Abstract
Objective
This study examined the effects of age at injury on the persistence of behavior problems and social skill deficits in young children with complicated mild to severe traumatic brain injury (TBI).
Method
A concurrent cohort/prospective research design was used with repeated assessments of children with TBI (n = 82) or Orthopedic Injury (OI) (n = 114). Parents completed the Child Behavior Checklist, the Behavior Rating Inventory of Executive Functions, and the Preschool and Kindergarten Behavior Scales or the Home and Community Social and Behavior Scales shortly after injury to assess preinjury functioning, and at an extended follow-up an average of 38 months postinjury. Generalized linear modeling was used to examine the relationship of age at injury to the maintenance of behavior problems, and logistic regression was used to examine the persistence of clinically significant behavior problems.
Results
At the extended follow-up, severe TBI was associated with significantly greater anxiety problems relative to the Group OI. With increasing time since injury, children who sustained a severe TBI at an earlier age had significantly higher levels of parent-reported symptoms of ADHD and anxiety than children who were older at injury.
Conclusions
Findings suggest that longer-term treatment for behavior problems may be needed after severe TBI, particularly for those injured at an earlier age.
Keywords: traumatic brain injury, long-term behavior problems, young children
Introduction
Children who sustain a traumatic brain injury (TBI) commonly exhibit long-term behavior difficulties that are among the most troubling consequences of brain injury (Schwartz et al., 2003; Taylor et al., 2002; Chapman et al., 2010; Andrews, Rose, & Johnson, 1998; Ganesalingam, Sanson, Anderson, & Yeates, 2006; Ganesalingam, Sanson, Anderson, & Yeates, 2007; Catroppa, Anderson, Morse, Haitou, & Rosenfeld, 2008; Yeates et al., 2010). A series of recent studies demonstrated that behavior is adversely affected after TBI in young children, with symptoms failing to resolve at long-term follow-ups conducted one year or more postinjury. Persisting symptoms included those related to Attention Deficit/ Hyperactivity Disorder (ADHD), externalizing behavior problems, executive dysfunction (Chapman et al., 2010), and social competence deficits (Yeates et al., 2010). Catroppa and colleagues (2008) also examined functional outcomes in young, preschool aged children 5 years postinjury and found deficits in adaptive functioning, behavior, and academic achievement. Additionally, all of these studies found a relationship between long-term problems and injury severity, with significantly greater behavior problems among those with severe injury.
These findings are consistent with investigations of school-age children and adolescents that have reported elevated rates of both internalizing (e.g., Bloom et al., 2001; Max et al., 1998c; Wade, Michaud, & Brown, 2006) and externalizing behavior problems (Bloom et al., 2001; Max et al., 1998d; Schwartz et al., 2003) after TBI. Childhood TBI has also been linked to elevated rates of clinical syndromes, including ADHD (Wassenberg, Max, Lind-gren, & Schatz, 2004; Bloom et al., 2001; Max et al., 1998a; Max et al., 2005), oppositional defiant disorder (ODD; Max et al., 1998a; Max et al., 1998b; Max et al., 1998c; Bloom et al., 2001), and anxiety disorders (Max et al., 1998c; Levi, Drotar, Yeates, & Taylor, 1999; Wade, Michaud, & Brown, 2006; Grados et al., 2008; Vasa et al., 2002). However, research with school-age children suggests that internalizing problems are more likely to resolve over time than externalizing problems (Bloom et al., 2001). Because the current body of research has focused predominantly on school-age children and adolescents, research examining the long-term development and maintenance of behavior problems among young children with TBI is needed (Catroppa et al., 2008; Chapman et al., 2010; Yeates et al., 2010).
Early childhood is theorized to be a time of increased vulnerability to the long-term effects of neurological insult (Taylor & Alden, 1997; Ewing-Cobbs, Prasad, Landry, Kramer, & DeLeon, 2004). Specifically, injuries occurring during early childhood have been purported to compromise subsequent development to a greater extent than later insults (Taylor & Alden, 1997). Examining the role of age at injury with regard to symptoms of anxiety one year postinjury, Vasa and colleagues (2002) found that among children with severe TBI, younger age at injury was positively correlated with postinjury anxiety symptoms, particularly obsessive–compulsive behavior, separation anxiety, and simple phobias. However, the bulk of the research to date that has examined the effect of age at injury on TBI sequelae has largely focused on neurocognitive and academic outcomes rather than behavior outcomes in school-age children. These studies indicate that children who are younger at the time of injury (less than 7–8 years old) exhibit worse long-term neurocognitive and academic outcomes and less recovery relative to children injured at older ages (Anderson & Moore, 1995; Verger et al., 2000; Anderson, Catroppa, Morse, Haritou, & Rosenfeld, 2000) with the effect of age more salient among those with severe injury (Anderson, Catroppa, Morse, Haritou, & Rosenfeld, 2000). Anderson and Moore (1995) found that IQ scores for younger children (less than 7 years of age at injury) remained stable during the initial two years postinjury, whereas those of older children increased significantly, suggesting less recovery in intellectual functioning after early injury. Younger age at injury has also been associated with less recovery in a variety of specific abilities, including attention (Ewing-Cobbs et al., 1998; Anderson et al., 2010), perceptual motor skills (Ewing-Cobbs et al., 1998), visuospatial abilities (Verger et al., 2000; Anderson et al., 2010), language, memory (Anderson et al., 2010), processing speed (Anderson et al., 2010; Anderson, Catroppa, Godfrey, & Rosenfeld, 2012), and executive functions (Anderson et al., 2010; Slomine et al., 2002).
However, not all studies have found poorer outcomes among children injured at an earlier age. Ewing-Cobbs and colleagues (1997) found that age at injury was unrelated to neuropsychological test performance when comparing children who were ages 4 to 41 months at the time of injury with those who were ages 42 to 72 months at the time of injury. Similarly, Yeates and colleagues (2002) found that age at injury did not moderate group differences on a range of neuropsychological measures including short-term memory (STM), verbal fluency, intelligence, and motor integration. The single exception was performance on the Contingency Naming Task, on which children who were younger at the time of injury (less than 7 years) exhibited more pronounced deficits 12 months postinjury than older children. In the same cohort of children injured between the ages of 6 and 12 years, Taylor and colleagues (2002) found no evidence for moderating effects of age at injury on behavior deficits and long-term academic ability.
Because of these inconsistent findings, it is unclear whether the association between earlier age at injury and poorer neurocognitive outcomes is limited to children with severe TBI. Some studies have found that younger children have poorer outcomes regardless of their injury severity (Anderson & Moore, 1995; Verger et al., 2000), whereas others found a relationship between intellectual outcomes and age at injury only among those with severe TBI. For example, Anderson and colleagues (2000) found that children with severe injury who were between the ages of 3 and 7 years exhibited less recovery from baseline to 12 months postinjury than did children with severe injury who were 8–12 years of age at the time of injury, whereas similar effects of age at injury were not observed among those with mild to moderate TBI (Anderson, Catroppa, Morse, Haritou, & Rosenfeld, 2000).
Although research indicates that TBI is associated with long-term behavior problems among school-age children, few studies have comprehensively described the long-term behavioral functioning of children injured at an early age. Research investigating the relation of age of injury to the persistence of behavior problems is also lacking. The aim of the current investigation was to fill this gap in knowledge by investigating associations of age at injury to long-term behavior problems in children injured in early childhood. We hypothesized that severe TBI would be associated with higher levels of behavior problems and higher rates of clinically significant problems at the extended follow-up and that both more severe TBI and younger age at injury would be associated with more persistent attention problems, anxiety, and externalizing behavior problems.
Method
Participants
A concurrent cohort/prospective research design was used with repeated assessments of children aged 3–7 years with TBI or OI requiring hospitalization. An OI comparison group was recruited to control for the experience of hospitalization and preexisting factors that might make the child vulnerable to injury. Participants were recruited from three children's hospitals and one general hospital. Parents completed retrospective ratings of children's preinjury behavior problems, executive function behaviors, and social competence at a baseline assessment conducted shortly after injury (mean number of days = 39.92; SD = 19.57). Relevant demographic information was also collected at the baseline assessment. At an extended follow-up a minimum of 24 months postinjury (mean number of month = 38.34; SD = 10.29), 68 parents of children with TBI (19 severe, 49 complicated mild to moderate) and 75 with children who sustained an orthopedic injury (OI) again completed the measures of child behavior, executive function, and social competence. Of the 196 families who completed the baseline assessment, 143 (72%) participated in the extended follow-up. Those who completed the follow-up were younger at the time of injury and significantly more likely to have sustained a TBI versus OI (p < .05). Analysis failed to reveal any other significant differences in baseline characteristics between participants and nonparticipants (all ps ≥ .44 for the nonsignificant variables).
The sample was divided into three groups: severe TBI, complicated mild to moderate TBI, and OI. Inclusionary criteria included having sustained the injury between 36 and 83 months of age, no evidence of child abuse as the cause of the injury, no history of documented neurological problems or developmental delays preinjury, and English as the primary language in the home. To be eligible, all children had to be hospitalized for at least one night. Among those with TBI, additional eligibility criteria included an alteration of neurological functioning as measured by a Glasgow Coma Scale (GCS) score less than 13 or evidence of trauma-related abnormality as seen on MRI or computerized tomography. Children in the severe TBI group had a GCS score less than or equal to 8 as the lowest postresuscitation score; those in the complicated mild to moderate TBI group had either a GCS score of 9–12 or a GCS score of 13–15 accompanied by evidence of abnormality on imaging. The OI group included children who sustained a bone fracture, other than to the skull, and had no alterations in consciousness or other symptoms of head trauma.
Procedure
The study was approved by the Institutional Review Boards at each study site, and informed consent was obtained from the parent or legal guardian once the child was known to be in stable medical condition. Medical charts were reviewed for relevant information. At the baseline and extended follow-up assessments, parents completed questionnaires regarding the child's behavior and social competence that are described below.
Demographic Measures
Relevant demographic and injury-related information was collected at the baseline study visit. Family income was estimated using the census tract median income for the zip code of the participant's primary residence. A composite measure of socioeconomic status (SES) was constructed by averaging z scores for primary caregiver education and median census tract income.
Parent-Report Measures
The Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2000, 2001) is a parent rating of child behavior problems that is widely used in both clinical and research settings. Per the CBCL manual, parents with children younger than the age of 6 years received the CBCL 1[1/2]–5 version and those with children 6 years or older received the CBCL 6–18 version. For the current study, scores for internalizing behaviors and externalizing behaviors subscales were used, along with the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM–IV)–oriented Anxiety and Attention Deficits/ Hyperactivity clinical subscales. The CBCL has high test–retest reliability and criterion validity (Achenbach & Rescorla, 2000, 2001) and is sensitive to behavior problems after TBI (Taylor et al., 2002; Schwartz et al., 2003). DSM-oriented clinical scales were examined because of their correspondence to clinical diagnoses. For example, the DSM-Oriented Anxiety scale has a greater degree of correspondence with clinical diagnoses than the Anxious/ Depressed Syndrome scale (Ebesutani et al., 2009). For the CBCL Anxiety and Attention Deficits/ Hyperactivity DSM-oriented clinical scales, t scores are truncated at 50, resulting in a restricted range of scores. In an effort to alleviate this problem, raw scores were used in all analyses except when calculating the proportion of participants who met criteria for clinically elevated behavior problems. Consistent with prior investigations of pediatric TBI, a t score greater than or equal to 63 was used as a clinical cutoff for significant behavior problems (Schwartz et al., 2003; Chapman et al., 2010).
The Preschool and Kindergarten Behavior Scales–Second Edition (PKBS–2; Merrell, 2002) and the Home and Community Social and Behavior Scales (HCSBS; Merrell & Caldarella, 2002) were used to assess social competence. The PKBS and HCSBS are similar in structure and content but are normed for younger (ages 3 to 6 years) and older (ages 5 to 18 years) children, respectively. For the purposes of this study, parents of children younger than 6 years of age completed the PKBS and those with children ages 6 or older completed the HCSBS. Both measures have demonstrated satisfactory reliability and validity (Lund & Merrell, 2001; Merrell, 1996; Merrell & Boelter, 2001; Merrell, Streeter, & Boelter, 2001). For this study, we used the social competence composite from each measure to obtain a single measure of this dimension. The two sets of z scores demonstrated substantial correlations across time, supporting the assumption that they provide equivalent measures of social competence. A clinical cutoff of z = 1.5 was used to indicate clinically significant deficits in social competence.
Parents also completed the Behavior Rating Inventory of Executive Function (BRIEF; Gioia, Isquith, Guy, & Kenworthy, 2000), a rating of the child's executive functioning abilities. Parents of children ages 3 to 5 years old were administered the preschool version (Gioia, Espy, & Isquith, 2000), and parents of children ages 6 and older were administered the school-age version (Gioia, Isquith, Guy, & Kenworthy, 2000). This measure has demonstrated high levels of internal consistency and stability and acceptable levels of both interrater and test–retest reliability (Gioia, Espy, & Isquith, 2000; Gioia, Isquith, Guy, & Kenworthy, 2000). The General Executive Composite (GEC), or total score, was used as a broad measure of executive ability. Clinically significant deficits in executive function behaviors were defined as t scores ≥63 (Chapman et al., 2010).
Statistical Analyses
Means, standard deviations, and simple correlations were used to summarize the overall distribution of the data and to describe bivariate relationships among the variables in the study. General linear mixed model analysis was used to examine the persistence of behavior problems over time as a function of injury severity, time since injury, and age at injury. The initial model included all interactions involving injury group, time since injury, and age at injury; covariates included retrospective ratings of preinjury behavior functioning completed by the parents at the baseline assessment, child's race (White vs. non-White), sex (male or female), and SES. To illustrate significant interactions, we reported the estimated values for the dependent variables at one standard deviation above or below the mean age at injury and mean time since injury. To make the models more parsimonious, manual backward elimination was used where initial models were trimmed by eliminating nonsignificant higher-level interactions, starting with three-way interactions, and then reestimating the model before eliminating lower level interactions and main effects. Use of this method is consistent with previous research (e.g., Yeates et al., 2010; Taylor et al., 2002; Yeates et al., 2002; Yeates et al., 2004; McCoy, McMillen, & Spitznagel, 2008; van der Heijden, Donders, Stijen, & Moons, 2006). Backwards manual elimination of nonsignificant factors can also be justified as a means to increase the numerical stability and generalizability of results (Hegewald, Pfahlberg, & Uter, 2003). We used logistic regression to test the relationship between time since injury, age at injury, and TBI severity on the likelihood of exhibiting clinically significant levels of behavior problems, controlling for the same covariates included in mixed model analysis. In reporting the results of continuous and logistic regression, we retained age at injury and time since injury in all models, even if statistically nonsignificant, because these factors were central to the aims of the study. Additionally, we retained child's gender as this information is relevant for interpretations and comparisons on the CBCL clinical scales. We also determined the proportion of participants by injury group that met criteria for clinically significant behavior problems at the extended follow-up.
Results
Participants
Means and standard deviations for baseline data for those who completed the extended follow-up can be found in Table 1. Included for descriptive purposes in Table 1 is the family census tract median income and primary caregiver education; however, the composite SES measure was used in subsequent analyses.
Table 1.
Demographic Information at Baseline Assessment
| OI | Complicated mild to moderate TBI | Severe TBI | |
|---|---|---|---|
| n | 117 | 63 | 23 |
| Lowest GCS | N/A | 13.45 (1.98) | 3.83 (1.69) |
| Age at injury, Mean (SD) | 5.11 (1.07) | 5.04 (1.19) | 4.95 (1.00) |
| Child's race (% white) | 75.6 | 66.2 | 69.6 |
| Child's gender (% male) | 58.0 | 56.9 | 69.6 |
| Primary caregiver education n (% of sample) | 53 (45.4%) High school or GED or less, 64 (54.7%) Some college or more | 34 (54.0%) High school or GED or less, 29 (46.0%) Some college or more | 16 (69.6%) High school or GED or less, 7 (30.4%) Some college or more |
| Days from injury to baseline visit, Mean (SD)a,b | 35.18 (15.01) | 46.00 (23.02) | 47.35 (23.50) |
| Time since injury at extended follow-up in months, Mean (SD)b | 41.11 (9.32) | 34.78 (10.25) | 37.48 (11.25) |
| Median census tract incomea | $63,924 ($23,582) | $58,111 ($26,762) | $54,308 ($15,823) |
Note. GCS = Glasgow Coma Scale; OI = orthopedic injury; TBI = traumatic brain injury.
Significant difference (p > .05) between OI and severe TBI.
Significant difference (p > .05) between OI and complicated mild to moderate TBI.
Demographic comparisons of the injury groups revealed no significant differences in primary caregiver education or the child's sex, race, or age at injury (p > .05). 42% of the severe group, 14% of the complicated mild to moderate group, and 10% of the OI group reported receiving psychopharmacological interventions at the extended follow-up (χ2 (2, n = 141) = 12.20, p = .002). The majority of the reported medications (approximately 68%) were used to address symptoms related to ADHD. Group differences were found in the number of days from injury to the baseline visit, with the OI group having a shorter time from injury to visit than either the severe or mild to moderate TBI group. Additionally, the OI group had a significantly longer time since injury to the extended visit relative to the complicated mild to moderate TBI group, and the OI group had a significantly greater median income than the severe TBI group (see Table 1).
Simple correlation coefficients among baseline variables ranged from 0.003 between the Internalizing Behaviors subscale and age at injury to 0.79 for both the Externalizing Behaviors subscale and the BRIEF GEC and the ADHD subscale and the BRIEF GEC. The CBCL Externalizing and ADHD subscales were also highly correlated (r = .71). We examined and failed to find evidence of multicollinearity among the predictor variables. The combined family income and maternal education variables were moderately correlated with the behavioral measures, with correlations ranging from −0.23 on the Anxiety subscale to −0.42 on the Externalizing subscale. Examination of the distributions revealed skewness values that ranged from −.97 for PKBS/HCSBC to 1.55 for the CBCL Anxiety subscale. Kurtosis values ranged from −.04 for PKBS/ HCSBS to 2.67 for the CBCL ADHD subscale.
Longitudinal Analysis of Behavior Outcomes
Means and standard deviations for the behavior measures at the baseline and extended follow-up are presented in Table 2. Results from mixed model analysis revealed significant main effects for group for Externalizing, t = 2.90, p = .004, the BRIEF GEC, t = 2.43, p = .01, and Internalizing, t = 2.58, p = .01. Simple effects tests indicated that the severe TBI group was elevated relative to the OI and complicated mild to moderate TBI group on all three measures. Interactions of group × time since injury × age at injury for were found for both the CBCL ADHD scale, t =−2.22, p = .02, and CBCL Anxiety scale, t =−2.16, p = .03 with moderate corresponding effect sizes (partial η2 = .04 for the ADHD scale and partial η2 = .05 for the Anxiety scale). For both measures, ratings were higher for the severe TBI than for the other two groups, but only for children with younger age at injury at a longer time since injury. The latter findings are illustrated in Figures 1 and 2, with estimates based on raw scores that were 1 SD above and below the sample mean. Group comparisons failed to reveal significant differences on ratings of social competence.
Table 2.
Means and Standard Deviations for Behavioral Measures
| Outcome | Assessment | OI group | Complicated mild/moderate TBI group | Severe TBI group |
|---|---|---|---|---|
| Externalizing | Baseline | T = 48.99 (10.54) | T = 50.80 (10.86) | T = 50.89 (12.39) |
| Extended | T = 53.19 (6.90) | T = 55.12 (7.81) | T = 59.68 (10.88) | |
| ADHD | Baseline | T = 55.36 (8.13) | T = 53.61 (5.81) | T = 53.36 (6.74) |
| Raw = 4.14 (3.46) | Raw = 4.70 (3.60) | Raw = 5.79 (4.89) | ||
| Extended | T = 48.89 (11.23) | T = 50.63 (12.37) | T = 58.32 (13.30) | |
| Raw = 6.08 (7.73) | Raw = 6.96 (7.75) | Raw = 13.95 (12.77) | ||
| BRIEF GEC | Baseline | T = 48.53 (11.61) | T = 50.02 (14.04) | T = 53.68 (15.46) |
| Extended | T = 49.03 (11.73) | T = 52.24 (14.92) | T = 59.63 (14.20) | |
| Internalizing | Baseline | T = 48.74 (8.61) | T = 49.80 (10.11) | T = 50.95 (14.72) |
| Extended | T = 53.97 (6.90) | T = 54.55 (8.10) | T = 60.00 (9.33) | |
| Anxiety | Baseline | T = 53.47 (5.74) | T = 53.97 (6.60) | T = 53.89 (4.95) |
| Raw = 2.89 (2.66) | Raw = 3.35 (3.05) | Raw = 3.74 (4.26) | ||
| Extended | T = 54.35 (7.31) | T = 55.47 (8.04) | T = 62.47 (13.38) | |
| Raw = 4.49 (5.54) | Raw = 5.12 (6.04) | Raw = 10.47 (9.50) | ||
| PKBS/HCSBC | Baseline | 0.36 (0.90) | 0.32 (0.87) | −0.38 (1.24) |
| Extended | 0.37 (0.88) | 0.13 (1.08) | −0.52 (1.19) |
Note. The baseline assessment was conducted a mean of 40 days postinjury and extended follow-up a mean of 38 months postinjury. For the CBCL clinical scales (ADHD and Anxiety), raw scores were used in analyses because of the restricted range of the T-scores. OI = orthopedic injury; TBI = traumatic brain injury; ADHD = Attention Deficit/ Hyperactivity Disorder; BRIEF GEC = Behavior Rating Inventory of Executive Function General Executive Composite; PKBS/HCSBC = Social competence as assessed by the Preschool and Kindergarten Behavior Scales–Second Edition/Home in children < 6 years and Community Social and Behavior Scales in children ≥ 6 years.
Figure 1.
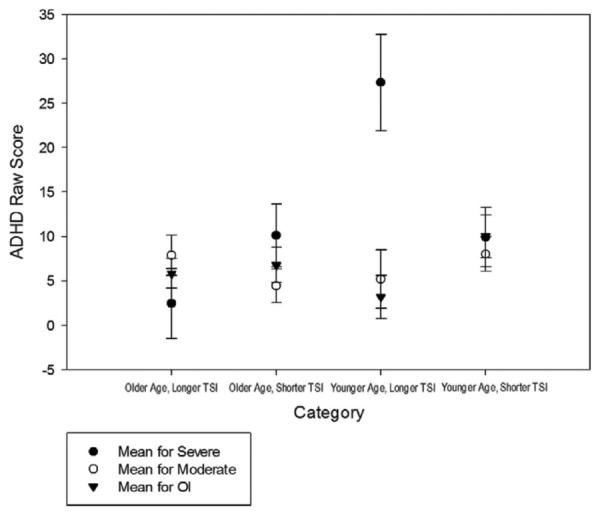
Estimated values of CBCL ADHD subscale raw scores one standard deviation above and below (±1 SD) the sample mean. Older age = 1 SD above the sample mean age; younger age = 1 SD below the sample mean age; longer TSI = 1 SD above the sample mean time since injury; shorter TSI = 1 SD below the sample mean time since injury.
Figure 2.
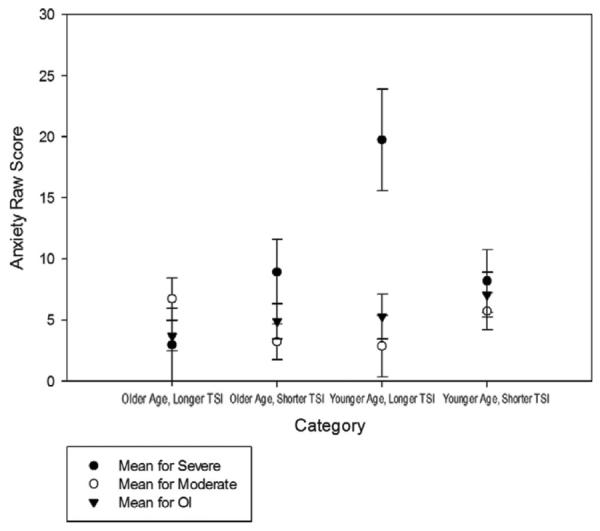
Estimated values of CBCL Anxiety subscale raw score one standard deviation above and below (±1 SD) the sample mean. Older age = 1 SD above the sample mean age; younger age = 1 SD below the sample mean age; longer TSI = 1 SD above the sample mean time since injury; shorter TSI = 1 SD below the sample mean time since injury.
Rates of Clinically Elevated Behavior Ratings at Extended Follow-Up
Rates of clinical elevations in behavior ratings were consistently higher in the severe TBI group than in the other two groups. For the severe TBI group, complicated mild to moderate TBI group, and OI group, respectively, 36.8%, 18.4%, and 11.0% had elevations on Externalizing; 42.1%, 18.4%, and 16.2% on the CBCL ADHD subscale; 42.1%, 26.5%, and 14.7% on BRIEF GEC; 36.8%, 12.2%, and 12.3% on Internalizing; and 26.3%, 10.2%, and 10.8% on Anxiety. However, only the group difference on the Anxiety subscale was significant controlling for SES, race, and baseline behavior ratings (see Table 3). Results as illustrated in Figure 3 indicated that the severe TBI group had a significantly higher rate of score elevations relative to the OI group but not relative to the mild to moderate TBI group. The baseline (preinjury) rating was the most consistent predictor of clinical elevations across all of the rating scales.
Table 3.
Results From Logistic Regression Indicating Predictors of Persistent Clinically-significant Elevations at the Extended Follow-Up
| Outcome | Predictor | Adjusted odds ratio (95% confidence interval) | p |
|---|---|---|---|
| Externalizing | Pre-morbid behavior | 1.13 (1.06–1.21) | <.0001 |
| Age at injury | 1.00 (.58–1.73) | .97 | |
| Time since injury | .49 (.21–1.13) | .09 | |
| Gender | 1.71 (.45–6.42) | .42 | |
| Injury group | 2.98 (.58–15.23) | .06 | |
| ADHD | Pre-morbid behavior | 1.27 (1.10–1.47) | .0007 |
| Age at injury | .83 (.51–1.34) | .45 | |
| Time since injury | 1.00 (.52–1.91) | .98 | |
| Gender | 2.13 (.63–7.12) | .21 | |
| Injury group | 2.27 (.51–10.08) | .24 | |
| GEC | Pre-morbid behavior | 1.08 (1.04–1.13) | .0001 |
| Age at injury | 1.19 (.74–1.90) | .45 | |
| Time since injury | 1.29 (.69–2.38) | .41 | |
| Gender | 1.78 (.60–5.26) | .29 | |
| Injury group | 2.71 (.66–10.99) | .15 | |
| Internalizing | Pre-morbid behavior | 1.12 (1.04–1.20) | .008 |
| Age at injury | .93 (.55–1.56) | .78 | |
| Time since injury | .68 (33–1.42) | .30 | |
| Gender | 1.78 (.49–6.45) | .37 | |
| Injury group | .46 (.06–3.20) | .56 | |
| Anxiety | Pre-morbid behavior | 1.35 (1.14–1.60) | .0004 |
| Age at injury | .86 (.52–1.42) | .57 | |
| Time since injury | .95 (.50–1.81) | .89 | |
| Gender | 1.36 (.44–4.22) | .59 | |
| Injury group | 3.98 (.94–16.73) | .02 | |
| PKBS/HCSBS | Pre-morbid behavior | 13.07 (.97–175.35) | .05 |
| Age at injury | 1.41 (.60–3.29) | .41 | |
| Time since injury | .72 (.21–2.39) | .59 | |
| Gender | .29 (.04–1.81) | .18 | |
| Injury group | 9.47 (.50–179.16) | .21 |
Note. ADHD = Attention Deficit/Hyperactivity Disorder; GEC = General Executive Composite; PKBS/HCSBC = Social competence as assessed by the Preschool and Kindergarten Behavior Scales–Second Edition/Home in children < 6 years and Community Social and Behavior Scales in children ≥ 6 years.
Figure 3.
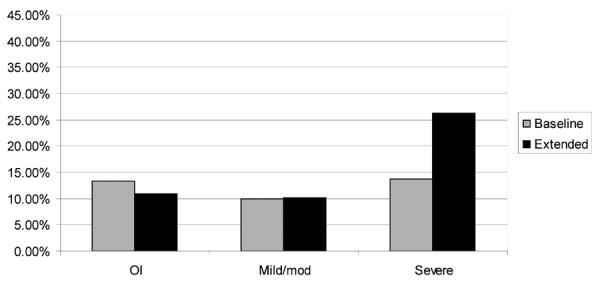
Proportion of participants in each group meeting criteria for clinically significant behavior problems on the CBCL Anxiety subscale at baseline and extended follow-up. Clinical significance defined as t score ≥ 63.
Discussion
The current study examined the moderating effects of injury severity, age at injury, and time since injury on the persistence of behavior problems, social problems, and executive functioning deficits in a large cohort of young children with TBI more than 2 years postinjury. Consistent with our hypothesis, age at injury, in conjunction with time since injury and injury severity, moderated long-term behavior outcomes on the CBCL ADHD and Anxiety subscales. Specifically, with increasing time since injury, children who sustained a severe TBI at an earlier age reported significantly higher levels of symptoms than children who were older at injury. Age at injury did not moderate other behavior outcomes including social competence, executive dysfunction, overall internalizing symptoms, or overall externalizing symptoms. As anticipated, children with severe TBI had significantly higher levels of internalizing and externalizing behavior problems as well as higher levels of executive dysfunction.
Our primary study hypothesis was that age at injury would moderate the persistence of behavior problems on the CBCL ADHD, Anxiety, and Externalizing Behaviors subscales, such that children who were younger at injury were expected to evidence greater behavior problems at the extended follow-up. The results partially supported these predictions. Consistent with our hypothesis, a triple interaction among injury group, time since injury, and age at injury was found for both ADHD and anxiety symptoms on the CBCL. The interactions revealed higher levels of persistent symptoms among children who were younger at the time of injury.
Past research suggests that a relationship exists between ADHD and anxiety disorders, with rates of comorbidity reportedly as high as 25% (Schatz & Rostain, 2006). Symptoms of ADHD and anxiety may be related to long-term neurocognitive deficits in the domains of attention and executive functioning that are more prominent among children who are younger at the time of injury (Ewing-Cobbs et al., 1998; Anderson et al., 2010; Slomine et al., 2002). Deficits in these domains have been suggested to contribute to decreased behavior regulation and attentional capabilities (Barkley, 1997) and decreased ability to regulate emotional reactions (e.g., Baum et al., 2010; Morgan & Lilenfeld, 2000), which in turn may affect behavioral functioning. The correlations reported in the current study suggest a substantial amount of shared variance among the Externalizing Behaviors subscale, the ADHD subscale, and the GEC.
We also hypothesized that severe TBI would be associated with clinically significant levels of behavior problems at the extended follow-up. Although the severe TBI had higher rates of clinically elevated behavior ratings, groups differences were significant only on the Anxiety scale in analyses controlling for background factors and preinjury ratings. Previous research reported that social deficits are common postinjury (e.g., Janusz, Kirkwood, Yeates, & Taylor, 2002; Warschausky, Cohen, Parker, Levendosky, & Okun, 1997), suggesting that our measures were insensitive to social skills deficits in childhood TBI or that these deficits are less evident in younger children.
Overall, this study adds to previous research demonstrating effects of school-age TBI on long-term behavior problems (Schwartz et al., 2003; Bloom et al., 2001; Ganesalingam, Sancon, Anderson, & Yeates, 2006; Ganesalingam, Sancon, Anderson, & Yeates, 2007; Taylor et al., 2002). Specifically, the findings confirm past findings of internalizing and externalizing problems (Bloom et al., 2001; Max et al., 1998c, 1998d; Schwartz et al., 2003; Wade, Michaud, & Brown, 2006) and elevated rates of clinical symptomology, including ADHD (Wassenberg, Max, Lindgren, & Schatz, 2004; Bloom et al., 2001; Max et al., 1998a; Max et al., 2005) and anxiety disorders (Max et al., 1998c; Levi, Drotar, Yeates, & Taylor, 1999; Wade, Michaud, & Brown, 2006; Grados et al., 2008; Vasa et al., 2002). These findings confirm previous reports indicating that behavior problems and symptoms of clinical disorders are worse among children with severe TBI (Catroppa et al., 2008; Taylor et al., 2002; Schwartz et al., 2003). The results are also in accord with previous reports of persistent behavior problems in the severe TBI group (Chapman et al., 2010; Yeates et al., 2010). The current study extends these findings by demonstrating that behavior problems continue to be present at a further follow-up conducted an average of 38 months postinjury.
These findings are contrary to prior research that failed to reveal associations of age at injury with injury severity (Anderson & Moore, 1995; Verger et al., 2000) and are instead compatible with other studies that have examined the role of age at injury with regard to long-term neurocognitive outcomes, showing that children who are younger and sustained severe injury often experience greater long-term deficits (Anderson, Catroppa, Morse, Haritou, & Rosenfeld, 2000; Ewing-Cobbs et al., 1998). The current study extends these findings by demonstrating that behavior problems, specifically ADHD symptoms and anxiety, may also be related to age at injury and injury severity, so that children who are younger and sustain a severe injury exhibit higher levels of symptoms over time.
The primary limitation of the current study is the reliance on retrospective parent ratings of premorbid behavior functioning. Because parents rated premorbid symptoms after the injury occurred, they may have been biased by the child's current behavior problems. Also of consideration, controlling for baseline behavior may have limited our ability to detect long-term behavior deficits as parent ratings of behavior problems may have been elevated at baseline. The use of the CBCL also has limitations. The two versions of the CBCL that are used in this age range are not identical. Of relevance to the current study, the content of the Anxiety scales differs between versions, as anxiety is thought to manifest differently in school-age and preschool-age children (Achenbach & Rescorla, 2000, 2001). At the extended follow-up, eight participants received the preschool version of the CBCL (three OI, five complicated mild to moderate, and no Severe). To examine the possibility that findings differed for the two versions of the CBCL scale, the continuous and logistic regression models were rerun with version considered as an additional factor. No significant differences were found between the models with and without version type as a factor. The current study also included a relatively small number of children with severe TBI, which may have limited our ability to describe the behavior functioning of this subgroup. The small overall sample size at the extended follow-up may also explain the failure to find group differences in clinically elevated behavior problems. The confidence interval for the CBCL Anxiety scale was especially large relative to that of the other behavioral measures. Additionally, simple correlations among the behavioral measures revealed a high degree of shared variance among the behavioral measures, specifically, the BRIEF GEC, CBCL ADHD, and CBCL Externalizing; however, among these measures, significant findings were only found for the CBCL ADHD scale. While these findings suggest that long-term symptoms of ADHD and Anxiety may be uniquely affected by age at injury and injury severity, the current results will need to be replicated with larger samples and broader ranges of age at injury. A further limitation is attrition at the extended follow-up, with higher attrition within the OI group and among older participants; this bias for participants who were younger at the time of injury may be especially germane the current study that sought to examine the role of age at injury. Finally, future investigations may need to use structured diagnostic interviews, observational measures, or teacher report measures to obtain more in-depth information about behavior functioning across settings and contexts.
The current study is among the first of which we are aware to examine the effect of age at injury on the maintenance of behavior problems at least two years post-TBI in a sample of young children. The use of a comparison group of children that sustained an orthopedic injury also allowed meaningful conclusions to be made about the specific effects of head injury relative to other types of traumatic injury. Another strength of the current study is the comprehensiveness of the behavior domains assessed, including externalizing and internalizing behavior problems, DSM–IV–oriented symptoms of clinical disorders, social competence deficits, and problems related to executive functioning.
The current results suggest that care after an early TBI must continue long-term, as behavioral effects often persist with the passage of time. Given that severe TBI is associated with greater behavior problems several years postinjury, health care providers need to closely monitor these issues and diligently refer patients to appropriate services as necessary. The results further suggest that children who are younger at the time of injury are at increased risk for greater long-term behavior problems, specifically for symptoms of ADHD and anxiety. Future studies examining the nature of long-term behavior problems and issues that exacerbate these problems will be helpful for clinicians who deliver postinjury rehabilitation services and develop interventions for those with TBI.
Impact and Implications
The current study adds to the literature by describing the long-term behavior sequelae of traumatic brain injury (TBI) (average of 38 months postinjury) in young children while also addressing the role of age at injury. Although age at injury has been examined in relation to neurocognitive sequelae after TBI, less is known about age-at-injury effects on long-term behavior outcomes.
For clinical practice, the findings suggest that longer-term treatment may be necessary after TBI in young children. More specifically, children who are younger at injury may be particularly at risk for the development of symptoms of ADHD and anxiety, and thus may be benefit from greater postinjury intervention.
The current study offers valuable information regarding children who may benefit the most from postinjury interventions. An understanding of the nature of long-term behavior problems and issues that exacerbate these problems, such as time since injury and age at injury, is relevant for clinicians who provide postinjury rehabilitation services and seek to develop interventions.
Acknowledgments
We acknowledge the contributions of Christine Abraham, Andrea Beebe, Lori Bernard, Anne Birnbaum, Beth Bishop, Tammy Matecun, Karen Oberjohn, Elizabeth Roth, and Elizabeth Shaver in data collection. The Cincinnati Children's Medical Center Trauma Registry, Rainbow Pediatric Trauma Center, Rainbow Babies & Children's Hospital, Nationwide Children's Hospital Trauma Program, and MetroHealth Center Department of Pediatrics and Trauma Registry provided assistance with recruitment. The research reported here was supported by grant R01 HD42729 from National Institute of Child Health and Human Development (NICHD), in part by United States Public Health Service National Institutes of Health (NIH) grant M01 RR 08084, and by Trauma Research grants from the State of Ohio Emergency Medical Services, all to Dr. Shari L. Wade. The project described was also supported by the National Center for Research Resources and the National Center for Advancing Translational Sciences, NIH, through grant 8 UL1 TR000077-04. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. Dr. Keith O. Yeates received support from career development grant K02 HD44099 from NICHD.
References
- Achenbach TM, Rescorla LA. Manual for ASEBA preschool forms & profiles. University of Vermont, Research Center for Children, Youth, & Families; Burlington, VT: 2000. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for ASEBA school-aged forms & profiles. University of Vermont, Research Center for Children, Youth, & Families; Burlington, VT: 2001. [Google Scholar]
- Anderson V, Catroppa C, Godfrey C, Rosenfeld G. Intellectual ability 10 years after traumatic brain injury in infancy and childhood: What predicts outcomes? Journal of Neurotrauma. 2012;29:143–153. doi: 10.1089/neu.2011.2012. doi:10.1089/neu.2011.2012. [DOI] [PubMed] [Google Scholar]
- Anderson V, Catroppa C, Morse S, Haritou F, Rosenfeld J. Recovery of intellectual ability following Traumatic Brain Injury in childhood: Impact of injury severity and age at injury. Pediatric Neurosurgery. 2000;32:282–290. doi: 10.1159/000028956. doi:10.1159/000028956. [DOI] [PubMed] [Google Scholar]
- Anderson V, Jacobs R, Spencer-Smith M, Coleman L, Anderson P, Williams J, Leventer R. Does early age at brain insult predict worse outcome? Neuropsychological implications. Journal of Pediatric Psychology. 2010;35:716–727. doi: 10.1093/jpepsy/jsp100. doi:10.1093/jpepsy/jsp100. [DOI] [PubMed] [Google Scholar]
- Anderson V, Moore C. Age at injury as a predictor of outcome following pediatric head injury: A longitudinal perspective. Child Neuropsychology. 1995;1:187–202. doi:10.1080/09297049508400224. [Google Scholar]
- Andrews TK, Rose FD, Johnson DA. Social and behavioural effects of traumatic brain injury in children. Brain Injury. 1998;12:133–138. doi: 10.1080/026990598122755. doi:10.1080/026990598122755. [DOI] [PubMed] [Google Scholar]
- Barkley RA. Behavioral inhibition, sustained attention, and executive functions: Constructing a unifying theory of ADHD. Psychological Bulletin. 1997;121:65–94. doi: 10.1037/0033-2909.121.1.65. doi:10.1037/0033-2909.121.1.65. [DOI] [PubMed] [Google Scholar]
- Baum KT, Byers AW, deGrauw TJ, Dunn DW, Bates JE, Howe SR, Austin JK. The effect of temperament and neuropsychological functioning on behavior problems in children with new-onset seizures. Epilepsy & Behavior. 2010;17:467–473. doi: 10.1016/j.yebeh.2010.01.010. doi:10.1016/j.yebeh.2010.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bloom DR, Levin HS, Ewing-Cobbs L, Saunders AE, Song J, Fletcher JM, Kowatch RA. Lifetime and novel psychiatric disorders after pediatric traumatic brain injury. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:572–579. doi: 10.1097/00004583-200105000-00017. doi:10.1097/00004583-200105000-00017. [DOI] [PubMed] [Google Scholar]
- Catroppa C, Anderson VA, Morse SA, Haitou F, Rosenfeld JV. Outcome and predictors of functional recovery 5 years following pediatric traumatic brain injury (TBI) Journal of Pediatric Psychology. 2008;33:707–708. doi: 10.1093/jpepsy/jsn006. doi:10.1093/jpepsy/jsn006. [DOI] [PubMed] [Google Scholar]
- Chapman LA, Wade SL, Walz NC, Taylor HG, Stancin T, Yeates KO. Clinically significant behavior problems during the initial 18 months following early childhood Traumatic Brain Injury. Rehabilitation Psychology. 2010;55:48–57. doi: 10.1037/a0018418. doi:10.1037/a0018418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ebesutani C, Bernstein A, Nakamura BJ, Chorpita BF, Higa-McMillan CK, Weisz JR. Concurrent validity of the child behavior checklist DSM-oriented scales: Correspondence with DSM diagnoses and comparison to syndrome scales. Journal of Psychopathology and Behavioral Assessment. 2010;32:373–384. doi: 10.1007/s10862-009-9174-9. doi:10.1007/s10862-009-9174-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing-Cobbs L, Fletcher JM, Levin HS, Francis DJ, Davidson K, Miner ME. Longitudinal neuropsychological outcome in infants and preschoolers with traumatic brain injury. Journal of the International Neuropsychological Society. 1997;3:581–591. [PubMed] [Google Scholar]
- Ewing-Cobbs L, Prasad M, Fletcher JM, Levin HS, Miner ME, Eisenberg HW. Attention after pediatric traumatic brain injury: A multidimensional assessment. Child Neuropsychology. 1998;4:35–48. doi:10.1076/chin.4.1.35.3194. [Google Scholar]
- Ewing-Cobbs L, Prasad MR, Landry SH, Kramer L, DeLeon R. Executive functions following traumatic brain injury in young children: A preliminary analysis. Developmental Neuropsychology. 2004;26:487–512. doi: 10.1207/s15326942dn2601_7. doi:10.1207/s15326942dn2601_7. [DOI] [PubMed] [Google Scholar]
- Ganesalingam K, Sancon A, Anderson V, Yeates KO. Self regulation as a mediator of the effects of childhood traumatic brain injury on social and behavioral functioning. Journal of the International Neuropsychological Society. 2007;13:298–311. doi: 10.1017/S1355617707070324. doi:10.1017/S1355617707070324. [DOI] [PubMed] [Google Scholar]
- Ganesalingam K, Sanson A, Anderson V, Yeates KO. Self-regulation and social and behavioral functioning following childhood Traumatic Brain Injury. Journal of the International Neuropsychological Society. 2006;12:609–621. doi: 10.1017/S1355617706060796. doi:10.1017/S1355617706060796. [DOI] [PubMed] [Google Scholar]
- Gioia GA, Espy KA, Isquith PK. Behavior rating inventory of executive function—preschool version. Psychological Assessment Resources; Lutz, FL: 2000. [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior rating inventory of executive function. Psychological Assessment Resources; Odessa, FL: 2000. [Google Scholar]
- Grados MA, Vasa RA, Riddle MA, Slomine BS, Salorio C, Christensen J, Gerring J. New onset obsessive-compulsive symptoms in children and adolescents with severe traumatic brain injury. Depression and Anxiety. 2008;25:398–407. doi: 10.1002/da.20398. doi:10.1002/da.20398. [DOI] [PubMed] [Google Scholar]
- Hegewald J, Pfahlberg A, Uter W. A backwards-manual selection macro for binary logistic regression in the SAS v. 8.02 PROC LOGISTIC procedure. Paper presented at the Proceedings of the North East SAS Users Group; Washington, D. C.. Sep, 2003. [Google Scholar]
- Janusz JA, Kirkwood MW, Yeates KO, Taylor HG. Social problem-solving skills in children with traumatic brain injury: Long-term outcomes and prediction of social competence. Child Neuropsychology. 2002;8:179–194. doi: 10.1076/chin.8.3.179.13499. doi:10.1076/chin.8.3.179.13499. [DOI] [PubMed] [Google Scholar]
- Levi RB, Drotar D, Yeates KO, Taylor HG. Posttraumatic stress symptoms in children following orthopedic or traumatic brain injury. Journal of Clinical Child Psychology. 1999;28:232–243. doi: 10.1207/s15374424jccp2802_10. doi:10.1207/s15374424jccp2802_10. [DOI] [PubMed] [Google Scholar]
- Lund J, Merrell KW. Social and antisocial behavior of children with learning and behavioral disorders: Construct validity of the Home and Community Social Behavior Scales. Journal of Psychoeducational Assessment. 2001;19:112–122. doi:10.1177/073428290101900201. [Google Scholar]
- Max JE, Arndt S, Castillo CS, Bokura H, Robin DA, Lindgren SD, Mattheis PJ. Attention-deficit hyperactivity symptomology after traumatic brain injury: A prospective study. Journal of the American Academy of Child & Adolescent Psychiatry. 1998a;37:841–847. doi: 10.1097/00004583-199808000-00014. doi:10.1097/00004583-199808000-00014. [DOI] [PubMed] [Google Scholar]
- Max JE, et al. Oppositional defiant disorder symptomology after traumatic brain injury: A prospective study. Journal of Nervous and Mental Disease. 1998b;186:325–332. doi: 10.1097/00005053-199806000-00001. doi:10.1097/00005053-199806000-00001. [DOI] [PubMed] [Google Scholar]
- Max JE, et al. Posttraumatic stress symptomology after childhood traumatic brain injury. Journal of Nervous and Mental Disease. 1998c;186:589–596. doi: 10.1097/00005053-199810000-00001. doi:10.1097/00005053-199810000-00001. [DOI] [PubMed] [Google Scholar]
- Max JE, et al. Psychiatric disorders in children and adolescents after severe traumatic brain injury: A controlled study. Journal of the American Academy of Child & Adolescent Psychiatry. 1998d;37:832–840. doi: 10.1097/00004583-199808000-00013. doi:10.1097/00004583-199808000-00013. [DOI] [PubMed] [Google Scholar]
- Max JE, et al. Predictors of secondary attention deficits/ hyperactivity disorder in children and adolescents 6 to 24 months after traumatic brain injury. Journal of the American Academy of Child & Adolescent Psychiatry. 2005;44:1041–1049. doi: 10.1097/01.chi.0000173292.05817.f8. doi:10.1097/01.chi.0000173292.05817.f8. [DOI] [PubMed] [Google Scholar]
- McCoy H, McMillen C, Spitznagel EL. Older youth leaving the foster care system: Who, what, when, where, and why? Children and Youth Services Review. 2008;30:735–745. doi: 10.1016/j.childyouth.2007.12.003. doi:10.1016/j.childyouth.2007.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrell KW, Boelter E. An investigation of the relationships between social behavior and ADHD in children and youth: Construct validity of the Home and Community Behavior Scales. Journal of Emotional and Behavioral Disorders. 2001;9:260–269. doi:10.1177/106342660100900406. [Google Scholar]
- Merrell KW, Caldarella P. Home & community social behavior scales. Assessment Intervention Resources; Eugene, OR: 2002. [Google Scholar]
- Merrell KW, Streeter AL, Boelter EW. Validity of the home and community social behavior scales: Comparisons with five behavior-rating scales. Psychology in the Schools. 2001;38:313–325. doi:10.1002/pits.1021. [Google Scholar]
- Merrell KW. Social-emotional assessment in early childhood: The preschool and kindergarten behavior scales. Journal of Early Intervention. 1996;20:132–145. doi:10.1177/105381519602000205. [Google Scholar]
- Merrell KW. Preschool and kindergarten behavior scales. 2nd ed. PRO-ED; Austin, TX: 2002. [Google Scholar]
- Morgan AB, Lilenfeld SO. A meta-analysis of the relation between antisocial behavior and neuropsychological measures of executive function. Clinical Psychology Review. 2000;20:113–156. doi: 10.1016/s0272-7358(98)00096-8. doi:10.1016/S0272-7358(98)00096-8. [DOI] [PubMed] [Google Scholar]
- Schatz DB, Rostain AL. ADHD with comorbid anxiety: A review of the current literature. Journal of Attention Disorders. 2006;10:141–149. doi: 10.1177/1087054706286698. doi:10.1177/1087054706286698. [DOI] [PubMed] [Google Scholar]
- Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, Stancin T. Long-term behavior problems following pediatric traumatic brain injury: Prevalence, predictors, and correlates. Journal of Pediatric Psychology. 2003;28:251–263. doi: 10.1093/jpepsy/jsg013. doi:10.1093/jpepsy/jsg013. [DOI] [PubMed] [Google Scholar]
- Slomine BS, Gerring JP, Grados MA, Vasa R, Brady KD, Christensen JR, Denckla MB. Performance on measures of `executive functions' following pediatric traumatic brain injury. Brain Injury. 2002;16:759–772. doi: 10.1080/02699050210127286. doi:10.1080/02699050210127286. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Alden J. Age-related differences in outcomes following childhood brain insults: An introduction and overview. Journal of the International Neuropsychological Society. 1997;3:555–567. [PubMed] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. doi:10.1037/0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- van der Heijden GJ, Donders AR, Stijen T, Moons K. Imputation of missing values is superior to complete case analysis and the missing-indicator method in multivariable diagnostic research: A clinical example. Journal of Clinical Epidemiology. 2006;59:1102–1109. doi: 10.1016/j.jclinepi.2006.01.015. doi:10.1016/j.jclinepi.2006.01.015. [DOI] [PubMed] [Google Scholar]
- Vasa RA, Gerring JP, Grados M, Slomine B, Christensen JR, Rising W, Riddle MA. Anxiety after severe pediatric closed head injury. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:148–156. doi: 10.1097/00004583-200202000-00008. doi:10.1097/00004583-200202000-00008. [DOI] [PubMed] [Google Scholar]
- Verger K, Junque C, Jurado MA, Tresserras P, Bartumeus F, Nogues P, Poch JM. Age effects on long-term neuropsychological outcomes in paediatric traumatic brain injury. Brain Injury. 2000;14:495–503. doi: 10.1080/026990500120411. doi:10.1080/026990500120411. [DOI] [PubMed] [Google Scholar]
- Wade SL, Michaud L, Brown TM. Putting the pieces together: Preliminary efficacy of a family problem-solving intervention for children with traumatic brain injury. The Journal of Head Trauma Rehabilitation. 2006;21:57–67. doi: 10.1097/00001199-200601000-00006. doi:10.1097/00001199-200601000-00006. [DOI] [PubMed] [Google Scholar]
- Warschausky S, Cohen EH, Parker JG, Levendosky AA, Okun A. Social problem-solving skills of children with traumatic brain injury. Pediatric Rehabilitation. 1997;1:77–81. doi: 10.3109/17518429709025850. doi:10.3109/17518429709025850. [DOI] [PubMed] [Google Scholar]
- Wassenberg R, Max JE, Lindgren SD, Schatz A. Sustained attention in children and adolescents after traumatic brain injury: Relation to severity of injury, adaptive functioning, ADHD and social background. Brain Injury. 2004;18:751–764. doi: 10.1080/02699050410001671775. doi:10.1080/02699050410001671775. [DOI] [PubMed] [Google Scholar]
- Yeates KO, Swift E, Taylor HG, Wade SL, Drotar D, Stancin T, Minich N. Short- and long-term social outcomes following pediatric traumatic brain injury. Journal of the International Neuropsychological Society. 2004;10:412–426. doi: 10.1017/S1355617704103093. [DOI] [PubMed] [Google Scholar]
- Yeates KO, Taylor HG, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term neuropsychological outcomes after traumatic brain injury in children. Neuropsychology. 2002;16:514–523. doi: 10.1037//0894-4105.16.4.514. doi:10.1037/0894-4105.16.4.514. [DOI] [PubMed] [Google Scholar]
- Yeates KO, Taylor HG, Walz NC, Stancin T, Wade SL. The family environment as a moderator of psychosocial outcomes following traumatic brain injury in young children. Neuropsychology. 2010;24:345–356. doi: 10.1037/a0018387. doi:10.1037/a0018387. [DOI] [PMC free article] [PubMed] [Google Scholar]


