Abstract
Context:
Cutaneous infections are common in wrestlers. Although many are simply a nuisance in the everyday population, they can be problematic to wrestlers because such infections may result in disqualification from practice or competition. Prompt diagnosis and treatment are therefore important.
Evidence Acquisition:
Medline and PubMed databases, the Cochrane Database of Systematic Reviews, and UpToDate were searched through 2012 with the following keywords in various combinations: skin infections, cutaneous infections, wrestlers, athletes, methicillin-resistant Staphylococcus aureus, skin and soft tissue infections, tinea corporis, tinea capitis, herpes simplex, varicella zoster, molluscum contagiosum, verruca vulgaris, warts, scabies, and pediculosis. Relevant articles found in the primary search, and selected references from those articles were reviewed for pertinent clinical information.
Results:
The most commonly reported cutaneous infections in wrestlers are herpes simplex virus infections (herpes gladiatorum), bacterial skin and soft tissue infections, and dermatophyte infections (tinea gladiatorum). The clinical appearance of these infections can be different in wrestlers than in the community at large.
Conclusion:
For most cutaneous infections, diagnosis and management options in wrestlers are similar to those in the community at large. With atypical presentations, testing methods are recommended to confirm the diagnosis of herpes gladiatorum and tinea gladiatorum. There is evidence to support the use of prophylactic medications to prevent recurrence of herpes simplex virus and reduce the incidence of dermatophyte infections in wrestlers.
Keywords: wrestlers; cutaneous infections; herpes gladiatorum, tinea gladiatorum; skin and soft tissue infections
Cutaneous infections affecting wrestlers frequently result in lost time from practice and competition and can substantially affect individual wrestler and team success. From 1988 to 2004, approximately 20% of practice-related sports medicine conditions in National Collegiate Athletic Association (NCAA) wrestlers leading to lost practice time involved cutaneous infections.5,63
Examination
In the NCAA, the sports medicine team typically performs screenings several times per week during practices and before all competitions according to published guidelines.63 Outside the NCAA, requirements for screening vary; however, the National Federation of State High School Associations (NFHS) Sports Medicine Advisory Committee (SMAC) has also published guidelines.65
A systematic head-to-toe examination is important for a thorough and efficient skin check. It is standard practice to have the wrestlers undress completely except for briefs and to position them in a well-lit area, standing with feet spread to shoulder width and arms abducted to 90° with thumbs pointed to the ceiling. Wrestlers should maintain a thumbs- up position to prevent hiding known skin lesions by rotating their arms as the examination progresses. Special attention should be given to the scalp because tinea can be easily missed and can contribute to wrestler-to-wrestler spread of this pathogen.51 If long briefs are worn, they should be raised above midthigh.
Return to Play
In general, an athlete may return to participation after treatment for the skin infection has been instituted and lesions are resolving. However, this varies with the type of infection. The SMAC of the NFHS65 and the NCAA64 have published return-to-play criteria (Table 1).
Table 1.
| Condition | National Collegiate Athletic Association | National Federation of State High School Associations |
|---|---|---|
| Herpes gladiatorum | No new lesions for 72 hours before the examination | No new vesicle formation and no swollen lymph nodes near the affected area |
| Resolution of all systemic symptoms in primary cases | Lesions must be well healed with well-adherent scabs | |
| All lesions must be dry and covered by a firm adherent crust; moist, active lesions cannot be covered to allow participation | If antiviral therapy used, withhold from wrestling for 5 days | |
| Treatment with appropriate systemic antiviral therapy for at least 120 hours before and at the time of competition | ||
| Bacterial skin and soft tissue infections | Completed 72 hours of antibiotic therapy | Completed 72 hours of antibiotic therapy |
| No moist or draining lesions | No moist or draining lesions, and lesion should have a well-adherent scab | |
| No new skin lesions for 48 hours before competition | Lesions should be covered with a bio-occlusive dressing until completely healed | |
| Moist or draining lesions cannot be covered for participation | ||
| Tinea gladiatorum | A minimum of 72 hours of topical antifungal therapy for tinea corporis | A minimum of 72 hours of systemic or topical antifungal therapy for tinea corporis |
| A minimum of 2 weeks of systemic antifungal therapy for tinea capitis | No specific recommendation for tinea capitis | |
| Lesions can be covered with a bio-occlusive dressing for return to competition after a period of adequate pharmacotherapy | Lesions can be covered with a bio-occlusive dressing for return to competition after a period of adequate pharmacotherapy | |
| Varicella zoster virus | Lesions must be covered with a firm adherent crust | Primary outbreaks require 10-14 days of systemic antiviral medication |
| No evidence of secondary bacterial infection | Secondary outbreaks require 5 days of systemic antiviral medication | |
| Lesions must be scabbed over with no discharge | ||
| No new lesions in preceding 48 hours | ||
| Molluscum contagiosum | Lesions must be curetted or removed | Lesions should be covered if prone to bleeding |
| Solitary or locally clustered lesions can be covered with a gas-permeable membrane and tape | ||
| Verruca vulgaris | Lesions must be “adequately covered” or curetted | Lesions should be covered if prone to bleeding |
| Facial lesions can be covered with a mask | ||
| Scabies | A negative microscopic skin prep before return to competition | |
| Pediculosis | Appropriate pharmacotherapy and completeness of response confirmed by examination |
Types of Infections
Herpes Gladiatorum
In wrestlers, herpes simplex virus (HSV) causes nongenital cutaneous infections, commonly termed herpes gladiatorum (HG).18,32,49,66,68,78 The usual culprit is HSV type 1, with HSV type 2 responsible for a minority of cases.
Description/Diagnosis
The annual estimated incidence of HG in NCAA wrestlers is 20% to 40%.49 From 1993 to 2004, HG was the most common reported cutaneous infection leading to lost practice time in NCAA wrestlers, accounting for 40.5% of all such infections.5 Numerous wrestling team and training camp epidemics have highlighted the substantial transmission potential of HSV.11,12,18,32
Transmission generally occurs primarily through skin-to-skin contact,11,49 for example, by exposure of abraded skin or mucosa to the lesions or mucocutaneous secretions of an infected individual.66
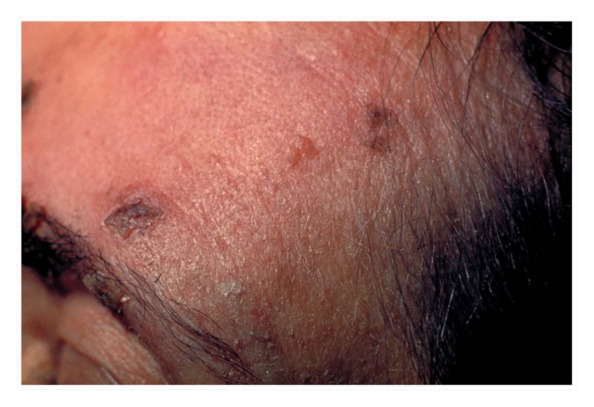
HSV replicates in skin cells and neurons and then travels to sensory dorsal root ganglia, where lifelong latency is established.79 An incubation period of 4 to 7 days from exposure to lesion appearance has been observed in a population of wrestlers during an epidemic.11 A prodrome of burning, tingling, or stinging may occur, and the infected individual may have a variety of systemic signs and symptoms.66,81 Numerous grouped painful vesicles or pustules on an erythematous base develop and then evolve into moist ulcerations, followed by crusted plaques (Figure 1). HG lesions generally appear 1 to 2 days after prodromal symptoms begin,66 and healing occurs within 10 days after the initial appearance without scarring.66
Figure 1.

Herpes gladiatorum lesions on the forehead of this wrestler appear as grouped vesicles and crusted plaques.
The distribution of HG lesions tends to be more diffuse than in typical HSV infections. HG lesions occur on body surface areas that frequently come in contact with an opponent, such as the face, head, neck, ears, and upper extremities,49,66,81 reinforcing the theory that transmission is primarily through skin-to-skin contact. Lesion location frequently reflects the wrestler’s handedness11; that is, lesions commonly occur on a wrestler’s dominant side, believed to result from the common “lock-up” position.11,49 Because HG lesions are often abraded during competition, lesions frequently have an atypical appearance81 and can be mistaken for many other cutaneous diseases.35
After the first outbreak resolves and latency is established, reactivation and recurrent outbreaks can be triggered by factors such as stress, fever, sun exposure, temperature extremes, trauma, or immunosuppression.78 Recurrences occur at the site of the initial outbreak (a fact that aids in diagnosis56), tend to be milder than the initial infection,66 and are of shorter duration.78
Careful examination of the eyes and oral and nasal cavities is imperative when HG is suspected because mucosal and ocular involvement by HSV can occur.40,47,49,78 Inoculation of the eyes was seen in an HG epidemic among high school wrestlers in Minnesota; approximately 8% developed ocular involvement.47 Ocular involvement is of particular concern because herpetic keratitis, if it arises, may cause corneal scarring and blindness.40,78 Inoculation of the oral mucosa causes gingivostomatitis.66 Autoinoculation while shaving can result in hair follicle lesions (herpetic sycosis),78 which can be indistinguisable from bacterial folliculitis.
Microbiological testing may be helpful in the diagnosis of HG.11,32 One study revealed that more than 90% of HG cases were misdiagnosed by physicians, who used viral culture only 18% of the time,32 suggesting both a role for microbiological testing and a lack of testing being performed in the community. Testing a lesion is best accomplished by unroofing an intact vesicle, absorbing the vesicular fluid, and scraping the lesion’s base with a swab78 that lacks calcium alginate (an inhibitor of HSV growth) and has a plastic or metal shaft (to avoid cell toxicity in cultures potentially caused by wood).60 Diagnostic yield is highest from samples obtained within the first 24 to 48 hours.78 Viral culture has variable sensitivity, depending on the state of the lesion at the time of sampling and sampling technique (52% to 93% for vesicles, 41% to 72% for ulcers, and 19% to 27% for crusted lesions39) and a near 100% specificity.39 Real-time polymerase chain reaction is a substantially more sensitive option, with specificity comparable with that of culture39,74,78 (sensitivity and specificity of 98% to 100%74), but its utility is limited by substantially higher cost and availability. The choice of diagnostic testing should be guided by the provider’s expertise and by test availability; lesions should be sampled as early as possible.
Treatment
The cornerstone of HG management is the early detection and isolation of infected wrestlers. Treatment of an acute HG eruption includes oral antiviral medications (Table 2), started within 24 hours of developing symptoms.8,13,19,31 In a placebo-controlled study, valacyclovir (500 mg twice daily for 7 days) was effective in decreasing the duration of visible HG lesions and viral shedding during recurrent outbreaks.13
Table 2.
| Indication | Medication | Dosing Regimen |
|---|---|---|
| Primary infection | ||
| Adult | Acyclovir | 400 mg, PO, 3×/d, or 200 mg, PO, 5×/d for 7-10 d |
| Famciclovir | 250 mg, PO, 3×/d for 7-10 d | |
| Valacyclovir | 1000 mg, PO, 2×/d for 7-10 d | |
| ≤ 12 years old | Acyclovir | 40-80 mg/kg daily in 3 divided doses for 5-10 d (max, 1 g/d) |
| Valacyclovir | 20 mg/kg, PO, 3×/d for 5-10 d | |
| Recurrent infection | ||
| Adulta | Acyclovir | 800 mg, PO, 2×/d for 5 d, or 400 mg, PO, 3×/d for 5 d |
| Famciclovir | 125 mg, PO, 2×/d for 5 d, or 1 g, PO, 2× for 1 d | |
| Valacyclovir | 1 g, PO, daily for 5 d, or 500 mg, PO, 2×/d for 3-7 d | |
| Prophylaxis | ||
| > 12 years oldb | Acyclovir | 400 mg, PO, 2×/d |
| Famciclovir | 250 mg, PO, 2×/d | |
| Valacyclovir | 500 mg, PO, once daily, or 1 g, PO, once daily | |
PO, orally.
Same as for primary infection, ≤ 12 years old.
Insufficient evidence to recommend use of prophylaxis in children < 12 years old.
The SMAC of the NFHS65 and the NCAA64 recommend consideration of season-long oral antiviral prophylaxis for wrestlers with a history of an HG outbreak (SORT B). A double-blind study found that oral valacyclovir was significantly more effective than a placebo for prophylaxis against acute HG reactivation in wrestlers10; effective doses were 500 mg per day for wrestlers with a history of more than 2 years and 1000 mg per day for wrestlers with a history of less than 2 years. Valacyclovir prophylaxis has not been associated with substantial side effects.16,36
Bacterial Infections
In wrestlers, bacterial skin and soft tissue infections (SSTIs) are spread by physical contact and shared equipment, develop in abraded skin, and are frequently competition-disqualifying.
Description/Diagnosis
From 1993 to 2004, SSTIs were the second-most-common reported cutaneous infections leading to lost practice time in NCAA wrestlers, accounting for 24.9% of all such infections.5 Community-associated methicillin-resistant Staphylococcus aureus (MRSA) SSTIs are being reported with increasing frequency in wrestlers and athletic populations in general.22-24,58
SSTIs are categorized according to the layers of skin involved and whether or not they are complicated, that is, involve signs of systemic toxicity, a widespread or rapidly expanding area of involvement, disproportionate pain, skin sloughing, cutaneous bleeding, or skin crepitus.20
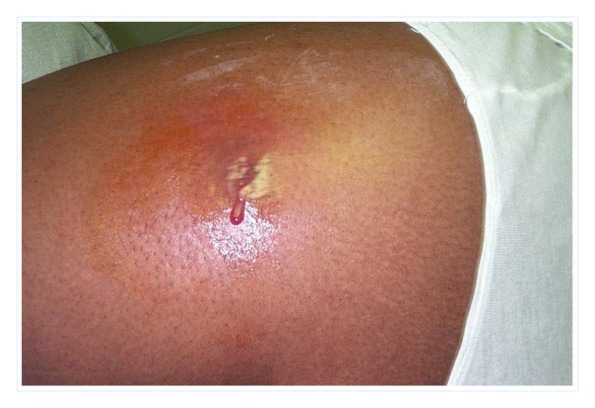
Erysipelas and cellulitis are nonpurulent, diffuse SSTIs caused mainly by staphylococci or streptococci. Erysipelas is commonly caused by beta-hemolytic streptococci.20 It involves the superficial layers of the dermis and presents as sharply demarcated, intensely red plaques on the skin (Figure 2).15 Cellulitis is typically caused by streptococci or staphylococci20 in the deeper dermis and subcutaneous tissue15 and presents as erythematous patches without discrete borders and underlying subcutaneous edema (Figure 3).
Figure 2.

Erysipelas presents as sharply demarcated red plaques. Photo courtesy of Poupou l’quourouce.
Figure 3.

Cellulitis on the leg with erythema and subcutaneous edema. Photo courtesy of Colm Anderson.
Bacterial folliculitis and furuncles are often caused by S. aureus, occurring when hair follicles become infected.81 Folliculitis presents as perifollicular erythematous papules or pustules in areas exposed to friction (Figure 4).81 A furuncle is a purulent infection extending from a follicle into the dermis and subcutaneous tissues, presenting as an inflammatory nodule (Figure 5).75 If multiple adjacent infected follicles coalesce, a carbuncle forms.75 Furuncles and carbuncles may present with spontaneous drainage from individual follicles.
Figure 4.

Folliculitis in the axilla with multiple perifollicular erythematous papules and pustules.
Figure 5.

A furuncle with a central follicular pustule surrounded by an inflammatory nodule.
The diagnosis of an SSTI is usually clinical. Cultures of uncomplicated SSTIs infrequently alter management and are therefore not routinely recommended.20 Consensus guidelines recommend cultures when there is a purulent lesion and at least 1 of the following features: treatment with antibiotics, signs of systemic toxicity, multiple or large lesions, a bite as the cause, association with water exposure, lack of response to initial treatment, or occurrence during a suspected outbreak.75 Culturing when antibiotics are used allows sensitivities to be determined, which can guide antibiotic choices in the case of a poor response to the initial antibiotic.
Methicillin-Resistant Staphylococcus aureus Infection
MRSA SSTIs frequently manifest as rapidly progressive and frequently purulent lesions (Figure 6). Although the lesion caused by MRSA is frequently described as a “spider bite” at onset,20,80,81 there are no specific signs to distinguish community-acquired MRSA SSTIs from other SSTIs.20,62
Figure 6.
Methicillin-resistant Staphylococcus aureus cutaneous abscess with spontaneous drainage. Photo courtesy of the Centers for Disease Control and Prevention/Bruno Coignard/Jeff Hageman.
Impetigo
Impetigo is an SSTI caused by staphylococci or streptococci with a clinically unique appearance. The hallmark of impetigo is multiple “honey-crusted” lesions, usually occurring on the face or extremities in clusters. In the bullous form, lesions start as vesicles that enlarge to form flaccid purulent bullae that eventually rupture, leaving thin brown crusts (Figure 7).75 In the nonbullous form, individual vesicles surrounded by erythema progress to pustules and then thick, adherent yellow crusts.75
Figure 7.
Bullous impetigo on the arm with vesicles, bullae, and adherent brown crusts. Photo courtesy of the Centers for Disease Control and Prevention.
Treatment
It is imperative that affected wrestlers be isolated until adequate treatment is administered. Strict hygiene of affected wrestlers is indicated to prevent spread of pathogens.
SSTIs are generally treated with systemic antibiotics (Table 3),20,75 with the exception of localized, uncomplicated abscesses that can be managed with incision and drainage alone20,62 and areas of limited impetigo or folliculitis that can be treated with topical agents.
Table 3.
| Indication | Medication | Dosage | Comments |
|---|---|---|---|
| Impetigo | |||
| Adult | Dicloxacillin | 250 mg, PO, 4× daily | |
| Cephalexin | 250 mg, PO, 4× daily | ||
| Clindamycin | 300-400 mg, PO, 3× daily | ||
| Erythromycin | 250 mg, PO, 4× daily | Some Staphylococcus and Streptococcus strains may be resistant | |
| Mupirocin 2% ointment | Apply 3× daily | For areas of limited involvement | |
| Children | Dicloxacillin | 12 mg/kg/d, PO, 4 divided doses | |
| Cephalexin | 25 mg/kg/d, PO, 4 divided doses | ||
| Clindamycin | 10-20 mg/kg/d, PO, 3 divided doses | ||
| Erythromycin | 40 mg/kg/d, PO, 4 divided doses | Some Staphylococcus and Streptococcus strains may be resistant | |
| Mupirocin 2% ointment | Apply 3× daily | For areas of limited involvement | |
| Skin and soft tissue infection: MSSA | |||
| Adult | Dicloxacillin | 500 mg, PO, 4× daily | |
| Cephalexin | 500 mg, PO, 4× daily | ||
| Doxycycline | 100 mg, PO, 2× daily | ||
| Clindamycin | 300-450 mg, PO, 3× daily | ||
| Children | Dicloxacillin | 25 mg/kg/d, PO, 4 divided doses | |
| Cephalexin | 25 mg/kg/d, PO, 4 divided doses | ||
| Clindamycin | 10-20 mg/kg/d, PO, 3 divided doses | ||
| Skin and soft tissue infection: MRSA | |||
| Adult | Doxycycline | 100 mg, PO, 2× daily | |
| Trimethoprim-sulfamethoxazole | 1 or 2 double-strength tablets, PO, 2× daily | ||
| Clindamycin | 300-450 mg, PO, 3× daily | Possible cross-resistance and emergence of resistance in erythromycin-resistant strains, and possible inducible MRSA resistance | |
| Linezolid | 600 mg, PO, 2× daily | ||
| Mupirocin 2% cream | Apply 3× daily | For folliculitis with an area of limited involvement | |
| Children | Trimethoprim-sulfamethoxazole | 8-12 mg/kg/d, PO, 2 divided doses | |
| Clindamycin | 10-20 mg/kg/d, PO, 3 divided doses | Possible cross-resistance and emergence of resistance in erythromycin-resistant strains, and possible inducible MRSA resistance | |
| Linezolid | 10 mg/kg/d, PO, 2 divided doses | ||
| Mupirocin 2% cream | Apply 3× daily | For folliculitis with an area of limited involvement | |
MRSA, methicillin-resistant Staphylococcus aureus; MSSA, methicillin-susceptible S. aureus; PO, orally.
A recent systemic review found no difference between penicillin and cephalosporin or among different generations of cephalosporin in the treatment of cellulitis and erysipelas.50 For isolated cellulitis (no associated abscess) when MRSA is not suspected, 5 to 10 days of empiric therapy covering beta-hemolytic streptococci is recommended,55 with an oral beta-lactam antibiotic the appropriate first-line choice. Poor response to initial treatment or signs of systemic toxicity should alert the physician to the possibility of MRSA. Oral antibiotics effective against community-acquired MRSA include trimethoprim-sulfamethoxazole, tetracycline, clindamycin, and linezolid.20,55 Cases involving signs of systemic toxicity, rapidly progressive or expansive areas of involvement, or failure to improve after 48 hours of oral antibiotic therapy should be considered for hospitalization and intravenous antibiotic therapy. When an SSTI is located over joints, the examination should evaluate for septic bursitis or a septic joint.
For impetigo, oral and topical medications are available (Table 3),20,75 which appear to have equal treatment efficacy.38,54,75 In a recent systematic review, oral penicillin was found to be inferior to erythromycin and cloxacillin.54 Typically, topical therapy is reserved for cases with a small number of lesions and limited area of involved skin.
Most purulent SSTIs should undergo incision and drainage,62 followed by probing of the wound cavity to break up loculations.75 The only exception may be if adequate spontaneous drainage is apparent. For small furuncles, application of moist heat may facilitate drainage, which generally resolves the problem.75
Any purulent lesion in which MRSA is suspected should be treated with incision and drainage.62,75 The decision to follow incision and drainage with antibiotics in the case of suspected MRSA is less clear. In 2 randomized placebo-controlled studies, antibiotics used after incision and drainage of purulent uncomplicated MRSA infections did not significantly reduce treatment failures within 7 days.70,73 However, 1 study73 did show a statistically significant decrease in subsequent MRSA lesions within 30 days when oral trimethoprim-sulfamethoxazole was given after incision and drainage. Current Infectious Disease Society of America guidelines recommend antibiotic treatment after incision and drainage of suspected MRSA lesions for patients with severe or extensive disease, rapid progression of associated cellulitis, signs of systemic toxicity, lesions that are difficult to drain (eg, in groin or axilla), and a lack of response to incision and drainage alone.55
Decolonization of MRSA carriers has a limited role. Although a number of whole-body antimicrobial decolonization protocols exist, typically involving topical antimicrobial scrubs and nasal mupirocin,9,34,57 available evidence for the overall utility and correct setting for these protocols is limited.20,59,80 Decolonization can be considered for individuals with recurrent MRSA infection, for close contacts who are culture-confirmed carriers, and in a MRSA outbreak in the training room setting.44,55,65 Decolonization can be a daily body wash with chlorhexidine (2% to 4% solution) plus mupirocin (2% ointment) applied to each nare 2 to 3 times daily for 5 to 10 days.44
Dermatophyte Infections
Dermatophyte skin infections, a common nuisance in wrestlers, are generally benign but frequently competition-disqualifying. Trichophyton tonsurans accounts for most outbreaks in wrestlers.2
Description/Diagnosis
Dermatophytes infect the outer layers of the epidermis. Infection of glabrous skin is tinea corporis. Infection of scalp hair and hair follicles is tinea capitis (tinea capitis gladiatorum35,48). In wrestlers, these infections are collectively termed tinea gladiatorum (TG)28 or tinea corporis gladiatorum.2
From 1993 to 2004, TG was the third-most-common reported cutaneous infection leading to lost practice time in NCAA wrestlers, accounting for 22.1% of all such infections.5 One study found that 60% of college wrestlers and 52% of high school wrestlers suffered at least one TG infection during the course of a season.81 Numerous epidemics have occurred in wrestlers,17,28,33,35,37,48,67 who appear to serve as asymptomatic reservoirs for the pathogen (reported prevalence, 20% to 24%).3,46
Transmission occurs through arthrospores with extended survival time shed in skin scales.51 TG infections are primarily transmitted via person-to-person contact.2,37,51 An asymptomatic carrier state plays a role in the transmission of TG,46,51,52,69 with the scalp being a likely source.51
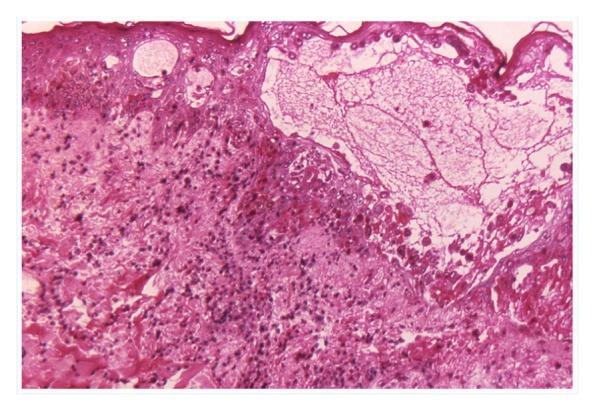
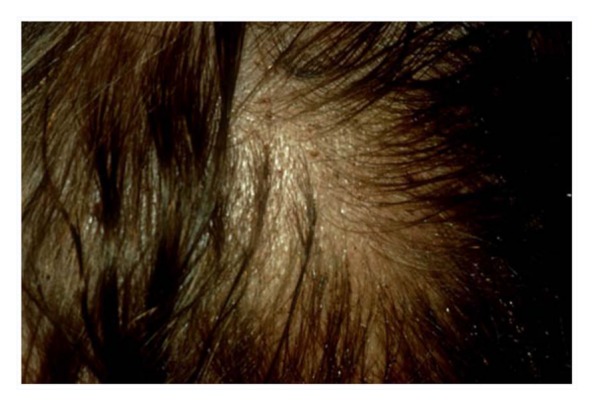
Tinea capitis caused by T. tonsurans begins with sharply demarcated, erythematous, scaly patches that spread outward (Figure 8). Over weeks to months, erythema fades, and hairs break off flush with the scalp, leaving a patch of alopecia with follicular plugs that create a characteristic “black dot” appearance.41 In some cases, inflammation and painful regional lymphadenopathy occur.41
Figure 8.
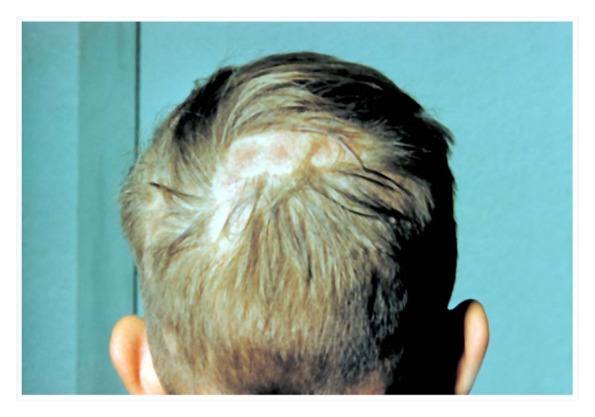
Tinea capitis presents as a sharply demarcated, erythematous, scaly patch. This lesion has progressed to alopecia. Photo courtesy of the Centers for Disease Control and Prevention.
Local pruritus, erythema, and burning typically accompany tinea corporis.41,51 Typically, these lesions are sharply demarcated, erythematous, scaly, annular plaques or papules with raised borders and central clearing (Figure 9).2,51,81 The lesion spreads outward as the center clears.41 In TG, a typical tinea appearance is frequently absent2,51,81 because wrestlers often present early during routine skin checks and because lesions can be abraded during competition (Figure 10).
Figure 9.

Tinea gladiatorum lesions on the neck of this wrestler with a typical appearance: erythematous annular plaques with central clearing and surface scale at the periphery of the lesion.
Figure 10.

An abraded tinea gladiatorum lesion on the arm lacks a typical appearance.
With a typical appearance, a clinical diagnosis is possible. It is important to examine the scalp carefully because early lesions can be subtle and frequently asymptomatic.41 However, because of the atypical appearance in wrestlers, diagnostic testing is recommended.
Diagnosis is confirmed with potassium hydroxide preparation or culture (sensitivity, 88%; specificity, 95%).51 For tinea capitis, samples are obtained by epilating hairs. The presence of spores on hair under microscopic examination is diagnostic.41 For tinea corporis, samples are obtained by scraping the outer edge of the lesion. Spores or hyphae, under microscopic examination, are diagnostic. Potassium hydroxide preparation is more practical than culture for the training room setting because it is quick and inexpensive. Fungal culture can be used for confirmation, but its training room utility is limited by a lag time of up to 2 weeks for results.51
Treatment
Early detection and isolation of wrestlers with active lesions is recommended until adequate treatment is ensured. Appropriate treatment for localized, uncomplicated tinea corporis includes topical treatment for a minimum of 2 weeks (Table 4).14,39,81 Fungicidal allylamines are more efficacious than fungistatic agents such as the imidazoles.14 Topical agents should cover the lesion and a 2-cm circumference and should be applied to the area for 1 week after the lesion has resolved.14 Two to 8 weeks of oral treatment with a fungicidal agent is recommended for diffuse or inflammatory cases of tinea corporis and for tinea capitis (Table 4).14,39,42,53,81 Oral medications can have rare but potentially serious adverse effects, most notably hepatotoxicity; laboratory monitoring is generally required (Table 4).
Table 4.
| Indication | Medication | Dosing Regimen | Comments |
|---|---|---|---|
| Tinea capitis: Diffuse/inflammatory tinea corporis treatment | |||
| Adult | Terbinafine | 250 mg, PO, daily for 2-4 wk | Potential rare hepatotoxicity, anemia, neutropenia, thrombocytopenia, agranulocytosis. LFT elevations in approximately 3%-4% treated. Possible gastrointestinal upset. Obtain baseline CBC and LFT and repeat every 4-6 wk during treatment. |
| Itraconazole | 200 mg, PO, daily for 2-6 wk | Potential rare hepatotoxicity. LFT elevations in approximately 2%-4% treated. Possible gastrointestinal upset. Obtain baseline LFT and repeat every 4-6 wk during treatment. | |
| Ketoconazole | 200 mg, PO, daily for 2-4 wk | Potential severe hepatotoxicity/hepatic failure (1:10,000 treated), hemolytic anemia, neutropenia. Possible gastrointestinal upset. Avoid alcohol because of liver effects and disulfiram-type effect. Obtain baseline CBC and LFT and repeat every month during treatment. | |
| Children | Griseofulvin (micronized) | 20 mg/kg, PO, daily for 8 wk | For child >30 kg. Rare hepatotoxicity and photosensitivity. Possible leukopenia and granulocytopenia. Possible gastrointestinal upset. Obtain CBC and LFT at 6 wk of treatment. |
| Terbinafine | Weight, 10-20 kg: 62.5 mg, PO, daily for 2-4 wk | For child >2 years old. Potential rare hepatotoxicity, anemia, neutropenia, thrombocytopenia, agranulocytosis. LFT elevations in approximately 3%-4% treated. Possible gastrointestinal upset. Obtain baseline CBC and LFT and repeat every 4-6 wk during treatment. | |
| Weight, 20-40 kg: 125 mg, PO, daily for 2-4 wk | |||
| Weight >40 kg: same as adult dosing | |||
| Tinea corporis: Limited area treatment | |||
| Clotrimazole cream | Applied to lesion and surrounding area twice daily | ||
| Miconazole cream | Applied to lesion and surrounding area twice daily | ||
| Terbinafine cream | Applied to lesion and surrounding area twice daily | ||
| Butenafine cream | Applied to lesion and surrounding area once daily | ||
| Prophylaxis | |||
| Adult | Fluconazole | 100 mg, PO, 1x/wk | Rare severe hepatotoxicity/hepatic failure, leukopenia, thrombocytopenia, agranulocytosis. Possible gastrointestinal upset. Avoid alcohol because of liver effects and disulfiram-type effect. Obtain baseline CBC and LFT and repeat every 4-6 wk during treatment. |
CBC, complete blood count; LFT, liver function test; PO, orally.
Antifungal treatment and prophylaxis have been studied in wrestlers. In a randomized prospective trial investigating TG in high school wrestlers, oral fluconazole resulted in negative fungal cultures faster than topical clotrimazole.52 Although this difference did not reach statistical significance, oral antifungals are a practical option because compliance with topical treatments is notoriously difficult.21 In a crossover study of a team of male high school wrestlers over the course of a season, oral itraconazole prophylaxis (200 mg twice daily for 1 day every 2 weeks during the season) decreased the incidence of tinea corporis compared with no prophylaxis.45 In a randomized, double-blind, placebo-controlled study, oral fluconazole taken for 3 months (100 mg once a week) was statistically superior to a placebo in the prevention of TG in high school wrestlers during a season.53 In a 10-year prospective longitudinal study of 373 high school wrestlers,21 fluconazole prophylaxis (100 mg once daily for 3 days at the onset of the season and then at weeks 6 to 8 midseason) was associated with a dramatic reduction in the incidence of TG, with no substantial adverse events.
Varicella Zoster Virus
Varicella zoster virus (VZV) causes a systemic infection characterized by a rash. From 1993 to 2004, VZV accounted for 4.8% of all NCAA practice-related skin infections.5 These infections are frequently competition disqualifying.
Description/Diagnosis
In the United States, 95% of adults more than 40 years old have serologic evidence of previous infection by VZV.4 Varicella (chickenpox) is the primary infection caused by VZV and typically occurs in childhood. After primary infection, most individuals are no longer susceptible because of established immunity, although a new primary infection is possible, especially in immunocompromised individuals.25 Reactivation of a latent virus generally occurs decades after resolution of the primary infection, causing herpes zoster (shingles).
VZV is spread person to person in vesicular fluid from skin lesions or infected respiratory tract secretions61 and enters susceptible individuals via the respiratory tract or conjunctiva.25 After entering the host, VZV travels to the sensory dorsal root ganglia where latency is established.43
A prodrome similar to HSV infections precedes the rash of varicella by approximately 24 hours and may include fever, anorexia, and pharyngitis.6 Similarly, a proteome precedes the rash of herpes zoster infection by days to weeks.43 The rash of varicella is diffuse and involves separate pruritic 2- to 4-mm erythematous papules, with surface vesicles creating a “dew drop on petal” appearance (Figure 11) arising in successive crops over several days.6 The herpes zoster rash has a localized dermatomal distribution and involves clusters of lesions similar to those seen in varicella that coalesce into larger papules or plaques (Figure 12). Areas affected by herpes zoster may be hypersensitive to touch and substantial pruritus.43 Vesicular lesions in varicella and herpes zoster evolve through pustular, ulcerative, and crust stages, with complete resolution occurring in 2 to 4 weeks.6,43 Infected individuals are contagious until all lesions have formed crusts, which usually occurs 4 to 5 days after the onset of rash.4
Figure 11.

Varicella zoster virus lesions initially present as erythematous papules with surface vesicles, creating a “dew drop on petal” appearance. Photo courtesy of the Centers for Disease Control and Prevention/Dr Heinz F. Eichenwald.
Figure 12.
Varicella zoster virus (herpes zoster) lesions on the forehead are found in a dermatomal distribution and in various stages: vesicles, crusted papules, and crusted plaques. Photo courtesy of the Centers for Disease Control and Prevention/Dr Heinz F. Eichenwald.
All VZV infections can present with systemic manifestations, such as pneumonia, encephalitis, or hepatitis.4 Herpes zoster specifically may result in substantially morbid ocular involvement (herpes zoster ophthalmicus) or postherpetic neuralgia.4,43
The diagnosis of VZV infections is usually made on clinical grounds. A complete head-to-toe physical examination is imperative. In atypical presentations, as in HG, diagnostic testing may be useful.7 Polymerase chain reaction testing has good sensitivity and specificity.72
Treatment
Live attenuated vaccine is highly effective in the primary prevention of varicella in otherwise healthy children.77 Nationwide vaccination programs (1995 until 2004) decreased varicella cases from 83% to 93%.25 Consequently, many wrestlers are currently afforded primary protection against varicella. A recent systematic review found evidence to support oral acyclovir (800 mg 5 times a day) within the first 24 hours of the onset rash to reduce the maximum number of the lesions and time to full crusting of lesions.77 This treatment can hasten return to competition.
Molluscum Contagiosum
Molluscum contagiosum (MC) is a cutaneous viral infection commonly transmitted among wrestlers, primarily by skin-to-skin contact.68,81 These infections can be competition-disqualifying in wrestlers if not appropriately managed.
Description/Diagnosis
MC is usually asymptomatic, and the 1- to 10-mm flesh-colored to pink, pearly, isolated, or clustered papules have a small central umbilication (Figure 13). They have a predilection for the face, neck, and trunk. Untreated lesions can trigger adjacent symptomatic eczematous lesions in chronic sufferers or may become secondarily infected with S. aureus.81
Figure 13.

Molluscum contagiosum presents as pearly papules measuring 1 to 10 mm with central umbilication. Photo courtesy of Evanherk (Netherlands).
The diagnosis of MC is usually clinical. In uncertain cases, a positive identification is made if the Tzanck test reveals diagnostic molluscum bodies under microscopic examination.71
Treatment
MC lesions should be treated promptly. A recent review found that no single intervention was convincingly effective in the treatment of nongenital MC in healthy individuals.79 Proposed therapies include cryotherapy,1,68,81 sharp curettage,1,68,81 imiquimod,1,68,81 retinoids,1 5-fluorouracil,1 electrodessication,1 silver nitrate,68 salicylic acid,81 and pulse-dye laser.81 Physical destruction of the lesion through curettage is easily accomplished in the training room setting via the sharp edge of a tongue depressor split longitudinally.1
Verruca Vulgaris
Verruca vulgaris (VV), the common wart, is a nongenital cutaneous viral infection caused by various human papillomavirus and is transmitted primarily by skin-to-skin contact.68 Smoking, toxins, and certain medications may predispose to infection.30 These infections can be competition-disqualifying in wrestlers if not appropriately managed.
Description/Diagnosis
VV lesions are typically firm, skin-colored papules with rough, hyperkeratotic, villiform surfaces (Figure 14). They have a predilection for the hands and fingers, although they can occur anywhere on the body. VV may become painful and tender, depending on the degree of local trauma and the location on the body, with plantar foot and periungual locations commonly causing pain.68 Human papillomavirus can infect mucous membranes,30 causing conjunctival warts or oral focal epithelial hyperplasia.
Figure 14.

Verruca vulgaris presents as papules with rough, hyperkeratotic, villiform surfaces; it commonly affects the hands.
Diagnosis is typically made on clinical grounds. The examiner should evaluate the eyes and oral and nasal cavities. Some cases may present a diagnostic challenge because of an atypical appearance, for example, when the lesion has been traumatized through wrestling. In such cases, excision and dermatopathologic examination may be helpful for diagnosis.30,68
Treatment
VV lesions should be addressed promptly. Proposed therapies include topical acid preparations, cantharidin, podophyllin, tretinoin, intralesional bleomycin, topical 5-fluorouracil, as well as curettage. Curettage and coverage are recommended in the training room setting because of low cost and speed of treatment.
Scabies
Skin infestation with the mite Sarcoptes scabiei, variety hominis, causes scabies. Although the prevalence of this infestation is not clearly identified in wrestling populations, worldwide annual prevalence is approximately 300 million cases.60 This infestation is not common in wrestling populations; however, it is disqualifying.
Description/Diagnosis
Scabies are turtle-shaped, 8-legged parasites less than 0.5 mm in size, contracted by direct contact with infected persons or (rarely) from towels and linens of affected persons. Mites burrow into the skin, where female mites lay eggs that hatch into larvae. Mature mites return to the surface, copulate, and repeat the cycle.
Symptoms appear within a few weeks of infection, usually as pruritus worsens at night. A papular rash arises shortly after pruritus begins. The resulting papules, which are typically erythematous and only a few millimeters in size, are nonspecific in appearance (Figure 15).
Figure 15.

Scabies presents as erythematous nonspecific papules that commonly appear in the interdigital web spaces. Photo courtesy of the Centers for Disease Control and Prevention.
Three features are useful for diagnosis: history of close contact with similar rash or known scabies infestation, a typical distribution, and linear skin lesions from burrows. The rash typically involves skin folds or areas of skin under increased pressure from clothing (eg, interdigital web spaces, axillary folds, groin, extensor surfaces of knees and elbows), with sparing of the head and back. Burrows sometimes cause narrow linear streaks (red, brown, or gray) a few millimeters long, which are helpful in diagnosis. Microscopic examination of skin scrapings confirms the diagnosis.
Treatment
Wrestlers with scabies should be isolated from contact sports until adequate treatment is ensured. NCAA rules require a negative scabies test before resuming wrestling.63 Prevention relies on limiting direct contact with infected persons, treating all members of the household, washing and heat-drying all linens and clothing, and avoidance of shared linens.27
Scabies is effectively treated with a one-time total body application of permethrin 1% cream. It should be washed off 8 to 14 hours after application. Sparring partners and other close contacts should also be treated. An effective alternative is 200 mcg/kg of oral ivermectin, repeated 2 weeks after the first dose. Itching, which can last a few weeks after eradication, can be treated with oral antihistamines.76
Pediculosis
Head lice (Pediculosis humanus capitis) and body lice (Pediculosis humanus humanus) are usually acquired from direct contact with infected persons and uncommonly from sharing clothing, such as sports uniforms and headgear. These conditions are disqualifying in competitive wrestlers.
Description/Diagnosis
Head and body lice are 1 to 3 mm in length and more oblong. Head and pubic lice cling to hairs and lay eggs (nits) that are cemented to the base of the hair. Body lice live in clothing seams, lay eggs in the seams, and return to skin every few days for a blood meal.
Pruritus is common, but wrestlers may be asymptomatic. Infected areas may have small inflammatory papules or punctuate hemorrhagic lesions from bites. Lice may be visible on hair (Figure 16). Excoriations from scratching may be present.
Figure 16.
Head lice appear on hair shafts and on the skin, and excoriations are present as small crusts on the skin. © DermAtlas; http://www.DermAtlas.org.
Diagnosis of pubic and head lice is usually made by identification of lice and nits in the affected area. Combing the hair with a nit comb (a comb specifically designed with closely spaced teeth) can produce nits and lice for identification by the naked eye.
Treatment
Wrestlers with Pediculosis should be isolated from contact sports until adequate treatment is ensured. NCAA rules require treated wrestlers to be reexamined for complete treatment response before resuming wrestling.63 Treatment should involve mechanical removal of lice and nits with careful combing, laundering and hot-air drying of all clothing and linens, and application of topical 1% permethrin or pyrethrin cream. The agents should be applied to affected body areas and then rinsed off after 10 minutes. Treatment should be repeated in 7 days.26,29
Conclusion
Early diagnosis and treatment of cutaneous infections in wrestlers is important. Prompt diagnosis allows isolation of affected wrestlers to prevent spread among close contacts, and early initiation of treatment ensures as fast a return to competition as possible. Prophylaxis with systemic medications should be considered for HG and TG.
Footnotes
The following authors declared potential conflicts of interest: John H. Wilckins, MD, receives publication royalites from Wolters Kluwer.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the US Navy Bureau of Medicine and Surgery, the US Army Medical Department, the US Navy at large, or the US Army at large.
References
- 1. Adams BB. Skin infections in athletes. Dermatol Nurs. 2008;20:39-44 [PubMed] [Google Scholar]
- 2. Adams BB. Tinea corporis gladiatorum. J Am Acad Dermatol. 2002;47:286-290 [DOI] [PubMed] [Google Scholar]
- 3. Adams BB. Tinea corporis gladiatorum: a cross-sectional study. J Am Acad Dermatol. 2000;43:1039-1041 [DOI] [PubMed] [Google Scholar]
- 4. Advisory Committee on Immunization Practices Prevention of varicella: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 1996;45:1-25 [PubMed] [Google Scholar]
- 5. Agel J, Ransone J, Dick R, Oppliger R, Marshall SW. Descriptive epidemiology of collegiate men’s wrestling injuries: National Collegiate Athletic Association Injury Surveillance System, 1988-1989 through 2003-2004. J Athl Train. 2007;42:303-310 [PMC free article] [PubMed] [Google Scholar]
- 6. Albrecht MA. Clinical features of varicella-zoster virus infection: chickenpox. http://www.uptodate.com/contents/clinical-features-of-varicella-zoster-virus-infection-chickenpox?source=search_result&selectedTitle=1%7E150 Accessed November 7, 2011
- 7. Albrecht MA. Diagnosis of varicella-zoster virus infection. http://www.uptodate.com/contents/diagnosis-of-varicella-zoster-virus-infection?source=search_result&selectedTitle=1%7E150 Accessed November 7, 2011
- 8. Albrecht MA. Treatment of genital herpes simplex virus infection. http://www.uptodate.com/contents/treatment-of-genital-herpes-simplex-virus-infection?source=search_result&selectedTitle=1%7E77 Accessed November 7, 2011
- 9. Ammerlaan HSM, Kluytmans JAJW, Berkhout H, et al. Eradication of carriage with methicillin-resistant Staphylococcus aureus: effectiveness of a national guideline. J Antimicrob Chemother. 2011;66:2409-2417 [DOI] [PubMed] [Google Scholar]
- 10. Anderson BJ. The effectiveness of valacyclovir in preventing reactivation of herpes gladiatorum in wrestlers. Clin J Sport Med. 1999;9:86-90 [DOI] [PubMed] [Google Scholar]
- 11. Anderson BJ. The epidemiology and clinical analysis of several outbreaks of herpes gladiatorum. Med Sci Sports Exerc. 2003;35:1809-1814 [DOI] [PubMed] [Google Scholar]
- 12. Anderson BJ. Prophylactic valacyclovir to prevent outbreaks of primary herpes gladiatorum at a 28-day wrestling camp. Jpn J Infect Dis. 2006;59:6-9 [PubMed] [Google Scholar]
- 13. Anderson BJ. Valacyclovir to expedite the clearance of recurrent herpes gladiatorum. Clin J Sport Med. 2005;15:364-366 [DOI] [PubMed] [Google Scholar]
- 14. Andrews MD, Burns M. Common tinea infections in children. Am Fam Physician. 2008;77:1415-1420 [PubMed] [Google Scholar]
- 15. Baddour LM. Cellulitis and erysipelas. http://www.uptodate.com/contents/cellulitis-and-erysipelas Accessed November 7, 2011
- 16. Baker DA, Blythe JG, Miller JM. Once-daily valacyclovir hydrochloride for suppression of recurrent genital herpes. Obstet Gynecol. 1999;94:103-106 [DOI] [PubMed] [Google Scholar]
- 17. Beller M, Gessner BD. An outbreak of tinea corporis gladiatorum on a high school wrestling team. J Am Acad Dermatol. 1994;31:197-201 [DOI] [PubMed] [Google Scholar]
- 18. Belongia EA, Goodman JL, Holland EJ, et al. An outbreak of herpes gladiatorum at a high-school wrestling camp. N Engl J Med. 1991;325:906-910 [DOI] [PubMed] [Google Scholar]
- 19. Bope ET, Kellerman ED. Conn’s Current Therapy 2012: Expert Consult. Philadelphia, PA: Elsevier; 2012 [Google Scholar]
- 20. Breen JO. Skin and soft tissue infections in immunocompetent patients. Am Fam Physician. 2010;81:893-899 [PubMed] [Google Scholar]
- 21. Brickman K, Einstein E, Sinha S, Ryno J, Guiness M. Fluconazole as a prophylactic measure for tinea gladiatorum in high school wrestlers. Clin J Sport Med. 2009;19:412-414 [DOI] [PubMed] [Google Scholar]
- 22. Buss BF, Mueller SW, Theis M, Keyser A, Safranek TJ. Population-based estimates of methicillin-resistant Staphylococcus areus (MRSA) infections among high school athletes: Nebraska, 2006-2008. J Sch Nurs. 2009;25:282-291 [DOI] [PubMed] [Google Scholar]
- 23. Centers for Disease Control Methicillin-resistant Staphylococcus aureus among players on a high school football team: New York City, 2007. MMWR Morb Mortal Wkly Rep. 2009;58:52-55 [PubMed] [Google Scholar]
- 24. Centers for Disease Control Methicillin-resistant Staphylococcus aureus infections among competitive sports participants: Colorado, Indiana, Pennsylvania, and Los Angeles County, 2000-2003. MMWR Morb Mortal Wkly Rep. 2003;52:793-795 [PubMed] [Google Scholar]
- 25. Centers for Disease Control and Prevention Epidemiology and prevention of vaccine-preventable diseases. http://www.cdc.gov/vaccines/pubs/pinkbook/index.html Accessed December 10, 2012
- 26. Centers for Disease Control and Prevention Parasites: lice, head lice. http://www.cdc.gov/parasites/lice/head/ Accessed December 10, 2012
- 27. Centers for Disease Control and Prevention Parasites: scabies. http://www.cdc.gov/parasites/scabies/ Accessed December 10, 2012
- 28. Cohen BA, Schmidt C. Tinea gladiatorum [letter]. N Engl J Med. 1992;327:820. [DOI] [PubMed] [Google Scholar]
- 29. Dodd CS. Interventions for treating head lice. Cochrane Database Syst Rev. 2001;2:CD001165. [DOI] [PubMed] [Google Scholar]
- 30. Drake LA, Ceilley RI, Cornelison RL, et al. Guidelines of care for warts: human papillomavirus. J Am Acad Dermatol. 1995;32:98-103 [DOI] [PubMed] [Google Scholar]
- 31. Drugge JM, Allen PJ. A nurse practitioner’s guide to the management of herpes simplex virus-1 in children. Pediatr Nurs. 2008;34:310-318 [PubMed] [Google Scholar]
- 32. Dworkin MS, Shoemaker PC, Spitters C, et al. Endemic spread of herpes simplex virus type 1 among adolescent wrestlers and their coaches. Pediatr Infect Dis J. 1999;18:1108-1109 [DOI] [PubMed] [Google Scholar]
- 33. El Fari M, Graser Y, Presber W, Tietz HJ. An epidemic of tinea corporis caused by Trichophyton tonsurans among children (wrestlers) in Germany. Mycoses. 2000;43:191-196 [DOI] [PubMed] [Google Scholar]
- 34. Ellis MW, Griffith ME, Dooley DP, et al. Targeted intranasal mupirocin to prevent colonization and infection by community-associated methicillin-resistant Staphylococcus aureus strains in soldiers: a cluster randomized controlled trial. Antimicrob Agents Chemother. 2007;51:3591-3598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ergin S, Ergin C, Erdogan BS, Kaleli I, Evliyaoglu D. An experience from an outbreak of tinea capitis gladiatorum due to Trichophyton tonsurans. Clin Exp Dermatol. 2006;31:212-214 [DOI] [PubMed] [Google Scholar]
- 36. Fife KH, Warren TJ, Justus SE, Heitman CK. An international, randomized, double-blind, placebo-controlled, study of valacyclovir for the suppression of herpes simplex virus type 2 genital herpes in newly diagnosed patients. Sex Transm Dis. 2008;35:668-673 [DOI] [PubMed] [Google Scholar]
- 37. Frisk A, Heilborn H, Melen B. Epidemic occurrence of trichophytosis among wrestlers. Acta Derm Venereol. 1966;46:453-456 [PubMed] [Google Scholar]
- 38. George A, Rubin G. A systematic review and meta-analysis of treatments for impetigo. Br J Gen Pract. 2003;53:480-487 [PMC free article] [PubMed] [Google Scholar]
- 39. Geretti AM. Genital herpes. Sex Transm Infect. 2006;82:31-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Goldman L, Schafer AI, eds. Goldman’s Cecil Medicine. 24th ed. Philadelphia, PA: Elsevier; 2012 [Google Scholar]
- 41. Goldstein AO, Goldstein BG. Dermatophyte (tinea) infections. http://www.uptodate.com/contents/dermatophyte-tinea-infections?source=search_result&selectedTitle=1%7E150 Accessed November 7, 2011
- 42. Habif TP. Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 5th ed. Edinburgh, Scotland: Mosby; 2010 [Google Scholar]
- 43. Harpaz R, Ortega-Sanchez IR, Seward JF. Prevention of herpes zoster: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2008;57:1-30 [PubMed] [Google Scholar]
- 44. Harris A. Prevention and control of methicillin-resistant Staphylococcus aureus in adults. http://www.uptodate.com/contents/prevention-and-control-of-methicillin-resistant-staphylococcus-aureus-in-adults?source=search_result&search=prevention+and+control+of+meth&selectedTitle=10%7E150 Accessed December 10, 2012
- 45. Hazen PG, Weil ML. Itraconazole in the prevention and management of dermatophytosis in competitive wrestlers. J Am Acad Dermatol. 1997;36:481-482 [DOI] [PubMed] [Google Scholar]
- 46. Hedayati MT, Afshar P, Shokohi T, Aghili R. A study on tinea gladiatorum in young wrestlers and dermatophyte contamination of wrestling mats from Sari, Iran. Br J Sports Med. 2007;41:332-334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Holland EJ, Mahanti RL, Belongia EA, et al. Ocular involvement in an outbreak of herpes gladiatorum. Am J Ophthalmol. 1992;114:680-684 [DOI] [PubMed] [Google Scholar]
- 48. Ilkit M, Ali Saracli M, Kurdak H, et al. Clonal outbreak of Trichophyton tonsurans tinea capitis gladiatorum among wrestlers in Adana, Turkey. Med Mycol. 2010;48:480-485 [DOI] [PubMed] [Google Scholar]
- 49. Johnson R. Herpes gladiatorum and other skin diseases. Clin Sports Med. 2004;23:473-484 [DOI] [PubMed] [Google Scholar]
- 50. Kilburn SA, Featherstone P, Higgins B, Brindle R. Interventions for cellulitis and erysipelas. Cochrane Database Syst Rev. 2010;6:CD004299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kohl TD, Lisney M. Tinea gladiatorum: wrestling’s emerging foe. Sports Med. 2000;29:439-447 [DOI] [PubMed] [Google Scholar]
- 52. Kohl TD, Martin DC, Berger MS. Comparison of topical and oral treatments for tinea gladiatorum. Clin J Sport Med. 1999;9:161-166 [DOI] [PubMed] [Google Scholar]
- 53. Kohl TD, Martin DC, Nemeth R, Hill T, Evans D. Fluconazole for the prevention and treatment of tinea gladiatorum. Pediatr Infect Dis J. 2000;19:717-722 [DOI] [PubMed] [Google Scholar]
- 54. Koning S, van der Sande R, Verhagen AP, et al. Interventions for impetigo. Cochrane Database Syst Rev. 2012;1:CD003261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Lambert M. IDSA guidelines on the treatment of MRSA infections in adults and children. Am Fam Physician. 2011;84:455-463 [Google Scholar]
- 56. Landry GL, Chang CJ. Herpes and tinea in wrestling: managing outbreaks, knowing when to disqualify. Phys Sportsmed. 2004;32:34-41 [DOI] [PubMed] [Google Scholar]
- 57. Lee AS, Macedo-Vinas M, Francois P, et al. Impact of combined low-level mupirocin and genotypic chlorhexidine resistance on persistent methicillin-resistant Staphylococcus aureus carriage after decolonization therapy: a case-control study. Clin Infect Dis. 2011;52:1422-1430 [DOI] [PubMed] [Google Scholar]
- 58. Lindenmayer JM, Schoenfeld S, O’Grady R, Carney JK. Methicillin-resistant Staphylococcus aureus in a high school wrestling team and the surrounding community. Arch Intern Med. 1998;158:895-899 [DOI] [PubMed] [Google Scholar]
- 59. Loeb M, Main C, Eady A, Walker-Dilks C. Antimicrobial drugs for treating methicillin-resistant Staphylococcus aureus colonization. Cochrane Database Syst Rev. 2003;4:CD003340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases. 7th ed. Philadelphia, PA: Churchill Livingstone; 2010 [Google Scholar]
- 61. Marin M, Guris D, Chaves SS, Schmid S, Seward JF. Prevention of varicella: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2007;56:1-40 [PubMed] [Google Scholar]
- 62. May TJ, Safranek S. Clinical inquiries: when should you suspect community-acquired MRSA? How should you treat it? J Fam Pract. 2009;58:276, 278. [PubMed] [Google Scholar]
- 63. National Collegiate Athletic Association 2011-12 NCAA sports medicine handbook. http://www.ncaapublications.com/productdownloads/MD11.pdf Accessed November 7, 2011
- 64. National Collegiate Athletic Association Wrestling 2010 and 2011 rules and interpretations. Appendix B: Skin infections in wrestling. http://matref0.tripod.com/Rule%20Books/2009ncaarules.pdf Accessed November 7, 2011
- 65. National Federation of State High School Association, Sports Medicine Advisory Committee Sports related skin infections position statement and guidelines. http://www.doe.k12.de.us/infosuites/students_family/diaa/files/110410SportsRel_SkinInfect_PSGuide.pdf Accessed November 7, 2011
- 66. Pecci M, Comeau D, Chawla V. Skin conditions in the athlete. Am J Sports Med. 2009;37:406-418 [DOI] [PubMed] [Google Scholar]
- 67. Pique E, Copado R, Cabrera A, et al. An outbreak of tinea gladiatorum in Lanzarote. Clin Exp Dermatol. 1999;24:7-9 [PubMed] [Google Scholar]
- 68. Pleacher MD, Dexter WW. Cutaneous fungal and viral infections in athletes. Clin Sports Med. 2007;26:397-411 [DOI] [PubMed] [Google Scholar]
- 69. Poisson DM, Rousseau D, Defo D, Esteve E. Outbreak of tinea corporis gladiatorum, a fungal skin infection due to Trichophyton tonsurans, in a French high level judo team. Euro Surveill. 2005;10:187-190 [PubMed] [Google Scholar]
- 70. Rajendran PM, Young D, Maurer T, et al. Randomized, double-blind, placebo-controlled trial of cephalexin for treatment of uncomplicated skin abscesses in a population at risk for community-acquired methicillin-resistant Staphylococcus aureus infection. Antimicrob Agents Chemother. 2007;51:4044-4048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Ruocco E, Brunetti G, Del Vecchio M, Ruocco V. The practical use of cytology for diagnosis in dermatology. J Eur Acad Dermatol Venereol. 2011;25:125-129 [DOI] [PubMed] [Google Scholar]
- 72. Sauerbrei A, Eichhorn U, Schacke M, Wutzler P. Laboratory diagnosis of herpes zoster. J Clin Virol. 1999;14:31-36 [DOI] [PubMed] [Google Scholar]
- 73. Schmitz GR, Bruner D, Pitotti R, et al. Randomized controlled trial of trimethoprim-sulfamethoxazole for uncomplicated skin abscesses in patients at risk for community-associated methicillin-resistant Staphylococcus aureus infection. Ann Emerg Med. 2010;56:283-287 [DOI] [PubMed] [Google Scholar]
- 74. Schmutzhard J, Merete Riedel H, Zweygberg Wirgart B, Grillner L. Detection of herpes simplex virus type 1, herpes simplex virus type 2 and varicella-zoster virus in skin lesions: comparison of real-time PCR, nested PCR and virus isolation. J Clin Virol. 2004;29:120-126 [DOI] [PubMed] [Google Scholar]
- 75. Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clin Infect Dis. 2005;41:1373-1406 [DOI] [PubMed] [Google Scholar]
- 76. Strong M, Johnstone P. Interventions for treating scabies. Cochrane Database Syst Rev. 2007;3:CD000320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Swingler G. Chickenpox [published online August 1, 2007]. Clin Evid. [Google Scholar]
- 78. Usatine RP, Tinitigan R. Nongenital herpes simplex virus. Am Fam Physician. 2010;82:1075-1082 [PubMed] [Google Scholar]
- 79. van der Wouden JC, van der Sande R, van Suijlekom-Smit LWA, et al. Interventions for cutaneous molluscum contagiosum. Cochrane Database Syst Rev. 2009;4:CD004767. [DOI] [PubMed] [Google Scholar]
- 80. Weber K. Community-associated methicillin-resistant Staphylococcus aureus infections in the athlete. Sports Health. 2009;1:405-410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Zinder SM, Basler RSW, Foley J, Scarlata C, Vasily DB. National Athletic Trainers’ Association position statement: skin diseases. J Athl Train. 2010;45:411-428 [DOI] [PMC free article] [PubMed] [Google Scholar]