Abstract
Marshall´s syndrome is a form of acquired cutis laxa without systemic involvement, which is preceded by an inflammatory dermatitis with a neutrophilic component. We report a case of a 6-year-old boy with clinical and histopathological features of this syndrome. The etiology remains unknown and there is no definitive treatment.
Keywords: Atrophy, Cutis laxa, Elastic tissue
Abstract
Síndrome de Marshall é uma forma de cutis laxa adquirida, sem envolvimento sistêmico, que é precedida por uma dermatite inflamatória com componente neutrofílico. Relatamos o caso de um menino de 6 anos de idade com as características clínicas e histopatológicas desta síndrome. A etiologia desta doença permanece desconhecida e ainda não existe um tratamento definitivo.
INTRODUCTION
Marshall´s syndrome is a rare pediatric skin disease characterized by urticarial or papular eruption followed by acute destruction of elastic tissue, resulting in skin atrophy and severe physical disfigurement. In 1966, Marshall, Heyl & Weber, from South Africa, described a disease in young children with characteristics resembling those of anetoderma and cutis laxa, which they called "postinflammatory elastolysis and cutis laxa" (PECL). The authors present the case of a child with clinical and histophatological features of this syndrome, which resulted in decreased skin elasticity and wrinkled skin.
CASE REPORT
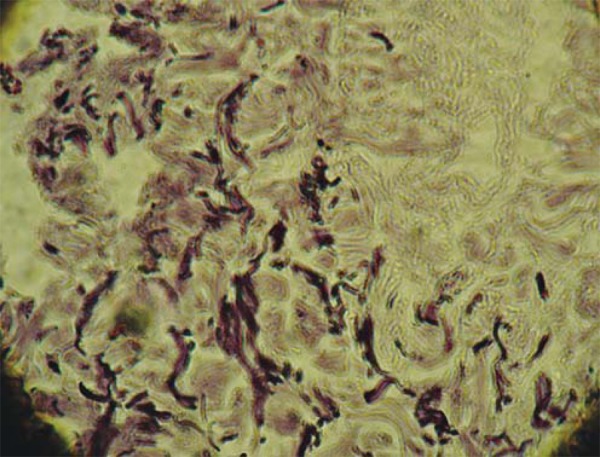
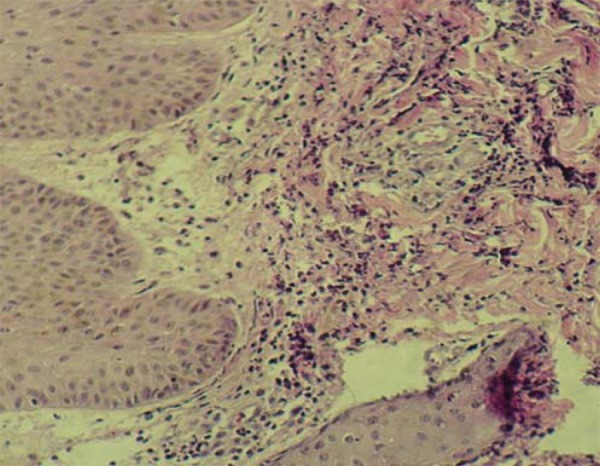
A 6-year-old boy, phototype IV, from Rio de Janeiro, Brazil, arrived at the Pediatric Dermatology Service with infiltrated, well circumscribed erythematous and edematous plaques with polycyclic configuration, on his face, back and extremities for two months, associated with episodes of fever (Figures 1 and 2). He had not taken any medication. Laboratory studies revealed normal blood count values (except for a high eosinophils rate - 7%). Serological reactions for syphilis (VDRL), HIV and baciloscopy were negative. Serum α1antitrypsin was not available. A biopsy specimen obtained from one of the infiltrated plaques showed a neutrophilic disease with edema of the dermal papillae and dense neutrophilic dermal infiltrate (Figure 3). Treatment with Dapsone (1mg/Kg/day) and Prednisone (0.5mg/Kg/day) was initiated. All inflammatory plaques resolved slowly and left atrophic, wrinkled areas, causing a premature aging appearance (Figure 4). A biopsy specimen of the atrophic cutaneous areas showed decreased thickness of the reticular dermis. Acid orcein staining showed marked decrease in the number of elastic fibers in the reticular dermis. The existing fibers were shortened and fragmented, but collagen appeared normal (Figure 5). The patient evolved with other recurrent episodes and, as a result, new wrinkled areas every time he failed to follow treatment recommendations.
FIGURE 1.

Clinic - Acute phase. Indurated well-circumscribed erythematous plaques on the back
FIGURE 2.

Acute phase: Infiltrated erythematous and edematous plaques on the face, arm and chest
FIGURE 3.

Histopathology - Acute phase. Hematoxylin-eosin 400X - Dense neutrophilic dermal infiltrate with edema of the dermal papillae
FIGURE 4.
Clinic - Chronic phase: Atrophic, wrinkled areas on the back
FIGURE 5.
Histopathology - Chronic phase. Acid orcein staining (1000 X) - with a decrease in the number of elastic fibers in the reticular dermis. The existing fibers are shortned and fragmented
DISCUSSION
Marshall´s syndrome was first described by Marshall, Heyl and Weber in 1966, in a group of five South African children who had acute erythematous, infiltrated papular eruption.1
Cutis laxa refers to a heterogenous group of diseases with the particular clinical appearance of premature aging. This disorder of elastic tissue can either be inherited or acquired. The inherited form can be autosomal dominant (which may have a delayed onset), recessive or x-linked (both are present at birth). Acquired cutis laxa is rare and can be subdivided into type I and II. Type I acquired cutis laxa can be either generalized or localized and this form may occur at any age, although with usual onset in adulthood. Most of the cases reported in the literature refer to the generalized form of type I, which usually follows episodes of inflammatory dermatosis, hypersensitivity reaction to insect bites or drugs, neoplastic disorders or in association with particular diseases. Systemic involvement is common.2,3 Type II, or Marshall's syndrome, is characterized by acute inflammatory skin lesions with subsequent development of localized areas of elastolysis. This form is also called "postinflammatory elastolysis and cutis laxa" and occurs more often in infancy or childhood.2
The pathogenesis of acquired cutis laxa remains unknown, but a number of hypotheses have been proposed. Elastic fibers are made up of two components: a microfibrillar component and an amorphous one, in which the fibrils are embedded. Elastase acts on this amorphous component, as microfibrils are susceptible to digestion by other enzymes such as trypsin and pepsin. Alteration or partial destruction of the amorphous component of the elastic tissue would affect skin tension and pulmonary compliance. Neutrophils are an important source of elastase, in addition to the pancreas. One hypothesis suggests excessive elastase activity as a result of large amounts of elastase being released by neutrophils and macrophages close to elastic fibers in some patients with localized, acquired cutis laxa.2,4 Goltz et al postulated a dysfunction in elastase inhibitors with an abnormal copper metabolism to explain the pathogenesis of the disease.5 The main elastase inhibitor is alpha 1 antitrypsin, which might prevent proteolysis of pulmonary tissue. Patients with cutis laxa and pulmonary involvement have shown low levels of this enzyme.6 Copper plays an important role in the formation of lysine polymers, which form the crosslinkage bonds that result in the structural integrity of both elastic and collagen fibers. Copper deficiencies lead to low lysyl oxidase activity and subsequent failure of the mechanism of crosslinkage and elastolysis.3,6,7 An immunomediated mechanism has been also suspected.4
Marshall´s disease starts at the age of 1-4 years, in previously healthy infants with a negative family history. The course is prolonged and is characterized by a relapsing acute inflammatory phase which lasts several months or years. Morphologically, the acute phase consists of firm, erythematous, infiltrated lesions lasting about a week or fortnight, often as rings with a collarette of scales or as diffuse plaques (or both types together). The face and neck are affected in most of the cases but other skin surfaces can also be affected. In these areas this results in decreased elasticity, laxity and usually in mild atrophy. A senile or aged facial expression is characteristic. In some cases, most of the body surface is involved.8
The diagnosis is strongly suggested clinically, but requires histopathological confirmation. The inflammatory phase shows capillary dilatation and a perivascular infiltrate composed of neutrophils and eosinophils. A dermal edema can be present. In the chronic phase, the most common finding is a marked reducti on of elastic fibers at all levels of the skin with the residual fibers being fragmented and of irregular thickness. Collagen fibers are usually normal.2,9
The main differential diagnosis of Marshall´s syndrome includes anetoderma and mid dermal elastolysis. Anetoderma is characterized by smaller lesions showing a herniation at palpation, unlike Marshall´s syndrome. Mid dermal elastolysis can be distinguished from this syndrome based on the elastolysis pattern, which is confined to the mid reticular dermis. Also, mid dermal elastolysis tends not to affect the face.10
There is no satisfactory treatment for cutis laxa. Dapsone was given to patients in the inflammatory phase and successfully controled swelling. However, it did not prevent disease progression. Plastic surgical repair seems to be the only hope for these patients in need of physical appearance improvement.2
Footnotes
* Study carried out at the Municipal Hospital Jesus (Hospital Municipal Jesus) - Rio de Janeiro (RJ), Brazil.
Conflict of interest: None
Financial funding: None
REFERENCES
- 1.Marshall J, Heyl T, Weber HW. A report on a new variety of this phenomenon and a discussion of some syndromes characterized by elastolysis. S Afr Med J. 1966;40:1016–1022. [PubMed] [Google Scholar]
- 2.Riveros CJ, Gavilán MF, França LF, Sotto MN, Takahashi MD. Acquired localized cutis laxa confined to the face: case report and review of the literature. Int J Dermatol. 2004;43:931–935. doi: 10.1111/j.1365-4632.2004.01946.x. [DOI] [PubMed] [Google Scholar]
- 3.Reed WB, Horowitz RE, Beighton P. Acquired cutis laxa: primary generalized elastolysis. Arch Dermatol. 1971;103:661–669. [PubMed] [Google Scholar]
- 4.Machet MC, Machet L, Vaillant L, Estève E, de Muret A, Arbeille A, et al. Acquired localized cutis laxa due to cutaneous lymphoplasmacytoid lymphoma. Arch Dermatol. 1995;131:110–111. [PubMed] [Google Scholar]
- 5.Machet MC, Machet L, Vaillant L, Estève E, de Muret A, Arbeille A, et al. Cutis laxa: a manifestation of generalized elastolysis. Arch Dermatol. 1965;92:373–385. doi: 10.1001/archderm.92.4.373. [DOI] [PubMed] [Google Scholar]
- 6.Lewis PG, Hood AF, Barnett NK, Holbrook KA. Post-inflammatory elastolysis and cutis laxa. J Am Acad Dermatol. 1990;22:40–48. doi: 10.1016/0190-9622(90)70005-3. [DOI] [PubMed] [Google Scholar]
- 7.Fornieri C, Quaglino D, Lungarella G, Cavarra E, Tiozzo R, Giro MG, et al. Elastin production and degradation in cutis laxa acquisita. J Invest Dermatol. 1989;93:147–153. doi: 10.1111/1523-1747.ep12396893. [DOI] [PubMed] [Google Scholar]
- 8.Verhagen AR, Woerdeman MJ. Post-inflammatory elastolysis and cutis laxa. Br J Dermatol. 1975;92:183–190. doi: 10.1111/j.1365-2133.1975.tb03056.x. [DOI] [PubMed] [Google Scholar]
- 9.Nanko H, Jepsen LV, Zachariae H, Søgaard H. Acquired cutis laxa (generalized elastolysis): light and electron microscopic studies. Acta Dermatovener. 1979;59:315–324. [PubMed] [Google Scholar]
- 10.Lewis KG, Bercovitch L, Dill SW, Robinson-Bostom L. Acquired disorders of elastic tissue: Part II. Decreased elastic tissue. J Am Acad Dermatol. 2004;51:165–185. doi: 10.1016/j.jaad.2004.03.016. [DOI] [PubMed] [Google Scholar]


