A comparison of the Useful Field of View® (UFOV) and Trail Making Test Part B (Trails B) found that the UFOV risk index was a superior test in predicting on-road outcomes, but the Trails B had acceptable accuracy and was comparable to the other UFOV subtests.
MeSH TERMS: aging, automobile driving, cognition, ROC curve, vision tests
Abstract
The Useful Field of View® (UFOV) and Trail Making Test Part B (Trails B) are measures of divided attention. We determined which measure was more accurate in predicting on-road outcomes among drivers (N = 198, mean age = 73.86, standard deviation = 6.05). Receiver operating characteristic curves for the UFOV (Risk Index [RI] and Subtests 1–3) and Trails B significantly predicted on-road outcomes. Contrasting Trails B with the UFOV RI and subtests, the only difference was found between the UFOV RI and Trails B, indicating the UFOV RI was the best predictor of on-road outcomes. Misclassifications of drivers totaled 28 for the UFOV RI, 62 for Trails B, and 58 for UFOV Subtest 2. The UFOV RI is a superior test in predicting on-road outcomes, but the Trails B has acceptable accuracy and is comparable to the other UFOV subtests.
Safe driving is largely dependent on the preservation of visual and cognitive abilities. In older adults, age-related declines and the effects of medical conditions can compromise visual–cognitive functions, which may lead to unsafe driving. One specific visual–cognitive function, divided attention, which decreases as people age, has received particular interest as a predictor of driving performance in older drivers (Ball, Beard, Roenker, Miller, & Griggs, 1988). Divided attention, also called attention switching or set shifting, is the ability to construct information from multiple sources that are critical to the execution of a specific task (e.g., driving). In essence, drivers are required to shift attention between various stimuli while successfully completing more than one action at a time.
Impairment of divided attention occurs when a person has an inability to inhibit previously learned responses and, as a consequence, is unable to shift attention to the relevant stimulus, thus making errors of preservation (Milner, 1963). Executing a maneuver that requires precise tracking of vehicle position (e.g., turning or merging) in the presence of potential conflicts (e.g., a pedestrian crossing the intersection) is dependent on the driver’s ability to divide attention effectively. In the literature on older drivers, divided attention has mainly been measured with the Useful Field of View® Subtest 2 (UFOV 2; Ball, Owsley, Sloane, Roenker, & Bruni, 1993) and the Trail Making Test Part B (Trails B; Reitan, 1958).
Useful Field of View and On-Road Studies
The useful field of view is defined as the area around a point of fixation from which information is stored and interpreted during a visual task (Mackworth, 1965). This field corresponds to the peripheral visual field around the point of fixation from which information can be processed without movement of the eyes or the head (Ball et al., 1988). Visual attention is tested with the UFOV, a computer-based test measuring the speed and accuracy of visual search (speed of processing), divided attention, and selective attention (Ball & Owsley, 1993).
Research has indicated that advancing age is associated with decreased performance on the UFOV because of the higher prevalence of visual search, attention, and speed of processing deficits (Ball et al., 1988) as well as poorer vision and mental status (Ball & Owsley, 1993). Among older adults, UFOV Risk Index (RI) impairment has been shown to predict driving competence (Owsley et al., 1998), vehicle crashes (Ball et al., 1993; Owsley et al., 1998; Rubin et al., 2007), and driving safety (Clay et al., 2005). Additionally, older drivers with UFOV 2 impairments have 2.3 times higher risk for crash involvement (Owsley et al., 1998). The UFOV 2 also differentiates safe from unsafe drivers with conditions such as Alzheimer’s disease (Duchek, Hunt, Ball, Buckles, & Morris, 1998), HIV, multiple sclerosis, stroke, traumatic brain injury (Ball et al., 2002; Fisk, Novack, Mennemeier, & Roenker, 2002; Marcotte et al., 2004; Mazer et al., 2003), and Parkinson’s disease (Classen et al., 2011; Uc et al., 2006).
Trails B and On-Road Studies
Since its introduction in 1944, the Trail Making Test has been widely used as a test of executive function and visual–perceptual and visual–motor tracking (Lezak, 1995). The test is given in two parts. Part A (“Trails A”) requires participants to connect a series of consecutively numbered circles and involves visual scanning, number recognition, numeric sequencing, and motor speed. Part B (“Trails B”) requires participants to connect a series of numbered and lettered circles, alternating between the two sequences. In this case, one assesses set shifting or mental flexibility in managing more than one stimulus at a time. The Trail Making Test was originally used as a test for intelligence screening (Reitan, 1958) but is frequently used in the off-road portion of driving studies because of its sensitivity to divided attention and psychomotor speed (Bédard, Parkkari, Weaver, Riendeau, & Dahlquist, 2010; Hunt & Bassi, 2010; Stav, Justiss, McCarthy, Mann, & Lanford, 2008; Uc et al., 2006).
Validity of the Trails B as a predictor for failing an on-road test has been established in many driving studies. For example, researchers have found the Trails B to be a valid predictor of on-road performance in 127 community-dwelling older licensed drivers (Classen et al., 2008) and in people with Parkinson’s disease (Classen et al., 2011; Uc et al., 2006). Others (Marshall et al., 2007; Novack et al., 2006) have found the Trails B to be a valid predictor of driving performance in patients with brain injury or predictive of simulated driving performance in older adults (Mullen, Weaver, Riendeau, Morrison, & Bédard, 2010).
Rationale and Significance
Taken together, UFOV (especially UFOV 2) and Trails B, measure the construct of divided attention. The reviewed literature has shown that strong evidence exists to support the UFOV and Trails B as valid predictors of driving performance in older drivers as well as in populations with neurological disorders. Although both tests measure divided attention, the cognitive requirements differ. The UFOV requires accurate processing of visual information involving primarily the frontal and parietal brain regions. Conversely, Trails B has greater memory demands (i.e., remembering numbers and alphabet) involving mainly the frontal lobe. The primary aim of this study was to discern which of the measures (UFOV RI, UFOV Subtests 1–3, or Trails B) were more accurate in predicting pass–fail outcomes in an on-road test among community-dwelling older adults and to compare differences between the accuracy of the UFOV and Trails B when predicting pass–fail outcomes among this population.
If our research found that the Trails B compared well to the UFOV, it could yield cost and time savings to driving rehabilitation specialists and occupational therapy practitioners; if not, then it would confirm that the UFOV is the superior test for determining divided attention. Therefore, we determined, in a group of community-dwelling older licensed drivers (ages 65–89) whether Trails B predicted pass–fail outcomes of an on-road test in a similar fashion as the UFOV RI and the UFOV 2.
Method
Research Design
We used data from the Institute of Mobility, Activity and Participation’s data pool collected from 2004 to 2006 (N = 118) and from 2010 to 2011 (N = 80). The data consisted of results from older drivers undergoing a comprehensive driving evaluation, which included a clinical test as well as an on-road test. Although the data were collected at two time points, both datasets had the same protocol for the clinical and on-road components. We received institutional review board approval from the university’s ethics board, and each participant provided informed consent before participating in the study.
Participants
In total, 198 community-dwelling drivers with a mean age of 73.9 (standard deviation [SD] = 6.1) were recruited via flyer distribution at community facilities, newspaper advertisements, and word-of-mouth referrals in north central Florida. Drivers were included if they were age 65–89, had a valid driver’s license, had been driving 3 mo before or at the time of recruitment, had Mini-Mental State Examination (MMSE; Folstein, Folstein, & McHugh, 1975) scores of >24, and had the physical ability to complete a clinical battery of tests and an on-road driving test. Drivers were excluded if they had medical advice not to drive, uncontrolled seizures in the past year, or used medications that caused central nervous system impairments. Participants were paid $100 for completing the studies.
Procedure
All older drivers completed an intake questionnaire, self-report measures, a brief clinical test battery, and an on-road test. It took approximately 2.5 hr to complete the battery of clinical tests and 45 min to complete the on-road test. Testing was performed by a certified driver rehabilitation specialist (CDRS) or a trained driving evaluator.
Measures
Intake Form.
We collected data on demographic information (age, gender, race, education), medications, and driving history and driving habits via standardized methods previously described (Classen et al., 2008; Stav et al., 2008).
Clinical Tests.
The validated clinical test battery included tests of vision, vision–cognition, cognition, and motor performance and has been documented in previous studies (Classen et al., 2008; Stav et al., 2008). For the purpose of this study, we include only information on the abilities described next.
Vision.
Visual acuity was tested using the Optec® 2500 visual analyzer (Stereo Optical Company Inc., Chicago). We categorized binocular visual acuity as 20/20–20/40 and ≤20/50.
Visual Cognition.
We used the three UFOV subtests (UFOV 1 = visual search and visual processing; UFOV 2 = divided attention; UFOV 3 = selective attention) and the UFOV RI to assess the visual–cognitive function (Ball et al., 1993; Edwards et al., 2006). The three UFOV subtests measure performance, or the threshold exposure duration at which tasks are completed correctly, in milliseconds. UFOV 1 measures the threshold exposure duration for correct performance of identifying whether a car or truck icon was presented inside a box on a computer screen. UFOV 2 measures the threshold exposure duration for correct performance of a central identification task in conjunction with the task of localizing a varied peripheral target. UFOV 3 measures the threshold exposure duration for correct performance of a central identification task and peripheral localizing task, but the peripheral target is embedded in a field of distractors. The range for performance of each task is 16–500 ms. When participants exceed 500 ms on a subtest, they do not continue to the next subtest.
A five-category UFOV RI (1 = very low risk, 2 = low risk, 3 = low–moderate risk, 4 = moderate–high risk, and 5 = high risk; UFOV User’s Guide Version 6.0.6), developed from a composite of the three subtests, is predictive of driving crashes in older drivers (Ball et al., 1993; Goode et al., 1998). Administration of this standardized test does not require specialty training, is conducted on a touch screen, and is completed within 15 min. The software costs about $500, with additional costs of about $4,500 for computer equipment. In this article, we report performance on the UFOV RI and UFOV 1–3.
Cognition.
We used the MMSE (maximum score = 30, with scores <24 indicative of cognitive impairment) as an indicator of baseline cognitive functioning (Folstein et al., 1975). We also administered the Trails B to assess divided attention. Trails B is a standardized paper-and-pencil test and takes about 75 s to complete, with a 180-s cutoff (Reynolds, 2002). In this study, participants were allowed to complete the Trails B regardless of how long it took them.
On-Road Test.
The on-road test was conducted on a standardized road course with demonstrated reliability and validity among older drivers (Justiss, Mann, Stav, & Velozo, 2006; Posse, McCarthy, & Mann, 2006). This test occurred on the same day as the clinical test administration, unless adverse weather necessitated rescheduling. For the on-road evaluations, we used a dual-brake–controlled 2004 Buick Century. The trained driving evaluator or CDRS observed driver performance from the passenger seat. The Global Rating Score (GRS) road-test outcome is a pass–fail measure of driving: 3 = pass, 2 = pass with restrictions or recommendations, 1 = fail with remediation, 0 = fail not remediable. For the purpose of this study, we dichotomized the final outcome into a pass–fail measure.
Data Management and Analysis
Trained research assistants entered the data into a secure and password-protected database at the university. The principal investigator conducted periodic quality control checks to ensure data accuracy through corrections and identification of missing data. We used PASW Statistics Version 18 (IBM Corporation, Armonk, NY) and SAS Version 9.2 (SAS, Inc., Cary, NC) to perform the analyses.
We conducted descriptive analyses for the demographics, driving history and habits, health-related characteristics, clinical tests, and on-road test data. We determined the criterion validity of the UFOV and Trails B using receiver operating characteristic (ROC) curves. In this study, we viewed an area under the curve (AUC; an index of discriminability) of between 0.7 and 0.9 as having an acceptable magnitude (Streiner & Cairney, 2007). We generated the ROC curve and AUC estimates with SAS Version 9.2. Using cutpoints based on sensitivity and specificity values, we presented the ROC curves for UFOV 1–3, UFOV RI, and Trails B.
On the basis of the cutpoints, we also calculated the associated sensitivity, specificity, error, positive predictive value (PPV), negative predictive value (NPV), and misclassifications (false positives and negatives):
Sensitivity is the predictor test’s ability to obtain a positive test (failing the on-road test) when the condition really exists (a true positive).
Specificity is the predictor test’s ability to obtain a negative result (passing the on-road test) when the condition is really absent (a true negative).
PPV is the probability that the participant will, given a certain cutpoint on the predictor test, fail the on-road test.
NPV is the probability that the participant will, given a cutpoint on the predictor test, pass the on-road test.
The number of false positives (those who receive a failing score but pass the on-road test) and false negatives (those who receive a passing score but fail the on-road test) and the sensitivity and specificity values change with a different cutoff value (Streiner & Cairney, 2007).
The AUC of the ROC curves was based on a 95% confidence interval (CI) and p ≤ .05 to indicate statistical significance. Using DeLong, DeLong, and Clarke-Pearson's (1988) method and to discern a statistically significant difference between the AUC of the independent ROC curves (UFOV RI, UFOV 1–3, and Trails B), we also conducted a contrast analysis with SAS Version 9.2 via the ROCCONTRAST statement in the LOGISTIC procedure.
Results
Driver Characteristics
Table 1 provides the demographics, number of medications, clinical tests, and on-road performance for the drivers. Participants, a majority of whom were women, were mainly White and well educated, and more than half drove 6–7 days/wk. The most commonly avoided conditions were rush-hour traffic and night driving. Drivers had an average self-reported medication use of 7.2 (SD = 4.6). The vision test indicated that the older drivers generally adhered to the Florida State visual requirements.1 As a group, the drivers were well within the acceptable ranges for the MMSE, Trails B, and the UFOV, but about a quarter of the sample failed the on-road test.
Table 1.
Descriptive Statistics for Driver Characteristics, Medications, Comorbidities, Clinical, and On-Road Tests (N = 198)
| Driver Characteristics | Mean (SD) or Frequency (%) | Sample Size |
| Age | 73.86 (6.05) | |
| Gender | ||
| Female | 119 (60.1) | |
| Male | 79 (39.9) | |
| Race | ||
| White | 178 (89.9) | |
| Other | 18 (9.1) | |
| Missing | 2 (1.0) | |
| Education | ||
| ≤High school | 39 (19.7) | |
| Vocational training after high school | 50 (25.3) | |
| ≥College | 107 (54.0) | |
| Missing | 2 (1) | |
| No. medications | 7.22 (4.55) | 194 |
| No. crashes (12 mo) | 18 (25.3) | 118 |
| No. crashes (3 yr) | 12 (15.4) | 78 |
| Driving days per week | ||
| 0–3 | 35 (17.7) | |
| 4–5 | 52 (26.3) | |
| 6–7 | 103 (52.0) | |
| Missing | 8 (4.0) | |
| Avoidance | ||
| Rush hour or heavy traffic | 73 (37.6) | 194 |
| Interstate or highway driving | 24 (12.5) | 192 |
| Rain | 25 (13.0) | 193 |
| Night | 20 (22.5) | 89 |
| Left-hand turns | 27 (13.9) | 194 |
| Other driving situations | 19 (9.8) | 194 |
| Visual acuity: Both | ||
| Vision 20/20–20/40 | 164 (82.8) | |
| Vision 20/50–20/200 | 18 (9.1) | |
| Missing | 16 (8.1) | |
| Visual acuity: Right | ||
| Vision 20/20–20/40 | 170 (85.9) | |
| Vision 20/50–20/200 | 22 (11.1) | |
| Missing | 6 (3.0) | |
| Visual acuity: Left | ||
| Vision 20/20–20/40 | 174 (87.9) | |
| Vision 20/50–20/200 | 18 (9.1) | |
| Missing | 6 (3.0) | |
| UFOV subset | ||
| UFOV 1 (ms) | 32.60 (42.62) | |
| UFOV 2 (ms) | 123.89 (112.01) | |
| UFOV 3 (ms) | 269.88 (118.91) | 196 |
| UFOV risk index | ||
| Very low | 89 (44.9) | |
| Low | 50 (25.3) | |
| Low to moderate | 31 (15.7) | |
| Moderate to high | 20 (10.1) | |
| High to very high | 6 (3.0) | |
| Missing | 2 (1.0) | |
| Trails B | 117.52 (85.91) | |
| MMSE total | 27.92 (5.58) | |
| Road test pass | 165 (83.3) |
Note. For the data collected from 2004 to 2006, we collected crash frequency in the past 12 mo, whereas the data collected from 2010 to 2011 show crash frequency over a period of 3 yr. Other racial categories included African American, American Indian or First Nations, Asian, and Native Hawaiian/Pacific Islander. SD = standard deviation; UFOV = Useful Field of View; MMSE = Mini-Mental State Examination; Trails B = Trail Making Test Part N.
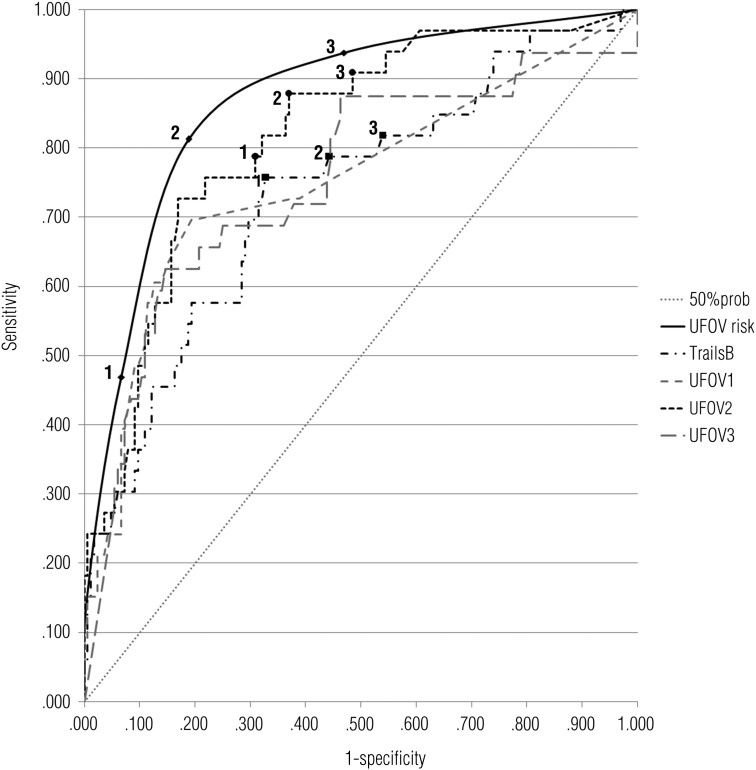
ROC Curves With AUCs
Each ROC curve (UFOV RI and Subtests 1–3 and Trails B), as indicated by the AUC, statistically significantly predicted passing or failing the on-road test with acceptable accuracy (>.70; Streiner & Cairney, 2007). The largest AUC was for the UFOV RI (.86) and UFOV 2 (.82). These findings are illustrated in Supplemental Table 1, available online at http://ajot.aotapress.net (navigate to this article, and click on “Supplemental Materials”).
ROC Curves Contrasted With Trails B
Table 2 indicates the results for each of the UFOV ROCs when contrasted with the Trails B. The only significant difference (estimate = .13, standard error = .05, p = .02) appeared when the UFOV RI was contrasted with the Trails B. Thus, when compared with Trails B, the UFOV RI is a statistically significant better predictor of passing or failing the on-road test. However, the ROC curve for the Trails B was not significantly different from any of the other tests.
Table 2.
ROC Curves Indicating the Contrast With Trails B for Each UFOV Subtest and Risk Index (N = 198)
| Contrast | Estimate | Standard Error | 95% Confidence Interval | p |
| UFOV RI–Trails B | .13 | .05 | [.02, .23] | .02 |
| UFOV 1–Trails B | .02 | .06 | [–.11, .15] | .76 |
| UFOV 2–Trails B | .09 | .053 | [–.02, .19] | .09 |
| UFOV 3–Trails B | .02 | .075 | [–.12, .17] | .76 |
Note. The estimate is derived from subtracting the AUCs of the test indicated in the Contrast column. ROC = receiver operating characteristic; AUC = area under the curve; UFOV = Useful Field of View; 1 = Subtest 1; 2 = Subtest 2; 3 = Subtest 3; RI = Risk Index.
Figure 1 illustrates the ROC curves for Trails B and each of the UFOV tests. Each curves’ AUC exceeds the 50% probability line (also indicated in Supplemental Table 1). Thus, the magnitude of accuracy for each of the curves in predicting on-road outcomes is clearly observable. The values of the three arbitrarily chosen cutpoints for Trails B, UFOV RI, and UFOV 2 (Figure 1) are presented in detail in Table 3, with sensitivity, specificity, PPV, NPV, error, and misclassifications (false positives and negatives) indicated for each of the cutpoints chosen for illustrative purposes.
Figure 1.
Receiver operating characteristic curves for Useful Field of View (UFOV) Subtests 1, 2, and 3; UFOV RI; and Trail Making Test Part B with three arbitrarily chosen cutpoints for UFOV 2, UFOV RI, and Trails B (N = 198).
Note. UFOV risk = UFOV Risk Index; 50% probability is the diagonal dotted line indicating that the area under the curve = 50%.
Table 3.
ROC Curve for UFOV RI, UFOV Subtest 2, and Trails B With Cutpoints Illustrating Sensitivity, Specificity, PPV, NPV, Error, and Misclassifications
| Measure and Cutpoint | SEN | SPE | PPV | NPV | ERROR | MIS+ | MIS− | MIS Total |
| Trails B, s | ||||||||
| Cutpoint 1, ≥106.7 | .76 | .67 | .32 | .93 | .57 | 54 | 8 | 62 |
| Cutpoint 2, ≥90.5 | .79 | .56 | .26 | .93 | .66 | 73 | 7 | 80 |
| Cutpoint 3, ≥82.97 | .82 | .46 | .23 | .93 | .72 | 89 | 6 | 95 |
| UFOV 2, ms | ||||||||
| Cutpoint 1, ≥130.7 | .79 | .69 | .34 | .94 | .52 | 51 | 7 | 58 |
| Cutpoint 2, ≥106.6 | .88 | .63 | .32 | .96 | .49 | 61 | 4 | 65 |
| Cutpoint 3, ≥66.75 | .91 | .52 | .27 | .97 | .58 | 80 | 3 | 83 |
| UFOV RI | ||||||||
| Cutpoint 1, ≥4 | .47 | .93 | .58 | .90 | .60 | 11 | 17 | 28 |
| Cutpoint 2, ≥3 | .81 | .81 | .46 | .96 | .38 | 31 | 6 | 37 |
| Cutpoint 3, ≥2 | .94 | .54 | .28 | .98 | .54 | 78 | 2 | 80 |
Note. N = 198. UFOV RI is the probability of being crash involved (2 = low; 3 = low–moderate, 4 = moderate–high). MIS+ = positive misclassifications (false positive or the number of drivers who passed the on-road test are incorrectly identified fail by the clinical test); MIS− = negative misclassifications (false negative, or the number of drivers who failed the on-road test are incorrectly identified pass by the clinical test; MIS Total = total misclassifications; NPV = negative predictive value; PPV = positive predictive value; RI = Risk Index; ROC = receiver operating characteristic; SEN = sensitivity; SPE = specificity; 2 = Subtest 2; UFOV = Useful Field of View.
ROC Curves With Cutpoints for UFOV RI, UFOV 2, and Trails B
The cutpoint of 106.7 s for the Trails B shown in Table 3 indicates that sensitivity = 76%, specificity = 67%, PPV = 32%, NPV = 93%, and error = 57%. Although the sensitivity was overall lower than that for the third cutpoint (82.97 s; sensitivity = 82%), the specificity was better (67% vs. 46%), and the error associated with the first cutpoint was 15% less than that for the third cutpoint. Thus, choosing the first cutpoint will result, overall, in fewer misclassifications of drivers: that is, 62 misclassifications for the first cutpoint (≥106.7 s) versus 95 for the third cutpoint (≥82.97 s).
In comparing cutpoints across Trails B, UFOV 2, and UFOV RI, the fewest total misclassifications occur at the first cutpoint (≥4) of the UFOV RI. Specifically, of 198 drivers, the fewest total misclassifications occurred for 28 (14%) drivers for the UFOV RI, 62 (31.3%) for the Trails B, and 58 (29.3%) for UFOV 2. The sensitivity of UFOV RI for the first cutpoint, however, was 47% with an error of 60%, the worst compared with that for the first cutpoint for Trails B, with sensitivity of 76% and an error of 57%, or for the first cutpoint for the UFOV 2, with sensitivity of 79% and an error of 52%. Comparing Trails B with the UFOV 2, we observed similar ROC curve properties, with Trails B having 4 more misclassifications and a 5% higher error rate.
Discussion
This study determined, in a group of community-dwelling older licensed drivers, whether Trails B predicts pass–fail outcomes of an on-road test in a fashion similar to the UFOV RI and the UFOV 2. Overall, the participants were White, of a high educational level, and nearly daily drivers who reported avoidance behaviors. Although the group reported a variety of medications used, they had adequate visual, visual–cognitive (UFOV), cognitive, and motor performance skills; as such, they can be considered a relatively healthy group of older drivers.
Each of the ROC curves indicated that the five tests could predict on-road outcomes with acceptable accuracy. However, the most accurate prediction was observed for UFOV RI (AUC = .86) and UFOV 2 (AUC = .82). When the Trails B was contrasted with the UFOV RI, the findings indicated that the latter was a superior screening test in predicting on-road outcomes among older drivers. However, when contrasted with the UFOV 1, 2, and 3, Trails B was comparable in accuracy to predict on-road outcomes.
In comparing Trails B cutpoints with those of UFOV RI and UFOV 2, three important findings emerged: First, screening tools predictive of on-road driving performance require high sensitivity (true positives or failures) with good PPV (probability that the participants, given a certain cutpoint on the screening test, will fail the road test) and low misclassifications. Decisions regarding the ultimate cutpoint should be based on the accuracy of the screening test yet also correct classifications of the drivers. Thus, researchers are encouraged to report not only sensitivity and specificity but also the positive and negative predictive values, error, and misclassifications associated with ROCs.
Second, Trails B, when compared with the UFOV 2, had 4 more misclassified drivers. Compared with the cost associated with obtaining and administering the UFOV, however, the Trails B allows for cheaper, quicker, and easier test administration. Occupational therapists may consider using the Trails B, per protocol, when they do not have access to the UFOV.
Third, the UFOV RI yielded the fewest misclassifications—28 of 198—at a cutpoint of ≥4 when compared with the best cutpoints for Trails B (62) and UFOV 2 (58). However, its sensitivity was low (47%), and its error was high (.60). In this sample, at least, a cutpoint ≥ 3 seems to be a better choice despite the fact that 37 drivers may be misclassified.
Limitations and Future Research
The predominantly White sample was not representative of the general spectrum of older adults, lacking adequate representation of minorities and those with low educational status. Generalizations can only be made to drivers who fit the participants’ profile.
Spectrum bias was evident in our study because >80% of the participants passed the on-road test, and as such the predictive value of the tests examined may be inflated. Because of the high proportion of participants who did well on the tests and passed the on-road component (spectrum bias), a possibility exists that specificity, PPV, and NPV are inflated. We had missing data, as indicated in Table 1, and all participants were from one geographical area in the United States. Because data were collected at two time points (2004–2006 and 2010–2011), not all variables were consistent; for example, we collected crash frequency in the last 12 mo of 2004–2006, whereas for 2010–2011 we collected crash data over a 3-yr period.
Future research may determine how concurrent validity of the UFOV RI versus Trails B for on-road outcomes may be examined in a prospective study. Likewise, predictive validity of the UFOV RI versus Trails B for on-road outcomes may also be examined longitudinally. This study contributes to the literature by suggesting that the UFOV RI, when compared with the UFOV 2 and Trails B, is a superior tool to predict on-road outcomes in older drivers. However, as a predictive tool of on-road outcomes, the Trails B yields similar results to the UFOV 2. Trails B is cheaper and easier to administer than the UFOV 2, and as such may be used as a screening tool by clinicians who do not have access to the UFOV testing battery to identify at-risk older drivers.
Major Study Findings and Applications to Occupational Therapy Practice
When contrasted with the Trails B and other UFOV subtests, the UFOV RI is a superior screening test for predicting on-road outcomes among community-dwelling older licensed drivers. As a screening tool, Trails B has acceptable accuracy, with an AUC = 73%, and is comparable to UFOV Subtests 1–3 in predicting on-road outcomes. Researchers must consider various UFOV and Trails B ROC curve cutpoints and misclassification of participants, beyond sensitivity and specificity values, to make fair determinations in identifying at-risk older drivers. This research may guide clinical practice by determining more accurate cutpoints for identifying at-risk older drivers and the utility of this statistical approach.
Acknowledgments
The project was funded by the Department of Transportation (DOT 00063055; Principal Investigator, Sherrilene Classen) and Florida Department of Transportation Project BDK77.
Footnotes
Visual acuity = (1) Each or both eyes without correction 20/40; if 20/50 or less, applicant is referred to an eye specialist for possible improvement; (2) each or both eyes with correction 20/70; worse eye must be better than 20/200; (3) if one eye is blind, the other must be 20/40 with or without correction. The absolute visual acuity minimum = 20/70. Bioptic telescopes are not allowed. Visual fields = Minimum field requirement 130° horizontal.
Contributor Information
Sherrilene Classen, Sherrilene Classen, PhD, MPH, OTR/L, is Professor and Director, School of Occupational Therapy, Elborn College, Western University, London, Ontario, Canada, N6A 5B9; sclassen@uwo.ca. At the time of the study, she was Director, Institute for Mobility, Activity and Participation, and Associate Professor, Department of Occupational Therapy, College of Public Health and Health Professions, University of Florida, Gainesville.
Yanning Wang, Yanning Wang, MS, is Doctoral Student, Department of Epidemiology, College of Public Health and Health Professions, University of Florida, Gainesville.
Alexander M. Crizzle, Alexander M. Crizzle, PhD, MPH, is Postdoctoral Associate, Institute for Mobility, Activity and Participation, and Department of Occupational Therapy, College of Public Health and Health Professions, University of Florida, Gainesville
Sandra M. Winter, Sandra M. Winter, PhD, OTR/L, is Research Coordinator, Institute for Mobility, Activity and Participation, and Postdoctoral Associate, Department of Occupational Therapy, College of Public Health and Health Professions, University of Florida, Gainesville
Desiree N. Lanford, Desiree N. Lanford, MOT, OTR/L, CDRS, is Certified Driving Rehabilitation Specialist, Institute for Mobility, Activity and Participation and Department of Occupational Therapy, College of Public Health and Health Professions, University of Florida, Gainesville
References
- Ball K. K., Beard B. L., Roenker D. L., Miller R. L., Griggs D. S. Age and visual search: Expanding the Useful Field of View. Journal of the Optical Society of America A: Optics and Image Science. 1988;5:2210–2219. doi: 10.1364/josaa.5.002210. http://dx.doi.org/10.1364/JOSAA.5.002210 . [DOI] [PubMed] [Google Scholar]
- Ball K. K., Berch D. B., Helmers K. F., Jobe J. B., Leveck M. D., Marsiske M., Willis S. L. Advanced Cognitive Training for Independent and Vital Elderly Study Group. Effects of cognitive training interventions with older adults: A randomized controlled trial. JAMA. 2002;288:2271–2281. doi: 10.1001/jama.288.18.2271. http://dx.doi.org/10.1001/jama.288.18.2271 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball K. K., Owsley C. The Useful Field of View Test: A new technique for evaluating age-related declines in visual function. Journal of the American Optometric Association. 1993;64:71–79. [PubMed] [Google Scholar]
- Ball K. K., Owsley C., Sloane M. E., Roenker D. L., Bruni J. R. Visual attention problems as a predictor of vehicle crashes in older drivers. Investigative Ophthalmology and Visual Science. 1993;34:3110–3123. [PubMed] [Google Scholar]
- Bédard M. B., Parkkari M., Weaver B., Riendeau J., Dahlquist M. Assessment of driving performance using a simulator protocol: Validity and reproducibility. American Journal of Occupational Therapy. 2010;64:336–340. doi: 10.5014/ajot.64.2.336. http://dx.doi.org/10.5014/ajot.64.2.336 . [DOI] [PubMed] [Google Scholar]
- Classen S., Horgas A., Awadzi K., Messinger-Rapport B., Shechtman O., Joo Y. Clinical predictors of older driver performance on a standardized road test. Traffic Injury Prevention. 2008;9:456–462. doi: 10.1080/15389580802260026. http://dx.doi.org/10.1080/15389580802260026 . [DOI] [PubMed] [Google Scholar]
- Classen S., Witter D. P., Lanford D. N., Okun M. S., Rodriguez R. L., Romrell J., Fernandez H. H. Usefulness of screening tools for predicting driving performance in people with Parkinson’s disease. American Journal of Occupational Therapy. 2011;65:579–588. doi: 10.5014/ajot.2011.001073. http://dx.doi.org/10.5014/ajot.2011.001073 . [DOI] [PubMed] [Google Scholar]
- Clay O. J., Wadley V. G., Edwards J. D., Roth D. L., Roenker D. L., Ball K. K. Cumulative meta-analysis of the relationship between Useful Field of View and driving performance in older adults: Current and future implications. Optometry and Vision Science. 2005;82:724–731. doi: 10.1097/01.opx.0000175009.08626.65. http://dx.doi.org/10.1097/01.opx.0000175009.08626.65 . [DOI] [PubMed] [Google Scholar]
- DeLong E. R., DeLong D. M., Clarke-Pearson D. L. Comparing the areas under two or more correlated receiver operating characteristic curves: A nonparametric approach. Biometrics. 1988;44:837–845. [PubMed] [Google Scholar]
- Duchek J. M., Hunt L., Ball K. K., Buckles V., Morris J. C. Attention and driving performance in Alzheimer’s disease. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 1998;53:130–141. doi: 10.1093/geronb/53b.2.p130. http://dx.doi.org/10.1093/geronb/53B.2.P130 . [DOI] [PubMed] [Google Scholar]
- Edwards J. D., Ross L. A., Wadley V. G., Clay O. J., Crowe M., Roenker D. L., Ball K. K. The Useful Field of View test: Normative data for older adults. Archives of Clinical Neuropsychology. 2006;21:275–286. doi: 10.1016/j.acn.2006.03.001. http://dx.doi.org/10.1016/j.acn.2006.03.001 . [DOI] [PubMed] [Google Scholar]
- Fisk G. D., Novack T., Mennemeier M., Roenker D. Useful Field of View after traumatic brain injury. Journal of Head Trauma Rehabilitation. 2002;17:16–25. doi: 10.1097/00001199-200202000-00004. http://dx.doi.org/10.1097/00001199-200202000-00004 . [DOI] [PubMed] [Google Scholar]
- Folstein M. F., Folstein S. E., McHugh P. R. “Mini-Mental State”: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. http://dx.doi.org/10.1016/0022-3956(75)90026-6 . [DOI] [PubMed] [Google Scholar]
- Goode K. T., Ball K. K., Sloane M., Roenker D. L., Roth D. L., Myers R. S., Owsley C. Useful Field of View and other neurocognitive indicators of crash risk in older adults. Journal of Clinical Psychology in Medical Settings. 1998;5:425–440. http://dx.doi.org/10.1023/A:1026206927686 . [Google Scholar]
- Hunt L. A., Bassi C. J. Near-vision acuity levels and performance on neuropsychological assessments used in occupational therapy. American Journal of Occupational Therapy. 2010;64:105–113. doi: 10.5014/ajot.64.1.105. http://dx.doi.org/10.5014/ajot.64.1.105 . [DOI] [PubMed] [Google Scholar]
- Justiss M. D., Mann W. C., Stav W., Velozo C. Development of a behind-the-wheel driving performance assessment for older adults. Topics in Geriatric Rehabilitation. 2006;22:121–128. [Google Scholar]
- Lezak M. Neuropsychological assessment. 3rd ed. New York: Oxford University Press; 1995. [Google Scholar]
- Mackworth N. H. Visual noise causes vision tunnel. Psychonomic Science. 1965;3:67–68. [Google Scholar]
- Marcotte T. D., Wolfson T., Rosenthal T. J., Heaton R. K., Gonzalez R., Ellis R. J., Grant I. A multimodal assessment of driving performance in HIV infection. Neurology. 2004;63:1417–1422. doi: 10.1212/01.wnl.0000141920.33580.5d. [DOI] [PubMed] [Google Scholar]
- Marshall S. C., Molnar F., Man-Son-Hing M., Blair R., Brosseau L., Finestone H. M., Wilson K. G. Predictors of driving ability following stroke: A systematic review. Topics in Stroke Rehabilitation. 2007;14:98–114. doi: 10.1310/tsr1401-98. http://dx.doi.org/10.1310/tsr1401-98 . [DOI] [PubMed] [Google Scholar]
- Mazer B. L., Sofer S., Korner-Bitensky N., Gelinas I., Hanley J., Wood-Dauphinee S. Effectiveness of a visual attention retraining program on the driving performance of clients with stroke. Archives of Physical Medicine and Rehabilitation. 2003;84:541–550. doi: 10.1053/apmr.2003.50085. http://dx.doi.org/10.1053/apmr.2003.50085 . [DOI] [PubMed] [Google Scholar]
- Milner B. Effects of different brain lesions on card sorting: The role of the frontal lobes. Archives of Neurology. 1963;9:90–100. http://dx.doi.org/10.1001/archneur.1963.00460070100010 . [Google Scholar]
- Mullen N. W., Weaver B., Riendeau J. A., Morrison L. E., Bédard M. Driving performance and susceptibility to simulator sickness: Are they related? American Journal of Occupational Therapy. 2010;64:288–295. doi: 10.5014/ajot.64.2.288. http://dx.doi.org/10.5014/ajot.64.2.288 . [DOI] [PubMed] [Google Scholar]
- Novack T. A., Baños J. H., Alderson A. L., Schneider J. J., Weed W., Blankenship J., Salisbury D. UFOV performance and driving ability following traumatic brain injury. Brain Injury. 2006;20:455–461. doi: 10.1080/02699050600664541. http://dx.doi.org/10.1080/02699050600664541 . [DOI] [PubMed] [Google Scholar]
- Owsley C., Ball K. K., McGwin G., Jr, Sloane M. E., Roenker D. L., White M. F., Overley E. T. Visual processing impairment and risk of motor vehicle crash among older adults. JAMA. 1998;279:1083–1088. doi: 10.1001/jama.279.14.1083. http://dx.doi.org/10.1001/jama.279.14.1083 . [DOI] [PubMed] [Google Scholar]
- Posse C., McCarthy D. P., Mann W. C. A pilot study of interrater reliability of the Assessment of Driving-Related Skills: Older driver screening tool. Topics in Geriatric Rehabilitation. 2006;22:113–120. [Google Scholar]
- Reitan R. M. Validity of the Trail Making Test as an indicator of organic brain damage. Perceptual and Motor Skills. 1958;8:271–276. [Google Scholar]
- Reynolds C. Comprehensive Trail Making Test (CTMT) Austin, TX: Pro-Ed; 2002. [Google Scholar]
- Rubin G. S., Ng E. S., Bandeen-Roche K., Keyl P. M., Freeman E. E., West S. K. A prospective, population-based study of the role of visual impairment in motor vehicle crashes among older drivers: The SEE study. Investigative Ophthalmology and Visual Science. 2007;48:1483–1491. doi: 10.1167/iovs.06-0474. http://dx.doi.org/10.1167/iovs.06-0474 . [DOI] [PubMed] [Google Scholar]
- Stav W. B., Justiss M. D., McCarthy D. P., Mann W. C., Lanford D. N. Predictability of clinical assessments for driving performance. Journal of Safety Research. 2008;39:1–7. doi: 10.1016/j.jsr.2007.10.004. http://dx.doi.org/10.1016/j.jsr.2007.10.004 . [DOI] [PubMed] [Google Scholar]
- Streiner D. L., Cairney J. What’s under the ROC? An introduction to receiver operating characteristics curves. Canadian Journal of Psychiatry. 2007;52:121–128. doi: 10.1177/070674370705200210. [DOI] [PubMed] [Google Scholar]
- Uc E. Y., Rizzo M., Anderson S. W., Sparks J., Rodnitzky R. L., Dawson J. D. Impaired visual search in drivers with Parkinson’s disease. Annals of Neurology. 2006;60:407–413. doi: 10.1002/ana.20958. http://dx.doi.org/10.1002/ana.20958 . [DOI] [PubMed] [Google Scholar]