, Short TG, Yuen PM, Poon AH, Apfel CC, Gan TJ. The additive interactions between ondansetron and droperidol for preventing postoperative nausea and vomiting. Anesth Analg. 2006;103:1155–62. doi: 10.1213/01.ane.0000239223.74552.0a. [DOI] [PubMed] [Google Scholar]
- 12.Charbit B, Albaladejo P, Funck-Brentano C, Legrand M, Samain E, Marty J. Prolongation of QTc interval after postoperative nausea and vomiting treatment by droperidol or ondansetron. Anesthesiology. 2005;102:1094–100. doi: 10.1097/00000542-200506000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Charbit B, Alvarez JC, Dasque E, Abe E, Demolis JL, Funck-Brentano C. Droperidol and ondansetron-induced QT interval prolongation: a clinical drug interaction study. Anesthesiology. 2008;109:206–12. doi: 10.1097/ALN.0b013e31817fd8c8. [DOI] [PubMed] [Google Scholar]
- 14.Nagele P, Pal S, Brown F, Blood J, Miller JP, Johnston J. Postoperative QT Interval Prolongation in Patients Undergoing Noncardiac Surgery under General Anesthesia. Anesthesiology. 2012;117:321–8. doi: 10.1097/ALN.0b013e31825e6eb3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, Moher D, Becker BJ, Sipe TA, Thacker SB for the Meta-analysis Of Observational Studies in Epidemiology Group. Meta-analysis of Observational Studies in Epidemiology: A Proposal for Reporting. JAMA. 2000;283:2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Ann Intern Med. 2009;151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 17.Zhang F, Gu W, Dong R, Dong Q, Yu B. Anesthetic management of pheochromocytoma resection in a patient with F4 and a complete endocardial cushion defect. Acta Anaesthesiol Scand. 2010;54(6):785–6. doi: 10.1111/j.1399-6576.2009.02188.x. [DOI] [PubMed] [Google Scholar]
- 18.Thiruvenkatarajan V, Osborn KD, Van Wijk RM, Euler P, Sethi R, Moodie S, Biradar V. Torsade de pointes in a patient with acute prolonged QT syndrome and poorly controlled diabetes during sevoflurane anaesthesia. Anaesth Intensive Care. 2010;38(3):555–9. doi: 10.1177/0310057X1003800323. [DOI] [PubMed] [Google Scholar]
- 19.Mizutani K, Toyoda Y, Kubota H. Torsade de pointes ventricular tachycardia following coronary artery spasm during general anaesthesia. Anaesthesia. 1996;51(9):858–60. doi: 10.1111/j.1365-2044.1996.tb12617.x. [DOI] [PubMed] [Google Scholar]
- 20.Kulkarni P, Bhattacharya S, Petros AJ. Torsade de pointes and long QT syndrome following major blood transfusion. Anaesthesia. 1992;47(2):125–7. doi: 10.1111/j.1365-2044.1992.tb02008.x. [DOI] [PubMed] [Google Scholar]
- 21.Alexander MG, Potgieter PD. Atypical ventricular tachycardia (torsade de pointes). A postoperative enigma. Anaesthesia. 198;38(3):269–74. doi: 10.1111/j.1365-2044.1983.tb13989.x. [DOI] [PubMed] [Google Scholar]
- 22.Lustik SJ, Eichelberger JP, Chhibber AK, Bronsther O. Torsade de pointes during orthotopic liver transplantation. Anesth Analg. 1998;87(2):300–3. doi: 10.1097/00000539-199808000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Abe K, Takada K, Yoshiya I. Intraoperative torsade de pointes ventricular tachycardia and ventricular fibrillation during sevoflurane anesthesia. Anesth Analg. 1998;86(4):701–2. doi: 10.1097/00000539-199804000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Soroker D, Ezri T, Szmuk P, Merlis P, Epstein M, Caspi A. Perioperative torsade de pointes ventricular tachycardia induced by hypocalcemia and hypokalemia. Anesth Analg. 1995;80(3):630–3. doi: 10.1097/00000539-199503000-00039. [DOI] [PubMed] [Google Scholar]
- 25.Nuttall GA, Eckerman KM, Jacob KA, Pawlaski EM, Wigersma SK, Marienau ME, Oliver WC, Narr BJ, Ackerman MJ. Does low-dose droperidol administration increase the risk of drug-induced QT prolongation and torsade de pointes in the general surgical population? Anesthesiology. 2007;107(4):531–6. doi: 10.1097/01.anes.0000281893.39781.64. [DOI] [PubMed] [Google Scholar]
- 26.Saitoh K, Suzuki H, Hirabayashi Y, Fukuda H, Igarashi T, Inoue S, Shimizu R, Mitsuhata H. Nicorandil successfully abolished intraoperative torsade de pointes. Anesthesiology. 1998;88(6):1669–71. doi: 10.1097/00000542-199806000-00033. [DOI] [PubMed] [Google Scholar]
- 27.Richardson MG, Roark GL, Helfaer MA. Intraoperative epinephrine-induced torsades de pointes in a child with long QT syndrome. Anesthesiology. 1992;76(4):647–9. doi: 10.1097/00000542-199204000-00027. [DOI] [PubMed] [Google Scholar]
- 28.Michalets EL, Smith LK, Van Tassel ED. Torsade de pointes resulting from the addition of droperidol to an existing cytochrome P450 drug interaction. Ann Pharmacother. 1998;32(7–8):761–5. doi: 10.1345/aph.17351. [DOI] [PubMed] [Google Scholar]
- 29.Takenaka I, Aoyama K, Iwagaki T, Ishimura H, Kadoya T. Development of torsade de pointes caused by exacerbation of QT prolongation during clipping of cerebral artery aneurysm in a patient with subarachnoid haemorrhage. Br J Anaesth. 2006;97(4):533–5. doi: 10.1093/bja/ael183. [DOI] [PubMed] [Google Scholar]
- 30.Vourc’h G, Tanniéres ML. Cardiac arrhythmia induced by pneumoencephalography. Br J Anaesth. 1978;50(8):833–9. doi: 10.1093/bja/50.8.833. [DOI] [PubMed] [Google Scholar]
- 31.Katz RI, Quijano I, Barcelon N, Biancaniello T. Ventricular tachycardia during general anesthesia in a patient with congenital long QT syndrome. Can J Anaesth. 2003;50(4):398–403. doi: 10.1007/BF03021039. [DOI] [PubMed] [Google Scholar]
- 32.Perrault LP, Denault AY, Carrier M, Cartier R, Bélisle S. Torsades de pointes secondary to intravenous haloperidol after coronary bypass grafting surgery. Can J Anaesth. 2000;47(3):251–4. doi: 10.1007/BF03018922. [DOI] [PubMed] [Google Scholar]
- 33.Suri R, Poist ES, Hager WD, Gross JB. Unrecognized bulimia nervosa: a potential cause of perioperative cardiac dysrhythmias. Can J Anaesth. 1999;46(11):1048–52. doi: 10.1007/BF03013200. [DOI] [PubMed] [Google Scholar]
- 34.Chvilicek JP, Hurlbert BJ, Hill GE. Diuretic-induced hypokalaemia inducing torsades de pointes. Can J Anaesth. 1995;42(12):1137–9. doi: 10.1007/BF03015102. [DOI] [PubMed] [Google Scholar]
- 35.Kobza R, Kottkamp H, Hindricks G. Images in cardiovascular medicine. Torsade de pointes in a patient with Wolff-Parkinson-White syndrome. Circulation. 2005;111(13):e173–4. doi: 10.1161/01.CIR.0000162298.17567.1F. [DOI] [PubMed] [Google Scholar]
- 36.Haverkamp W, Hördt M, Breithardt G, Borggrefe M. Torsade de pointes secondary to d, l-sotalol after catheter ablation of incessant atrioventricular reentrant tachycardia--evidence for a significant contribution of the “cardiac memory”. Clin Cardiol. 199;21(1):55–8. doi: 10.1002/clc.4960210111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Werner CR, Riessen R, Gregor M, Bitzer M. Unexpected complication following esophageal variceal hemorrhage - Case 2/2011. Dtsch Med Wochenschr. 2011;136(5):217. doi: 10.1055/s-0030-1247621. [DOI] [PubMed] [Google Scholar]
- 38.Vrolix M, Piessens J, De Geest H. Torsades de pointes after intracoronary papaverine. Eur Heart J. 1991;12(2):273–6. doi: 10.1093/oxfordjournals.eurheartj.a059880. [DOI] [PubMed] [Google Scholar]
- 39.Sosin MD, Cadigan PJ, Connolly DL. Should you remove an implantable loop recorder after the diagnosis is made? Heart. 2003;89(9):1013. doi: 10.1136/heart.89.9.1013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ejiri S, Shoda R, Sumitani T, Okuda K, Kojima A. Three cases of primary aldosteronism including one case with postoperative ventricular tachycardia. Hinyokika Kiyo. 1986;32(1):67–76. [PubMed] [Google Scholar]
- 41.Kim GB, Cho HY, Kwon BS, Bae EJ, Noh CI, Choi JY, Yun YS, Choi Y, Ha JW. QT interval prolongation and ventricular fibrillation in childhood end-stage renal disease. Int J Cardiol. 2008;127(3):e126–8. doi: 10.1016/j.ijcard.2007.04.126. [DOI] [PubMed] [Google Scholar]
- 42.Kappos KG, Kranidis AJ, Anthopoulos LP. Torsades de pointes following radiofrequency catheter His ablation. Int J Cardiol. 1996;57(2):177–9. doi: 10.1016/s0167-5273(96)02821-5. [DOI] [PubMed] [Google Scholar]
- 43.Laub GW, Muralidharan S, Janeira L, Moore RA, Clancy R, Adkins MS, Fernandez J, Anderson WA, McGrath LB. Refractory postoperative torsades de pointes syndrome successfully treated with isoproterenol. J Cardiothorac Vasc Anesth. 1993;7(2):210–2. doi: 10.1016/1053-0770(93)90221-6. [DOI] [PubMed] [Google Scholar]
- 44.Grimm W, Hoffmann J, Menz V, Maisch B. Transient QT prolongation with torsades de pointes tachycardia after ablation of permanent junctional reciprocating tachycardia. J Cardiovasc Electrophysiol. 1999;10(12):1631–5. doi: 10.1111/j.1540-8167.1999.tb00227.x. [DOI] [PubMed] [Google Scholar]
- 45.Turner S, Mathews L, Pandharipande P, Thompson R. Dolasetron-induced torsades de pointes. J Clin Anesth. 2007;19(8):622–5. doi: 10.1016/j.jclinane.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 46.van der Heide K, de Haes A, Wietasch GJ, Wiesfeld AC, Hendriks HG. Torsades de pointes during laparoscopic adrenalectomy of a pheochromocytoma: a case report. J Med Case Reports. 2011;12;5(1):368. doi: 10.1186/1752-1947-5-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Thompson LD, Cohen AJ, Bellasis RM. Polymorphous ventricular tachycardia following cardiopulmonary bypass. J Natl Med Assoc. 1996;88(1):49–51. [PMC free article] [PubMed] [Google Scholar]
- 48.Kodama K, Igase M, Kazatani Y, Matsuzaki K, Murakami E, Kokubu T. Detection of perioperative coronary vasospasm on iodine-123-MIBG, thallium-201 and iodine-123-BMIPP myocardial SPECT images. J Nucl Med. 1995;36(11):2050–2. [PubMed] [Google Scholar]
- 49.Lee JY, Lee JH, An EH, Song JG, Park PH. Postanesthetic torsade de pointes in a patient with unrecognized long QT syndrome -A case report- Korean J Anesthesiol. 2011;60(4):294–7. doi: 10.4097/kjae.2011.60.4.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kim HT, Lee JH, Park IB, Heo HE, Kim TY, Lee MJ. Long QT syndrome provoked by induction of general anesthesia -A case report- Korean J Anesthesiol. 2010;59 (Suppl):S114–8. doi: 10.4097/kjae.2010.59.S.S114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hamaguchi E, Kawano H, Kawahito S, Kitahata H, Oshita S. Torsade de pointes associated with severe bradycardia after induction of general anesthesia. Masui. 2011;60(9):1097–100. [PubMed] [Google Scholar]
- 52.Tajiri O, Ito H, Yago Y, Masumori Y. Torsade de pointes (TdP) observed during general anesthesia for cerebral aneurysm clipping in a patient with QT prolongation. Masui. 2011;60(9):1090–3. [PubMed] [Google Scholar]
- 53.Shibata J, Fujisawa T, Shimizu S, Ide S, Kumasaka M, Sugiyama D, Hishinuma M, Kitoh T. Case of myotonic dystrophy with pulmonary atelectasis and torsade de pointes in the perioperative period. Masui. 2008;57(10):1253–6. [PubMed] [Google Scholar]
- 54.Yamaguchi S, Watanabe K, Mishio M, Okuda Y, Kitajima T. A case of cardiac arrest after torsades de pointes due to prolonged QT interval syndrome possibly associated with subarachnoid hemorrhage. Masui. 1999;48(6):644–6. [PubMed] [Google Scholar]
- 55.Amagasa M, Sato S, Suzuki M, Otabe K. An electrocardiographic abnormality called torsade de pointes in a patient of subarachnoid hemorrhage. No Shinkei Geka. 1988;16(5 Suppl):457–62. [PubMed] [Google Scholar]
- 56.Saussine M, Massad I, Raczka F, Davy JM, Frapier JM. Torsade de pointes during sevoflurane anesthesia in a child with congenital long QT syndrome. Paediatr Anaesth. 2006;16(1):63–5. doi: 10.1111/j.1460-9592.2005.01593.x. [DOI] [PubMed] [Google Scholar]
- 57.Chin JH, Park JY, Kim YK, Kim SH, Kong YG, Park PH, Hwang GS. Torsades de pointes triggered by severe diastolic hypotension with low hematocrit in the neohepatic stage of liver transplantation: a case report. Transplant Proc. 2010;42(5):1959–62. doi: 10.1016/j.transproceed.2010.02.093. [DOI] [PubMed] [Google Scholar]
- 58.Hodak SP, Moubarak JB, Rodriguez I, Gelfand MC, Alijani MR, Tracy CM. QT prolongation and near fatal cardiac arrhythmia after intravenous tacrolimus administration: a case report. Transplantation. 1998;66(4):535–7. doi: 10.1097/00007890-199808270-00021. [DOI] [PubMed] [Google Scholar]
- 59.Hsieh YC, Chow LH, Wong TD, Jeng KN, Lui PW, Lee TY. Acquired long QT syndrome in a child undergoing craniotomy: a case report. Zhonghua Yi Xue Za Zhi (Taipei) 1995;56(3):215–9. [PubMed] [Google Scholar]
- 60.Tacken MC, Bracke FA, Van Zundert AA. Torsade de pointes during sevoflurane anesthesia and fluconazole infusion in a patient with long QT syndrome. A case report. Acta Anaesthesiol Belg. 2011;62(2):105–8. [PubMed] [Google Scholar]
- 61.Abi-Gerges N, Philp K, Pollard C, Wakefield I, Hammond TG, Valentin J-P. Sex differences in ventricular repolarization: from cardiac electrophysiology to Torsades de Pointes. Fundam Clin Pharmacol. 2004;18:139–51. doi: 10.1111/j.1472-8206.2004.00230.x. [DOI] [PubMed] [Google Scholar]
- 62.Drici M-D, Clément N. Is Gender a Risk Factor for Adverse Drug Reactions?: The Example of Drug-Induced Long QT Syndrome. Drug Safety. 2001;24:575–85. doi: 10.2165/00002018-200124080-00002. [DOI] [PubMed] [Google Scholar]
- 63.Curry TB, Gaver R, White RD. Acquired long QT syndrome and elective anesthesia in children. Paediatr Anaesth. 2006;16:471–8. doi: 10.1111/j.1460-9592.2005.01746.x. [DOI] [PubMed] [Google Scholar]
- 64.Mehta D, Sanatani S, Whyte SD. The effects of droperidol and ondansetron on dispersion of myocardial repolarization in children. Paediatr Anaesth. 2010;20:905–12. doi: 10.1111/j.1460-9592.2010.03408.x. [DOI] [PubMed] [Google Scholar]
- 65.McKechnie K, Froese A. Ventricular tachycardia after ondansetron administration in a child with undiagnosed long QT syndrome. Can J Anaesth. 2010;57:453–7. doi: 10.1007/s12630-010-9288-2. [DOI] [PubMed] [Google Scholar]
- 66.Siddique SM, Shariff N, Vesuwala N, Hafiz T. Metoclopramide as a Possible Cause of Prolonged QT Syndrome and Torsade de Pointes in a Patient With Heart Failure and Renal Insufficiency. Ann Intern Med. 2009;150:502–4. doi: 10.7326/0003-4819-150-7-200904070-00016. [DOI] [PubMed] [Google Scholar]
- 67.Kuczkowski KM. Crack cocaine-induced long QT interval syndrome in a parturient with recreational cocaine use. Ann Fr Anesth Reanim. 2005;24:697–8. doi: 10.1016/j.annfar.2005.03.017. [DOI] [PubMed] [Google Scholar]
- 68.Schwartz PJ, Zaza A, Locati E, Moss AJ. Stress and sudden death. The case of the long QT syndrome. Circulation. 1991;83:II71–80. [PubMed] [Google Scholar]