Abstract
Helicobacter pylori-infected subjects exhibited a strong decline in antral secretory leukocyte protease inhibitor (SLPI) levels compared to H. pylori-negative subjects and subjects from whom H. pylori had been eradicated (P = 0.002). This reduction was specific for the antrum, whereas SLPI expression in corpus and duodenum was not affected. Antral SLPI levels were inversely correlated with inflammatory scores of antrum-predominant gastritis.
Helicobacter pylori infection has been linked to the development of a variety of gastroduodenal diseases, including gastroduodenal ulcers, gastric adenocarcinoma, and mucosa-associated lymphatic tissue lymphoma (8). The central process responsible for the initiation of the H. pylori-mediated inflammation is the interaction between the bacterium and the gastric epithelial surface (10, 12). The interaction between H. pylori and epithelial cells leads subsequently to inflammation and cellular damage. In this context, protease inhibitors play an important role in controlling the activity of proteases that are released at sites of necrosis or apoptosis. Secretory leukocyte protease inhibitor (SLPI) is a serine protease inhibitor that has multiple biological activities. It possesses inhibitory activity toward several serine proteases (13). Furthermore, it has bactericidal and antifungal activity (7) and is involved in the regulation of cell proliferation (19). In vivo, SLPI was shown to be involved in destructive pulmonary diseases (6) or wound healing (1). Taking into account the presence of SLPI in the intestine (2, 15) and its role in inflammatory processes, we studied gastroduodenal SLPI expression in the context of H. pylori infection in healthy volunteers.
For analyzing SLPI expression in the context of H. pylori infection, 20 healthy volunteers (14 males and 6 females; 31 ± 7 years old; H. pylori positive, n = 10; H. pylori negative, n = 10) were included after giving written informed consent. After eradication therapy, 9 of 10 initial H. pylori-positive subjects agreed to participate in this study again after 3 months (H. pylori-eradicated group, n = 9). During upper gastrointestinal-endoscopy, multiple biopsies from antrum, corpus, and duodenal bulb were obtained. H. pylori status was determined by three standard methods—histology, 13C urea breath test, and rapid urease test—as described previously (5, 9, 11). Subjects were regarded as H. pylori negative (or positive) if all three tests were either negative or positive. SLPI expression was studied by quantitative reverse transcription-PCR (RT-PCR), enzyme-linked immunosorbent assay, and immunohistochemistry. RNA extraction, RT, and quantitative RT-PCR were performed as described previously (18) by using the following primers: SLPI (5′-GAGATGGATGGCCAGTGCAAGC-3′ and 5′-GCTGTGTGCCAAGCCTTTCCC-3′) and β-actin (5′-CATGCCATCCTGCGTCTGGACC-3′ and 5′-ACATGGTGGTGCCGCCAGACAG-3′). Total protein lysate was extracted by standard methods, and SLPI was determined by using the SLPI kit (R&D Systems, Minneapolis, Minn.). Immunohistochemical studies were performed with a polyclonal anti-SLPI rabbit antiserum and the Vectastain ABC-AP kit (Vector, Burlingame, Calif.). Data were analyzed with paired and unpaired t tests (two-sided) or one-way analysis of variance. The correlation was analyzed by using a Spearman's nonparametric test.
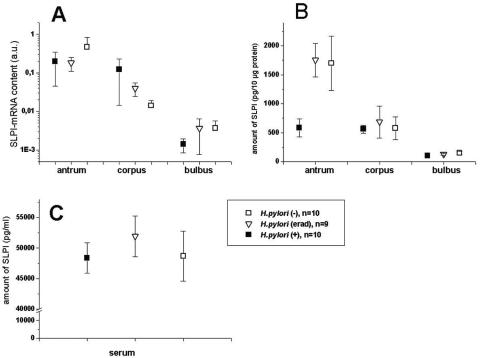
As shown in Fig. 1, SLPI expression differed with respect to location. Antral biopsies contained about three times more SLPI than samples from the corpus, which had higher SLPI levels than duodenal mucosa (Fig. 1B). In general, the amounts of SLPI protein were accompanied by corresponding levels of the SLPI transcript (Fig. 1A), suggesting that the location-dependent variations are either due to (i) transcriptional regulation or (ii) cellular distribution of SLPI-expressing cells in the stomach. Since it is known that the antral mucosa contains the largest proportion of the deep foveolar glands, the cellular distribution of SLPI-expressing cells is likely to be the primary cause for the location-dependent differences.
FIG. 1.
Detection of SLPI in gastric biopsies. All values are shown as means and standard deviation. (A) SLPI mRNA content of the biopsies. (B) Amount of SLPI protein in the total lysate of gastric biopsies. The antra of H. pylori-positive individuals contained significantly less SLPI than that in H. pylori-negative (P = 0.03) and H. pylori-eradicated (erad) probands (P = 0.002). (C) Levels of SLPI in serum.
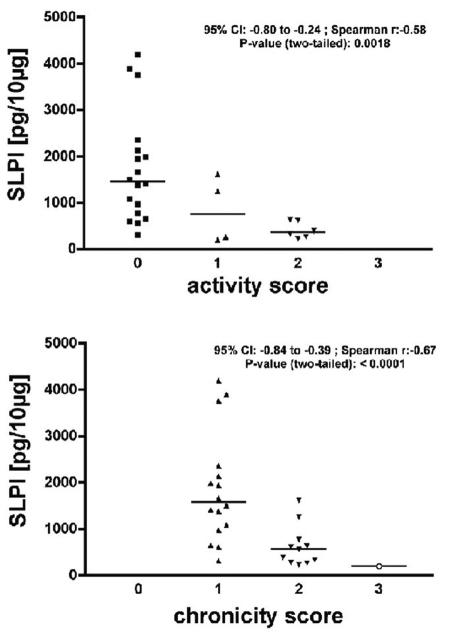
In addition, significantly decreased SLPI levels were found in antral mucosa of H. pylori-positive subjects (Fig. 1B). Levels of SLPI in the corpus, duodenal bulb, and serum (Fig. 1C) of these subjects were not changed, implying that the SLPI downregulation in the antrum is a local phenomenon. The decline of SLPI in the antrum was found to be inversely correlated to the degree of inflammation (Fig. 2). Since SLPI downregulation was completely reversed after eradication (Fig. 1B), H. pylori and/or the associated gastritis could be the primary cause for this observation. The inverse correlation between the rate of inflammation and mucosal SLPI level in the antrum are in line with the local nature of type B gastritis in European countries (3). H. pylori infection has two major pathophysiological pathways: (i) an antrum-predominant gastritis with a hypersecreting phenotype leading to duodenal ulcers and (ii) a corpus-predominant or pan-gastritis, resulting in hyposecretion, atrophy, and subsequent development of gastric tumors (8). In this context, it is notable that all of our H. pylori-infected probands exhibited an antrum-predominant gastritis, suggesting that the downregulation of antral SLPI levels is linked to the hypersecreting pathway. Since this study comprised healthy asymptomatic H. pylori-infected probands, we cannot conclude about SLPI levels in patients with corpus-predominant or pan-gastritis. Additional studies are necessary to investigate whether SLPI downregulation is a rather general phenomenon of mucosal inflammation or specific for the antrum-predominant gastritis caused by H. pylori.
FIG. 2.
Correlation between antral SLPI contents and inflammatory scores. The severity of inflammation was graded according to the updated Sydney system (5). Levels of SLPI in antral biopsies from all three groups were correlated to corresponding activity and chronicity scores. The line represents the median of the data that were analyzed by nonparametric Spearman correlation. CI, confidence interval.
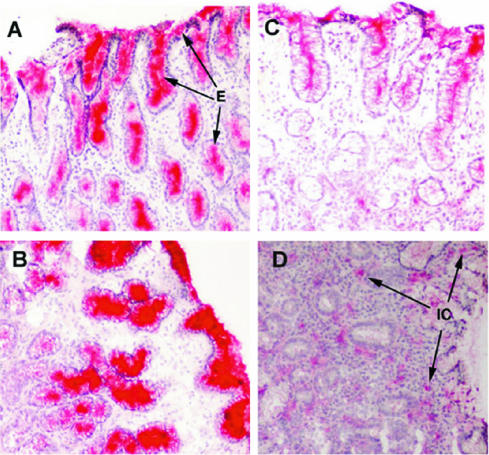
Immunohistochemistry showed that the diminished SLPI content of the gastric mucosa was a result of reduced SLPI expression by epithelial cells and that inflammatory cells contribute only little to mucosal SLPI expression (Fig. 3). Interestingly, the reduction of mucosal SLPI levels was not accompanied by a corresponding decrease in the SLPI transcript levels, implying a translational or posttranslational regulation. In vitro studies have shown that the proinflammatory cytokines as well as bacterial lipopolysaccharide can induce SLPI gene expression (4, 16). In contrast, H. pylori infection was associated with decreased SLPI levels in our study. Since we are not able to distinguish between the constitutive and potential inflammation-induced expression of SLPI, the decreased SLPI levels in the antrum might be a combination of translational and posttranslational effects (e.g., consumption and higher degradation) and the transcriptional induction by proinflammatory cytokines. Functionally, decreased antral SLPI levels might lead to higher proteolytic activity of serine proteases in the mucosal microenvironment, as proposed by others (14). Furthermore, SLPI was found to be involved in NF-κB signaling in lung tissue (17). Based on this finding, SLPI could represent a regulator of the NF-κB pathway that is activated in response to H. pylori (12). Whether SLPI has antibacterial activity toward H. pylori, as shown for other bacteria (7), has not been studied, but this potential interaction could represent an additional defense mechanism of gastric mucosa.
FIG. 3.
Detection of SLPI in the gastric mucosa by immunohistochemistry. Signals illustrating SLPI appear in red, whereas the nuclei are counterstained with hematoxylin. The stainings of H. pylori-negative (A and B) and H. pylori-positive (C and D) specimens demonstrate representatively the in vivo expression of SLPI. In addition to epithelial cells (E) of the mucosa and deep foveolar secretory glands, inflammatory cells (IC) are present in H. pylori-positive tissue specimens. Control experiments performed with unrelated rabbit antiserum as the primary antibody did not show specific staining (data not shown).
In conclusion, the epithelium-specific protease inhibitor SLPI was found to be differentially expressed in distinct regions of the gastroduodenal mucosa. Infection by H. pylori and/or the associated gastritis resulted in a local loss of SLPI in the antrum, whereas corpus, duodenal, and systemic SLPI types of expression were not affected. The loss of SLPI is regulated at translational or posttranslational level and is completely reversed after eradication therapy.
Acknowledgments
We thank the endoscopic team for its assistance and Ursula Stolz, Simone Philipsen, and Nadine Siebert for experimental work.
This work was supported in part by the “Deutsche Forschungsgemeinschaft,” Germany (We2170/3-1).
Editor: V. J. DiRita
REFERENCES
- 1.Ashcroft, G. S., K. Lei, W. Jin, G. Longenecker, A. B. Kulkarni, T. Greenwell-Wild, H. Hale-Donze, G. McGrady, X. Y. Song, and S. M. Wahl. 2000. Secretory leukocyte protease inhibitor mediates non-redundant functions necessary for normal wound healing. Nat. Med. 6:1147-1153. [DOI] [PubMed] [Google Scholar]
- 2.Bergenfeldt, M., M. Nystrom, M. Bohe, C. Lindstrom, A. Polling, and K. Ohlsson. 1996. Localization of immunoreactive secretory leukocyte protease inhibitor (SLPI) in intestinal mucosa. J. Gastroenterol. 31:18-23. [DOI] [PubMed] [Google Scholar]
- 3.Cave, D. R. 2001. Chronic gastritis and Helicobacter pylori. Semin. Gastrointest. Dis. 12:196-202. [PubMed] [Google Scholar]
- 4.Ding, A., N. Thieblemont, J. Zhu, F. Jin, J. Zhang, and S. Wright. 1999. Secretory leukocyte protease inhibitor interferes with uptake of lipopolysaccharide by macrophages. Infect. Immun. 67:4485-4489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dixon, M. F., R. M. Genta, J. H. Yardley, and P. Correa. 1996. Classification and grading of gastritis. The updated Sydney system. International Workshop on the Histopathology of Gastritis, Houston 1994. Am. J. Surg. Pathol. 20:1161-1181. [DOI] [PubMed] [Google Scholar]
- 6.Gipson, T. S., N. M. Bless, T. P. Shanley, L. D. Crouch, M. R. Bleavins, E. M. Younkin, V. Sarma, D. F. Gibbs, W. Tefera, P. C. McConnell, W. T. Mueller, K. J. Johnson, and P. A. Ward. 1999. Regulatory effects of endogenous protease inhibitors in acute lung inflammatory injury. J. Immunol. 162:3653-3662. [PubMed] [Google Scholar]
- 7.Hiemstra, P. S., R. J. Maassen, J. Stolk, R. Heinzel-Wieland, G. J. Steffens, and J. H. Dijkman. 1996. Antibacterial activity of antileukoprotease. Infect. Immun. 64:4520-4524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Konturek, P. C., W. Bielanski, S. J. Konturek, and E. G. Hahn. 1999. Helicobacter pylori associated gastric pathology. J. Physiol. Pharmacol. 50:695-710. [PubMed] [Google Scholar]
- 9.Leodolter, A., J. E. Dominguez-Munoz, U. von Arnim, S. Kahl, U. Peitz, and P. Malfertheiner. 1999. Validity of a modified 13C-urea breath test for pre- and posttreatment diagnosis of Helicobacter pylori infection in the routine clinical setting. Am. J. Gastroenterol. 94:2100-2104. [DOI] [PubMed] [Google Scholar]
- 10.Lindholm, C., M. Quiding-Jarbrink, H. Lonroth, and A. M. Svennerholm. 2001. Induction of chemokine and cytokine responses by Helicobacter pylori in human stomach explants. Scand. J. Gastroenterol. 36:1022-1029. [DOI] [PubMed] [Google Scholar]
- 11.Malfertheiner, P., D. Enrique, H. Heckenmuller, M. Neubrand, H. P. Fischer, and T. Sauerbruch. 1996. Modified rapid urease test for detection of Helicobacter pylori infection. Eur. J. Gastroenterol. Hepatol. 8:53-56. [DOI] [PubMed] [Google Scholar]
- 12.Naumann, M. 2001. Host cell signaling in Helicobacter pylori infection. Int. J. Med. Microbiol. 291:299-305. [DOI] [PubMed] [Google Scholar]
- 13.Potempa, J., E. Korzus, and J. Travis. 1994. The serpin superfamily of proteinase inhibitors: structure, function, and regulation. J. Biol. Chem. 269:15957-15960. [PubMed] [Google Scholar]
- 14.Sallenave, J. M., J. Shulmann, J. Crossley, M. Jordana, and J. Gauldie. 1994. Regulation of secretory leukocyte proteinase inhibitor (SLPI) and elastase-specific inhibitor (ESI/elafin) in human airway epithelial cells by cytokines and neutrophilic enzymes. Am. J. Respir. Cell Mol. Biol. 11:733-741. [DOI] [PubMed] [Google Scholar]
- 15.Si-Tahar, M., D. Merlin, S. Sitaraman, and J. L. Madara. 2000. Constitutive and regulated secretion of secretory leukocyte proteinase inhibitor by human intestinal epithelial cells. Gastroenterology 118:1061-1071. [DOI] [PubMed] [Google Scholar]
- 16.Sumi, Y., H. Muramatsu, K. Hata, M. Ueda, and T. Muramatsu. 2000. Secretory leukocyte protease inhibitor is a novel inhibitor of fibroblast-mediated collagen gel contraction. Exp. Cell Res. 256:203-212. [DOI] [PubMed] [Google Scholar]
- 17.Taggart, C. C., C. M. Greene, N. G. McElvaney, and S. O'Neill. 2002. Secretory leucoprotease inhibitor prevents LPS-induced Ikappa Balpha degradation without affecting phosphorylation or ubiquitination. J. Biol. Chem. 277:33648-33653. [DOI] [PubMed] [Google Scholar]
- 18.Wex, T., G. Treiber, U. Lendeckel, and P. Malfertheiner. 2003. A two step method for the extraction of high-quality RNA from endoscopic biopsies. Clin. Chem. Lab. Med. 41:1033-1337. [DOI] [PubMed] [Google Scholar]
- 19.Zhang, D., R. C. Simmen, F. J. Michel, G. Zhao, D. Vale-Cruz, and F. A. Simmen. 2002. Secretory leukocyte protease inhibitor mediates proliferation of human endometrial epithelial cells by positive and negative regulation of growth-associated genes. J. Biol. Chem. 277:29999-30009. [DOI] [PubMed] [Google Scholar]