Abstract
Background:
The minimal repair technique for sports hernias repairs only the weak area of the posterior abdominal wall along with decompressing the genitofemoral nerve. This technique has been shown to return athletes to competition rapidly. This study compares the clinical outcomes of the minimal repair technique with the traditional modified Bassini repair.
Hypothesis:
Athletes undergoing the minimal repair technique for a sports hernia would return to play more rapidly compared with athletes undergoing the traditional modified Bassini repair.
Methods:
A retrospective study of 28 patients who underwent sports hernia repair at the authors’ institution was performed. Fourteen patients underwent the modified Bassini repair, and a second group of 14 patients underwent the minimal repair technique. The 2 groups were compared with respect to time to return to sport, return to original level of competition, and clinical outcomes.
Results:
Patients in the minimal repair group returned to sports at a median of 5.6 weeks (range, 4-8 weeks), which was significantly faster compared with the modified Bassini repair group, with a median return of 25.8 weeks (range, 4-112 weeks; P = 0.002). Thirteen of 14 patients in the minimal repair group returned to sports at their previous level, while 9 of 14 patients in the Bassini group were able to return to their previous level of sport (P = 0.01). Two patients in each group had recurrent groin pain. One patient in the minimal repair group underwent revision hernia surgery for recurrent pain, while 1 patient in the Bassini group underwent hip arthroscopy for symptomatic hip pain.
Conclusion:
The minimal repair technique allows athletes with sports hernias to return to play faster than patients treated with the modified Bassini.
Keywords: sports hernia, minimal repair technique, modified Bassini technique, groin pain, femoral acetabular impingement
Sports hernias have gained recent attention as a cause of unresponsive groin pain in athletes.4 Groin pain caused by sports hernias can be disabling, and it has ended the careers of some high-level athletes.12 The exact cause of sports hernias is not completely known and remains heavily debated. A popular belief is that repetitive loading of the pubic symphysis during sports activities leads to symphyseal disc degeneration with loss of mechanical stability.5 The decreased stability of the pelvis leads to increased stress across the pelvic musculature and parasymphyseal tendon attachments, such as the rectus and adductors. Muschaweck and Berger described sports hernias as a weakness of the transversalis fascia portion of the posterior wall of the inguinal canal.14 This weakness in the pelvic floor can lead to localized bulging and compression of the genital branch of the genitofemoral nerve.13 Compression of the nerve may be a major source of pain in these patients.
Athletes with sports hernias who fail conservative treatment will often require surgical intervention to relieve their pain and allow them to return to play. Several procedures to treat sports hernias have been described in the literature and include primary pelvic floor repair without mesh,11,14 open anterior mesh repair,6,8 and laparoscopic mesh repair.7 A commonly used technique to treat sports hernias is the modified Bassini technique.3,16,19 This technique plicates the inferolateral border of the rectus abdominis fascia to the pubis and inguinal ligament and is designed to address the generalized weakness of the posterior abdominal wall.1 A newer minimal repair technique has been described by Muschaweck and Berger.14 This technique involves a minimal opening in the defect of the posterior abdominal wall, decompression of the genital branch of the genitofemoral nerve, and tension-free repair of the transversalis fascia. A theoretical advantage of the minimal repair technique is an earlier return to play. This study compares the minimal repair technique with the traditional modified Bassini technique for sports hernias. We hypothesized that the modified repair technique would lead to an earlier return to play with similar improvements in pain.
Materials and Methods
A retrospective study of patients undergoing surgical treatment for their sports hernia was performed after approval by the University of Virginia Internal Review Board. Between 1999 and 2009, 32 patients were diagnosed with sports hernia and underwent surgical repair by a single surgeon at the authors’ institution. Twenty-eight of these patients were available for follow-up (88%). The traditional repair group consisted of 14 of 17 patients (82% follow-up) who underwent the modified Bassini repair. The newer minimal repair group consisted of 14 of 15 patients (93% follow-up) who underwent Muschaweck and Berger’s minimal repair technique. All patients in the beginning of the study underwent the modified Bassini repair based on the senior surgeon’s experience and comfort. A change in the surgeon’s technique occurred after an expert in the minimal repair technique visited the authors’ institution. The indications for the surgery did not change with the change in technique.
Diagnosis
The diagnosis of sports hernia was based on the clinical history and physical examination. Each patient had the complaint of disabling groin pain associated with exertion, along with the clinical examination of pain with Valsalva and partial sit-up. Other physical findings included pain over the pubis and inguinal area to palpation. Imaging studies used to evaluate the patients included magnetic resonance imaging of the pelvis and ultrasound of the groin.
Surgical Procedures
In the modified Bassini repair, the aponeurosis of the transverse abdominis was sutured to the shelving edge of the inguinal ligament to reinforce the entire pelvic floor (Figure 1).2 The periosteum of the pubis was incised multiple times to aid in healing, followed by reapproximation of the external oblique over the spermatic cord.
Figure 1.
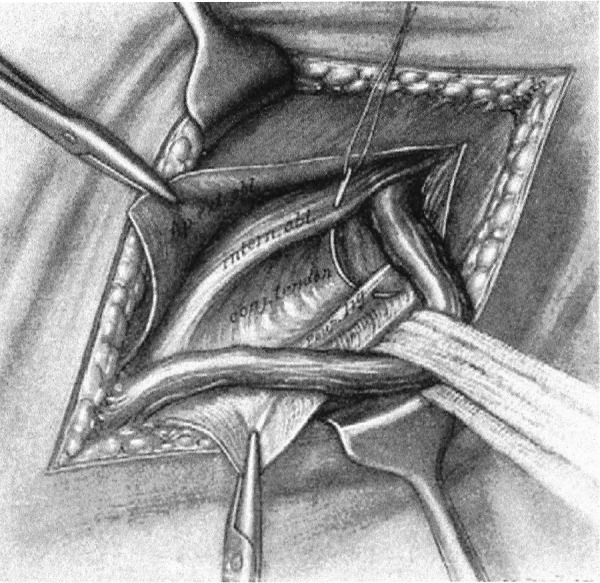
Modified Bassini technique: Through an oblique incision, the inguinal canal was opened and the spermatic cord was isolated. Typically, a complete tear of the transversalis fascia was not found. The floor of the inguinal canal was repaired with interrupted sutures placed through the internal oblique and transversalis fascia. Reprinted with permission from Banks and Cotlar.2
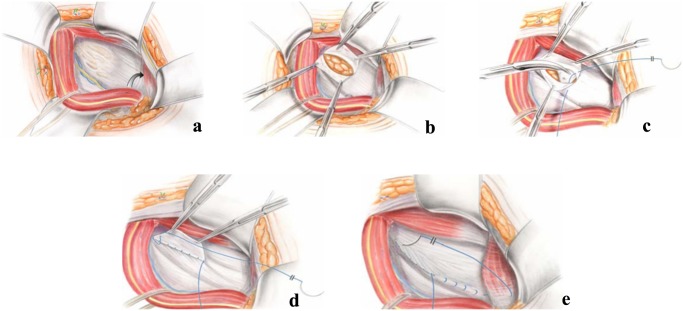
The minimal repair technique involved a smaller incision in which a tear in the external oblique fascia was often found and extended to expose the floor of the canal (Figure 2a).14 The genital branch of the genitofemoral nerve was identified, protected, and decompressed. The distinct weakness in the pelvic floor was repaired with sutures in running fashion instead of toward the inguinal ligament (Figures 2b to 2e). Only the damaged area of the posterior wall was incised for repair; any redundancy of the internal inguinal ring was also repaired. The external oblique muscle was reapproximated over the spermatic cord.
Figure 2.
Minimal repair technique: (a) A small tear in the external oblique was identified and extended to expose the posterior wall of the inguinal canal. (b) The weakness in the posterior floor of the inguinal canal was identified and opened. (c-e) The defect in the posterior wall was repaired in a running fashion. Reprinted with permission from Muschaweck and Berger.14
Rehabilitation
The same rehabilitation protocol was used for both surgical techniques. Division I and high school athletes had their progress monitored by their respective certified athletic trainers. Athletes without trainers were under the supervision of physical therapists. Rehabilitation for both the minimal repair group and modified Bassini group progressed as tolerated once the wound had healed appropriately (Table 1). Athletes initially began rehabilitation in the pool with standing hip adduction/abduction and partial squats and progressed to abdominal resistance exercises and running as tolerated. Sport-specific drills were included in the rehabilitation once the athlete tolerated running and advanced until the return to sports.
Table 1.
Rehabilitation protocol followed by both groupsa
| Phase | Activities |
|---|---|
| 1 | Rest and ice allowing incision to heal |
| Light stretching | |
| 2 | Isometric supine hip abduction and adduction |
| Resisted isometric hip flexion | |
| Stationary bike without resistance | |
| Pool standing hip abduction/adduction and squats | |
| 3 | Core stabilization |
| Standing hip 4-way with resistance | |
| Crunches to fatigue | |
| Prone hip internal and external rotation | |
| Bike and elliptical without resistance | |
| Continue pool training | |
| 4 | Wall squats (45°-90°) |
| Lunges | |
| Bike and elliptical with resistance | |
| Running in a single plane | |
| Box jumps | |
| Continue core strengthening | |
| 5 | Sports-specific activities |
| Sprinting, cutting, and twisting activities | |
| Progress resistance to tolerance | |
| Full return to sport |
The athletes were allowed progress as tolerated through the different phases. Athletic trainers or physical therapists monitored the progress of the athletes and determined when they could move to the next phase.
Radiographic Review
The anteroposterior radiographs of the pelvis were determined to be acceptable if comparable obturator foramen rotation was present and the coccyx was centered over and measured 2 to 4 cm above the pubic symphysis. On frog-leg lateral, the radiograph was acceptable if the anterior and posterior femoral head-neck junctions were clearly definable. Plain anteroposterior radiographs of the hips were examined for a “crossover” sign (Figure 3) and the frog-leg lateral radiographs for cam lesions by measuring the alpha angle (Figure 4). Cam lesions were identified by alpha angles greater than 55°, while pincer lesions were identified by a positive crossover sign.
Figure 3.
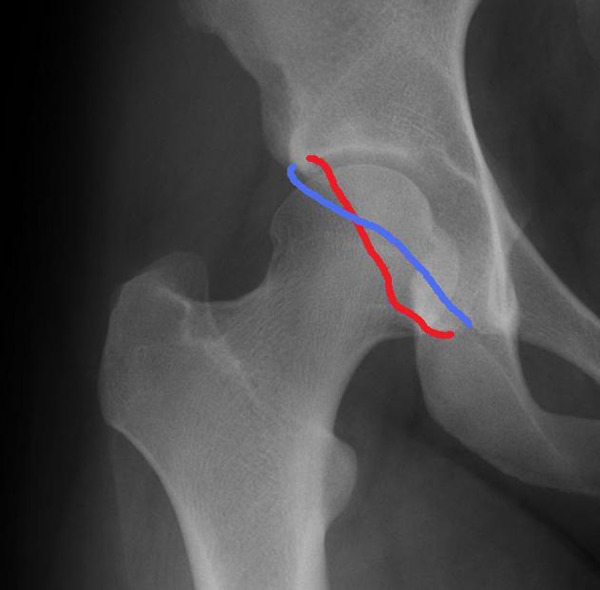
“Crossover” sign: Anteroposterior radiographs were used to determine the presence of a crossover sign, which is consistent with a pincer lesion. The anterior wall is outlined in red and the posterior acetabular wall in blue. Typically, the anterior wall remains medial to the posterior wall. If the anterior wall crosses the posterior wall and becomes more lateral than the posterior, this is considered a crossover sign.
Figure 4.
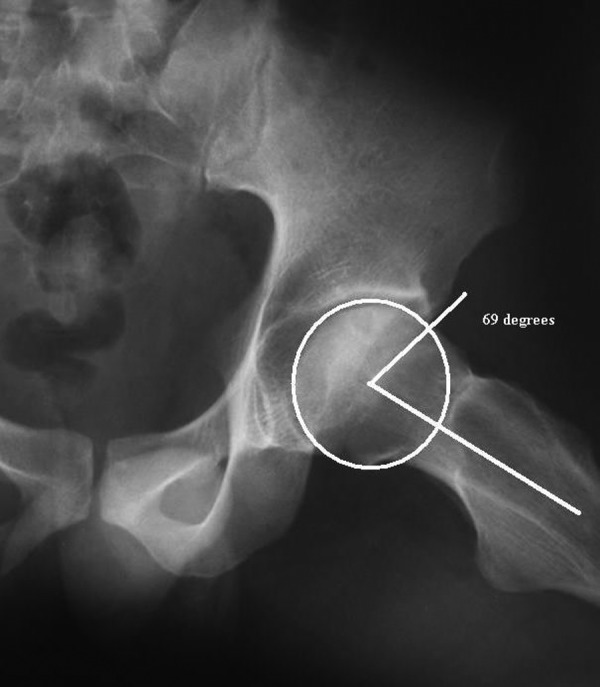
Measurement of alpha angle: The alpha angle on the frog-leg lateral films was measured by drawing a best-fit sphere around the femoral head. The point where the femoral head deviated away from this best-fit sphere was marked, and a line drawn from the center of the sphere to this point was drawn. The angle was measured between the longitudinal axis of the femoral neck and the line connecting the center of the sphere to the point where the head deviates from the best-fit sphere. An angle of 55° or more represented a cam lesion.
Chart Review and Phone Follow-up
Patient charts were reviewed for outcomes, including recurrent groin pain and the need for revision surgery. Patients were also contacted via telephone to complete a survey of return to sports, overall satisfaction with the procedure, pre- and postoperative Tegner activity scores, complications, current medication usage, and visual analog scale pain scores. All scores were determined at the time of phone follow-up. Patients were asked to complete a preoperative Tegner score18 by memory. The Tegner score was repeated to represent their current activity level. The clinical outcome of each patient was determined by both phone follow-up and chart review for recurrent groin pain and the need for further surgery.
Statistical Analysis
Data did not follow a normal distribution; therefore, a Mann-Whitney U test was used to compare the 2 surgical groups along with a chi-square test to compare binary data. A test was considered statistically significant if the P value was 0.05 or less.
Results
Demographics
The Bassini group consisted of 12 college and 2 high school male athletes. The minimal repair group was 11 college athletes, 2 high school athletes, and an active 32-year-old—all male patients. The median age was 25 years in the Bassini group and 22 years in the minimal repair group (P = 0.32). The median time between surgery and follow-up for the Bassini repair group was 54 months (range, 20-119 months) and 28 months (range, 24-43 months) for the minimal repair group (P = 0.06).
Hip examination revealed anterior impingement signs (decreased hip flexion, adduction, and internal rotation) in 2 of 14 (14%) patients in the Bassini group and 6 of 14 (43%) patients in the minimal repair group (P = 0.09). Thirteen of 14 patients in the Bassini group and 10 of 14 in the minimal repair group had magnetic resonance imaging findings of osteitis pubis or increased signal in the pelvic musculature. The most common magnetic resonance imaging finding of patients with sports hernias was edema at the symphysis pubis and the surrounding soft tissue (Figure 5). Ultrasound confirmed the diagnosis of sports hernia in 2 of 14 patients in the minimal repair group but was not used in any of the patients of the Bassini group. Plain radiographs, including anteroposterior and lateral frog-leg views, were available for all 28 participants in the study. At least 1 radiographic sign of femoral acetabular impingement (FAI) was found in 10 of 14 (71%) athletes in the modified Bassini group and 11 of 14 (79%) patients in the minimal repair group. Ten athletes in each group had cam lesions with the average alpha angle in the modified Bassini group of 64.2° ± 14.3° and 68.4° ± 20.3° in the minimal repair group (P = 0.39). A crossover sign was identified in 2 patients of the modified Bassini group and 3 patients of the minimal repair group.
Figure 5.
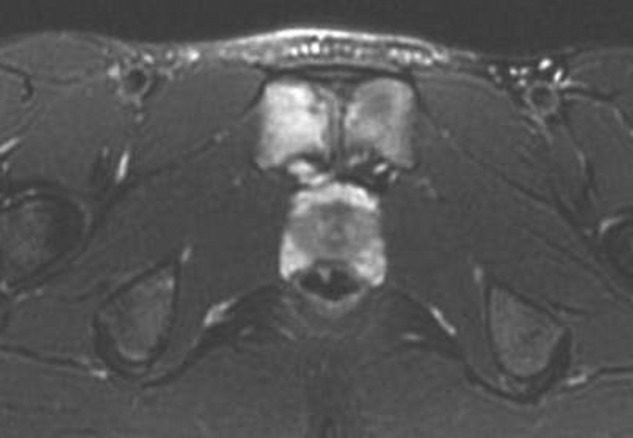
Pubic symphysis edema: T2 axial magnetic resonance imaging cut through the pubic symphysis. Bone edema is seen on both sides of the pubic symphysis.
Return to Sports
Thirteen of 14 athletes (92.8%) in the minimal repair group were able to return to their preinjury level of play, while 9 of 14 (64.3%) in the modified Bassini group were able to do so (P = 0.01). Median time to return to play was 5.6 weeks (range, 4-8 weeks) for the minimal repair group and 25.8 weeks (range, 4-112 weeks) for the modified Bassini group (P = 0.002). Time to return to play was not associated with the clinical symptoms of impingement (P = 0.49) or radiographic presence of FAI (P = 0.15). There was no association between the ability to return to play and the presence of anterior impingement signs (P = 0.47) or radiographic FAI (P = 0.74).
Outcomes
Two patients in each group developed recurrent groin pain. One patient in the minimal repair group required revision hernia surgery, while 1 patient in the Bassini group underwent hip arthroscopy for symptomatic FAI. Patients in the minimal repair group felt “back to normal” at a median of 5.9 weeks (range, 2-9 weeks), while those in the traditional repair group took a median of 19.9 weeks (range, 6-52 weeks) (P < 0.001). Return to work or school was significantly faster in the minimal repair group: 4.6 days (range, 3-14 days) versus 11.8 days (range, 1-30 days), respectively (P = 0.04). Ninety-three percent of the patients (13 of 14) undergoing the minimal repair technique were satisfied with the procedure, while 79% (11 of 14) undergoing the modified Bassini procedure were satisfied (P = 0.25). There were no significant differences in visual analog scale scores or change in Tegner scores from pre- to postoperative period between the 2 surgical techniques (Table 2). There were 2 minor complications in the minimal repair group and none in the traditional repair group. Both complications in the minimal repair group were superficial wound infections that were successfully treated with oral antibiotics.
Table 2.
Results of phone follow-up comparing the minimal repair technique group versus the modified Bassini group
| Minimal Repair | Bassini | P | |
|---|---|---|---|
| Weeks to return to sport | 5.6 | 25.6 | 0.002* |
| Returned to same sport level | 13 of 14 (92.8%) | 9 of 14 (64.3%) | 0.01* |
| Days to return to school/work | 4.6 | 11.8 | 0.04* |
| Satisfied with procedure | 13 of 14 (92.8%) | 11 of 14 (78.6%) | 0.25 |
| Weeks to feel normal | 5.9 | 19.9 | < 0.001* |
| Current visual analog scale | 1.1 | 1.5 | 0.82 |
| Previous Tegner score | 8.1 | 9.3 | 0.02* |
| Current Tegner score | 7.9 | 8.3 | 0.35 |
| Change in Tegner score | 0.733 | 1 | 0.85 |
P < 0.05.
Discussion
The results show that the minimal repair technique allows a more rapid return to sports compared with the traditional modified Bassini technique (5.6 vs 25.8 weeks, respectively). The same rehabilitation protocol was used for both techniques. Each patient was allowed to progress through one’s rehabilitation protocol as tolerated, and progress was monitored by the each individuals’ school athletic trainer or a trained physical therapist. The minimal repair technique involves a localized repair of an area of weakness in the pelvic floor and decompression of the genital branch of the genitofemoral nerve. The smaller incision and localized repair of the pelvic floor may have allowed the minimal repair group to accelerate its rehabilitation program. A significantly larger portion of the patients undergoing the minimal repair technique were able to return to their preinjury level of play compared with the modified Bassini technique. The ability to return to sports varies with the technique (Table 3).
Table 3.
Return to sport after sports hernia repaira
| Author | No. of Patients | Technique | Return to Sport, % | Time to Return, mo |
|---|---|---|---|---|
| Steele et al17 | 40 | Bassini | 77 | 4 |
| Meyers et al12 | 157 | Pelvic floor reconstruction | 97 | 3 (88%), 6 (96%) |
| Van Der Donckt et al19 | 41 | Bassini | 90 | 7 |
| Kumar et al9 | 35 | Open repair of posterior inguinal canal with mesh and repair of the external oblique aponeurosis | 93 | 6 |
| Polglase et al15 | 64 | Bassini repair or plication of the transversalis fascia | 94 | 6.9 |
| Ahumada et al1 | 12 | Open inguinal repair (9 with mesh) | 100 | 4 |
The percentage of patients who were able to return to sports and the time to return to sport varied depending on the technique used.
A sports hernia is considered to be a weakness in the posterior abdominal wall and not a true herniation into the inguinal canal. The weakness leads to the bulging of the posterior wall of the inguinal canal, which can compress surrounding structures, such as the genital branch of the genitofemoral nerve.14 The abnormality in the posterior wall is typically a circumscribed area with normal tissue surrounding the defect.14 The minimal repair technique repairs only the abnormal bulging section of the posterior wall. There is minimal dissection of uninjured tissue, leading to a smaller zone of injury and less tissue to heal after surgery. The modified Bassini repair requires dissection of not just abnormal tissue but also normal healthy tissue to repair the defect in the posterior abdominal wall. The increased dissection with the modified Bassini technique increases the soft tissue that must heal before the athlete can return to play. The decreased soft tissue dissection required by the minimal repair technique and less tissue volume to heal postoperatively may be a key to the shorter time to return to play. An important aspect to pain relief from the minimal repair technique is decompressing the genital branch of the genitofemoral nerve. By directly visualizing and decompressing the nerve, a major pain generator of the sports hernia may be removed. In addition, by repairing the fascial laxity of the posterior wall, stress is taken off the nerve and abdominal wall, thus decreasing the pain. These 2 components make the minimal repair technique effective in relieving pain in patients with sports hernias.14
An association between FAI and athletic pubalgia/sports hernias has been reported.17 Weir and colleagues found that 94% of patients with long-standing adductor-related groin pain had radiographic evidence of FAI.20 Our results show that 75% of our entire cohort had radiographic signs of FAI, while 29% had signs of anterior impingement. No difference was seen between the groups in the prevalence of radiographic FAI. The average alpha angle between the 2 groups was similar. The high prevalence of associated FAI and sports hernia may shed light on the cause of sports hernias in athletes. The exact association is not known but may be due to increased stresses across the groin musculature owing to biomechanical changes associated with FAI. Pelvic instability may play a role in the development of sports hernias. Cutting and twisting can lead to the breakdown of the disc of the pubic symphysis.5 The loss of the disc leads to decreased pelvic instability and increased stress on the surrounding tissue, such as tendinous attachments and pelvic musculature. In the setting of FAI, the decreased hip range of motion may be compensated for by movement elsewhere in the pubic symphysis. Pelvic instability can lead to increased stresses across the musculature of the groin and possibly to a sports hernia. Larson et al reviewed 37 hips in 31 patients presenting with both hip and groin pain.10 Sixteen patients were treated with sports hernia repair. Twenty-five percent of the patients treated surgically for sports hernia repair with associated FAI were able to return to sports, while 11 eventually required hip arthroscopy for continued intra-articular pain. In this study, nearly 79% of the patients were able to return to sports. Eight of the 28 patients had intra-articular symptoms, with 1 requiring hip arthroscopy for treatment of FAI. Two other patients, including 1 athlete in each group, required revision hernia surgery. Many of the study patients underwent hernia surgery before a full understanding of FAI. We did not specifically look for FAI in patients who had recurrent pain after hernia surgery, which may explain the low number of patients treated for FAI even though it was present.
Limitations to this study include its retrospective nature and data collection, as well as the varied time to follow-up for the 2 groups. Ideally, physical examination findings would be included with the 2-year follow-up. The time to follow-up was not similar between the 2 procedures because the 2 groups were not treated concurrently. The average follow-up for the modified Bassini was significantly longer than the follow-up for the minimal repair technique. Because of this, the 2 procedures were evaluated at different phases of recovery. The results of the modified Bassini may have deteriorated with time. The minimal repair may also see more failures as follow-up increases.
Conclusion
Patients undergoing a newer minimal repair technique for their sports hernia returned to sports faster compared with patients treated with the modified Bassini technique. The decreased soft tissue trauma from the minimal repair technique and nerve decompression may be the keys to the early return to sports in these patients. A high prevalence of FAI was seen in patients with sports hernias. Evaluation of FAI in patients with sports hernias should be routine.
Footnotes
The authors report no potential conflicts of interest in the development and publication of this manuscript.
References
- 1. Ahumada LA, Ashruf S, Espinosa-de-los-Monteros A, et al. Athletic pubalgia: definition and surgical treatment. Ann Plast Surg. 2005;55:393-396 [DOI] [PubMed] [Google Scholar]
- 2. Banks SB, Cotlar AM. Classic groin hernia repair . . . lest we forget. Curr Surg. 2005;62:249-252 [DOI] [PubMed] [Google Scholar]
- 3. Caudill P, Nyland J, Smith C, Yerasimides J, Lach J. Sports hernias: a systematic literature review. Br J Sports Med. 2008;42:954-964 [DOI] [PubMed] [Google Scholar]
- 4. Farber AJ, Wilckens JH. Sports hernia: diagnosis and therapeutic approach. J Am Acad Orthop Surg. 2007;15:507-514 [DOI] [PubMed] [Google Scholar]
- 5. Garvey JF, Read JW, Turner A. Sportsman hernia: what can we do? Hernia. 2010;14:17-25 [DOI] [PubMed] [Google Scholar]
- 6. Hemingway AE, Herrington L, Blower AL. Changes in muscle strength and pain in response to surgical repair of posterior abdominal wall disruption followed by rehabilitation. Br J Sports Med. 2003;37:54-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ingoldby CJ. Laparoscopic and conventional repair of groin disruption in sportsmen. Br J Surg. 1997;84:213-215 [DOI] [PubMed] [Google Scholar]
- 8. Irshad K, Feldman LS, Lavoie C, et al. Operative management of “hockey groin syndrome”: 12 years of experience in National Hockey League players. Surgery. 2001;130:759-764 [DOI] [PubMed] [Google Scholar]
- 9. Kumar A, Doran J, Batt ME, Nguyen-Van-Tam JS, Beckingham IJ. Results of inguinal canal repair in athletes with sports hernia. J R Coll Surg Edinb. 2002;47:561-565 [PubMed] [Google Scholar]
- 10. Larson CM, Pierce BR, Giveans MR. Treatment of athletes with symptomatic intra-articular hip pathology and athletic pubalgia/sports hernia: a case series. Arthroscopy. 2011;27:768-775 [DOI] [PubMed] [Google Scholar]
- 11. Meyers WC, Foley DP, Garrett WE, Lohnes JH, Mandlebaum BR. Management of severe lower abdominal or inguinal pain in high-performance athletes: PAIN (Performing Athletes With Abdominal or Inguinal Neuromuscular Pain Study Group). Am J Sports Med. 2000;28:2-8 [DOI] [PubMed] [Google Scholar]
- 12. Meyers WC, McKechnie A, Philippon MJ, et al. Experience with “sports hernia” spanning two decades. Ann Surg. 2008;248:656-665 [DOI] [PubMed] [Google Scholar]
- 13. Minnich JM, Hanks JB, Muschaweck U, Brunt LM, Diduch DR. Sports hernia: diagnosis and treatment highlighting a minimal repair surgical technique. Am J Sports Med. 2011;39:1341-1349 [DOI] [PubMed] [Google Scholar]
- 14. Muschaweck U, Berger L. Minimal repair technique of sportsmen’s groin: an innovative open-suture repair to treat chronic inguinal pain. Hernia. 2010;14:27-33 [DOI] [PubMed] [Google Scholar]
- 15. Polglase AL, Frydman GM, Farmer KC. Inguinal surgery for debilitating chronic groin pain in athletes. Med J Aust. 1991;155:674-677 [PubMed] [Google Scholar]
- 16. Preskitt JT. Sports hernia: the experience of Baylor University Medical Center at Dallas. Proc (Bayl Univ Med Cent). 2011;24:89-91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Steele P, Annear P, Grove JR. Surgery for posterior inguinal wall deficiency in athletes. J Sci Med Sport. 2004;7:415-421 [DOI] [PubMed] [Google Scholar]
- 18. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43-49 [PubMed] [Google Scholar]
- 19. Van Der Donckt K, Steenbrugge F, Van Den Abbeele K, Verdonk R, Verhelst M. Bassini’s hernial repair and adductor longus tenotomy in the treatment of chronic groin pain in athletes. Acta Orthop Belg. 2003;69:35-41 [PubMed] [Google Scholar]
- 20. Weir A, de Vos RJ, Moen M, Holmich P, Tol JL. Prevalence of radiological signs of femoroacetabular impingement in patients presenting with long-standing adductor-related groin pain. Br J Sports Med. 2011;45:6-9 [DOI] [PubMed] [Google Scholar]