Abstract
The molecular diagnosis of respiratory infection can be performed using different commercial multiplex-based PCR kits whose performances have been previously compared individually to those of conventional techniques. This study compared the practicability and the diagnostic performances of six CE-marked kits available in 2011 on the French market, including 2 detecting viruses and atypical bacteria (from Pathofinder and Seegene companies) and 4 detecting only viruses (from Abbott, Genomica, Qiagen and Seegene companies). The respective sensitivity, specificity, accuracy and agreement of each multiplex technique were calculated by comparison to commercial duplex PCR tests (Argene/bioMérieux) used as gold standard. Eighty-eight respiratory specimens with no pathogen (n = 11), single infections (n = 33) or co-infections (n = 44) were selected to cover 9 viruses or groups of viruses and 3 atypical bacteria. All samples were extracted using the NUCLISENS® easyMAG™ instrument (bioMérieux). The overall sensitivity ranged from 56.25% to 91.67% for viruses and was below 50% with both tests for bacteria. The overall specificity was excellent (>94% for all pathogens). For each tested kit, the overall agreement with the reference test was strong for viruses (kappa test >0.60) and moderate for bacteria. After the extraction step, the hands-on time varied from 50 min to 2h30 and the complete results were available in 2h30 to 9 h. The spectrum of tested agents and the technology used to reveal the PCR products as well as the laboratory organization are determinant for the selection of a kit.
Introduction
The global burden of acute respiratory infection (ARI) remains a huge problem of Public Health. In developed countries, the number of viral respiratory episodes per year has been estimated between 6 and 10 in children before school age versus 3 to 5 in those after this age and ARI represents the cause of 30 to 40% of hospital admissions in this category of patients [1] [2]. A wide range of pathogens are involved in ARI, including bacteria and viruses.
The diagnosis of ARI relies both on clinical examination, radiological exploration and biological nonspecific inflammatory tests (including the level of protein C reactive or procalcitonin). The identification of the causative agent(s) is often omitted or limited to a few pathogens easy to detect by rapid antigen direct tests (influenza viruses and respiratory syncytial virus (RSV) in respiratory specimens, Streptococcus pneumoniae and Legionella pneumophila in urine specimens). However, the distinction between viral and bacterial infections is often impossible by using non-microbiological criteria [3]–[4].
The need for precise and rapid identification of the causative agents of ARI has been reviewed recently [2], [5]–[6]. The main advantages of this strategy are (i) a better use of antimicrobials including antiviral drugs and antibiotics [3], [7] and thus limiting the development of bacterial resistance, (ii) the reduction of unnecessary paraclinical explorations and of the duration of hospitalization [8], (iii) the rapid implementation of isolation measures when necessary, thus limiting the risk of nosocomial transmission, (iv) the collection in real time of new epidemiological data on the seasonal spread of pathogens, and (v) the identification of simultaneous or successive infections [6], [9]–[10] that may justify specific intervention or explain the severity of the clinical picture.
The detection of agent’s genome responsible for respiratory infection have been revolutionized by recent advances in the field of nucleic acid amplification tests and notably of multiplex PCR [4], [11]–[14]. In addition to their excellent sensitivity, much superior to that of conventional techniques [15], these techniques allow the simultaneous detection of a wide range of pathogens, mostly viruses [16]–[19], but also atypical bacteria (including Mycoplasma pneumoniae, Chlamydophila pneumoniae, L. pneumophila and Bordetella pertussis) [20]–[23], with a short-time return of the results to clinicians.
The objective of the present study was to evaluate the technical performances of six commercial kits based on multiplex PCR and available on the European market at the beginning of 2011 for the diagnosis of respiratory infection. The kits were compared to a combination of biplex PCR tests used as gold standard on a panel of respiratory secretions selected for their content in various infectious agent(s). The performances of each kit for detecting different respiratory pathogens, including sensitivity, specificity, accuracy and agreement, were evaluated for each agent; other technical properties were also taken into consideration. Globally, the kits whose commercial development is still pursued were shown to be convenient for routine use in a clinical laboratory setting.
Materials and Methods
Presentation of the Kits used in this Study
Six kits based on multiplex detection of respiratory viruses or atypical bacteria and available in the French market in 2011 were tested. All were used as recommended by the manufacturers. The technologies are depicted in Figure 1. Letters A to F were used to design the kits in the following sections. Kit A corresponds to RespiFinder® SMART 22 (Pathofinder, Maastricht, The Netherlands); the reverse transcription and preamplification steps were performed on GeneAmp® PCR system 2700 (Applied Biosystems) and the hybridization, ligation and detection steps on the LightCycler®480 system (Roche Applied Science). Kit B corresponds to the Seeplex® RV15 OneStep ACE Detection and Pneumobacter ACE Detection (Seegene Inc., Seoul, South Korea); a GeneAmp® PCR system 9700 (Applied Biosystems) was used for amplification and the size of PCR products was read on a TapeStation after electrophoresis using ScreenTape. Kit C corresponds to the Magicplex RV Panel Real-time Test (Seegene Inc); the amplification was performed using GeneAmp® PCR system 9700 (Applied Biosystems) and the detection of PCR products was done on ABI7500 (Applied Biosystems). Kit D corresponds to Clart® Pneumovir (Genomica, Madrid, Spain); the amplification was performed on GeneAmp® PCR system 2700 (Applied Biosystems) and the hybridization of PCR products on the array was read using the Clinical Array System (CAR) (Genomica). Kit E corresponds to xTAG® respiratory Viral Panel fast (Abbott, Rungis, France) and kit F to ResPlex II Panel v2.0 (Qiagen, Hilden, Germany), for these two kits, the amplification was performed on GeneAmp® PCR system 9700 (Applied Biosystems) and the detection of PCR products on a Luminex platform (Bio-Plex, Bio-Rad).
Figure 1. Schematic synopsis of the design of the study.
(See text for correspondence between letters and commercial denominations).
The test used as gold standard for evaluating the six kits described above corresponds to a combination of 7 duplex Respiratory Multi Well System r-gene™ (Influenza A/B, RSV/hMPV, Rhino&EV/CC, AD/hBoV, Chla/Myco pneumo, HCoV/HPIV and Bordetella) commercialized by Argene/bioMérieux (Marcy l’Etoile, France). The real-time PCR reactions were performed on an ABI7500fast (Applied Biosystems).
The viruses and/or bacteria that could be detected by the 7 kits mentioned above are listed in Table 1.
Table 1. Presentation of the 7 kits used in the study for detecting viruses (see text for correspondence between letters and commercial denominations).
| Gold standard | A | B | C | D | E | F | |
| Influenza A viruses | Yes | Yes w diff A(H1N1)pdm09 | Yes | Yes | Yes w diff A(H1N1)pdm09 | Yes w diff (H1 and H3) | Yes |
| Other influenza viruses | B | B | B | B | B and C | B | B |
| Respiratory syncytial virus | Yes | Yes w diff | Yes w diff | Yes | Yes w diff | Yes | Yes w diff |
| Metapneumovirus | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Parainfluenza viruses | Yes | Yes w diff | Yes w diff | Yes w diff | Yes w diff | Yes w diff | Yes w diff |
| Picornaviruses (rhinovirus/enterovirus) | Yes | Yes | Yes w diff betweenrhinovirus A, B and C,and enterovirus | Yes | Yes w diff rhinovirus and enterovirus B | Yes | Yes w diff rhinovirus and coxsackie virus/echovirus |
| Coronaviruses | Yes | Yes w diff betweenthe 4 types | Yes (except HKU1) w diffbetween OC43and 229E/NL63 | Yes (except HKU1) wdiff between the3 types | Detection of 229E only | Yes w diff betweenthe 4 types | Yes w diff between the 4 types |
| Adenoviruses | Yes (A to G) | Yes | Yes | Yes | Yes | Yes | Yes (B and E only) |
| Bocavirus | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Mycoplasma pneumoniae | Yes | Yes | Yes | No | No | No | No |
| Chlamydophila pneumoniae | Yes | Yes | Yes | No | No | No | No |
| Bordetella pertussis | Yes | Yes | Yes | No | No | No | No |
Yes: group of pathogens detected; w diff: with differentiation between types. No: group of pathogens not detected.
Selection and Preparation of the Respiratory Samples
In order to constitute a representative panel of specimens containing a wide range of the respiratory pathogens (viruses and atypical bacteria) tested in the evaluated kits, 88 respiratory samples (30 from the University Hospital of Caen and 58 from the University Hospital of Saint-Etienne, France; one half being nasal swab and one half being respiratory secretions) were selected (by S.P., F.G., J.D. and A.V.) for the study. Viral and bacterial pathogens were routinely detected by immunofluorescence assay (respiratory syncytial viruses, influenza viruses, parainfluenza viruses, adenoviruses, and metapneumoviruses in Saint-Etienne) or molecular methods (home-brew method for influenza A H1N1pdm09 [24] in Saint-Etienne; Chlamylege kit from Argene/bioMérieux [20] for atypical bacteria in Saint-Etienne; home-brew molecular methods for viruses (rhinoviruses/enteroviruses, adenoviruses, bocavirus, coronaviruses, parainfluenza viruses and metapneumoviruses) in Caen [11], [15], [25]–[26]). The criteria of selection were (i) the presence of clinical ARI, (ii) the detection of a respiratory pathogen by the routine tests described above (except for 14 specimens that were tested initially negative), and (iii) a volume of sample of at least 1.6 ml. The study was conducted on the residual clinical specimens stored at −80°C; for this reason, no informed consent was required from the patients. However, the study was submitted to the approval of the local Ethic Committee of the University Hospital of Saint-Etienne. The results of these screening tests were taken into consideration for the selection of a representative diversity of respiratory pathogens but not for the final analysis because many specimens were found positive for additional pathogens with reference to this preliminary screening.
The samples were fractionated blindly (by M.L.) into 7 tubes containing 200 µl of specimen and frozen at −80°C. For each technique tested, one aliquot of each specimen was thawed and nucleic acids were extracted using the NUCLISENS® easyMAG™ (bioMérieux) in presence of 20 µl of proteinase K (10 mg/ml) and of internal control when available, as recommended by the manufacturers (Figure 1). The nucleic acids were eluted in a volume of 100 µl for kit A, 50 µl for kits B, C, D and F, and 55 µl for kit E; for the reference method, 400 µl of sample were eluted in 100 µl. The reverse transcription and PCR reactions were performed immediately after extraction. The extracts were then conserved at −80°C for further investigation if necessary.
Validation and Analysis of Results
When a signal was detected, it was considered as positive. The interpretation of the results obtained by each kit was validated with the acknowledgement of the corresponding supplier.
The respective sensitivity, specificity, accuracy and agreement (as evaluated by the Cohen kappa coefficient) of each tested kit were calculated by reference to the performances of the Argene/bioMérieux duplex tests used as gold standard.
Results
Characterization of the Panel and Overall Results
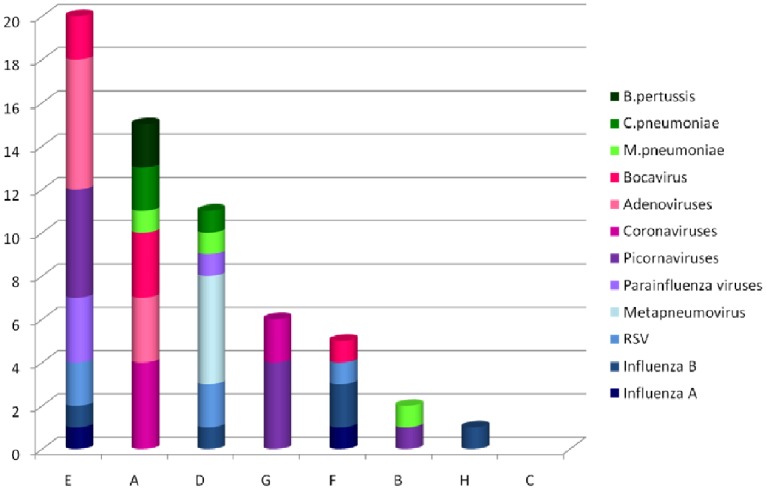
Following testing of the 88 samples with the reference method, the number of each pathogen considered to be present in the panel was as depicted in Table 2. Most pathogens, with the exception of influenza A virus, were frequently associated with at least another pathogen. The performances of each kit are summarized in Table 3 for viruses and in Table 4 for bacteria.
Table 2. List of pathogens that were considered to be present in the panel of the 88 specimens according the combination of duplex PCR tests (Argene/bioMérieux) used as gold standard.
| Pathogens | Single infections | Co-infections | Total | |
| with another pathogen | with at least 2 other pathogens | |||
| Influenza A viruses | 4 | 3 | 0 | 7 |
| Influenza B viruses | 0 | 5 | 0 | 5 |
| Respiratory syncytial virus | 3 | 4 | 6 | 13 |
| Metapneumovirus | 0 | 2 | 2 | 4 |
| Parainfluenza virusesa | 3 | 4 | 3 | 10 |
| Rhinoviruses/enteroviruses | 8 | 5 | 10 | 23 |
| Coronavirusesb | 7 | 5 | 13 | 25 |
| Adenoviruses | 2 | 9 | 11 | 22 |
| Bocaviruses | 1 | 4 | 7 | 12 |
| Mycoplasma pneumoniae | 2 | 4 | 4 | 10 |
| Chlamydophila pneumoniae | 1 | 1 | 2 | 4 |
| Bordetella pertussis | 2 | 4 | 3 | 9 |
| None | – | – | – | 11 |
type 1 (n = 2), type 3 (n = 3) and type 4 (n = 5).
type NL63 (n = 6), type OC43 (n = 8), type 229E (n = 1), type HKU1 (n = 6) and untyped (n = 4).
Table 3. Performances of the 6 kits evaluated in this study for a panel of 9 viruses or groups of viruses with reference to the combination of duplex PCR tests (Argene/bioMérieux) used as gold standard.
| Pathogens tested | No. of positive specimens with the reference test | Performances | Evaluated kits | |||||
| A | B | C | D | E | F | |||
| Influenza A | 7 | sensitivity % | 100 | 57.14 | 100 | 100 | 100 | 57.14 |
| specificity % | 100 | 100.00 | 98.78 | 98.78 | 100 | 100 | ||
| accuracy | 1.00 | 0.97 | 0.99 | 0.99 | 1.00 | 0.97 | ||
| kappa coefficient [95% confidence interval] | 1 [1;1] | 0.71 [0.40; 1] | 0.93 [0.79; 1] | 0.93 [0.79; 1] | 1 [1;1] | 0.71[0.40; 1] | ||
| Influenza B | 5 | sensitivity % | 80.00 | 60.00 | 100 | 100 | 60.00 | 60.00 |
| specificity % | 100 | 98.81 | 98.81 | 97.65 | 100 | 98.81 | ||
| accuracy | 0.99 | 0.97 | 0.99 | 0.98 | 0.98 | 0.97 | ||
| kappa coefficient [95% confidence interval] | 0.88 [0.66; 1] | 0.65 [0.28; 1] | 0.90 [0.72; 1] | 0.82 [0.58; 1] | 0.74 [0.39; 1] | 0.65 [0.28; 1] | ||
| RSV | 13 | sensitivity % | 92.31 | 92.31 | 100 | 100 | 92.31 | 69.23 |
| specificity % | 98.68 | 96.15 | 91.46 | 96.15 | 100 | 100 | ||
| accuracy | 0.98 | 0.95 | 0.92 | 0.97 | 0.99 | 0.95 | ||
| kappa coefficient [95% confidence interval] | 0.91 [0.79; 1] | 0.830 [0.67; 0.99] | 0.74 [0.56; 0.92] | 0.88[0.74; 1] | 0.95[0.86; 1] | 0.79 [0.60; 0.99] | ||
| Meta pneumovirus | 4 | sensitivity % | 100 | 75.00 | 100 | 100 | 100 | 75.00 |
| specificity % | 98.82 | 93.33 | 98.82 | 98.82 | 98.82 | 98.82 | ||
| accuracy | 0.99 | 0.92 | 0.99 | 0.99 | 0.99 | 0.98 | ||
| kappa coefficient [95% confidence interval] | 0.88[0.66; 1] | 0.42[0.08; 0.77] | 0.88[0.66; 1] | 0.88[0.66; 1] | 0.88 [0.66; 1] | 0.74 [0.39; 1] | ||
| Parainfluenza viruses | 10 | sensitivity % | 90.00 | 80.00 | 100 | 100 | 100 | 70.00 |
| specificity % | 97.50 | 97.50 | 92.86 | 97.50 | 97.50 | 100 | ||
| accuracy | 0.97 | 0.95 | 0.93 | 0.98 | 0.98 | 0.97 | ||
| kappa coefficient [95% confidence interval] | 0.83[0.66; 1] | 0.77[0.56; 0.99] | 0.73[0.53; 0.93] | 0.90[0.76; 1] | 0.90[0.76; 1] | 0.81[0.59; 1] | ||
| Rhinoviruses/enteroviruses | 23 | sensitivity % | 86.96 | 39.13 | 91.30 | 82.61 | 100 | 82.61 |
| specificity % | 91.55 | 100 | 84.42 | 90.28 | 83.33 | 94.20 | ||
| accuracy | 0.90 | 0.84 | 0.84 | 0.88 | 0.85 | 0.91 | ||
| kappa coefficient[95% confidence interval] | 0.75[0.59; 0.90] | 0.49[0.28; 0.70] | 0.64[0.50; 0.78] | 0.69 [0.52; 0.86] | 0.68[0.52; 0.83] | 0.77[0.61; 0.92] | ||
| Coronaviruses | 25 | sensitivity % | 80.00 | 24.00 a | 84.00 | 4.00 b | 76.00 | 48.00 |
| specificity % | 98.44 | 100 | 98.44 | 100 | 96.92 | 100 | ||
| accuracy | 0.93 | – | 0.94 | – | 0.91 | 0.85 | ||
| kappa coefficient[95% confidence interval] | 0.82[0.69; 0.96] | – | 0.85 [0.75; 0.96] | – | 0.77[0.61; 0.92] | 0.57 [0.37; 0.76] | ||
| Adenoviruses | 22 | sensitivity % | 63.64 | 45.45 | 86.36 | 59.09 | 45.45 | 31.82 |
| specificity % | 100 | 100 | 92.96 | 100 | 100 | 100 | ||
| accuracy | 0.91 | 0.86 | 0.91 | 0.90 | 0.86 | 0.83 | ||
| kappa coefficient[95% confidence interval] | 0.72 [0.55; 0.90] | 0.56 [0.35; 0.77] | 0.77 [0.61; 0.92] | 0.68 [0.50; 0.87] | 0.56 [0.36; 0.77] | 0.41 [0.19; 0.63] | ||
| Bocavirus | 12 | sensitivity % | 50.00 | 25.00 | 75.00 | 58.33 | 33.33 | 16.67 |
| specificity % | 100 | 100 | 97.44 | 98.70 | 100 | 100 | ||
| accuracy | 0.93 | 0.90 | 0.94 | 0.93 | 0.91 | 0.89 | ||
| kappa coefficient[95% confidence interval] | 0.63 [0.37; 0.90] | 0.37 [0.06; 0.67] | 0.75 [0.54; 0.96] | 0.66 [0.42; 0.91] | 0.46[0.16; 0.76] | 0.26[0; 0.55] | ||
| Overall(except coronaviruses)c | 96 | sensitivity % | 79.17 | 54.17 | 91.67 | 81.25 | 76.04 | 56.25 |
| specificity % | 98.41 | 98.16 | 94.32 | 97.28 | 97.46 | 99.08 | ||
| accuracy | 0.96 | 0.92 | 0.94 | 0.95 | 0.94 | 0.93 | ||
| kappa coefficient[95% confidence interval] | 0.81[0.75; 0.88] | 0.61[0.51; 0.70] | 0.77[0.70; 0.83] | 0.79[0.72; 0.86] | 0.76[0.69; 0.83] | 0.66[0.58; 0.73] | ||
Kit having no probe for the detection of HKU1 coronavirus.
Kit having a probe for detecting 229E coronavirus only.
All the tested kits did not detect all the coronavirus types (see notes a and b).
Table 4. Performances of the 2 kits evaluated in this study for a panel of 3 atypical bacteria with reference to the combination of duplex PCR tests (Argene/bioMérieux) used as gold standard.
| Pathogens tested | No. of positive specimenswith the reference test | Performances | Evaluated kits | |
| A | B | |||
| Mycoplasma pneumoniae | 10 | sensitivity % | 70.00 | 80.00 |
| specificity % | 100 | 98.73 | ||
| accuracy | 0.97 | 0.97 | ||
| kappa coefficient[.95% confidence interval] | 0.81 [0.59; 1] | 0.82 [0.63; 1] | ||
| Chlamydophila pneumoniae | 4 | sensitivity % | 50.00 | 50.00 |
| specificity % | 100 | 100 | ||
| accuracy | 0.98 | 0.98 | ||
| kappa coefficient[95% confidence interval] | 0.66 [0.21; 1] | 0.66 [0.21; 1] | ||
| Bordetella pertussis | 9 | sensitivity % | 11.11 | 11.11 |
| specificity % | 100 | 98.75 | ||
| accuracy | 0.91 | 0.90 | ||
| kappa coefficient[95% confidence interval] | 0.18 [0; 0.50] | 0.15 [0; 0.45] | ||
| Overall | 23 | sensitivity % | 43.48 | 47.83 |
| specificity % | 100 | 99.21 | ||
| accuracy | 0.95 | 0.95 | ||
| kappa coefficient[95% confidence interval] | 0.58 [0.38; 0.79] | 0.59 [0.39; 0.78] | ||
Sensitivity of the Tested Kits for Detecting Respiratory Pathogens
The overall sensitivity ranged from 56.25% to 91.67% for viruses (Table 3). Kits B and F exhibited the poorest sensitivity for most viral agents. The other tests were found sensitive for influenza viruses (except for kit E with influenza B virus), RSV, metapneumovirus and parainfluenza viruses, but less sensitive than the gold standard for rhinoviruses/enteroviruses, adenoviruses and bocavirus. The panel composition for coronaviruses (Table 2) explains the low sensitivity of kits B and D that detect only some types of these pathogens (Table 1). Regarding bacteria, the sensitivity of kits A and B was satisfying for Mycoplasma pneumoniae but of 50% for Chlamydophila pneumoniae and close to 10% for Bordetella pertussis (Table 4).
Other Performances of the Tested Kits
The overall specificity of all the kits was excellent (>94% for all pathogens); the lowest specificity was observed for rhinoviruses/enteroviruses with kits C and E (84.4% and 83.3%, respectively). Globally, the accuracy was adequate, even if lower values were observed for rhinoviruses/enteroviruses and adenoviruses. The Cohen kappa coefficient, which reflects the agreement with the gold standard, was globally strong for viruses (>0.60) (Table 3) and moderate for bacteria (0.41–0.60) (Table 4).
Practicability
The criteria evaluated for the technical and workflow characteristics of each kit are depicted in Table 5. Ten to 22 samples were analyzed in one run. The extraction step was controlled by the addition of an internal control in 3 of the 7 kits. Ten to 70 µl of extract were needed for analysis. After the extraction step, the hands-on time varied from 50 min to 2h15 depending on the number of reaction tube opening, the availability of ready-to-use reagents and the number of mastermix. The signal interpretation was driven by using dedicated software in only three kits. The run duration varied from 2h30 to 9 h.
Table 5. Practicability of each kit using the NUCLISENS easyMAG as extraction instrument (see text for correspondence between letters and commercial denominations).
| Gold standard | A | B | C | D | E | F | |
| Throughput (number of tested specimen/run) | 10 | 22 | 13 | 22 | 22 | 22 | 22 |
| Hands on time | 50 min | 2h15 | 2h15 | 1h45 | 2 h | 1h30 | 1h30 |
| Run duration | 2h30 | 7 h | 7 h | 5h30 | 9 h | 4h30 | 4h30 |
| Number of reaction tubes opening | 0 | 2 | 1 | 2 | 1 | 1 | 3 |
| Ready to use reagents | yes | no | no | no | yes | no | no |
| Addition of internal control at the extraction step | no | yes | no | no | no | yes | yes |
| Amplification of a cellular gene control | yes | no | yes | yes | no | no | no |
| Volume of extracted sample | 100 µl | 10 µl | 33 µl | 11 µl | 10 µl | 10 µl | 10 µl |
| Number of mixtures | 7 | 2 | 4 | 3 | 2 then 1 | 1 | 1 |
| Software for results interpretation | no | no | yes | no | yes | yes | no |
| Access to raw data | yes | yes | yes | yes | yes | yes | yes |
Discussion
To our knowledge, this study is the first that compared 6 commercialized multiplex PCR techniques for the detection of respiratory pathogens. Five of these kits (A, B, D, E and F) had been previously evaluated versus conventional techniques [27]–[31], home-brew PCR [29], [31]–[35], or other commercial multiplex kits [27]–[31], [33]–[34], [36]–[41]. However, none of these studies compared more than 4 commercialized techniques simultaneously. It is noteworthy that the 6 kits tested in this study do not constitute an exhaustive panel of the techniques presently commercialized on the world market but are representative of those available in Europe at the beginning of 2011.
The present comparison includes two multiplex techniques (A and B) that were able to detect respiratory viruses together with atypical bacteria. The molecular diagnosis of these bacteria is most often performed by using home-brew methods and few commercial techniques have been evaluated comparatively [20]–[23]. The simultaneous detection of atypical bacteria and viruses represents a great advantage in terms of clinical management. Indeed, in case of positive result for an atypical bacterium, a rapid treatment with an adapted antimicrobial drug can be proposed [22]; by contrast, if this information is lacking, there is a risk for prescribing no treatment, especially if the specimen is also found positive for one or several viruses, a rather common situation with the present panel. In the opposite case, the absence of atypical bacteria (together with the negativity of conventional bacterial cultures) would allow to spare useless antibiotic treatment and consequently the emergence of bacterial resistance [7].
This study exhibits a few limitations. No gold standard is available for each of the 12 pathogens tested in this study. Even if molecular techniques are globally considered as the most sensitive, it is difficult to identify a precise method as the reference for a given pathogen or family of pathogens. In addition, the sensitivity may vary when the test is adapted to the whole family (adenoviruses, rhinoviruses/enteroviruses, parainfluenza viruses, coronaviruses…) or specific for a single type. Despite this difficulty, the Argene/bioMérieux strategy, which consists in the combination of duplex real time PCR methods, was taken as gold standard in the present study; actually, the reduced primer competition due to a combination of biplex amplification together with a higher volume of extracted sample are indicative of a good sensitivity. The low number of strains for some pathogens (i.e. C.pneumophila) and the absence of others (notably parainfluenza virus type 2 and L.pneumophila) constitute an additional limit of the study for accurate comparisons. Another difficulty for comparing these different kits relies on the level of differentiation of the tested pathogens that varied greatly from a manufacturer to another; for instance, some kits were able to detect coronaviruses and parainfluenza viruses at the type or species level whereas others considered the genus level only. For adenoviruses and rhino/enteroviruses, most of the kits used genus-specific targets. Of note, none of the kits was able to detect Parechovirus despite the recent involvement of this genus of Picornaviridae in respiratory infection [42]–[43].
In terms of sensitivity, kits B and F exhibited the lowest results, in accordance to previous evaluations in comparison to other molecular tests [28], [30], [32]–[36] despite their good performance with reference to conventional techniques [34], [44]–[46]. These “pioneer” technologies were either stopped or improved through new generation kits, as exemplified by kit C that represents a further version of kit B and exhibits the best sensitivity for all the tested viruses. The fact that the panel included a large number of multiple infections could explain some missed results with the multiplex PCR assays tested in this study; indeed, this technology favors primers’ competition, notably for the pathogen(s) exhibiting the lower load in the specimen. This observation may explain the overall low sensitivity observed for coronaviruses, adenoviruses and bocaviruses. Concerning kit D, in accordance to previous results with home-brew PCR techniques [9], [18], it exhibited a correct sensitivity except for coronavirus, essentially because it detects only the 229E type. Kit E was extensively tested with good analytical performance [27]–[28], [30]–[31], [37]–[40]; the performances observed in this study confirm these results despite a few defects, notably for adenovirus, as reported before [30], [39]. The performances of kit A were satisfactory, in accordance with previous evaluations [29], [36], [38]–[39]; the poor results obtained with B. pertussis led to the change of the target used for detecting this bacterium.
Regarding the technical and workflow characteristics of the kits, it is important to favor techniques with ready-to-use reagents, little number of reaction tube opening and limited number of pipeting in order to reduce the risk of mistakes in reagent handling and of cross-contamination. In several companies, this trend was a marked feature for driving the evolution of their kit. The presence of an internal control and, if possible, of a cellular control is also recommended for checking the validity of negative results. Finally, although the results of all these techniques were available in less than 12 hours, the run duration varied significantly from a technique to another. Further studies would be needed for evaluating the consequence of this difference from a clinical point of view.
In conclusion, the present study constitutes an overview of the multiplex techniques that were available in 2011 on the European market for the diagnosis of respiratory infection. Their performances are globally satisfactory, at least for those that are still commercially-available in 2013. On the basis of the present evaluation, the spectrum of detected pathogens (with an advantage for the techniques detecting also atypical bacteria), the technology used for PCR product revelation and the laboratory organization appear as determinant features for the selection of a kit. Further studies are needed for evaluating the cost-benefit of these techniques in the clinical management of respiratory infection.
Acknowledgments
The suppliers of the kits evaluated in this study (Abbott, Argene/bioMérieux, BioNoBis, Eurobio, Eurogentec, Qiagen and R-Biopharm) are thoroughly acknowledged for providing the reagents free of charge and for their assistance in the validation of the results. The authors are indebted to Lucie Dancert for excellent technical support. Laurent Andréoletti, Bruno Lina, Florence Morfin and François Simon are thanked for helpful discussions in the setting of this project.
Funding Statement
The reagents were supplied by the respective manufacturers. The salaries of experimenters were paid by their respective institution. No current external funding sources were needed for this study.
References
- 1. Glezen P, Denny FW (1973) Epidemiology of acute lower respiratory disease in children. N Engl J Med 288: 498–505 doi:10.1056/NEJM197303082881005 [DOI] [PubMed] [Google Scholar]
- 2. Pavia AT (2011) Viral infections of the lower respiratory tract: old viruses, new viruses, and the role of diagnosis. Clin Infect Dis 52 Suppl 4S284–289 doi:10.1093/cid/cir043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gonzales R, Malone DC, Maselli JH, Sande MA (2001) Excessive antibiotic use for acute respiratory infections in the United States. Clin Infect Dis 33: 757–762 doi:10.1086/322627 [DOI] [PubMed] [Google Scholar]
- 4. Schnepf N, Resche-Rigon M, Chaillon A, Scemla A, Gras G, et al. (2011) High burden of non-influenza viruses in influenza-like illness in the early weeks of H1N1v epidemic in France. PLoS ONE 6: e23514 doi:10.1371/journal.pone.0023514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ginocchio CC (2011) Strengths and weaknesses of FDA-approved/cleared diagnostic devices for the molecular detection of respiratory pathogens. Clin Infect Dis 52 Suppl 4S312–325 doi:10.1093/cid/cir046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Pozzetto B, Grattard F, Pillet S (2010) Multiplex PCR theranostics of severe respiratory infections. Expert Rev Anti Infect Ther 8: 251–253 doi:10.1586/eri.09.131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brittain-Long R, Westin J, Olofsson S, Lindh M, Andersson L-M (2011) Access to a polymerase chain reaction assay method targeting 13 respiratory viruses can reduce antibiotics: a randomised, controlled trial. BMC Med 9: 44 doi:10.1186/1741-7015-9-44 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mahony JB, Blackhouse G, Babwah J, Smieja M, Buracond S, et al. (2009) Cost analysis of multiplex PCR testing for diagnosing respiratory virus infections. J Clin Microbiol 47: 2812–2817 doi:10.1128/JCM.00556-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Huguenin A, Moutte L, Renois F, Leveque N, Talmud D, et al. (2012) Broad respiratory virus detection in infants hospitalized for bronchiolitis by use of a multiplex RT-PCR DNA microarray system. J Med Virol 84: 979–985 doi:10.1002/jmv.23272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Paranhos-Baccalà G, Komurian-Pradel F, Richard N, Vernet G, Lina B, et al. (2008) Mixed respiratory virus infections. J Clin Virol 43: 407–410 doi:10.1016/j.jcv.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bellau-Pujol S, Vabret A, Legrand L, Dina J, Gouarin S, et al. (2005) Development of three multiplex RT-PCR assays for the detection of 12 respiratory RNA viruses. J Virol Methods 126: 53–63 doi:10.1016/j.jviromet.2005.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Fox JD (2007) Nucleic acid amplification tests for the detection and analysis of respiratory viruses: the future for diagnostics? Future Microbiol 2: 199–211 doi:10.2217/17460913.2.2.199 [DOI] [PubMed] [Google Scholar]
- 13. Loeffelholz MJ, Pong DL, Pyles RB, Xiong Y, Miller AL, et al. (2011) Comparison of the FilmArray Respiratory Panel and Prodesse real-time PCR assays for detection of respiratory pathogens. J Clin Microbiol 49: 4083–4088 doi:10.1128/JCM.05010-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mahony JB, Petrich A, Smieja M (2011) Molecular diagnosis of respiratory virus infections. Crit Rev Clin Lab Sci 48: 217–249 doi:10.3109/10408363.2011.640976 [DOI] [PubMed] [Google Scholar]
- 15. Freymuth F, Vabret A, Cuvillon-Nimal D, Simon S, Dina J, et al. (2006) Comparison of multiplex PCR assays and conventional techniques for the diagnostic of respiratory virus infections in children admitted to hospital with an acute respiratory illness. J Med Virol 78: 1498–1504 doi:10.1002/jmv.20725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Frobert E, Escuret V, Javouhey E, Casalegno JS, Bouscambert-Duchamp M, et al. (2011) Respiratory viruses in children admitted to hospital intensive care units: evaluating the CLART® Pneumovir DNA array. J Med Virol 83: 150–155 doi:10.1002/jmv.21932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Krunic N, Yager TD, Himsworth D, Merante F, Yaghoubian S, et al. (2007) xTAG RVP assay: analytical and clinical performance. J Clin Virol 40 Suppl 1S39–46 doi:10.1016/S1386-6532(07)70009-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Renois F, Talmud D, Huguenin A, Moutte L, Strady C, et al. (2010) Rapid detection of respiratory tract viral infections and coinfections in patients with influenza-like illnesses by use of reverse transcription-PCR DNA microarray systems. J Clin Microbiol 48: 3836–3842 doi:10.1128/JCM.00733-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Van Elden LJR, Van Loon AM, Van Alphen F, Hendriksen KAW, Hoepelman AIM, et al. (2004) Frequent detection of human coronaviruses in clinical specimens from patients with respiratory tract infection by use of a novel real-time reverse-transcriptase polymerase chain reaction. J Infect Dis 189: 652–657 doi:10.1086/381207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ginevra C, Barranger C, Ros A, Mory O, Stephan J-L, et al. (2005) Development and evaluation of Chlamylege, a new commercial test allowing simultaneous detection and identification of Legionella, Chlamydophila pneumoniae, and Mycoplasma pneumoniae in clinical respiratory specimens by multiplex PCR. J Clin Microbiol 43: 3247–3254 doi:10.1128/JCM.43.7.3247-3254.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Loens K, Beck T, Ursi D, Overdijk M, Sillekens P, et al. (2008) Evaluation of different nucleic acid amplification techniques for the detection of M. pneumoniae, C. pneumoniae and Legionella spp. in respiratory specimens from patients with community-acquired pneumonia. J Microbiol Methods 73: 257–262 doi:10.1016/j.mimet.2008.02.010 [DOI] [PubMed] [Google Scholar]
- 22. Lui G, Ip M, Lee N, Rainer TH, Man SY, et al. (2009) Role of “atypical pathogens” among adult hospitalized patients with community-acquired pneumonia. Respirology 14: 1098–1105 doi:10.1111/j.1440-1843.2009.01637.x [DOI] [PubMed] [Google Scholar]
- 23. McDonough EA, Barrozo CP, Russell KL, Metzgar D (2005) A multiplex PCR for detection of Mycoplasma pneumoniae, Chlamydophila pneumoniae, Legionella pneumophila, and Bordetella pertussis in clinical specimens. Mol Cell Probes 19: 314–322 doi:10.1016/j.mcp.2005.05.002 [DOI] [PubMed] [Google Scholar]
- 24. Duchamp MB, Casalegno JS, Gillet Y, Frobert E, Bernard E, et al. (2010) Pandemic A(H1N1)2009 influenza virus detection by real time RT-PCR: is viral quantification useful? Clin Microbiol Infect 16: 317–321 doi:10.1111/j.1469-0691.2010.03169.x [DOI] [PubMed] [Google Scholar]
- 25. Legrand L, Vabret A, Dina J, Petitjean-Lecherbonnier J, Stéphanie G, et al. (2011) Epidemiological and phylogenic study of human metapneumovirus infections during three consecutive outbreaks in Normandy, France. J Med Virol 83: 517–524 doi:10.1002/jmv.22002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dina J, Nguyen E, Gouarin S, Petitjean J, Parienti J-J, et al. (2009) Development of duplex real-time PCR for detection of two DNA respiratory viruses. J Virol Methods 162: 119–125 doi:10.1016/j.jviromet.2009.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Babady NE, Mead P, Stiles J, Brennan C, Li H, et al. (2012) Comparison of the Luminex xTAG RVP Fast assay and the Idaho Technology FilmArray RP assay for detection of respiratory viruses in pediatric patients at a cancer hospital. J Clin Microbiol 50: 2282–2288 doi:10.1128/JCM.06186-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Balada-Llasat J-M, LaRue H, Kelly C, Rigali L, Pancholi P (2011) Evaluation of commercial ResPlex II v2.0, MultiCode-PLx, and xTAG respiratory viral panels for the diagnosis of respiratory viral infections in adults. J Clin Virol 50: 42–45 doi:10.1016/j.jcv.2010.09.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bruijnesteijn van Coppenraet LES, Swanink CMA, Van Zwet AA, Nijhuis RHT, Schirm J, et al. (2010) Comparison of two commercial molecular assays for simultaneous detection of respiratory viruses in clinical samples using two automatic electrophoresis detection systems. J Virol Methods 169: 188–192 doi:10.1016/j.jviromet.2010.07.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Gharabaghi F, Hawan A, Drews SJ, Richardson SE (2011) Evaluation of multiple commercial molecular and conventional diagnostic assays for the detection of respiratory viruses in children. Clin Microbiol Infect 17: 1900–1906 doi:10.1111/j.1469-0691.2011.03529.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Jokela P, Piiparinen H, Mannonen L, Auvinen E, Lappalainen M (2012) Performance of the Luminex xTAG Respiratory Viral Panel Fast in a clinical laboratory setting. J Virol Methods 182: 82–86 doi:10.1016/j.jviromet.2012.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bibby DF, McElarney I, Breuer J, Clark DA (2011) Comparative evaluation of the Seegene Seeplex RV15 and real-time PCR for respiratory virus detection. J Med Virol 83: 1469–1475 doi:10.1002/jmv.22125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hayden RT, Gu Z, Rodriguez A, Tanioka L, Ying C, et al. (2012) Comparison of two broadly multiplexed PCR systems for viral detection in clinical respiratory tract specimens from immunocompromised children. J Clin Virol 53: 308–313 doi:10.1016/j.jcv.2011.12.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Li H, McCormac MA, Estes RW, Sefers SE, Dare RK, et al. (2007) Simultaneous detection and high-throughput identification of a panel of RNA viruses causing respiratory tract infections. J Clin Microbiol 45: 2105–2109 doi:10.1128/JCM.00210-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Wang W, Ren P, Sheng J, Mardy S, Yan H, et al. (2009) Simultaneous detection of respiratory viruses in children with acute respiratory infection using two different multiplex reverse transcription-PCR assays. J Virol Methods 162: 40–45 doi:10.1016/j.jviromet.2009.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Loens K, Van Loon AM, Coenjaerts F, Van Aarle Y, Goossens H, et al. (2012) Performance of different mono- and multiplex nucleic acid amplification tests on a multipathogen external quality assessment panel. J Clin Microbiol 50: 977–987 doi:10.1128/JCM.00200-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Rand KH, Rampersaud H, Houck HJ (2011) Comparison of two multiplex methods for detection of respiratory viruses: FilmArray RP and xTAG RVP. J Clin Microbiol 49: 2449–2453 doi:10.1128/JCM.02582-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Raymaekers M, De Rijke B, Pauli I, Van den Abeele A-M, Cartuyvels R (2011) Timely diagnosis of respiratory tract infections: evaluation of the performance of the Respifinder assay compared to the xTAG respiratory viral panel assay. J Clin Virol 52: 314–316 doi:10.1016/j.jcv.2011.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dabisch-Ruthe M, Vollmer T, Adams O, Knabbe C, Dreier J (2012) Comparison of three multiplex PCR assays for the detection of respiratory viral infections: evaluation of xTAG respiratory virus panel fast assay, RespiFinder 19 assay and RespiFinder SMART 22 assay. BMC Infect Dis 12: 163 doi:10.1186/1471-2334-12-163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Popowitch EB, O’Neill SS, Miller MB (2013) Comparison of four multiplex assays for the detection of respiratory viruses: Biofire FilmArray RP, Genmark eSensor RVP, Luminex xTAG RVPv1 and Luminex xTAG RVP FAST. J Clin Microbiol, in press doi:10.1128/JCM.03368-12 [DOI] [PMC free article] [PubMed]
- 41. Forman MS, Advani S, Newman C, Gaydos CA, Milstone AM, et al. (2012) Diagnostic performance of two highly multiplexed respiratory virus assays in a pediatric cohort. J Clin Virol 55: 168–172 doi:10.1016/j.jcv.2012.06.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Harvala H, Wolthers KC, Simmonds P (2010) Parechoviruses in children: understanding a new infection. Curr Opin Infect Dis 23: 224–230. [DOI] [PubMed] [Google Scholar]
- 43. Piralla A, Furione M, Rovida F, Marchi A, Stronati M, et al. (2012) Human parechovirus infections in patients admitted to hospital in Northern Italy, 2008–2010. J Med Virol 84: 686–690 doi:10.1002/jmv.23197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kim SR, Ki C-S, Lee NY (2009) Rapid detection and identification of 12 respiratory viruses using a dual priming oligonucleotide system-based multiplex PCR assay. J Virol Methods 156: 111–116 doi:10.1016/j.jviromet.2008.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Mak GC, Cheng PKC, Lim W (2011) Evaluation of Qiagen Resplex II for the detection of pandemic influenza A (H1N1) 2009 and influenza A (H3N2) virus. J Clin Virol 51: 88–89 doi:10.1016/j.jcv.2011.02.006 [DOI] [PubMed] [Google Scholar]
- 46. Yoo SJ, Kuak E-Y, Shin B-M (2007) Detection of 12 respiratory viruses with two-set multiplex reverse transcriptase-PCR assay using a dual priming oligonucleotide system. Korean J Lab Med 27: 420–427 doi:10.3343/kjlm.2007.27.6.420 [DOI] [PubMed] [Google Scholar]