Abstract
Purpose of Review
The last five years have witnessed an explosion in interest regarding cardiac arrhythmias and air pollution. The data have been strongest with respect to ventricular arrhythmias but there is accumulating evidence that air pollution is also associated with supraventricular arrhythmias.
Recent Findings
There is clear epidemiological evidence linking air pollution and cardiac mortality. Whether the cardiac mortality was from myocardial ischemia, congestive heart failure or arrhythmic, or all of these pathways is not clear from the epidemiological data. There is a large body of evidence that air pollution can modify autonomic tone. More recent data, utilizing patients with cardiac disease and implantable cardioverter defibrillators (ICDs) has clarified the association of air pollution and arrhythmias. Data is also accumulating that air pollution may be associated with atrial arrhythmias.
Summary
The incremental risk of air pollution in triggering arrhythmias or other acute cardiac events is greatest for those patients with underlying cardiac disease. Cardiovascular patients and those at high risk of cardiovascular disease should be educated about the risks for triggering of arrhythmias and other cardiac events by air pollution. These patients should monitor the local forecasted Air Quality Index and follow the recommendations to reduce exposures and limit activities.
Keywords: Air pollution, Ventricular arrhythmias, Atrial fibrillation, Sudden cardiac death
Introduction
The acute cardiovascular effects of air pollution have been apparent since the signature air pollution events of the mid-20th century. During the London fog episode of December 1952, between 3,500 and 4,000 excess deaths, primarily for respiratory and secondarily from cardiovascular causes, were attributed to the air pollution episode.[1] In the early 1990’s, time series analyses showed that deaths, and specifically respiratory and cardiovascular deaths increased on days following even modestly elevated air pollution concentrations.[2, 3] Whether cardiovascular events were the true underlying cause of death, were the sequelae of respiratory failure, or were miscoding or cross-coding of the true underlying cause was not clear from death certificate data. Studies of daily hospital admissions records suggested specific associations of air pollution with clinical diagnoses of acute cardiac events.[4, 5] The observation that air pollution was associated with the onset of clinically confirmed myocardial infarction [6] provided the first direct evidence of a link between acute exposures to community air pollution and cardiac events. Subsequent epidemiologic and experimental studies have convincingly demonstrated a linkage between modest increases in community air pollution and the triggering acute cardiovascular events. In 2004, the American Heart Association published a Scientific Statement that concluded that “studies have demonstrated a consistent increase risk for cardiovascular events in relation to both short- and long-term exposure to present-day concentrations of ambient particulate matter”.[7]
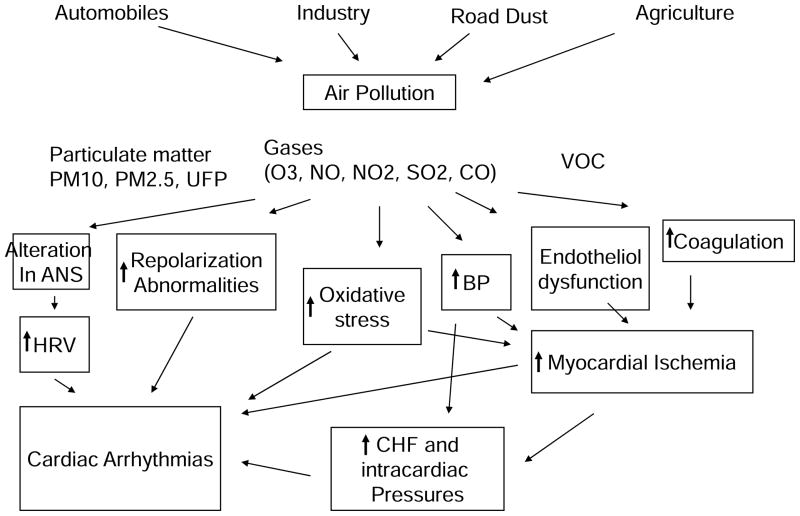
The mechanism of the increased mortality due to cardiovascular disease is not apparent, nor has it been narrowed to a specific pathway. Indeed there is evidence that air pollution may contribute to acute cardiac events through a wide range of pathways including systemic inflammation, activation of homeostatic pathways, impaired vascular function, accelerated atherosclerosis, plaque instability, altered autonomic control, and cardiac arrhythmias (Figure 1).[7] The purpose of this review is to update practicing cardiologists regarding new data associating air quality with one of these pathways, cardiac arrhythmias. The last five years have witnessed an explosion in interest regarding arrhythmias and air pollution. These data have been particularly strong in the area of ventricular arrhythmias but there is accumulating interest in effects on supraventricular arrhythmias.
Figure 1.
Potential schema for how air pollution increases the risk of cardiac arrhythmias. It is likely that there are direct effects (i.e. changes in ANS/HRV and repolarization), and indirect effects mediated via myocardial ischemia and heart failure.
Characteristics of Air Pollution
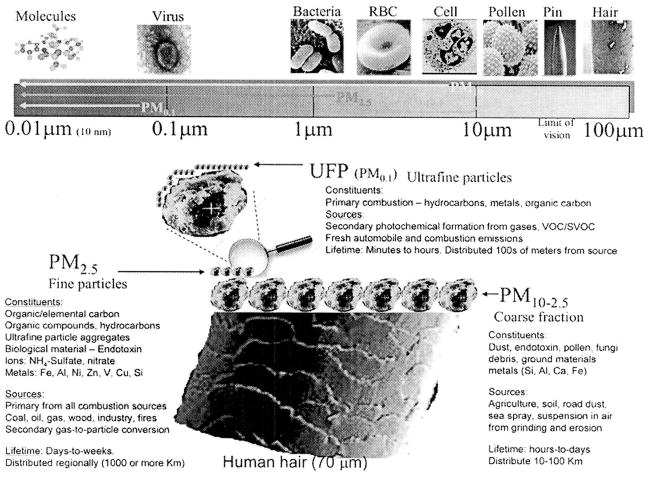
Air pollution is a mixture of several different constituents including particulate matter (PM), gases, and volatile and semi-volatile organic compounds. Particulate matter is classified by size of the particle into PM10 (≤ 10 microns in diameter), PM2.5 (≤ 2.5 microns) and ultra fine particles (UFP) (< 0.1 microns) (Figure 2). The smaller the particle the deeper the penetration into the lungs and the more likely to enter the bloodstream. PM10 reach the trachea, PM2.5 penetrate into the conducting airways and alveoli, and UFP are deposited throughout the respiratory system and even pass directly into the bloodstream. Size not only determines the sight of deposition within the lungs, but also is an indicator of the chemical composition and source of the particles.
Figure 2.
Types and sizes of air pollution. Reprinted with permission from Brook RD Cardiovascular effects of air pollution. Clinical Science (2008) 115, 175–187. [8]
Burning of fossil fuels in stationary (power plants and industry) and mobile (cars, trucks, planes, and ships) facilities accounts for the majority of pollution in developed countries. Byproducts of combustion includes the gases NO, NO2, CO, and SO2, organic and semi-volatile organic compounds, and solid and liquid particles (aerosols) including black carbon, organic carbon, and condensed metals. Volatile and semi-volatile organic compounds include benzene, toluene, xylene, and aromatic hydrocarbons. Direct emissions of particles from smokestacks and tailpipes include the UFP and PM2.5. In the atmosphere, the UFPs (the so-called nucleation mode) quickly agglomerate together and adsorb water, organics and other gases onto their surface to grow into larger particles in the PM2.5 size range (the so-called accumulation mode). Photochemical reactions in the atmosphere produce secondary pollutants including ozone (O3), and secondary fine particles such as sulfates and nitrates, which are predominantly in the PM2.5 size class. Road dust and wind-blown dust and other mechanically generated particles are sources of larger particulate matter, generally larger than PM2.5.
Long Term vs. Short Term Exposure and Mechanisms
Air pollution may contribute to cardiovascular disease by promoting the progression of coronary heart disease. For example, the rate development of atherosclerosis has been shown to be increased by long term air pollution exposure.[9–11] In addition to modifying myocardial substrate, air pollution may trigger acute cardiovascular events such as myocardial infarction, congestive heart failure or arrhythmias.[6, 12, 13] Triggering of acute cardiac events may be particularly relevant for individuals who are susceptible by nature of preexisting cardiovascular disease. Triggering of events has been shown to both occur within minutes to hours of exposures and with a lag time of hours to days.[6, 14] The potential mechanisms by which pollutants may cause acute cardiac events include alterations in autonomic function and myocardial repolarization, local and systemic inflammation, reactive oxygen species, coagulation, and myocardial ischemia.[7]
Endpoints and Methods of Air Pollution Studies
The association of air pollution and cardiovascular disease has been most extensively and convincingly demonstrated through epidemiologic studies. This epidemiologic evidence is largely based on three types of studies – time series (or case-crossover) analyses of counts of daily mortality or hospital admissions, repeated measures of panels of patients, and prospective follow-up studies of cohort of subjects. The largest body of evidence comes from analyses of daily mortality and hospital admissions. Hundreds of such analyses in the US and other countries have demonstrated a consistent association with air quality and overall mortality, cardiovascular mortality, and cardiovascular admissions.[7, 15] There is less convincing data on heart failure admissions and arrhythmias in these epidemiological approaches. Panel studies of individuals with repeated measures of clinical endpoints such as arrhythmias documented by ECGs, Holter monitors or Implanted Cardioverter Defibrillators (ICD) as well as potential markers of arrhythmic risk including changes in myocardial repolarization and altered heart rate variability (HRV), have consistently shown associations with daily measurements of air pollution in the community. Prospective follow-up studies of cohorts have assessed time to death and incidence of clinically verified cardiac events, associated with estimated measures of long-term average air pollution in the community or at the residential address of the participant.
The epidemiologic findings are supported by experimental evidence of causality and pathways. This evidence includes clinical studies of human volunteers exposed to controlled amounts of air pollution, and animal toxicology studies.
Cardiac Arrest and Myocardial Infarction
Short-term air pollution exposure has been associated with acute cardiac events, especially the triggering of myocardial infarction, in a limited number of epidemiologic studies. In a large study of over 300,000 myocardial infraction events abstracted from Medicare records in 21 U.S. cities, PM10 was associated with increased risk of MI [16]. In a study of 772 Boston area patients with confirmed myocardial infarctions [6], elevated concentrations of PM2.5 were associated with increased the risk of MI within a few hours and one day after exposure. In 5,144 out-of-hospital cardiac deaths in Rome, cardiac arrest was predicted by both particulate matter and CO on the day of death.[17] There was more of an air pollution effect for those over 65 years of age and a suggestion of a greater effect for those with hypertension and chronic pulmonary disease. In Indianapolis, witnessed cardiac arrests (n=511) were more likely with increased PM2.5 during the hour of the arrest.[18] On the other hand, a study from King County, Washington observed no association between air pollution and 1206 cardiac arrests.[19]
Cardiac Arrhythmias
A small number of studies have reported that PM exposure can trigger clinically meaningful changes in cardiac electrophysiology. Several studies have observed associations between community air pollution and cardiac arrhythmias, based on data from ICDs. These devices allow for the continuous monitoring of patients and the documentation of type and time of ventricular arrhythmias. In these studies, each patient serves as their own control, so that smaller numbers of participants are necessary. Dual-chamber ICDs also offer the opportunity to diagnose atrial arrhythmias, including atrial tachycardia and fibrillation.
The first of these ICD studies followed 100 patients in Eastern Massachusetts who had 223 ICD discharges for ventricular arrhythmias.[12] Higher levels of NO2 was associated with increased defibrillator therapy and for those patients with frequent episodes the association was also present for CO, black carbon, fine particles and was even stronger for NO. In another cohort in Eastern Massachusetts, 203 ICD patients followed for a mean of 3.1 years with 798 confirmed ventricular arrhythmias showed a linear exposure response between both PM2.5 and ozone and arrhythmias.[20] A study of 56 patients in St. Louis with 139 ventricular arrhythmias demonstrated significant increases in ventricular arrhythmias associated with increases in mean SO2 and nonsignificant increased risk with NO2 and elemental carbon in the 24 hours before the arrhythmias.[21] In a Gothenburg, Germany and Stockholm, Sweden study, 211 patients suffered 140 symptomatic ventricular arrhythmias.[22] There was an association between two-hour moving averages of PM10 and ventricular arrhythmias.
On the other hand, no clear pollution-related associations were observed in studies from Vancouver, a relatively clean metropolitan area, in a follow-up study of 50 patients with 257 ventricular arrhythmias (mean 2.3 arrhythmias/yr).[23, 24] In a large study of 518 patients and 6287 arrhythmias in Atlanta, GA there was a suggestion of effect for coarse particles (PM10 minus PM2.5), but little evidence for other air pollutants in the triggering of arrhythmias.[25]
There has been limited direct evidence for the induction of cardiac ischemia or repolarization abnormalities in the electrocardiogram associated with ambient PM concentrations in cardiac patients with repeated EKG by exposure to ambient levels of PM [26, 27]. Traffic-related combustion pollutants were most strongly related to the promotion of ST segment depression among elderly nonsmokers during exercise stress testing [28]. Moreover, very acute PM2.5 exposure within the past 1 or 4 hours has been associated with cardiac ischemia during exercise [29].New findings support these associations in elderly subjects [30]as well as in patients [31] with coronary artery disease in Boston. In the latter study, traffic-related PM was most strongly related to the incidence of ST-depression during 24 hour Holter monitoring and the risk for ischemia was greatest within the first month after a cardiac event in among patients with diabetes.
Emergency room visits for arrhythmias in Sao Paulo, Brazil were associated with air pollution in a model that evaluated not only pollutants but also different lag intervals. Arrhythmias including sinus tachycardia, atrial fibrillation and flutter, other supraventricular tachycardias, ventricular tachycardia and fibrillation were positively associated with increases in CO, NO2 and PM10.[32] The effects were acute and limited to the day of exposure. There was a threshold effect for gaseous pollutants but not for PM10.
In experimental studies, exposure to residual oil fly ash, a model of combustion particles, increased arrhythmia frequency in rats with preexisting premature ventricular complexes, suggesting that PM sensitizes ischemic myocardium to abnormal automaticity.[33] However, concentrated ambient particles (CAP) had no effect in rats.[34] Nevertheless, these experimental data suggest that PM exposure worsens myocardial ischemic sensitivity, likely by impairing myocardial perfusion, and enhances the propensity for ventricular arrhythmias.
Atrial Fibrillation
Although mechanisms may likely be similar, there is relatively scant evidence on the association of air pollution and supraventricular arrhythmias and in particular atrial fibrillation. In a sub-analysis of one of the Boston ICD studies, [20] there were 900 episodes of paroxysmal atrial fibrillation documented by the ICDs. Most of these supraventricular events were detected in single chamber devices and thus the arrhythmias documented were not of all atrial fibrillation episodes but rather a highly selected subset of rapid atrial fibrillation that caused the ICD to treat it as a ventricular arrhythmia. However, despite this limitation, there was a statistically significant association between atrial fibrillation and increased O3 in the hour before the arrhythmia. The risk estimate for a longer moving average was smaller suggesting an immediate effect and there was a positive but not statistically significant risk with fine particles, NO2, and black carbon.
Weekly 30 minute Holter for 24 weeks in 32 nonsmoking adults in Steubenville, Ohio, demonstrated an increased risk of supraventricular arrhythmias for 5-day moving averages of PM2.5, sulfate and ozone.[35] Patients with preexisting cardiac conditions such as prior myocardial infarction and hypertension were the most susceptible to pollution-induced supraventricular extrasystoles.
In a Holter study of 57 German men with coronary artery disease, elevated concentrations of particulate matter and NO2 increased the risk for supraventricular runs and ventricular runs.[36] Effects were found predominantly in the previous 24 to 72 hours air pollution and with the 5-day moving average.
Heart Rate Variability
Numerous studies have explored the associations between daily changes in air pollution exposure and measures of heart rate variability (HRV), a putative marker of cardiac autonomic function.[7, 15] Most, but not all, of these studies show a reduction in overall time domain HRV associated with air pollution. Some studies in younger patient have reported increases in HRV associated with particulate air pollution.[37, 38] Nevertheless, the general pattern suggests that PM exposure is associated with reductions in most indices of HRV (particularly among older or vulnerable individuals). Because overall HRV decreases in response to ambient PM exposure, decreased parasympathetic input to the heart may provide an important mechanistic link between air pollution and cardiovascular mortality by promoting fatal tachyarrhythmias.
In controlled exposure clinical studies, 76 young healthy students showed decreased heart rate variability indices associated with increases in levels of particulate matter, sulfate, nitrate, and ozone.[39] In 48 patients with coronary disease increases in particulate matter correlated with the risk of ST segment changes.[31] In an exposure study involving men with coronary artery disease showed in increase in ST-segment changes with diesel fumes.[40] In contrast, controlled exposure studies in young healthy individuals generally showed mixed results with most failing to show significant changes in ST segments, repolarization or heart rate variability.[37, 41] This is consistent with the observation above that young, presumably low risk individuals have reduced response to air pollution.
Individual Susceptibility
There is increasing evidence that pre-existing cardiovascular disease increases susceptibility to air pollution.[40–43] In addition, reduced defense to oxidative stress due to glutathione S-transferase M1 (GSTM1) deletion increase susceptibility.[44, 45] Diabetes and impaired glucose tolerance also likely predispose individuals to the risk of air pollution.[46] Finally current smokers [47] and individuals with COPD [43] appear more susceptible to the effects of air pollution.
Clinical Recommendations
The incremental risk of air pollution in triggering arrhythmias or other acute cardiac events is greatest for those patients with underlying cardiac disease.[8] Thus proper clinical management of cardiovascular patients and treatment of traditional cardiovascular risk factors will lessen vulnerability to air pollution. Cardiovascular patients and those at high risk of cardiovascular disease should be educated about the risks for triggering of arrhythmias and other cardiac events by air pollution. The patients should monitor the local forecasted Air Quality Index and follow the recommendations to reduce exposures and limit activities. Patients should avoid exposures to indoor air pollutants such as second hand tobacco smoke. Air conditioning and indoor air cleaning devices can have some short-term benefits, but only have been shown to have long term benefits with regular cleaning and maintenance.
Conclusion
Air pollution, a mixture of particles and gases, has been strongly associated with cardiovascular mortality. A proportion of the cardiovascular mortality is likely driven by ventricular and quite possibly supraventricular arrhythmias. Long term exposure to pollutants increases atherosclerosis and the risk of a subsequent MI. However, acute triggering of MI and arrhythmias has also been associated with increases in air pollution. It is nearly certain that pre-existing cardiovascular disease and smoking predispose individuals to adverse events with air pollution. It is also quite likely that genetic polymorphisms predispose to susceptibility.
Future studies will clarify whether air pollution contributes not only to ventricular arrhythmias and sudden death but to atrial fibrillation and the subsequent risk of stroke. These studies and data have important implications for arrhythmic health.
Acknowledgments
Supported in part by National Institute of Environmental Health Sciences grants ES-09825 and ES00002.
Abbreviations
- NO2
Nitrogen dioxide
- CO
Carbon monoxide
- SO2
Sulfur dioxide
- PM10
Particulate matter less than 10 micrometers in diameter
- PM2.5
Particulate matter less than 2.5 micrometers in diameter
- UFP
Ultra fine particles
- ICD
Implantable cardioverter defibrillator
- MI
Myocardial infarction
- HRV
Heart rate variability
References
- 1.U.K. Ministry of Health. Reports on Public Health and Medical Subjects. London: Ministry of Health; 1954. Mortality and Morbidity during the London Fog of December 1952. [Google Scholar]
- 2.Schwartz J, Dockery DW. Increased mortality in Philadelphia associated with daily air pollution concentrations. Am Rev Respir Dis. 1992;145:600–4. doi: 10.1164/ajrccm/145.3.600. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz J. What are people dying of on high air pollution days? Environ Res. 1994;64:26–35. doi: 10.1006/enrs.1994.1004. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz J, Morris R. Air pollution and hospital admissions for cardiovascular disease in Detroit, Michigan. Am J Epidemiol. 1995;142:23–35. doi: 10.1093/oxfordjournals.aje.a117541. [DOI] [PubMed] [Google Scholar]
- 5.Burnett RT, Dales R, Krewski D, et al. Associations between ambient particulate sulfate and admissions to Ontario hospitals for cardiac and respiratory diseases. Am J Epidemiol. 1995;142:15–22. doi: 10.1093/oxfordjournals.aje.a117540. [DOI] [PubMed] [Google Scholar]
- 6.Peters A, Dockery DW, Muller JE, Mittleman MA. Increased particulate air pollution and the triggering of myocardial infarction. Circulation. 2001;103:2810–5. doi: 10.1161/01.cir.103.23.2810. [DOI] [PubMed] [Google Scholar]
- 7.Brook RD, Franklin B, Cascio W, et al. Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation. 2004;109:2655–71. doi: 10.1161/01.CIR.0000128587.30041.C8. [DOI] [PubMed] [Google Scholar]
- 8.Brook RD. Cardiovascular effects of air pollution. Clinical Science. 2008;115:175–187. doi: 10.1042/CS20070444. [DOI] [PubMed] [Google Scholar]
- 9.Zanobetti A, Schwartz J. Particulate air pollution, progression, and survival after myocardial infarction. Environ Health Perspect. 2007;115:769–75. doi: 10.1289/ehp.9201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller KA, Siscovick DS, Sheppard L, et al. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med. 2007;356:447–58. doi: 10.1056/NEJMoa054409. [DOI] [PubMed] [Google Scholar]
- 11.Kunzli N, Jerrett M, Mack WJ, et al. Ambient air pollution and atherosclerosis in Los Angeles. Environ Health Perspect. 2005;113:201–6. doi: 10.1289/ehp.7523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peters A, Liu E, Verrier RL, et al. Air pollution and incidence of cardiac arrhythmia. Epidemiology. 2000;11:11–7. doi: 10.1097/00001648-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Ghio AJ, Gilbey JG, Roggli VL, et al. Diffuse alveolar damage after exposure to an oil fly ash. Am J Respir Crit Care Med. 2001;164:1514–8. doi: 10.1164/ajrccm.164.8.2102063. [DOI] [PubMed] [Google Scholar]
- 14.Zeka A, Zanobetti A, Schwartz J. Short term effects of particulate matter on cause specific mortality: effects of lags and modification by city characteristics. Occup Environ Med. 2005;62:718–25. doi: 10.1136/oem.2004.017012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pope CA, 3rd, Dockery DW. Health effects of fine particulate air pollution: lines that connect. J Air Waste Manag Assoc. 2006;56:709–42. doi: 10.1080/10473289.2006.10464485. [DOI] [PubMed] [Google Scholar]
- 16.Zanobetti A, Schwartz J. The effect of particulate air pollution on emergency admissions for myocardial infarction: a multicity case-crossover analysis. Environ Health Perspect. 2005;113:978–82. doi: 10.1289/ehp.7550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Forastiere F, Stafoggia M, Picciotto S, et al. A case-crossover analysis of out-of-hospital coronary deaths and air pollution in Rome, Italy. Am J Respir Crit Care Med. 2005;172:1549–55. doi: 10.1164/rccm.200412-1726OC. [DOI] [PubMed] [Google Scholar]
- **18.Rosenthal FS, Carney JP, Olinger ML. Out-of-hospital cardiac arrest and airborne fine particulate matter: a case-crossover analysis of emergency medical services data in Indianapolis, Indiana. Environ Health Perspect. 2008;116:631–6. doi: 10.1289/ehp.10757. Witnessed out of hospital cardiac risk was associated with PM2.5 exposure in the hour before the arrest. Unwitnessed out of hospital arrest did not correlate with exposure; however the time of the arrest is never clear in these individuals. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sullivan J, Ishikawa N, Sheppard L, et al. Exposure to ambient fine particulate matter and primary cardiac arrest among persons with and without clinically recognized heart disease. Am J Epidemiol. 2003;157:501–9. doi: 10.1093/aje/kwg015. [DOI] [PubMed] [Google Scholar]
- 20.Rich DQ, Schwartz J, Mittleman MA, et al. Association of short-term ambient air pollution concentrations and ventricular arrhythmias. Am J Epidemiol. 2005;161:1123–32. doi: 10.1093/aje/kwi143. [DOI] [PubMed] [Google Scholar]
- 21.Rich DQ, Kim MH, Turner JR, et al. Association of ventricular arrhythmias detected by implantable cardioverter defibrillator and ambient air pollutants in the St Louis, Missouri metropolitan area. Occup Environ Med. 2006;63:591–6. doi: 10.1136/oem.2005.023457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *22.Ljungman PL, Berglind N, Holmgren C, et al. Rapid effects of air pollution on ventricular arrhythmias. Eur Heart J. 2008;29:2894–901. doi: 10.1093/eurheartj/ehn463. A case crossover study of 211 patients with ICDs demonstrated an association between 2 hour moving averages of PM10, NO2 and ventricular arrhythmias. [DOI] [PubMed] [Google Scholar]
- 23.Rich KE, Petkau J, Vedal S, Brauer M. A case-crossover analysis of particulate air pollution and cardiac arrhythmia in patients with implantable cardioverter defibrillators. Inhal Toxicol. 2004;16:363–72. doi: 10.1080/08958370490439515. [DOI] [PubMed] [Google Scholar]
- 24.Vedal S, Rich K, Brauer M, et al. Air pollution and cardiac arrhythmias in patients with implantable cardioverter defibrillators. Inhal Toxicol. 2004;16:353–62. doi: 10.1080/08958370490439506. [DOI] [PubMed] [Google Scholar]
- 25.Metzger KB, Klein M, Flanders WD, et al. Ambient air pollution and cardiac arrhythmias in patients with implantable defibrillators. Epidemiology. 2007;18:585–92. doi: 10.1097/EDE.0b013e318124ff0e. [DOI] [PubMed] [Google Scholar]
- 26.Henneberger A, Zareba W, Ibald-Mulli A, et al. Repolarization changes induced by air pollution in ischemic heart disease patients. Environ Health Perspect. 2005;113:440–6. doi: 10.1289/ehp.7579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pekkanen J, Peters A, Hoek G, et al. Particulate air pollution and risk of ST-segment depression during repeated submaximal exercise tests among subjects with coronary heart disease: the Exposure and Risk Assessment for Fine and Ultrafine Particles in Ambient Air (ULTRA) study. Circulation. 2002;106:933–8. doi: 10.1161/01.cir.0000027561.41736.3c. [DOI] [PubMed] [Google Scholar]
- 28.Lanki T, de Hartog JJ, Heinrich J, et al. Can we identify sources of fine particles responsible for exercise-induced ischemia on days with elevated air pollution? The ULTRA study. Environ Health Perspect. 2006;114:655–60. doi: 10.1289/ehp.8578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lanki T, Hoek G, Timonen KL, et al. Hourly variation in fine particle exposure is associated with transiently increased risk of ST segment depression. Occup Environ Med. 2008;65:782–6. doi: 10.1136/oem.2007.037531. [DOI] [PubMed] [Google Scholar]
- 30.Gold DR, Litonjua AA, Zanobetti A, et al. Air pollution and ST-segment depression in elderly subjects. Environ Health Perspect. 2005;113:883–7. doi: 10.1289/ehp.7737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chuang KJ, Coull BA, Zanobetti A, et al. Particulate air pollution as a risk factor for ST-segment depression in patients with coronary artery disease. Circulation. 2008;118:1314–20. doi: 10.1161/CIRCULATIONAHA.108.765669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *32.Santos UP, Terra-Filho M, Lin CA, et al. Cardiac arrhythmia emergency room visits and environmental air pollution in Sao Paulo, Brazil. J Epidemiol Community Health. 2008;62:267–72. doi: 10.1136/jech.2006.058123. In a community study, both atrial and ventricular arrhythmia complaints were increased with higher levels of pollutants. However, the endpoint was a soft endpoint of arrhythmia symptoms and not documented arrhythmias. [DOI] [PubMed] [Google Scholar]
- 33.Wellenius GA, Saldiva PH, Batalha JR, et al. Electrocardiographic changes during exposure to residual oil fly ash (ROFA) particles in a rat model of myocardial infarction. Toxicol Sci. 2002;66:327–35. doi: 10.1093/toxsci/66.2.327. [DOI] [PubMed] [Google Scholar]
- 34.Wellenius GA, Batalha JR, Diaz EA, et al. Cardiac effects of carbon monoxide and ambient particles in a rat model of myocardial infarction. Toxicol Sci. 2004;80:367–76. doi: 10.1093/toxsci/kfh161. [DOI] [PubMed] [Google Scholar]
- 35.Sarnat SE, Suh HH, Coull BA, et al. Ambient particulate air pollution and cardiac arrhythmia in a panel of older adults in Steubenville, Ohio. Occup Environ Med. 2006;63:700–6. doi: 10.1136/oem.2006.027292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Berger A, Zareba W, Schneider A, et al. Runs of ventricular and supraventricular tachycardia triggered by air pollution in patients with coronary heart disease. J Occup Environ Med. 2006;48:1149–58. doi: 10.1097/01.jom.0000245921.15916.03. [DOI] [PubMed] [Google Scholar]
- *37.Peretz A, Kaufman JD, Trenga CA, et al. Effects of diesel exhaust inhalation on heart rate variability in human volunteers. Environ Res. 2008;107:178–84. doi: 10.1016/j.envres.2008.01.012. In a crossover controlled study, 16 healthy adults exposed to filtered air or two levels of diesel exhaust, there was an increase in HF power compared to FA at the higher levels of pollutants. However, the effect was small, and parameters exhibited no changes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Riediker M, Cascio WE, Griggs TR, et al. Particulate matter exposure in cars is associated with cardiovascular effects in healthy young men. Am J Respir Crit Care Med. 2004;169:934–40. doi: 10.1164/rccm.200310-1463OC. [DOI] [PubMed] [Google Scholar]
- 39.Chuang KJ, Chan CC, Su TC, et al. The effect of urban air pollution on inflammation, oxidative stress, coagulation, and autonomic dysfunction in young adults. Am J Respir Crit Care Med. 2007;176:370–6. doi: 10.1164/rccm.200611-1627OC. [DOI] [PubMed] [Google Scholar]
- 40.Mills NL, Tornqvist H, Gonzalez MC, et al. Ischemic and thrombotic effects of dilute diesel-exhaust inhalation in men with coronary heart disease. N Engl J Med. 2007;357:1075–82. doi: 10.1056/NEJMoa066314. [DOI] [PubMed] [Google Scholar]
- *41.Zareba W, Couderc JP, Oberdorster G, et al. ECG parameters and exposure to carbon ultrafine particles in young healthy subjects. Inhal Toxicol. 2009;21:223–33. doi: 10.1080/08958370802492407. In a crossover design of 12 subjects exposed to air polluted with carbon ultrafine particles there were trends indicating an increase in parasympathetic tone. However the study was small and underpowered. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chen JC, Stone PH, Verrier RL, et al. Personal coronary risk profiles modify autonomic nervous system responses to air pollution. J Occup Environ Med. 2006;48:1133–42. doi: 10.1097/01.jom.0000245675.85924.7e. [DOI] [PubMed] [Google Scholar]
- 43.Wheeler A, Zanobetti A, Gold DR, et al. The relationship between ambient air pollution and heart rate variability differs for individuals with heart and pulmonary disease. Environ Health Perspect. 2006;114:560–6. doi: 10.1289/ehp.8337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chahine T, Baccarelli A, Litonjua A, et al. Particulate air pollution, oxidative stress genes, and heart rate variability in an elderly cohort. Environ Health Perspect. 2007;115:1617–22. doi: 10.1289/ehp.10318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Weinhold B. One-two PM punch: gene combination increases vulnerability to air pollutant. Environ Health Perspect. 2007;115:A551. doi: 10.1289/ehp.115-a551b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *46.Whitsel EA, Quibrera PM, Christ SL, et al. Heart rate variability, ambient particulate matter air pollution, and glucose homeostasis: the environmental epidemiology of arrhythmogenesis in the women’s health initiative. Am J Epidemiol. 2009;169:693–703. doi: 10.1093/aje/kwn400. In the Women’s Health Initiative PM 10 exposure was inversely associated with heart rate variability. particularly in those with diabetes or prediabetes. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **47.Liao D, Whitsel EA, Duan Y, et al. Ambient particulate air pollution and ectopy--the environmental epidemiology of arrhythmogenesis in Women’s Health Initiative Study, 1999–2004. J Toxicol Environ Health A. 2009;72:30–8. doi: 10.1080/15287390802445483. In a large scale US study of women, PM2.5 and PM10 were associated with ventricular ectopy in current smokers, but not in nonsmokers suggesting that smokers are uniquely susceptable to air pollution. [DOI] [PMC free article] [PubMed] [Google Scholar]