Abstract
Lichen aureus (also called "lichen purpuricus") is an uncommon subtype of pigmented purpuric dermatosis. Clinically characterized by rust macules, papules or plaques, it is a chronic disease which more often affects young adults and is localized mainly on the lower extremities. The diagnosis is made on the basis of clinical and histopathological features. Dermoscopy findings are useful to confirm clinical diagnosis.
Keywords: Dermoscopy, Diagnosis, Lichenoid eruptions
Abstract
O líquen aureus (também denominado "liquen purpuricus") é um subtipo pouco comum entre as dermatoses purpúricas pigmentadas. Clinicamente caracterizado por máculas, pápulas ou placas de coloração ferruginosa, é doença crônica, que acomete mais frequentemente adultos jovens e localiza-se principalmente nos membros inferiores. O diagnóstico pode ser feito a partir das características clínicas e histopatológicas, sendo os achados dermatoscópicos úteis para corroborar o diagnóstico clínico.
INTRODUCTION
Lichen aureus (also called "lichen purpuricus") is an uncommon subtype of pigmented purpuric eruptions. 1 Clinically characterized by rust macules, papules or plaques, it is a chronic disease, which more often affects young adults and is localized mainly on the lower extremities. 2 The diagnosis is made on the basis of clinical and histopathological features. Dermoscopy findings are useful to confirm clinical diagnosis. 3
CASE REPORT
A 54-year-old woman, living in Rio de Janeiro since age 15, reported the appearance of a asymptomatic golden-brown macule on her left ankle, initially (9 months previously) measuring one centimeter and increasing in size over that period (Figure 1).
FIGURE 1.

Unilateral golden-brown macule on left ankle. Presence of purpuric dots within the lesion
Dermoscopy showed coppery-red pigmentation on background, permeated by dark brown network. In addition, linear vessels in the central portion of the lesion accompanied by punctate vessels and of peculiar circular conformation, especially in the periphery of the lesion (Figures 2 and 3).
FIGURE 2.

Dermoscopy findings. Coppery-red pigmentation on backgraund, permeated by dark brown network
FIGURE 3.

Linear vessels in the central portion of the lesion and punctate vessels, especially in the periphery of the lesion
Skin biopsy and histopathological examination showed vacuolization of the basal layer of the epidermis, lichenoid infiltrate in the dermis, extravasation of red blood cells and hemossiderin within macrophages (Figure 4).
FIGURE 4.
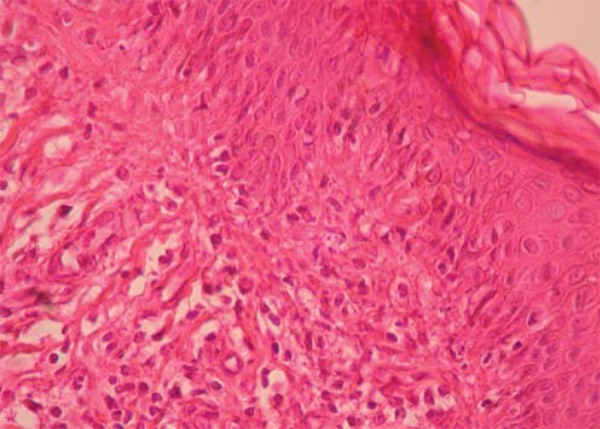
Histopathology showing vacuolization of the basal layer of epidermis, lichenoid infiltrate in the dermis and extravasation of red blood cells
Occlusive therapy with 0.05% clobetasol propionate was performed for three months, resulting in little improvement
DISCUSSION
Lichen purpuricus was first described in 1958 by Martin as a case for diagnosis.4 In 1960 Calnan reported a similar case of lichenoid pigmented lesion (lichen aureus). 1,4,5 Clinically, this dermatosis presents itself as macules, papules or plaques of varying sizes, rust or cupric coloration (golden), and sometimes may or may not show purpuric dots. 5 The lesions, in most cases, are asymptomatic, unilateral and solitary, but they may manifest in local pain and itching. 1 When multiple, they have linear arrangement with or without segmental and zosteriform distribution. 6 They are located more frequently at lower extremities, and can also affect upper extremities, hands, trunk and eyelids. 5 Differential diagnoses are other pigmented purpuric eruptions, traumatic bruises, purpura caused by drugs, contact dermatitis, mycosis fungoides and atypical forms of histiocytosis.7
Histopathology shows little or no epidermal alteration. In the dermis can be noted inflammatory typically band-like infiltrate of lymphocytes and histiocytes, extravasation of erythrocytes and hemosiderin within histiocytes. 8 The infiltrate, which in half of the cases spares the Grenz zone, tends to be denser than in other pigmented purpuric eruptions, and can be confused with that seen in early stages of mycosis fungoides.5,9,10 There are also fewer extravasated red blood cells than in other pigmented purpuric eruptions.
Dermoscopy is a non-invasive method which complements clinical examination and allows the physician directly to evaluate pigmented skin lesions. It has also been used in other areas of dermatology since there is a correlation between the morphological structures of these dermatoses and histopathological findings.
As published by Zaballos et al, describing the dermoscopy pattern of three cases of lichen aureus, the image may exhibit a diffuse copper background, with red globules, plaques and round-to-oval dots, some gray dots and a network of interconnected pigmented lines.3 The dermoscopy representation of dermal lynfohistiocytic infiltrate, together with extravasated red blood cells and hemosiderin-containing macrophages, found at histopathology, is given by the coppery background. 3,8 The dilated blood capillaries can be seen as red points, plaques and globules, with basal layer hyperpigmentation and incontinentia pigmenti represented by pigmented network lines.
Dermoscopy can be useful to support the clinical diagnosis of lichen aureus. This article contributes to describing the characteristic dermoscopic patterns of this condition, but further studies are required for them to be more precisely defined.
Footnotes
* Study conducted at Hospital Naval Marcílio Dias (HNMD) - Rio de Janeiro (RJ), Brazil.
Conflict of interest: None
Financial funding: None
REFERENCES
- 1.Cunha RR, Filho, Schwartz J, Zanol J. Líquen aureus "algesiogênico". An Bras Dermatol. 2006;81:163–165. [Google Scholar]
- 2.Schroeder-Devere T. Pigmented purpuricdermatoses. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's dermatology in general medicine. 7th. New York: McGraw-Hill; 2008. pp. 1633–1637. [Google Scholar]
- 3.Zaballos P, Puig S, Malvehy J. Dermoscopy of pigmented purpuric dermatoses (lichen aureus): a useful tool for clinical diagnosis. Arch Dermatol. 2004;140:1290–1291. doi: 10.1001/archderm.140.10.1290. [DOI] [PubMed] [Google Scholar]
- 4.Martin R. Case for diagnosis. Trans St Johns Hosp Dermatol Soc. 1958;40:93. [Google Scholar]
- 5.Nico M, Rivitti E. Líquen Áureo. An Bras Dermatol. 1996;71:47–49. [Google Scholar]
- 6.Dippel E, Schröder K, Goerdt S. Zosteriformer Lichen aureus. Hautarzt. 1998;49:135–138. doi: 10.1007/s001050050714. [DOI] [PubMed] [Google Scholar]
- 7.Rodríguez JH. Liquen aureus. Dermatol Peru. 2003;13:220–222. [Google Scholar]
- 8.Barnhill RL, Busam KJ, Nousari CH, Xu X, Barksdale SK. Vascular Diseases. In: Elder DE, Elenitsas R, Johnson BL Jr, Murphy GF, editors. Lever´s Histopathology of the Skin. 9th. Philadelphia: Lippincott Williams & Wilkins; 2005. pp. 233–237. [Google Scholar]
- 9.Price ML, Jones EW, Calnan CD, MacDonald DM. Lichen aureus: a localized persistent form of pigmented purpuric dermatitis. Br J Dermatol. 1985;112:307–314. doi: 10.1111/j.1365-2133.1985.tb04858.x. [DOI] [PubMed] [Google Scholar]
- 10.Fink-Puches R, Wolf P, Kerl H, Cerroni L. LiquenAureus. Clinicopathologic Features, Natural History, and Relationship to Mycosis Fungoides. Arch Dermatol. 2008;144:1269–1273. doi: 10.1001/archderm.144.9.1169. [DOI] [PubMed] [Google Scholar]


