Abstract
Background
Routine screening and advice regarding risky lifestyle behaviours is appropriate in the primary care setting, but often not implemented. Routine electronic collection of patients’ self-reported data may streamline the collection of such information.
Aim
To explore the perceptions of GPs and their attending patients regarding the acceptability of waiting-room touchscreen computers for the collection of health behaviour information. Uptake, ease of operation, and the perceived likelihood of future implementation were studied.
Design and setting
Cross-sectional health-risk survey. General practices in metropolitan areas in Australia.
Method
Practices were randomly selected by postcode. Consecutive patients who were eligible to take part in the study were approached in the waiting room and invited to do so. Participants completed the touchscreen health survey. A subsample of patients and GPs completed additional items regarding acceptability.
Results
Twelve general practices participated in the study, with 4058 patients (86%) and 51 of 68 (75%) GPs consenting to complete the health-risk survey, 596 patients and 30 GPs were selected to complete the acceptability survey. A majority of the 30 GPs indicated that the operation of the survey was not disruptive to practice and more than 90% of patients responded positively to all items regarding its operation. More than three-quarters of the patient sample were willing to consider allowing their responses to be kept on file and complete such surveys in the future.
Conclusion
As waiting-room-based collection of this information appears to be both feasible and acceptable, practitioners should consider collecting and incorporating routine patient-reported health behaviours for inclusion in the medical record.
Keywords: acceptability, chronic disease, e-health, general practice, primary care, touchscreen computer
INTRODUCTION
Chronic conditions are leading causes of morbidity and mortality internationally.1,2 In the case of highly prevalent chronic conditions, such as cancer, heart disease, diabetes, and depression, minimising their impacts requires improvements in prevention and early detection.3 Despite public-health campaigns, adherence to preventive health guidelines falls well short of optimal: in Australia only one in 10 adults meet the recommended dietary guidelines for fruit and vegetable intake,4 while participation rates for cancer screening are 56% for breast cancer and 61% for cervical cancer.5 Primary care is a key setting for systematically improving prevention, given that a large proportion of the population regularly visits a GP,6,7 and that both patients and GPs consider preventive care to be an important part of a GP’s role.8,9
Recommendations regarding preventive care are not implemented systematically in general practice.9 Less than half of general practice patients are adequately screened for risk of developing cardiovascular disease.10 Only 62% of eligible women (that is, women aged 50–69 years who visited a GP in Australia in 2003), receive mammography advice from their GPs.5 Important health-risk behaviours such as smoking11 and alcohol consumption12 can be poorly detected in the general practice setting. Time pressures appear to be a particular cause of inconsistency in detecting and advising patients who are at risk.8 Lack of staff and lack of financial reimbursement may also act as barriers to systematic prevention efforts in general practice.13
Electronic options for preventive health-risk management have grown substantially14 and have been shown to improve preventive care;15 these include breast and cervical screening.16 Collecting health-risk information from the patient in the waiting room is an under-explored opportunity to collect health information electronically. Routinely collected patient responses could be used to identify and prioritise preventive needs in addition to addressing the purpose of a particular visit. This is particularly important given the increasing health burden associated with health behavioural issues, which only the patient can report, such as nutrition,17 physical (in)activity,17 and depression.18 Patients may prefer electronic methods of data collection over print,19 and agree that electronic collection of personal data prior to consulting their GP will ensure a better focus on relevant preventive care issues.20 GPs have rated electronic data collection as useful for identifying patient status in relation to health behaviours such as smoking, alcohol use, and various types of health screening.20 Pilot work from other groups supports the potential of electronic approaches to identify patient risk and generate management recommendations.21
How this fits in
Previous studies have used touchscreen-based data-collection methods to obtain data on health behaviours in the research context. This study adds the views of patients and providers regarding the appropriateness of making such data collection a regular or routine part of a visit to primary care. The positive findings suggest that although not all patients would be willing to complete a full set of behavioural items at every primary care visit, it is highly likely that most would complete a full set of items on at least one occasion, with the majority willing to provide this information regularly. This overcomes one of the oft-cited barriers to increasing rates of preventive care; that is, lack of time to ask patients pertinent questions.
A key aspect of the success of electronic approaches is whether they are acceptable to users. Although computer-based records have become the norm in the primary care setting and are commonly used as a research tool,22 the acceptability of computer-based tools to regularly assess patients’ self-reported health behaviour has received little attention.23 The systematic implementation of electronic data collection requires three key elements:
a high proportion of patients must agree to complete relevant items and be able to complete sufficient items while waiting for their appointment;
the smooth operation of data collection is essential, including a perception that the computer technology is easy to use; and
patients must be willing to have their responses become part of their medical record and to continue the data-collection process at future appointments.
On the part of the provider, sustained implementation requires a perception that the approach does not unduly increase workload and is feasible to incorporate into practice.
This study aimed to explore the perceptions of a cross-section of GPs and the patients attending their practice regarding the acceptability of using waiting-room touchscreen computers to collect health-screening data. Uptake (patient response rates), operation (completion times and perceived ease of completion), and perceived future implementation were assessed.
METHOD
The data presented here are part of a larger dataset collected in general practices, which have been described in detail elsewhere.24
Recruitment of general practices and GPs
Twelve general practices in Australia participated in the study. GP practices were selected from three metropolitan and one non-metropolitan region via the Medical Directory of Australia and an online telephone directory. General practices were eligible if the equivalent of at least two full-time GPs consented to participate. Postcodes in each area were generated and practices within a randomly selected postcode were approached. An invitation letter, information statement, and consent form were sent out to GPs and practice managers; two follow-up telephone calls were made to the practice and additional information was sent out if requested.
Recruitment of patients
To be eligible to participate in the study patients had to be:
presenting for general practice care;
aged ≥18 years;
able to understand English; and
able to provide informed consent.
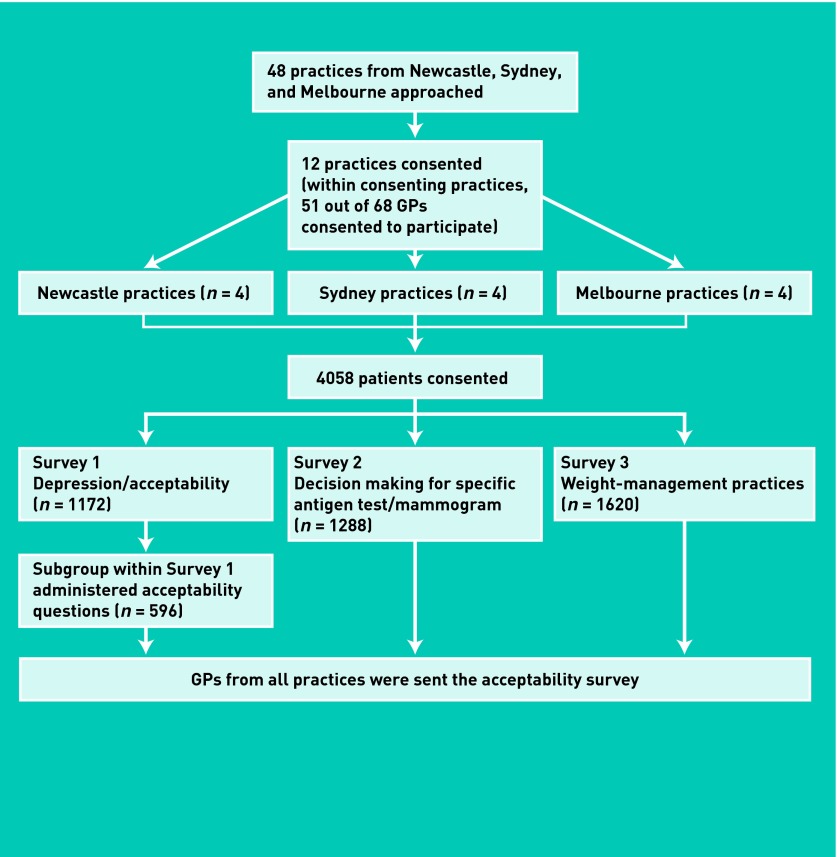
Consecutive participants who were eligible were approached by the research assistant in the practice waiting room and invited to participate in the study. The acceptability items (one of three surveys) were completed by a subsample of consecutive patients over the initial months of recruitment at all practices (Figure 1). Of those who were approached to complete this survey, 86% consented to participate. There was no indication of any difference in sex and estimated age between those who consented and those who did not consent to participate. Of those who consented, none specifically chose not to answer the acceptability questions.
Figure 1.
Flowchart of study design.
Data collection
Patients completed a survey by touchscreen computer in the waiting room of the general practice prior to their appointment; GPs completed a hard-copy survey on completion of the patient recruitment. A commercial program, Digivey Survey Suite software (CREOSO®), was used to create and administer the patient survey. The survey was administered using Dell Latitude XT2 touchscreen computers; all equipment was purchased in 2010.
A research assistant was present in the practice and was able to ensure that the laptops were not removed. Laptops were cleaned with alcohol wet wipes between each patient’s use of them.
Measures
GP acceptability
GPs reported whether the survey:
could be implemented as part of routine practice;
was an acceptable way to collect patient data prior to consultation;
was well received by patients;
was disruptive to the waiting area;
increased staff burden; or
increased patient waiting times.
Patient response rates and completion times
The study research assistant recorded the sex and estimated the age of each eligible patient who chose not to commence the survey. The touchscreen computer recorded survey completion times.
Patient demographics
Patients reported on their age, sex, highest level of education (primary school; high school; trade qualification; university qualification; other, for example, non-university diploma), private health insurance status, and whether or not they had a war veteran’s affairs card, or a commonwealth healthcare concession card, which served as an indicator of low income. Age was categorised into 18–24 years and 5-year brackets up to the age of 59 and all ages ≥60 years.
Patient health
Participants indicated the main reason for consulting their GP on the day. All completed items on previous medical history, current health status, and recent care in relation to depression, blood pressure, cholesterol, heart disease, diabetes, cancer, stroke, and chronic pain.
Depression was assessed using the 9-item Patient Health Questionnaire; a tool that has been used in the primary care setting and shows a high correlation with functional status on the 20-item Short Form Survey subscales.
Items on screening were only presented to those who were eligible for such care according to national guidelines on the basis of age, sex, and medical history. These responders were asked to indicate the timeframe in which they had their last screening test for colorectal cancer, breast cancer, cervical cancer, and melanoma.
Lifestyle risk-factor items used validated tools such as the Alcohol Use Disorders Identification Test — Consumption questionnaire and the New South Wales Health Survey. Cardiovascular disease metabolic risk-factor screening and body mass index were assessed via self-report. Although data on patient health is not reported here, completion of these items was incorporated in the assessment of survey completion times. The total number of survey items completed varied according to patient age, sex, and health status.
Patient acceptability
Participants indicated whether:
the survey instructions were easy to follow;
the questions were easy to understand;
the touchscreen was easy to use;
there was enough time to complete the questions prior to the appointment; and
they felt comfortable answering the questions.
The response categories were: strongly agree, agree, unsure, disagree, or strongly disagree.
Two further items asked whether the participant would be happy (yes, no, unsure) for the doctor to have a copy of the answers for their medical record and how often they would be willing to complete the touchscreen survey (once only, less than half of visits, half of visits, most visits, or every visit).
Statistical analyses
Data analyses were conducted using SAS (version 9.2). The response categories of strongly agree/agree were collapsed for all analyses, as were the strongly disagree/disagree response categories. Completion times for each participant were collapsed into three groups (<10 minutes, 10–15 minutes, >15 minutes) and a χ2 test was conducted to identify differences in completion time, according to participant characteristics.
Fisher’s exact tests were conducted to identify differences for each patient acceptability criterion (including all three response categories: yes, no, unsure) according to each participant characteristic (age group, sex, education [Year 10 or less, Higher School Certificate, trade qualification, university, or other], healthcare card or private health insurance status). With a sample size of 596 for each variable, the study has 70% power to detect a 10% difference in proportions at the 50% prevalence level (for example, yes = 328, no = 268). Using the actual data set (for example, yes = 583, no = 13), the study has almost 100% power.
RESULTS
GP and practice sample
A total of 48 practices were approached to participate, of which 12 consented, giving a practice consent rate of 25%. All practices were located in urban areas (according to the Accessibility/Remoteness Index of Australia classification) and practised bulk billing (no out-of-pocket costs) to veteran and healthcare card holders. All practices except one had a practice nurse; there were no differences in size (number of GPs) between practices that did and did not consent.
Within consenting practices, 51 out of 68 (75%) GPs who were approached consented to participate. An average of 5.4 GPs worked in a consenting practice. Of the consenting 51 GPs, 63% (n = 32) were males, 57% (n = 29) were aged ≥50 years, 51% (n = 26) had worked in general practice for >20 years, and 63% (n = 32) worked eight or more sessions a week.
Patient uptake
A total of 5667 patients were approached to participate in the larger study. Of the patients presenting for general practice care, 17% were not eligible (3% were non-English speaking; 43% were <18 years of age, 11% were unable to complete a survey due to reasons including visual impairment or feeling too sick, 3% were presenting for care to allied health practitioners, and 40% for other reasons (including having completed the survey previously and accompanying someone else who was the patient). A total of 4705 patients were eligible to participate. Of those eligible, 4058 (86%) agreed to participate. A comparison of the sex of patients who did and did not consent found no significant differences between the two groups (χ2 = 0.1.3089; degrees of freedom = 1; P = 0.253).
A subsample of 596 (15%) participants completed the acceptability items.
Perceived operation of the touchscreen survey
Of the 51 GPs who consented to participate, 30 (59%) completed the acceptability survey. There were no differences in sex between those who completed the survey and those who did not. The mean age of those who completed the survey was 49.7 years compared with 53 years for those who did not. The mean number of years practising as a GP for those who completed the survey was 20.4 years compared with 21.7 years for those who did not. A minority of the 30 GPs who completed the survey reported that the touchscreen survey:
increased patient waiting times (n = 7; 23%);
increased staff burden (n = 7; 23%); or
was disruptive to the waiting area (n = 2; 7%).
The majority of GPs reported that the touchscreen survey was well received by patients (n = 25; 83%).
Survey completion time was available for 2992 patients, representing 74% of consenting participants. Completion time was ≤15 minutes for 89% of patients, with 58% of patients completing the survey in <10 minutes. Completion time was not significantly different on the basis of age group (P = 0.297), sex (P = 0.792), education (P = 0.724), whether the patient had attended the clinic on a prior occasion (0.433), whether or not the purpose of the visit was for a new problem (P = 0.937), having a veteran’s card (P = 0.918), having a healthcare concession card (P = 0.612), or having private health insurance (P = 0.691).
Of the 596 participants who completed the module on acceptability, 593 reported that they had sufficient time to complete the survey while waiting for their appointment. As shown in Table 1, the responses to each survey item in relation to ease of operation were highly positive, being ≥95% for all groups with one exception; those aged ≥60 years were significantly less likely to report that the touchscreen was easy to use (94%, P<0.001).
Table 1.
Perceived acceptability of operation of touchscreen survey according to patient characteristics (n = 596)
| Characteristic | Instructions easy to follow | Questions easy to understand | Touchscreen easy to use | Patient felt comfortable answering questions |
|---|---|---|---|---|
|
|
|
|
|
|
| Yes, n (%) | Yes, n (%) | Yes, n (%) | Yes, n (%) | |
| Total | 594 (100) | 593 (100) | 583 (98) | 577 (97) |
|
| ||||
| Age, years | ||||
| 18–39 | 165 (99) | 166 (100) | 166 (100) | 161 (97) |
| 40–59 | 196 (100) | 196 (100) | 196 (100) | 186 (95) |
| ≥60 | 233 (100) | 231 (99) | 221 (94)a | 230 (98) |
|
| ||||
| Sex | ||||
| Male | 215 (100) | 214 (99) | 212 (98) | 210 (97) |
| Female | 379 (100) | 379 (100) | 371 (98) | 367 (97) |
|
| ||||
| Education | ||||
| Year 10 or below | 112 (98) | 112 (98) | 110 (96) | 111 (97) |
| HSC | 111 (100) | 111 (100) | 106 (95) | 107 (96) |
| Trade qualified | 91 (100) | 91 (100) | 89 (98) | 89 (98) |
| University | 262 (100) | 261 (100) | 260 (99) | 253 (97) |
| Other | 18 (100) | 18 (100) | 18 (100) | 17 (94) |
|
| ||||
| Healthcare card | ||||
| Yes | 129 (100) | 129 (100) | 126 (98) | 127 (98) |
| No | 465 (100) | 464 (99) | 457 (98) | 450 (96) |
|
| ||||
| Private health insurance | ||||
| Yes | 418 (100) | 417 (100) | 412 (98) | 403 (96) |
| No | 176 (99) | 176 (99) | 171 (97) | 174 (98) |
|
| ||||
| Reasons for visit | ||||
| New problem | 129 (100) | 129 (100) | 127 (98) | 127 (98) |
| Other | 465 (100) | 464 (99) | 456 (98) | 450 (96) |
P<0.001. HSC = Higher School Certificate.
Expected implementation of the touchscreen survey
The majority of the 30 GPs completing the acceptability survey reported that the touchscreen computer survey could be implemented as part of routine practice (n = 22) and was an acceptable way to collect patient data prior to general practice consultations (n = 26).
As shown in Table 2, 77% of patients were willing to have the survey data kept in the practice files, while 8% were unsure. Participants aged ≥60 years were more willing for the data to be kept on file than the younger age groups (P<0.001). More than 60% of participants were willing to complete this type of survey at each future GP visit, with no significant differences found in relation to sociodemographic characteristics.
Table 2.
Perceived acceptability of implementation of touchscreen survey according to patient characteristics.
| Characteristic | Data can go on file | Willing to complete surveys on each future visit | ||
|---|---|---|---|---|
|
|
|
|||
| Yes, n (%) | Unsure, n (%) | Yes, n (%) | Unsure, n (%) | |
| Total | 456 (77) | 48 (8) | 359 (60) | 98 (17) |
|
| ||||
| Age, years | ||||
| 18–39 | 111 (67) | 17 (10) | 102 (62) | 27 (16) |
| 40–59 | 144 (73) | 21 (11) | 121 (62) | 37 (19) |
| ≥60 | 201 (86)a | 10 (4.3) | 136 (58) | 34 (15) |
|
| ||||
| Sex | ||||
| Male | 163 (75) | 20 (9.3) | 122 (56) | 40 (19) |
| Female | 293 (77) | 28 (7.4) | 237 (63) | 58 (15) |
|
| ||||
| Education | ||||
| Year 10 or below | 95 (83) | 3 (2.6) | 72 (63) | 13 (11) |
| HSC | 86 (77) | 9 (8.1) | 71 (64) | 19 (17) |
| Trade qualification | 74 (81) | 6 (6.6) | 55 (60) | 14 (15) |
| University | 188 (72) | 30 (11) | 151 (58) | 50 (19) |
| Other | 13 (72) | 0 | 10 (59) | 2 (12) |
|
| ||||
| Healthcare card | ||||
| Yes | 98 (76) | 9 (7.0) | 74 (58) | 19 (15) |
| No | 358 (77) | 39 (8.4) | 285 (61) | 79 (17) |
|
| ||||
| Private health insurance | ||||
| Yes | 323 (77) | 37 (8.8) | 249 (59) | 73 (17) |
| No | 133 (75) | 11 (6.2) | 110 (63) | 25 (14) |
|
| ||||
| Reasons for visit | ||||
| New problem | 110 (85) | 6 (4.7) | 87 (68) | 22 (17) |
| Other | 346 (74) | 42 (9.0)b | 272 (58) | 76 (16)c |
P<0.005 for comparison of ‘yes’ versus ‘no’ versus ‘unsure’. The ‘No’ response data is not presented here but can be imputed.
P = 0.029.
P = 0.038. HSC = Higher School Certificate.
DISCUSSION
Summary
Although electronic devices are widely used, this study is one of very few to establish the acceptability and feasibility of such an approach for collecting routine preventive care data in the waiting rooms of general practices. High rates of ease of operation were reported by patients, while the majority of GPs indicated that the waiting-room computer survey was well received and not disruptive. As only 11% of participants took >15 minutes to complete the survey, the approach is likely to be accommodated during pre-appointment waiting times for most patients.
Given the generally acceptable accuracy of survey-based self-reporting for health behaviours such as smoking,25,26 alcohol use,27 and physical activity,28 the touchscreen approach is likely to provide information that is sufficiently accurate to act as a systematic prompt to preventive care by the GP. In the case of complex behaviours or conditions, such information could act as the first step in a screening or diagnostic process, alerting the GP to the need for a more in-depth assessment. Additionally, the use of electronic assessments allows for the tailoring of follow-up questions.
Strengths and limitations
Although the overall findings suggest that it is feasible and acceptable to use touchscreen computers to collect patients’ self-reported data for inclusion in the medical record, it should be noted that the findings of the study may not generalise to those who do not read English. However, it is likely that non-English versions of the tool could be developed, as could spoken-word versions. It is also likely that those GPs and patients who agreed to be involved in the study and who completed the survey would be more likely to take a positive view than those who did not participate; as such, it may be necessary to trial the approach with a less-enthusiastic group of participants.
Acceptability is likely to be slightly overestimated as non-participants may consider the process unacceptable and the survey items may have had a limited ability to discriminate between responses. Social desirability may also have resulted in an overestimation of acceptability. In addition, there is a chance that the sample may under-represent those patients who attend their GP infrequently.
Comparison with existing literature
High rates of acceptability (generally over 95%) regarding the ease of operation of the touchscreen survey suggest this approach is usable for the vast majority of patients. Although those aged ≥60 years were less likely to rate the touchscreen as easy to use than their younger counterparts, acceptability was still high at 94%; this suggests that only minor improvements in presentation or providing help for a small group of patients would be required to achieve full acceptance of electronic data collection in primary care.
Although rates of agreement for implementation were lower than for ease of operation, even a moderate level of participation is likely to substantially increase healthcare providers’ ability to readily identify patients who would benefit from some aspect of preventive care. A streamlined survey, particularly for those who make multiple visits within a 6- or 12-month period, may increase the proportion of patients who are willing to complete data collection on regular occasions.
These positive findings are not surprising in the context of previous studies,29–31 which have found high response rates using touchscreen-based data collection for health behaviours in clinical settings. How this study differs from the earlier work is in its focus on the views of patients and providers regarding the appropriateness of making such data collection a regular or routine part of a visit to primary care. The positive findings indicate that most patients would complete a full set of items on at least one occasion, with a majority willing to do so regularly. This overcomes one of the often cited barriers to increasing rates of preventive care; that is, the time that is needed to ask patients about their medical history, lifestyle, and behaviours. Simple algorithms can be used to alert the practitioner to the need to address the issue or to ask the patient to return to the practice to discuss important preventive health issues.
Implications for practice
Given the increasing importance of monitoring health behaviours to capitalise on opportunities for prevention, electronic monitoring, and collation of those responses, is likely to be valuable to healthcare providers as a means of prioritising preventive health issues for consultation. As waiting-room based collection of this information appears to be highly feasible and generally acceptable, it is timely for practitioners to identify options for collecting and incorporating routine patient-reported health behaviours as part of their medical record.
Acknowledgments
The authors gratefully acknowledge the contribution of the study participants. Project funding provided by the Cancer Institute of New South Wales, beyondblue and the National Heart Foundation, as well as infrastructure funding from Hunter Medical Research Institute, is also gratefully acknowledged.
Funding
This work was supported by a research grant from the National Heart Foundation and beyondblue (G0189464) as well as from the Cancer Institute of New South Wales (08/RFG/1-20). The funding bodies had no involvement in the design of the study, data collection, management, analysis, interpretation of data, drafting of the report, or decision to submit the report for publication.
Ethical approval
The study was approved by the Human Research Ethics Committees of the University of Newcastle (H-2009-0341), Monash University (2009001860) and University of New South Wales (HREC09393/UN H-2009-0341).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.Prevention CfDCa . Chronic diseases and health promotion. Atlanta, GA: Centre for Disease Control and Prevention; 2009. [Google Scholar]
- 2.Australian Bureau of Statistics . Chronic Disease. 1301.0 – Year Book Australia, 2009–10. Belconnen, ACT: ABS; 2010. [Google Scholar]
- 3.National Health Priority Action Council . National chronic disease strategy. Canberra: Australian Government Department of Health and Aging; 2006. [Google Scholar]
- 4.Magarey A, McKean S, Daniels L. Evaluation of fruit and vegetable intakes of Australian adults: the National Nutrition Survey 1995. Aust N Z J Public Health. 2007;30(1):32–37. doi: 10.1111/j.1467-842x.2006.tb00083.x. [DOI] [PubMed] [Google Scholar]
- 5.Cancer Council Australia . National Cancer Prevention Policy 2007–2009. NSW: Cancer Council Australia; 2011. [Google Scholar]
- 6.Britt H, Miller G, Charles J, et al. General practice activity in Australia 2006–07. Canberra: Australian Institute of Health and Welfare; 2008. [Google Scholar]
- 7.Hippisley-Cox J, Fenty J, Heaps M. Trends in Consultation Rates in General Practice 1995 to 2006: Analysis of the QRESEARCH database. London: QResearch and The Information Centre for Health and Social Care; 2007. [Google Scholar]
- 8.Sanson-Fisher R, Webb G, Reid A. Better Health Commission (Australia) Looking forward to better health. Vol. 3. Canberra: Australian Institute of Health and Welfare; 1986. The role of the medical practitioner as an agent for disease prevention; pp. 201–212. [Google Scholar]
- 9.Brotons C, Björkelund C, Bulc M, et al. Prevention and health promotion in clinical practice: the views of general practitioners in Europe. Prev Med. 2005;40(5):595–601. doi: 10.1016/j.ypmed.2004.07.020. [DOI] [PubMed] [Google Scholar]
- 10.Heeley EL, Peiris DP, Patel AA, et al. Cardiovascular risk perception and evidence–practice gaps in Australian general practice (the AusHEART study) Med J Aust. 2010;192(5):254–259. doi: 10.5694/j.1326-5377.2010.tb03502.x. [DOI] [PubMed] [Google Scholar]
- 11.Degenhardt L, Knox S, Barker B, et al. The management of alcohol, tobacco and illicit drug use problems by general practitioners in Australia. Drug Alcohol Rev. 2005;24(6):499–506. doi: 10.1080/09595230500292938. [DOI] [PubMed] [Google Scholar]
- 12.D’Amico EJ, Paddock SM, Burnam A, et al. Identification of and guidance for problem drinking by general medical providers: results from a national survey. Med Care. 2005;43(3):229–236. doi: 10.1097/00005650-200503000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Grol R, Wensing M. What drives change? Barriers to and incentives for achieving evidence-based practice. Med J Aust. 2004;180(6):S57–S60. doi: 10.5694/j.1326-5377.2004.tb05948.x. [DOI] [PubMed] [Google Scholar]
- 14.Shojania KG, Jennings A, Mayhew A, et al. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database Syst Rev. 2009;3:CD001096. doi: 10.1002/14651858.CD001096.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dexheimer JW, Sanders DL, Rosenbloom ST, Aronsky D. Prompting clinicians: a systematic review of preventive care reminders. AMIA Annu Symp Proc. 2005;938 [PMC free article] [PubMed] [Google Scholar]
- 16.Kupets R, Covens A. Strategies for the implementation of cervical and breast cancer screening of women by primary care physicians. Gynecol Oncol. 2001;83(2):186–197. doi: 10.1006/gyno.2001.6387. [DOI] [PubMed] [Google Scholar]
- 17.Australian Institute of Health and Welfare . Heart, stroke and vascular diseases — Australian facts 2004 (Cardiovascular Diseases Series No 22) Canberra: AIHW and National Heart Foundation of Australia; 2004. [Google Scholar]
- 18.World Health Organisation . The global burden of disease: 2004 update. Geneva: WHO; 2004. [Google Scholar]
- 19.Aiello EJ, Taplin S, Reid R, et al. In a randomized controlled trial, patients preferred electronic data collection of breast cancer risk-factor information in a mammography setting. J Clin Epidemiol. 2006;59(1):77–81. doi: 10.1016/j.jclinepi.2005.07.007. [DOI] [PubMed] [Google Scholar]
- 20.Bonevski B, Sanson-Fisher R, Campbell E, et al. Randomized controlled trial of a computer strategy to increase general practitioner preventive care. Prev Med. 1999;29(6):478–486. doi: 10.1006/pmed.1999.0567. [DOI] [PubMed] [Google Scholar]
- 21.Colombet I, Dart T, Leneveut L, et al. A computer decision aid for medical prevention: a pilot qualitative study of the Personalized Estimate of Risks (EsPeR) system. BMC Med Inform Decis Mak. 2003;3(1):13. doi: 10.1186/1472-6947-3-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.De Lusignan S, Van Weel C. The use of routinely collected computer data for research in primary care: opportunities and challenges. Fam Pract. 2006;23(2):253–263. doi: 10.1093/fampra/cmi106. [DOI] [PubMed] [Google Scholar]
- 23.Ahmad F, Hogg-Johnson S, Skinner HA. Assessing patient attitudes to computerized screening in primary care: psychometric properties of the computerized lifestyle assessment scale. J Med Internet Res. 2008;10(2):e11. doi: 10.2196/jmir.955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yoong SL, Carey ML, Sanson-Fisher RW, et al. Touch screen computer health assessment in Australian general practice patients: a cross-sectional study protocol. BMJ Open. 2012;2(4):pii: e001405. doi: 10.1136/bmjopen-2012-001405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patrick DL, Cheadle A, Thompson DC, et al. The validity of self-reported smoking: a review and meta-analysis. Am J Public Health. 1994;84(7):1086–1093. doi: 10.2105/ajph.84.7.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gorber SC, Schofield-Hurwitz S, Hardt J, et al. The accuracy of self-reported smoking: a systematic review of the relationship between self-reported and cotinine-assessed smoking status. Nicotine Tob Res. 2009;11(1):12–24. doi: 10.1093/ntr/ntn010. [DOI] [PubMed] [Google Scholar]
- 27.Del Boca FK, Darkes J. The validity of self-reports of alcohol consumption: state of the science and challenges for research. Addiction. 2003;98(Suppl 2):1–12. doi: 10.1046/j.1359-6357.2003.00586.x. [DOI] [PubMed] [Google Scholar]
- 28.Prince SA, Adamo KB, Hamel ME, et al. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5(1):56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bonevski B, Campbell E, Sanson-Fisher R. The validity and reliability of an interactive computer tobacco and alcohol use survey in general practice. Addict Behav. 2010;35(5):492–498. doi: 10.1016/j.addbeh.2009.12.030. [DOI] [PubMed] [Google Scholar]
- 30.Wolfenden L, Dalton A, Bowman J, et al. Computerized assessment of surgical patients for tobacco use: accuracy and acceptability. J Public Health. 2007;29(2):183–185. doi: 10.1093/pubmed/fdm015. [DOI] [PubMed] [Google Scholar]
- 31.Rhodes KV, Lauderdale DS, Stocking CB, et al. Better health while you wait: a controlled trial of a computer-based intervention for screening and health promotion in the emergency department. Ann Emerg Med. 2001;37(3):284–291. doi: 10.1067/mem.2001.110818. [DOI] [PubMed] [Google Scholar]