Abstract
Pediatric sleep disordered breathing (PSDB) is not only a very frequent condition affecting 2–4% of all children, but is also associated with an increased risk for a variety of manifestations underlying end-organ injury and dysfunction that impose both immediate and potentially long-term morbidities and corresponding inherent elevations in healthcare costs. One of the major problems with the creation of valid algorithms aiming to stratify diagnostic and treatment prioritization lies in our current inability to predict and identify those children who are most at-risk for PSDB-induced adverse consequences. Thus, improved our understanding of the mechanisms governing phenotype variance in PSDB is essential. Here, we examine some of the potential underpinnings of phenotypic variability in PSDB, and further propose a conceptual framework aimed at facilitating the process of advancing knowledge in this frequent disorder.
1. Pediatric Sleep Disordered Breathing (PSDB)
Obstructive sleep apnea syndrome (OSA) is a common condition in children affecting up to 2–4% of all children with a peak incidence between 1 and 8 years of age (Kaditis, 2012)
Increased upper airway resistance or periodic obstructions of the upper airway during sleep lead to increased intrathoracic inspiratory pressures, intermittent oxyhemoglobin desaturations that are usually accompanied by PaCO2 elevations, and promote the disruption of sleep integrity as manifested by EEG arousals, ultimately enhancing the risk for excessive daytime sleepiness, as well as multiple other associated morbidities (see below)(Gozal, 2000; Gozal et al., 2010; Gozal and Kheirandish-Gozal, 2009).
2. Pathophysiological Mechanisms in PSDB
It is now clear that no single causative factor can be ascribed as solely responsible for the occurrence of OSA. However, the interplay between 4 major factors may in fact account for the vast majority, if not for the totality of the cases in otherwise healthy children. More specifically, interactions between craniofacial and anatomical factors, lymphoid tissue growth patterns, upper airway inflammation, and neuromuscular reflexes appear to underlie the emergence of OSA. Taken together, these elements lead to a pharyngeal airway of reduced dimensions that also exhibits an increased collapsibility, particularly during sleep. Indeed, awake children with OSA demonstrate the ability to compensate against the collapsible forces, primarily through recruitment of upper airway dilator muscles that maintain airway patency, and upper airway constrictors that enable increased upper airway rigidity (Arens and Marcus 2004). Upon sleep onset, these compensatory mechanisms are dampened, and the underlying upper airway collapsibility becomes manifest, leading to CO2 retention (resistive loading and obstructive alveolar hypoventilation), lowered PaO2, and increasing respiratory effort, all of which are resolved upon the occurrence of cortical or sub-cortical arousals, the latter promoting sleep fragmentation and non-restorative sleep. Cephalometric surveys of children with OSA have overall suggested the presence of selected alterations in the dimensions and vectors of several craniofacial skeletal structures (Kawashima et al., 2002; Marino et al., 2009). For example, children with OSA are more likely to display mandibular retrognathia, smaller maxillary dimensions, greater posterior facial height, reduced maxillary protrusion and growth, and shorter and flattened dental arches( Shintani et al., 1996). Kawashima et al. (2002) evaluated the dentofacial morphology and the pharyngeal airway space in preschool children with OSA, and found that children with OSA had mandibular retrognathia and narrower pharyngeal airway space, while Marino and collaborators (2009) evaluated the craniofacial cephalometric features of preschool children with OSA using measurements derived from lateral cephalometry, and identified skeletal Class II patterns with retrognathic mandible and increased skeletal divergency among children with OSA. In contrast, Arens and collaborators (2001) were unable to replicate these findings, whereby the mandibular width, length, and volume were not different from in children with OSA when compared to control subjects. In a subsequent study that employed 3-dimensional reconstruction techniques, no significant differences in mandibular size and shape were identified among 24 children with OSA and 24 matched controls (Schiffman et al., 2004). Thus, substantial variance appears to exist as far as the presence of altered maxillo-mandibular measures along with the growth patterns of other craniofacial structures, and less than optimal understanding is currently present as to who these elements interplay to contribute to upper airway growth and function.
Adenotonsillar hypertrophy has been considered as the most important driver of risk for the occurrence of PSDB. However, the mechanistic pathways underlying normal and abnormal follicular lymphoid tissue proliferation and hyperplasia remain hitherto unknown. Furthermore, our understandings of the inflammatory processes within the upper airway that contribute to OSA occurrence or result from the presence of PSDB are still extremely poorly understood. In recent years, it has become apparent that an array of environmental or tissue-derived stimuli may lead to accelerated proliferation of lymphadenoid tissues within the upper airway, and that such processes trigger an inflammatory response, the latter being most likely implicated in the pathophysiology of PSDB. Accordingly, alterations in local (i.e., upper airway) and systemic inflammatory markers have been consistently reported in children with OSA (Li et al., 2007; Gozal et al.,2008; Goldbart et al.,2006; Kaditis et al., 2009; Shen et al., 2011), thereby suggesting that inflammation is an important precipitating risk factor for OSA. For example, increased expression of cysteinyl leukotrienes and changes in glucocorticoid receptor expression and activity have been reported by several investigators in the adenoids and tonsils of children with OSA, and putatively assigned a mechanistic role in the induction of hyperplasia and hypertrophy of these upper airway tissues (Goldbart et al., 2004; Kaditis et al.,2008; Goldbart et al., 2005; Tsaoussoglou et al., 2012).
In addition, initial epidemiologic evidence implicates respiratory viruses and airway irritants, e.g., exposure to cigarette smoke, to increased propensity for development of adenotonsillar hypertrophy (Goldbart et al., 2007; Snow et al., 2009; Castaneda et al., 2013). Furthermore, the co-existence of inflammatory processes in the context of airway disorders such as rhinosinusitis, allergic rhinitis, or asthma is not only higher in PSDB as compared to the prevalence in the general population, but appears to affect the severity of PSDB as well, thereby, suggesting possible interactions between inflammatory mediators released in the airway by these conditions and promotion of proliferation of lymphatic tissues (Ersu et al., 2004; Kheirandish-Gozal et al., 2011; Malakasioti et al., 2011; Ross et al., 2012). Further confirming the above mentioned assumptions, we have previously shown that T cell lymphocytes are in a highly proliferative state in the tonsils of children with OSA, and display increased production of pro-inflammatory cytokines, such as IL-1α, TNF-α, and IL-6 (Kim et al., 2009). Taken together, it is very plausible that an array of environmental factors, such as viruses or air pollution, may alter the typical milieu of the upper airway, and lead to local inflammatory responses that then result in mucosal swelling, lymphadenoid tissue proliferation, and culminate in upper airway obstructive events during sleep. Application of unbiased bioinformatic approaches of the transcriptome to decipher potential pathways associated with adenotonsillar proliferation in PSDB revealed that processes underlying inflammatory signaling, immune regulation, and immune tissue growth and remodeling are distinctly dysregulated in upper airway lymphoid tissues of children with OSA (Khalyfa et al., 2010).
In addition to the robust evidence implicating anatomic abnormalities and inflammatory processes in pediatric OSA, alterations in neuromuscular reflexes may also contribute and promote the increased airway collapsibility that characterizes PSDB. As a corollary to such assumption, we should point out that children with markedly enlarged tonsils and adenoids may present a completely normal polysomnographic pattern, while the reverse, i.e., relatively small tonsils and adenoids may be accompanied by markedly severe OSA. Furthermore, most children with OSA do not snore during wakefulness, and surgical extirpation of adenotonsillar tissues is not always accompanied by complete resolution of OSA (Bhattacharjee et al., 2010). Taken together, alterations in neuromuscular reflexes may underlie an important component of the risk for OSA, and indeed pediatric patients with OSA universally show altered active and passive properties of the upper airway during sleep (Marcus et al., 2004; Gozal and Burnside, 2004). More recently, studies employing computational fluid dynamic techniques interfaced with upper airway imaging suggest that higher airflow resistance is consistently present in the upper airway of children with OSA (Xu et al., 2006; Mihaescu et al., 2008).
In summary, the integrated interactive presence of varying degrees of nasal flow resistance, craniofacial characteristics, altered tissue size or mechanical properties, and neuromuscular deficits are critical components of the equation that will resolve the level of OSA risk for any given child. A missing ingredient to this equation is the degree of genetic contribution to the risk, and this area has only recently begun to be explored, particularly after family-based studies revealed the clustering of OSA (Redline et al.,1992).
3. Morbid Consequences of OSA
It should not be surprising to anyone that the major impetus driving the investigation of any given condition is the fact that such condition promotes the occurrence of adverse complications. In the last 3 decades, an ever growing number of studies have revealed significant associations between PSDB and multiple end-organ morbidities, primarily affecting CNS, cardiovascular, and metabolic systems (Gozal and Kheirandish-Gozal, 2012). A cardinal observation pertaining to any of these associations is the irrefutable fact that at any given level of PSDB severity, there is a fraction that manifests no evidence of morbidity. Conversely even in the presence of extremely mild PSDB, there is a subset of children that exhibits prominent morbidity. One putative explanation for the presence of such phenotypic variance may reside in the underlying presence of genetic variance, i.e., the presence of single nucleotide polymorphisms in specific genes that may account for the differential end-organ susceptibility in PSDB (Figure 1).
Figure 1.
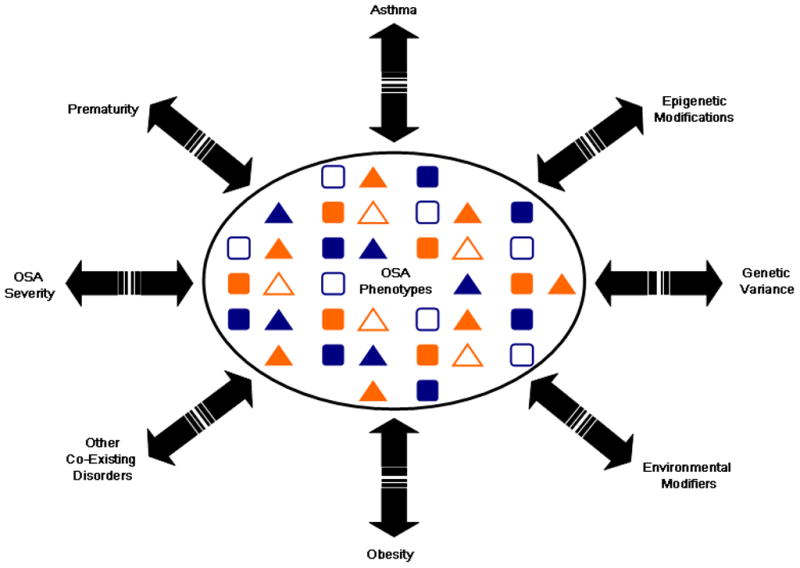
Schematic diagram illustrating the multiplicity of potential interactions between OSA and various factors that ultimately promote the occurrence of a great variety of phenotypes.
4. Genetic Determinants of Morbidity in PSDB
It is rather unfortunate that the field of genetic exploration of PSDB is really in its infancy. Indeed, only a limited number of reports on the associations between specific gene polymorphisms and PSDB-associated morbidity is currently available, but such preliminary findings further buttress the validity and the need for large population-based genome-wide association studies (GWAS) in this area.
4.1. Apolipoprotein E
Apolipoprotein E (ApoE) is a lipoprotein synthetized in the liver and brain that regulates components of cellular cholesterol deposition and transport. Apolipoprotein E (ApoE) exists as 3 alleles: ε2 (E2), ε3 (E3), and ε4 (E4), with the latter displaying reduced biological activity. Consequently, excess of ApoE4 allele frequency has been described in atherosclerosis, as well as in patients with memory disorders and late-onset familial and sporadic Alzheimer’s disease (AD) (Corder et al., 1993; Saunders et al., 1993; Sleegers et al., 2004; Baum et al., 2000).
The e4 allele is associated with reduced levels of ApoE, which alters cellular membrane stability and enhances the susceptibility to neuronal injury [59–60]. Interestingly, expression of the ε4 polymorphism was associated in some studies with increased prevalence of sleep-disordered breathing in adults, particularly before age 65 years ( Kadotani et al., 2001; Foley et al., 2001; Saarelainen et al., 1998; Larkin et al., 2006). Several years ago and then more recently, we examined whether reduced ApoE activity elicited increased vulnerability to some of the major constitutive elements that characterize OSA, namely intermittent hypoxia during sleep and sleep fragmentation. To this effect, both ApoE null mice and transgenic mice harboring the human ApoE-E4 allele demonstrated marked increases in the magnitude of cognitive deficits (Kheirandish et al., 2005; Kaushal et al., 2012). As a corollary of these animal model-based observations, an increased frequency of the ApoE4 allele emerged in children with OSA, as well as in children with OSA who manifest reduction in neurocognitive performance (Gozal et al., 2007; Kalra et al., 2008).
4.2. Uric Acid and OSAS in Different Populations
Several studies have suggested that significant differences exist in the frequency of morbidities among US and Greek children with PSDB, or even in the frequency of elevated markers of systemic inflammation (Gozal et al., 2012). To explore this issue further, Kaditis and colleagues examined urinary uric acid concentration patterns in Greek and US children suffering from OSA (Kaditis et al., 2010). In contrast with Greek children who exhibited increased uric acid urinary concentrations with increasing OSA severity, US children with OSA showed no association between OSA severity and uric acid. These studies further suggest that both genetic and environmental factors are most likely operational as far as the phenotypic manifestations of PSDB.
4.3. Sleepiness and TNF-α
TNF-α is one of the most important pro-inflammatory cytokines and has been strongly implicated in the regulation of sleep (Kruger, 2008). Among the multiple cell types that produce TNF-α, it can be synthesized and released in the brain by both neurons and glial cells. Both TNF receptors (p55 or TNFR1 and p75 or TNFR2) are constitutively and ubiquitously expressed in the nervous system (Pickering et al., 2005), and binding and downstream signaling of TNF-α underlie its biological effects in the CNS. TNF-α enhances slow wave sleep (SWS), and inhibition of TNF-α reduces the amount of spontaneous sleep. Exogenous injection of TNF-α induces sleepiness and elicits excess sleep in humans (Kruger, 2008), while sleep deprivation increases expression and biological activity of TNF-α in the brain. Excessive concentrations of TNF-α inhibit hippocampal long-term potentiation and impair cognitive function (Tancredi et al., 1992; Tobinick, 2009; Gozal et al., 2010). In adult patients with OSA, elevations in TNF-α serum concentrations are present, and similar observations have been reported in children with OSA, particularly when such children manifest excessive daytime sleepiness (EDS). Since at any level of OSA severity, only a fraction of children present with EDS, we sought to examine whether single nucleotide polymorphisms in the TNF gene may explain, at least in part, the dichotomy in the presence of EDS. We found that the presence of the TNF-α-308G gene polymorphism was closely associated with elevations in serum TNF-α levels, and that the presence of EDS was more likely to occur among those children with a positive TNF-α-308G gene polymorphism (Khalyfa et al., 2011). These findings have been recently substantiated by a meta-analysis (Huang et al., 2012).
4.4 Nicotinamide Adenine Dinucleotide Phosphate (NADPH) Oxidase, and Cognitive Function
Multiple lines of evidence primarily originating from animal models of OSA strongly support a major causative role of oxidative stress in the pathophysiology of end-organ injury. NADPH oxidase is a critically important enzyme that was initially discovered in phagocytic cells, but has since been shown as being expressed and constitutively active in a rather ubiquitous fashion (Jiang et al., 2011).
NADPH oxidase presents a pentameric structure with two membrane-bound subunits (gp91phox and p22phox) and three cytosolic subunits, namely p47phox, p67phox, and Rac, and these 5 sub-units form various functional heterodimers whose expression is heterotopically distributed in various cell types. A large number of polymorphisms has been identified for each of the genes involved in the NADPH oxidase complex, with some of these variants, e.g., 242 C>T or rs4673 in the p22phox subunit, being associated with hypertension, stroke, and ischemic heart disease (San José et al., 2008; Shimo-Nakanishi et al., 2004; Xaplanteris et al., 2010; Zalba et al., 2005).
Based on the extensive evidence implicating NADPH oxidase in the neuronal cell loss caused by intermittent hypoxia during sleep (Wang et al., 2010), a recent study revealed that 242 C>T polymorphism in the p22phox subunit explains a substantial proportion of the differences in cognitive function phenotype among children with OSA (Gozal et al., 2012).
4.5 Gene Variants in PSDB-Associated Metabolic Dysfunction
Fatty acid binding proteins (FABP) are an extensive family of molecules that serve as intracellular chaperones for lipids by coordinating cellular lipid responses, thereby emerging as critical players in metabolic regulation and in the inflammatory response (Zimmerman and Veerkamp, 2002). Adipocyte FABP, also termed FABP4, A-FABP, or aP2, was initially detected in mature adipocytes (Furuhashi et al., 2008; Maeda et al., 2005), and has been causally linked to a higher risk of metabolic disease. Indeed, circulating FABP4 levels correlate with the degree of metabolic dysfunction in children (Xu et al., 2007; Reinehr et al., 2007), and gene polymorphisms in the FABP4 gene have emerged as conferring a risk modifier effect on systemic inflammatory markers or in the risk for developing diabetes among obese children (Khalyfa et al., 2010). Since the FABP4 gene displays hypoxia response elements in its promoter, we explored whether FABP4 gene variants, could account for components of the variance in the frequency of metabolic dysfunction, in PSDB. Among the 11 FABP4 SNPs that were selected to cover the whole genomic sequence of FABP4, only the rs1054135 polymorphism was significantly more prevalent in PDSB-affected children, and manifested as increased FABP4 concentrations (Bhushan et al., 2011).
Other studies have examined metabolic variance in PSDB. In one of such studies, the insulin I/I genotype showed significantly more elevated insulin levels if PSDB was present among obese children (Carotenuto et al., 2009). The macrophage migration inhibitory factor gene (MIF) is a pro-inflammatory cytokine that has emerged as a mediator in multiple inflammatory disorders (Zernecke et al., 2008; Bernhagen et al., 2007). PSDB was not only associated with higher plasma MIF levels, but the MIF gene SNP rs10433310 polymorphism appeared to be significantly associated with cardiometabolic risk (Khalyfa et al., 2012).
In summary, the preliminary and relatively scarce evidence collected thus far supports the concept that similar to many other disorders, the phenotypic variation on PSDB can be explained in part by genotypic variance. There is no doubt that concerted efforts aiming at establishing extensive, well-phenotyped cohorts of children with and without PSDB, along with the concurrent availability of a biobank, will be critical to launch a valid GWAS exploration, such as to identify clusters of gene variants that may contribute to the end-organ morbidity of OSA.
5. PSDB Morbidity and the Epigenome
The compelling evidence presented thus far to illustrate the large variance in phenotypic expression of PSDB raises the possibility that among the genetic factors that underlie such variance, epigenetic modifications could be present among genes involved in inflammatory, vascular, neurocognitive or metabolic functions. Such changes in the epigenome would alter gene transcriptional activity, be potentially transmissible to subsequent generations, in the absence of any changes within the primary DNA sequence. Among the ever expanding list of molecular mechanisms involved in epigenetic alterations of DNA, DNA methylation, histone acetylation, and non-coding small RNA have been extensively studied, and constitute the major pathways (Delcuve et al., 2009). DNA methylation, primarily occurs at CpG dinucleotides within the genome or within CpG islands in the promoter regions of genes, and involves the enzymatic addition of a methyl group to the cytosine residue without changing the primary DNA sequence. Such modifications can alter the transcriptional activity of the gene, and result in altered gene expression, as well as affect the expression of genes in downstream-related networks (Yang et al., 2011).
In the context of PSDB, epigenetic alterations could develop as the direct effect of OSA, or could be merely representing pre-existing epigenetic changes that developed during preceding generations, during gestation, or during early post-natal life. As an initial effort to examine the hypothesis that changes in DNA methylation may be present in children with PSDB but with divergent systemic inflammatory responses, DNA was extracted from peripherally circulating monocytes of children with OSA who were matched for gender, ethnicity, BMI, and AHI, but who markedly differed in their serum levels of C-reactive proteins. Assessment of global DNA methylation levels among 24 major inflammatory-related genes followed by pyrosequencing-based confirmation of candidate genes revealed that the FOXP3 gene displayed significantly higher methylation levels in its promoter among children with high C-reactive protein serum levels (Kim et al., 2012). Since FOXP3 regulates the expression and conversion of T regulatory lymphocytes, it would be plausible to assume that reduced FOXP3 transcription would result in diminished T regulatory lymphocyte populations that would in turn lead to a shift of the immune system towards a preferential Th1 response. In corroboration of such hypothesis, T regulatory lymphocytes are indeed less abundant in a subset of children with PSDB, who also display a shift of their Th1/Th2 ratios toward Th1 predominance (Tan et al., 2013).
Analogously, abnormal endothelial cell function when assessed by post-occlusive hyperemic responses is only present in a subset of children with OSA (Bhattacharjee et al., 2012 ). It is now well established that the post-occlusive hyperemic response constitutes an endothelial nitric oxide synthase (eNOS)-dependent phenomenon. Furthermore, cell-specific expression of the eNOS gene is a highly regulated process mediated by epigenetic mechanisms that involve DNA methylation (Chan et al., 2004; Fish et al., 2005). Therefore, we recently examined whether changes in eNOS gene methylation in monocytes may accurately reflect divergent endothelial functional phenotypes in PSDB. Evidence for significant increases in the methylation of specific CpG sites within the promoter region of the eNOS gene emerged among those children with abnormal endothelial function (Kheirandish-Gozal et al., 2013).
Thus, the very preliminary and encouraging evidence available thus far appears to putatively ascribe a role for epigenetic mechanisms in the manifestations of PSDB-associated morbidities, and further justifies a much more expansive and deeper exploration of the epigenome in this context.
6. Conclusions
The existence of phenotype-genotype interactions in the context of PSDB appears to be irrefutable at this stage, in spite of the scarce cumulative evidence collected thus far in this context. It is highly likely that more in-depth characterization of such interactions will enable the formulation of a risk prediction signature panel for each of the morbidities associated with pediatric OSA. Identification of “vulnerable patients” based on the presence of specific gene variants, either in isolation or as panels, may allow for improved stratification of diagnostic screening and interventional algorithms aiming at minimizing the overall adverse consequences of pediatric OSA. The more recent evidence implicating epigenetic alterations in the variability of phenotype expression further attests to the complexity of this process, but concomitantly provides exciting prospects for improved understanding of PSDB and its consequences, and enable more individualized approaches to the diagnosis and treatment of children with OSA. For example, if indeed PSDB is the cause of epigenetic changes in a “morbidity”-associated gene of interest, such change may or may not reverse after conventional treatment of PSDB, and may require incremental therapies specifically targeting the epigenetic modification, such as to prevent PSDB from inducing organ morbidities many years after the disease resolved (i.e., preventing PSDB from being a childhood antecedent of adult disease). In this context, the role of lifestyle changes (exercise, diet) or specific medications (e.g., demethylating agents, histone modifiers) may be explored in high-risk patients.
Acknowledgments
Funding Sources: DG is supported by National Institutes of Health grants HL-65270, HL-086662, and HL-107160.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Arens R, Marcus CL. Pathophysiology of upper airway obstruction: a developmental perspective. Sleep. 2004;27:997–1019. doi: 10.1093/sleep/27.5.997. [DOI] [PubMed] [Google Scholar]
- Arens R, McDonough JM, Costarino AT, Mahboubi S, Tayag-Kier CE, Maislin G, Schwab RJ, Pack AI. Magnetic resonance imaging of the upper airway structure of children with obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 2001;164:698–703. doi: 10.1164/ajrccm.164.4.2101127. [DOI] [PubMed] [Google Scholar]
- Baum L, Chen L, Ng HK, Pang CP. Apolipoprotein E isoforms in Alzheimer’s disease pathology and etiology. Microsc Res Tech. 2000;50:278–81. doi: 10.1002/1097-0029(20000815)50:4<278::AID-JEMT5>3.0.CO;2-T. [DOI] [PubMed] [Google Scholar]
- Bernhagen J, Krohn R, Lue H, Gregory JL, Zernecke A, Koenen RR, Dewor M, Georgiev I, Schober A, Leng L, Kooistra T, Fingerle-Rowson G, Ghezzi P, Kleemann R, McColl SR, Bucala R, Hickey MJ, Weber C. MIF is a noncognate ligand of CXC chemokine receptors in inflammatory and atherogenic cell recruitment. Nat Med. 2007;13:587–96. doi: 10.1038/nm1567. [DOI] [PubMed] [Google Scholar]
- Bhattacharjee R, Kheirandish-Gozal L, Spruyt K, Mitchell RB, Promchiarak J, Simakajornboon N, Kaditis AG, Splaingard D, Splaingard M, Brooks LJ, Marcus CL, Sin S, Arens R, Verhulst SL, Gozal D. Adenotonsillectomy outcomes in treatment of obstructive sleep apnea in children: A multicenter retrospective study. Am J Resp Crit Care Med. 2010;182:676–683. doi: 10.1164/rccm.200912-1930OC. [DOI] [PubMed] [Google Scholar]
- Bhattacharjee R, Kim J, Alotaibi WH, Kheirandish-Gozal L, Capdevila OS, Gozal D. Endothelial dysfunction in children without hypertension: potential contributions of obesity and obstructive sleep apnea. Chest. 2012;141:682–91. doi: 10.1378/chest.11-1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhushan B, Khalyfa A, Spruyt K, Kheirandish-Gozal L, Capdevila OS, Bhattacharjee R, Kim J, Keating B, Hakonarson H, Gozal D. Fatty-acid binding protein 4 gene polymorphisms and plasma levels in children with obstructive sleep apnea. Sleep Medicine. 2011;12:666–71. doi: 10.1016/j.sleep.2010.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carotenuto M, Santoro N, Grandone A, Santoro E, Pascotto C, Pascotto A, Perrone L, del Giudice EM. The insulin gene variable number of tandem repeats (INSVNTR) genotype and sleep disordered breathing in childhood obesity. J Endocrinol Invest. 2009;32:752–5. doi: 10.1007/BF03346531. [DOI] [PubMed] [Google Scholar]
- Castaneda JL, Kheirandish-Gozal L, Gozal D, Accinelli RA The Pampa Cangallo IIA Research Group. Effect of reductions in biomass fuel exposure on symptoms of sleep apnea in children living in the Peruvian Andes: A preliminary field study. Pediatr Pulmonol. 2013 doi: 10.1002/ppul.22720. (in press) [DOI] [PubMed] [Google Scholar]
- Chan Y, Fish JE, D’Abreo C, Lin S, Robb GB, Teichert AM, Karantzoulis-Fegaras F, Keightley A, Steer BM, Marsden PA. The cell-specific expression of endothelial nitric-oxide synthase: A role for DNA methylation. J Biol Chem. 2004;279:35087–35100. doi: 10.1074/jbc.M405063200. [DOI] [PubMed] [Google Scholar]
- Corder EH, Saunders AM, Strittmatter WJ, Schmechel DE, Gaskell PC, Small GW, Roses AD, Haines JL, Pericak-Vance MA. Gene dose of apolipoprotein E type 4 allele and the risk of Alzheimer’s disease in late onset families. Science. 1993;261:921–3. doi: 10.1126/science.8346443. [DOI] [PubMed] [Google Scholar]
- Delcuve GP, Rastegar M, Davie JR. Epigenetic control. J Cell Physiol. 2009;219:243–50. doi: 10.1002/jcp.21678. [DOI] [PubMed] [Google Scholar]
- Ersu R, Arman AR, Save D, Karadag B, Karakoc F, Berkem M, Dagli E. Prevalence of snoring and symptoms of sleep-disordered breathing in primary school children in Istanbul. Chest. 2004;126:19–24. doi: 10.1378/chest.126.1.19. [DOI] [PubMed] [Google Scholar]
- Fish JE, Matouk CC, Rachlis A, Lin S, Tai SC, D’Abreo C, Marsden PA. The expression of endothelial nitric-oxide synthase is controlled by a cell-specific histone code. J Biol Chem. 2005;280:24824–24838. doi: 10.1074/jbc.M502115200. [DOI] [PubMed] [Google Scholar]
- Foley DJ, Masaki K, White L, Redline S. Relationship between apolipoprotein E epsilon4 and sleep-disordered breathing at different ages. JAMA. 2001;286:1447–1448. doi: 10.1001/jama.286.12.1447. [DOI] [PubMed] [Google Scholar]
- Furuhashi M, Fucho R, Görgün CZ, Tuncman G, Cao H, Hotamisligil GS. Adipocyte/macrophage fatty acid-binding proteins contribute to metabolic deterioration through actions in both macrophages and adipocytes in mice. J Clin Invest. 2008;118:2640–50. doi: 10.1172/JCI34750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldbart AD, Goldman JL, Li RC, Brittian KR, Tauman R, Gozal D. Differential expression of cysteinyl leukotriene receptors 1 and 2 in tonsils of children with obstructive sleep apnea syndrome or recurrent infection. Chest. 2004;126:13–18. doi: 10.1378/chest.126.1.13. [DOI] [PubMed] [Google Scholar]
- Goldbart AD, Veling MC, Goldman JL, Li RC, Brittian KR, Gozal D. Glucocorticoid receptor subunit expression in adenotonsillar tissue of children with obstructive sleep apnea. Pediatr Res. 2005;57:232–236. doi: 10.1203/01.PDR.0000150722.34561.E6. [DOI] [PubMed] [Google Scholar]
- Goldbart AD, Krishna J, Li RC, Serpero LD, Gozal D. Inflammatory mediators in exhaled breath condensate of children with obstructive sleep apnea syndrome. Chest. 2006;130:143–148. doi: 10.1378/chest.130.1.143. [DOI] [PubMed] [Google Scholar]
- Goldbart AD, Mager E, Veling MC, Goldman JL, Kheirandish-Gozal L, Serpero LD, Piedimonte G, Gozal D. Neurotrophins and tonsilllar hypertrophy in children with obstructive sleep apnea. Pediatr Res. 2007;62:489–494. doi: 10.1203/PDR.0b013e31814257ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gozal D. Obstructive sleep apnea in children. Minerva Pediatr. 2000;52:629–639. [PubMed] [Google Scholar]
- Gozal D, Burnside MM. Increased Upper Airway Collapsibility in Children with Obstructive Sleep Apnea during Wakefulness. Am J Respir Crit Care Med. 2004;169:163–167. doi: 10.1164/rccm.200304-590OC. [DOI] [PubMed] [Google Scholar]
- Gozal D, Capdevila OS, Kheirandish-Gozal L, Crabtree VM. Apolipoprotein E ε4 allele, neurocognitive dysfunction, and obstructive sleep apnea in school-aged children. Neurology. 2007;69:243–9. doi: 10.1212/01.wnl.0000265818.88703.83. [DOI] [PubMed] [Google Scholar]
- Gozal D, Capdevila OS, Kheirandish-Gozal L. Metabolic alterations and systemic inflammation in obstructive sleep apnea among nonobese and obese prepubertal children. Am J Respir Crit Care Med. 2008;177:1142–1149. doi: 10.1164/rccm.200711-1670OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gozal D, Kheirandish-Gozal L. Obesity and excessive daytime sleepiness in prepubertal children with obstructive sleep apnea. Pediatrics. 2009;123:13–8. doi: 10.1542/peds.2008-0228. [DOI] [PubMed] [Google Scholar]
- Gozal D, Khalyfa A, Capdevila OS, Kheirandish-Gozal L, Khalyfa AA, Kim J. Cognitive function in pre-pubertal children with obstructive sleep apnea: a modifying role for NADPH Oxidase p22 subunit gene polymorphisms? Antioxid Redox Signal. 2012;16:171–7. doi: 10.1089/ars.2011.4189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gozal D, Kheirandish-Gozal L, Bhattacharjee R, Kim J. C-reactive protein and obstructive sleep apnea syndrome in children. Frontiers in Bioscience. 2012;4:2410–22. doi: 10.2741/e553. [DOI] [PubMed] [Google Scholar]
- Gozal D, Kheirandish-Gozal L. Childhood obesity and sleep: relatives, partners, or both?--a critical perspective on the evidence. Ann N Y Acad Sci. 2012;1264:135–41. doi: 10.1111/j.1749-6632.2012.06723.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gozal D, Serpero LD, Kheirandish-Gozal L, Capdevila OS, Khalyfa A, Tauman R. Sleep measures and morning plasma TNF-alpha levels in children with sleep-disordered breathing. Sleep. 2010;33:319–25. doi: 10.1093/sleep/33.3.319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang J, Liao N, Huang QP, Xie ZF. Association between tumor necrosis factor-α-308G/A polymorphism and obstructive sleep apnea: a meta-analysis. Genet Test Mol Biomarkers. 2012;16:246–51. doi: 10.1089/gtmb.2011.0170. [DOI] [PubMed] [Google Scholar]
- Jiang F, Zhang Y, Dusting GJ. NADPH oxidase-mediated redox signaling: roles in cellular stress response, stress tolerance, and tissue repair. Pharmacol Rev. 2011;63:218–42. doi: 10.1124/pr.110.002980. [DOI] [PubMed] [Google Scholar]
- Kaditis AG, Ioannou MG, Chaidas K, Alexopoulos EI, Apostolidou M, Apostolidis T, Koukoulis G, Gourgoulianis K. Cysteinyl leukotriene receptors are expressed by tonsillar T cells of children with obstructive sleep apnea. Chest. 2008;134:324–331. doi: 10.1378/chest.07-2746. [DOI] [PubMed] [Google Scholar]
- Kaditis AG, Alexopoulos E, Chaidas K, Ntamagka G, Karathanasi A, Tsilioni I, Kiropoulos TS, Zintzaras E, Gourgoulianis K. Urine concentrations of cysteinyl leukotrienes in children with obstructive sleep-disordered breathing. Chest. 2009;135:1496–501. doi: 10.1378/chest.08-2295. [DOI] [PubMed] [Google Scholar]
- Kaditis AG, Gozal D, Snow AB, Kheirandish-Gozal L, Alexopoulos E, Varlami V, Papathanasiou AA, Capdevila OS, Bhattacharjee R, Kim J, Gourgoulianis K, Zintzaras E. Uric acid excretion in North American and Southeast European children with obstructive sleep apnea. Sleep Medicine. 2010;11:489–93. doi: 10.1016/j.sleep.2009.06.011. [DOI] [PubMed] [Google Scholar]
- Kaditis AG. Epidemiologic Aspects of Pediatric OSA around the World. In: Kheirandish-Gozal L, Gozal D, editors. Clinical guide to pediatric sleep medicine. Humana Press; 2012. pp. 279–290. [Google Scholar]
- Kadotani H, Kadotani T, Young T, Peppard PE, Finn L, Colrain IM, Murphy GM, Jr, Mignot E. Association between apolipoprotein E epsilon4 and sleep-disordered breathing in adults. JAMA. 2001;285:2888–90. doi: 10.1001/jama.285.22.2888. [DOI] [PubMed] [Google Scholar]
- Kalra M, Pal P, Kaushal R, Amin RS, Dolan LM, Fitz K, Kumar S, Sheng X, Guha S, Mallik J, Deka R, Chakraborty R. Association of ApoE genetic variants with obstructive sleep apnea in children. Sleep Med. 2008;9:260–5. doi: 10.1016/j.sleep.2007.05.001. [DOI] [PubMed] [Google Scholar]
- Kaushal N, Ramesh V, Gozal D. Human Apolipoprotein E4 targeted replacement in mice reveals increased susceptibility to sleep disruption and intermittent hypoxia. Am J Physiol (Regulatory, Integrative and Comparative Physiology) 2012;303:R19–R29. doi: 10.1152/ajpregu.00025.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawashima S, Peltomaki T, Sakata H, Mori K, Happonen RP, Ronning O. Craniofacial morphology in preschool children with sleep-related breathing disorder and hypertrophy of tonsils. Acta Paediatr. 2002;91:71–77. doi: 10.1080/080352502753457996. [DOI] [PubMed] [Google Scholar]
- Khalyfa A, Bhushan B, Hegazi M, Kim J, Kheirandish-Gozal L, Bhattacharjee R, Capdevila OS, Gozal D. Fatty-Acid Binding Protein 4 gene variants and childhood obesity: potential implications for insulin sensitivity and CRP levels. Lipids in Health and Disease. 2010;15(9):18. doi: 10.1186/1476-511X-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalyfa A, Gharib SA, Kim J, Dayyat E, Snow AB, Bhattacharjee R, Kheirandish-Gozal L, Goldman JL, Gozal D. Transcriptomic analysis identifies phosphatases as novel targets for adenotonsillar hypertrophy of pediatric OSA. Am J Resp Crit Care Med. 2010;181:1114–1120. doi: 10.1164/rccm.200909-1398OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalyfa A, Serpero LD, Kheirandish-Gozal L, Capdevila OS, Gozal D. TNF-a gene polymorphisms and excessive daytime sleepiness in pediatric obstructive sleep apnea. J Pediatr. 2011;158:77–82. doi: 10.1016/j.jpeds.2010.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalyfa A, Kheirandish-Gozal L, Sans Capdevila O, Bhattacharjee R, Gozal D. Macrophage migration inhibitory factor gene polymorphisms and plasma levels in children with obstructive sleep apnea. Pediatr Pulmonol. 2013 doi: 10.1002/ppul.22560. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kheirandish L, Row BW, Li RC, Brittian KR, Gozal D. Apolipoprotein E deficient mice exhibit increased vulnerability to intermittent hypoxia-induced spatial learning deficits. Sleep. 2005;28:1412–17. doi: 10.1093/sleep/28.11.1412. [DOI] [PubMed] [Google Scholar]
- Kheirandish-Gozal L, Dayyat EA, Eid NS, Morton RL, Gozal D. Obstructive sleep apnea in poorly controlled asthmatic children: effect of adenotonsillectomy. Pediatr Pulmonol. 2011;46:913–8. doi: 10.1002/ppul.21451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kheirandish-Gozal L, Khalyfa A, Gozal D, Bhattacharjee R, Wang Y. Endothelial dysfunction in children with obstructive sleep apnea is associated with epigenetic changes in the endothelial nitric oxide synthase gene. Chest. 2013 doi: 10.1378/chest.12-2026. ( in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Bhattacharjee R, Dayyat E, Snow A, Kheirandish-Gozal L, Goldman JL, Li RC, Serpero LD, Clair HB, Gozal D. Increased cellular proliferation and inflammatory cytokines in tonsils derived from children with obstructive sleep apnea. Pediatr Res. 2009;66:423–428. doi: 10.1203/PDR.0b013e3181b453e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim J, Bhattacharjee R, Khalyfa A, Kheirandish-Gozal L, Capdevila OS, Wang Y, Gozal D. DNA methylation in inflammatory genes among children with obstructive sleep apnea. Am J Respir Crit Care Med. 2012;185:330–8. doi: 10.1164/rccm.201106-1026OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krueger JM. The role of cytokines in sleep regulation. Curr Pharm Des. 2008;14:3408–16. doi: 10.2174/138161208786549281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larkin EK, Patel SR, Redline S, Mignot E, Elston RC, Hallmayer J. Apolipoprotein E and obstructive sleep apnea: evaluating whether a candidate gene explains a linkage peak. Genet Epidemiol. 2006;30:101–10. doi: 10.1002/gepi.20127. [DOI] [PubMed] [Google Scholar]
- Li AM, Hung E, Tsang T, Yin J, So HK, Wong E, Fok TF, Ng PC. Induced sputum inflammatory measures correlate with disease severity in children with obstructive sleep apnoea. Thorax. 2007;62:75–79. doi: 10.1136/thx.2006.060657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maeda K, Cao H, Kono K, Gorgun CZ, Furuhashi M, Uysal KT, Cao Q, Atsumi G, Malone H, Krishnan B, Minokoshi Y, Kahn BB, Parker RA, Hotamisligil GS. Adipocyte/macrophage fatty acid binding proteins control integrated metabolic responses in obesity and diabetes. Cell Metab. 2005;1:107–19. doi: 10.1016/j.cmet.2004.12.008. [DOI] [PubMed] [Google Scholar]
- Malakasioti G, Gourgoulianis K, Chrousos G, Kaditis A. Interactions of obstructive sleep-disordered breathing with recurrent wheezing or asthma and their effects on sleep quality. Pediatr Pulmonol. 2011;46:1047–54. doi: 10.1002/ppul.21497. [DOI] [PubMed] [Google Scholar]
- Marcus CL, Fernandes, Do Prado LB, Lutz J, Katz ES, Black CA, Galster P, Carson KA. Developmental changes in upper airway dynamics. J Appl Physiol. 2004;97:98–108. doi: 10.1152/japplphysiol.00462.2003. [DOI] [PubMed] [Google Scholar]
- Marino A, Malagnino I, Ranieri R, Villa MP, Malagola C. Craniofacial morphology in preschool children with obstructive sleep apnoea syndrome. Eur J Paediatr Dent. 2009;10:181–184. [PubMed] [Google Scholar]
- Mihaescu M, Murugappan S, Gutmark E, Donnelly LF, Kalra M. Computational modeling of upper airway before and after adenotonsillectomy for obstructive sleep apnea. Laryngoscope. 2008;118:360–2. doi: 10.1097/MLG.0b013e31815937c1. [DOI] [PubMed] [Google Scholar]
- Pickering M, Cumiskey D, O’Connor JJ. Actions of TNF-alpha on glutamatergic synaptic transmission in the central nervous system. Exp Physiol. 2005;90:663–70. doi: 10.1113/expphysiol.2005.030734. [DOI] [PubMed] [Google Scholar]
- Redline S, Tosteson T, Tishler PV, Carskadon MA, Millman RP. Studies in the genetics of obstructive sleep apnea. Familial aggregation of symptoms associated with sleep-related breathing disturbances. Am Rev Respir Dis. 1992;145:440–4. doi: 10.1164/ajrccm/145.2_Pt_1.440. [DOI] [PubMed] [Google Scholar]
- Reinehr T, Stoffel-Wagner B, Roth CL. Adipocyte fatty acid-binding protein in obese children before and after weight loss. Metabolism. 2007;56:1735–41. doi: 10.1016/j.metabol.2007.07.019. [DOI] [PubMed] [Google Scholar]
- Ross KR, Storfer-Isser A, Hart MA, Kibler AM, Rueschman M, Rosen CL, Kercsmar CM, Redline S. Sleep-disordered breathing is associated with asthma severity in children. J Pediatr. 2012;160:736–42. doi: 10.1016/j.jpeds.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saarelainen S, Lehtimäki T, Kallonen E, Laasonen K, Poussa T, Nieminen MM. No relation between apolipoprotein E alleles and obstructive sleep apnea. Clin Genet. 1998;53:147–8. doi: 10.1111/j.1399-0004.1998.tb02663.x. [DOI] [PubMed] [Google Scholar]
- San José G, Fortuño A, Beloqui O, Díez J, Zalba G. NADPH oxidase CYBA polymorphisms, oxidative stress and cardiovascular diseases. Clin Sci (Lond) 2008;114:173–82. doi: 10.1042/CS20070130. [DOI] [PubMed] [Google Scholar]
- Saunders AM, Schmader K, Breitner JC, Benson MD, Brown WT, Goldfarb L, Goldgaber D, Manwaring MG, Szymanski MH, McCown N. Apolipoprotein E epsilon 4 allele distributions in late-onset Alzheimer’s disease and in other amyloid-forming diseases. Lancet. 1993;342:710–1. doi: 10.1016/0140-6736(93)91709-u. [DOI] [PubMed] [Google Scholar]
- Schiffman PH, Rubin NK, Dominguez T, Mahboubi S, Udupa JK, O’Donnell AR, McDonough JM, Maislin G, Schwab RJ, Arens R. Mandibular dimensions in children with obstructive sleep apnea syndrome. Sleep. 2004;27:959–965. doi: 10.1093/sleep/27.5.959. [DOI] [PubMed] [Google Scholar]
- Shen Y, Xu Z, Shen K. Urinary leukotriene E4, obesity, and adenotonsillar hypertrophy in Chinese children with sleep disordered breathing. Sleep. 2011;34:1135–041. doi: 10.5665/SLEEP.1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimo-Nakanishi Y, Hasebe T, Suzuki A, Mochizuki H, Nomiyama T, Tanaka Y, Nagaoka I, Mizuno Y, Urabe T. Functional effects of NAD(P)H oxidase p22(phox) C242T mutation in human leukocytes and association with thrombotic cerebral infarction. Atherosclerosis. 2004;175:109–15. doi: 10.1016/j.atherosclerosis.2004.01.043. [DOI] [PubMed] [Google Scholar]
- Shintani T, Asakura K, Kataura A. Adenotonsillar hypertrophy and skeletal morphology of children with obstructive sleep apnea syndrome. Acta Otolaryngol Suppl. 1996;523:222–224. [PubMed] [Google Scholar]
- Sleegers K, Roks G, Theuns J, Aulchenko YS, Rademakers R, Cruts M, van Gool WA, Van Broeckhoven C, Heutink P, Oostra BA, van Swieten JC, van Duijn CM. Familial clustering and genetic risk for dementia in a genetically isolated Dutch population. Brain. 2004;127:1641–49. doi: 10.1093/brain/awh179. [DOI] [PubMed] [Google Scholar]
- Snow AB, Dayyat E, Montgomery-Downs HE, Kheirandish-Gozal L, Gozal D. Pediatric obstructive sleep apnea: a potential late consequence of respiratory syncitial virus bronchiolitis. Pediatr Pulmonol. 2009;44:1186–1191. doi: 10.1002/ppul.21109. [DOI] [PubMed] [Google Scholar]
- Tan HL, Gozal D, Wang Y, Bandla HPR, Bhattacharjee R, Kulkarni R, Kheirandish-Gozal L. Alterations in circulating T-cell lymphocyte populations in children with obstructive sleep apnea. Sleep. 2013 doi: 10.5665/sleep.2724. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tancredi V, D’Arcangelo G, Grassi F, Tarroni P, Palmieri G, Santoni A, Eusebi F. Tumor necrosis factor alters synaptic transmission in rat hippocampal slices. Neurosci Lett. 1992;146:176–8. doi: 10.1016/0304-3940(92)90071-e. [DOI] [PubMed] [Google Scholar]
- Tobinick E. Tumour necrosis factor modulation for treatment of Alzheimer’s disease: rationale and current evidence. CNS Drugs. 2009;23:713–25. doi: 10.2165/11310810-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Tsaoussoglou M, Lianou L, Maragozidis P, Hatzinikolaou S, Mavromati M, Orologas N, Panaghiotopoulou-Gartagani P, Rassidakis G, Balatsos NA, Chrousos G, Kaditis AG. Cysteinyl leukotriene receptors in tonsillar Band T-lymphocytes from children with obstructive sleep apnea. Sleep Med. 2012;13:879–85. doi: 10.1016/j.sleep.2012.03.010. [DOI] [PubMed] [Google Scholar]
- Xaplanteris P, Vlachopoulos C, Baou K, Vassiliadou C, Dima I, Ioakeimidis N, Stefanadis C. The effect of p22(phox) -930A/G, A640G and C242T polymorphisms of NADPH oxidase on peripheral and central pressures in healthy, normotensive individuals. Hypertens Res. 2010;33:814–8. doi: 10.1038/hr.2010.78. [DOI] [PubMed] [Google Scholar]
- Xu C, Sin S, McDonough JM, Udupa JK, Guez A, Arens R, Wootton DM. Computational fluid dynamics modeling of the upper airway of children with obstructive sleep apnea syndrome in steady flow. J Biomech. 2006;39:2043–2054. doi: 10.1016/j.jbiomech.2005.06.021. [DOI] [PubMed] [Google Scholar]
- Xu A, Tso AW, Cheung BM, Wang Y, Wat NM, Fong CH, Yeung DC, Janus ED, Sham PC, Lam KS. Circulating adipocyte-fatty acid binding protein levels predict the development of the metabolic syndrome: a 5-year prospective study. Circulatio. 2007;115:537–43. doi: 10.1161/CIRCULATIONAHA.106.647503. [DOI] [PubMed] [Google Scholar]
- Yang IV, Schwartz DA. Epigenetic control of gene expression in the lung. Am J Respir Crit Care Med. 2011;183:1295–1301. doi: 10.1164/rccm.201010-1579PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalba G, San José G, Moreno MU, Fortuño A, Díez J. NADPH oxidase-mediated oxidative stress: genetic studies of the p22(phox) gene in hypertension. Antioxid Redox Signal. 2005;7:1327–36. doi: 10.1089/ars.2005.7.1327. [DOI] [PubMed] [Google Scholar]
- Zernecke A, Bernhagen J, Weber C. Macrophage migration inhibitory factor in cardiovascular disease. Circulation. 2008;117:1594–1602. doi: 10.1161/CIRCULATIONAHA.107.729125. [DOI] [PubMed] [Google Scholar]
- Zimmerman AW, Veerkamp JH. New insights into the structure and function of fatty acid-binding proteins. Cell Mol Life Sci. 2002;59:1096–116. doi: 10.1007/s00018-002-8490-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


