Abstract
This case study describes a Major League Baseball player who was diagnosed with an axillary artery thrombosis due to arterial compression from throwing. The purpose of this article is to create awareness as to the signs and symptoms associated with arterial positional compression and the rehabilitative implications to surgical intervention.
Keywords: arterial positional compression, thoracic outlet syndrome, effort thrombosis, axillary artery thrombosis, overhead throwing athletes
The overhead throwing motion has 6 sequential phases: wind-up, early/late cocking, acceleration, deceleration, and follow-through. Within this throwing cycle, potential energy is generated and efficiently converted into kinetic energy that is transferred to the ball.14 As a result of this repetitive throwing activity, the overhead throwing athlete places extreme demand on his or her shoulder. Subsequently, during skeletal development, several adaptive morphologic changes occur, including increased glenohumeral external rotation, increased humeral head and glenoid retroversion, and anterior capsular laxity.4,7,8,13,20 These compensatory changes play an integral role in the delicate balance between the static and dynamic stabilization systems of the shoulder. However, they also place the musculoskeletal and vascular structures of the throwing shoulder at risk for injury.4
A baseball pitcher reaches a maximal internal rotational velocity of 6100 to 7510 deg/s.11 By increasing external rotation in the late cocking phase of throwing, the arc of rotation is expanded, and subsequently, velocity can be optimized. When the throwing shoulder is subject to stresses at a rate that exceeds the tissue’s maximum load to failure, acute or chronic/progressive damage to the shoulder’s stabilizing structures can occur.12 By examining the kinetics of the pitching motion, Fleisig and colleagues11 noted that within the late cocking phase, 67 Nm of shoulder internal rotation torque and a maximum anterior shear force of 380 N are generated shortly before the arm reaches maximum external rotation. If the internal rotation torque is increased to the point where the maximum anterior shear force of the shoulder is exceeded, injury to the throwing shoulder can occur. While an acute increase beyond the maximum anterior shear force across the shoulder can cause a tear within the anterior capsulolabral complex, repetitive submaximal forces can result in increased anterior capsular laxity as well as potential injury to the vascular structures surrounding the shoulder.2,3,5
Recent work by Bast et al3 assessed the effects of throwing on upper extremity arterial blood flow. A wrist/brachial index (WBI) vascular examination and a vascular ultrasound examination were performed on 18 pitchers before and after a 50-pitch workout session. Throwers with signs of shoulder laxity had a significant decrease in arterial blood flow compared with throwers with no evidence of laxity. This vascular insufficiency probably occurs because of the repetitive positional compression onto the third portion of the axillary artery as the humeral head translates anteriorly during the late cocking phase of throwing.9
Using duplex ultrasound, a correlation between clinically relevant axillary artery compression and increased anterior glenohumeral translation has been demonstrated in the overhead throwing position.17 This intermittent compression can cause chronic changes in downstream vascular sufficiency and potentially lead to an axillary artery aneurysm or thrombus in the overhead throwing athlete.16
Extrinsic positional compression causing distal occlusion can also occur within the subclavian artery at the level of the first rib, typically a congenital cervical rib or first rib anomaly, within the scalene triangle.9 While repetitive arterial positional compression is rare, it is an important problem in the elite overhead throwing athlete requiring recognition and treatment by the player’s medical staff.
Case Report
A 26-year-old right-handed Major League Baseball pitcher reported to the training staff after a regularly scheduled start that his right hand felt cool and he had a sensation of numbness in the distal aspect of his right long finger. In addition, he described his arm as having a “dead” and “heavy” feeling. His symptoms occurred initially after his postgame shower and did not resolve overnight, preventing him from sleeping. After questioning, he noted that these same symptoms occurred after a game 2 weeks prior but resolved completely that same night and were not reported to the training staff. He had an approximate 2-year history of distal right long finger numbness, which was not reported since he felt that his symptoms did not affect his ability to pitch. He also had a right shoulder labral tear that was treated nonsurgically.
Physical examination revealed an absent right radial pulse, visible pallor, and a right forearm and hand that were cool to the touch. There was full right shoulder and cervical range of motion but a noted sense of fatigue after repeated resisted strength movements to the right shoulder. Neurologic examination demonstrated decreased sensation at the distal aspect of the right long finger. He had decreased coordination of the right upper extremity when the arm felt fatigued and heavy. Provocative testing for thoracic outlet syndrome including the Adson test1 and the Wright19 hyperabduction test could not be performed because the radial pulse was already absent.
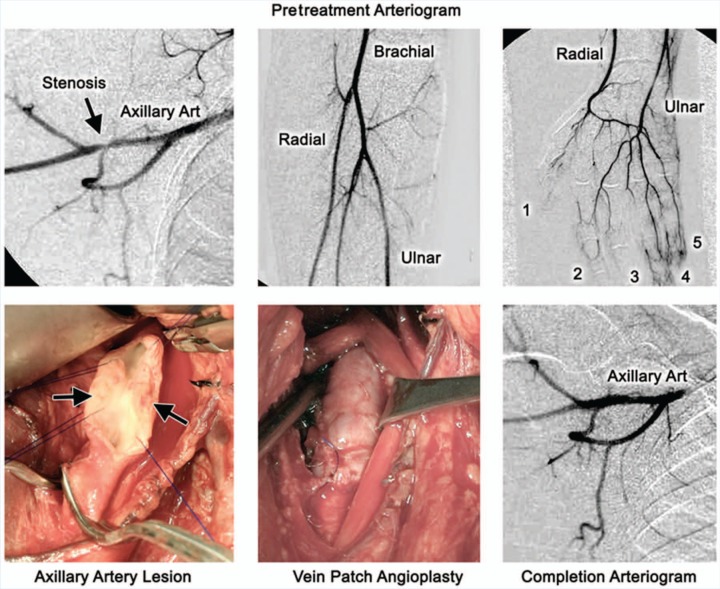
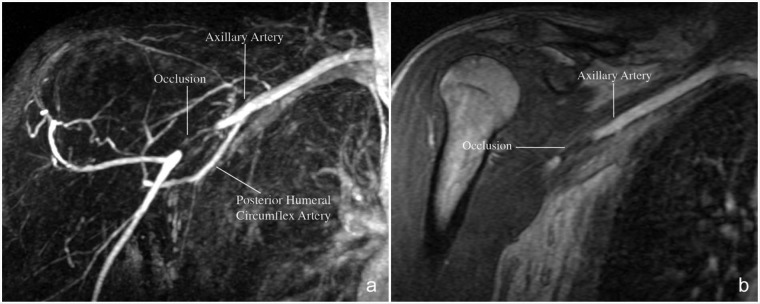
The following day, a contrast enhanced magnetic resonance angiogram of the right shoulder was performed, which demonstrated a 3.6-cm area of occlusion of the distal axillary artery, just proximal to the origin of the posterior humeral circumflex artery (Figure 1). The occlusion was confirmed by a right upper extremity conventional digital subtraction angiogram (Figure 2) and treated via catheter-directed thrombolysis administered just proximal to the occlusion. A repeat conventional angiogram the following day noted improved arterial flow but a residual stenotic area within the axillary artery. He was started on anticoagulant therapy and noted elimination of the heavy sensation in the right upper extremity in the ensuing days.
Figure 1.
Contrast-enhanced, 3-dimensional (a) digital subtracted and (b) gradient-recalled magnetic resonance angiogram of the right shoulder demonstrating a 3.6-cm area of occlusion of the distal axillary artery just proximal to the origin of the posterior humeral circumflex artery.
Figure 2.
Angiogram images demonstrating the axillary artery occlusion.
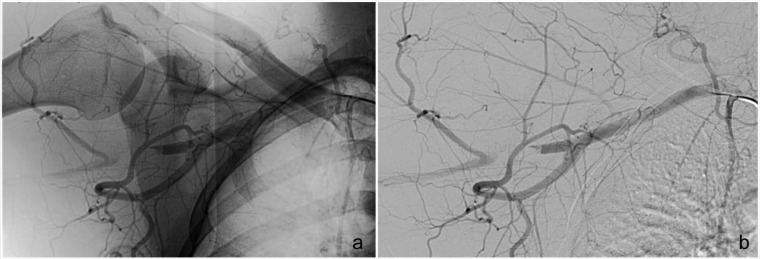
After further medical consultation, the affected segment of the axillary artery was excised and reconstructed using a reversed saphenous vein interposition bypass graft (Figure 3).9 Postoperatively, the player was placed on standardized oral anticoagulation and antiplatelet therapy for 6 weeks. At the 3-week postoperative point, he was allowed light cardiovascular exercises and lower body workouts with no weights in his hands or on the shoulders. Upper body exercises consisted of active and active-assisted elevation exercises, scapular stabilization exercises, and light upper extremity neural mobilizations. The initial focus was to regain shoulder range of motion gradually without stressing the surgical repair site.
Figure 3.
Intraoperative images demonstrating the pretreatment arteriogram, axillary artery lesion, vein patch angioplasty, and the completion arteriogram.
At the 6-week point, a follow-up arteriogram demonstrated good flow with the right arm at the side and in the abducted and externally rotated position (Figure 4). An upper body–resisted exercise program was then started consisting of tubing rows, latissimus dorsi pull-downs, internal/external rotation (IR/ER), proprioceptive neuromuscular facilitation (PNF) D2 flexion, light dumbbell serratus punches, side lying ER, and prone lower trapezius exercises. Exercises were progressed from arms at sides to positions of 90/90 over the next 2 weeks. At 8 weeks postoperatively, he was cleared to begin his throwing program initially with 25 throws at 60 feet and then progressed over the next month with scheduled throwing every other day (Table 1). During his throwing progression, there were no symptoms. A normal radial pulse was noted and no complaints of numbness in the long finger. He participated in spring training and is expected to play at the Major League level with no restrictions.
Figure 4.
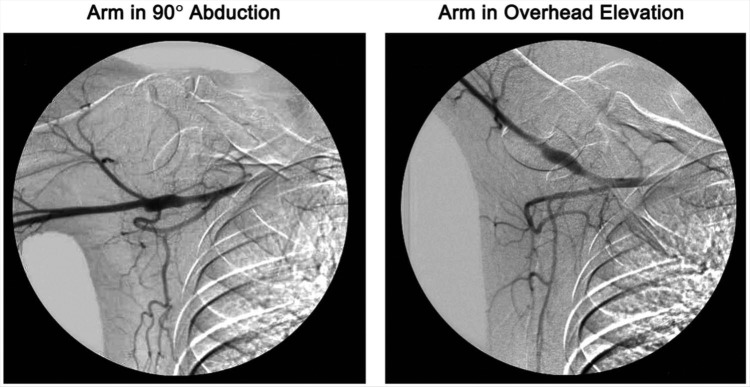
A follow-up arteriogram at the 6-week postoperative point, which demonstrates good flow with the right in the abducted position at 90° and with the arm in overhead elevation.
Table 1.
Rehabilitation throwing program
| Number of Throws/Distance | Number of Throws/Distance | ||
|---|---|---|---|
| Day 1 | 1 × 25 @ 60’ | Day 6 | 1 × 30 @ 90’, 1 × 25 @ 120’ |
| Day 2 | 2 × 25 @ 60’ | Day 7 | 2 × 20 @ 120’ |
| Day 3 | 1 × 25 @ 60’, 1 × 25 @ 90’ | Day 8 | 1 × 20 @ 120’, 1 × 20 @ 150’ |
| Day 4 | 1 × 30 @ 60’, 1 × 25 @ 90’ | Day 9 | 1 × 20 @ 150’,10 pitches (mound) |
| Day 5 | 1 × 30 @ 60’, 1 × 25 @ 90’ | Day 10 | Long toss, 35 pitch bullpen |
Discussion
This case highlights the importance for the entire medical staff to recognize the signs and symptoms of arterial positional compression in the overhead throwing athlete. Athletes will present with complaints of cold intolerance, hypersensitivity, ischemic pain, numbness, or arm fatigue during or immediately after practice and competition. The presentation is always late as only significant embolization or reduced flow to the hand will result in perceptible symptoms of temperature change and numbness. Pulse diminution is not always seen. A recent cross-sectional survey of elite volleyball players in the Dutch national leagues found symptoms ranging from 11% to 27% associated with posterior circumflex humeral artery aneurysmatic dilation and an associated distal occlusion.18 The high prevalence of symptoms of digital ischemia in this healthy athletic population further stresses the need for active surveillance by the medical staff. Along with a standardized history and physical examination, advanced imaging techniques can be utilized to verify whether the presenting symptoms are related to arterial positional compression.
Doppler ultrasonography, conventional or computed tomography (CT) angiography, and magnetic resonance (MR) angiography all provide potentially useful information for suspected arterial compromise in the overhead throwing athlete.6,10,15 MR angiography does not require arterial catheterization but rather an intravenous injection of gadolinium contrast and can be performed within 5 minutes using standardized software, providing an effective, relatively noninvasive form of screening for athletes at risk. While MR angiography is the best noninvasive imaging study that provides clinically relevant information and may exclude etiologies that mimic arterial compromise, contrast angiography remains the gold standard.6,10 In this case, MR angiography identified the blood clot in the patient’s right axillary artery, which was subsequently confirmed with conventional angiography and treated via catheter-directed thrombolysis.
For the overhead throwing athlete with arterial positional compression, successful treatment with physical therapy alone, thrombolytic therapy alone, or in combination with angioplasty and stenting has had limited success.9 Stress placed on the shoulder from a repetitive throwing motion results in an intimal tear within the vessel causing clotting, aneurysmal dilation, and resulting emboli. As a result, surgical intervention provides the best treatment for compressive lesions of the axillary artery and the best outcome for subsequent return to overhead throwing athletic activity, contingent upon a structured postoperative rehabilitation program. This rehabilitation program is similar for all surgical interventions that address compressive lesions of the axillary artery and its branches (Table 1).
Conclusion
Arterial positional compression is a serious condition that can present in overhead throwing athletes with complaints of cold intolerance, hypersensitivity, ischemic pain, numbness, or arm fatigue during or immediately after practice and competition. These findings present late in the disease process as only significant embolization or reduced flow to the hand will result in perceptible symptoms of temperature change and numbness. Prompt diagnosis using MR angiography followed by surgical intervention and a focused rehabilitation program can allow successful return to play for the athlete with symptomatic arterial positional compression.
Footnotes
The following authors declared potential conflicts of interest: Hollis G. Potter, MD, is Associate Editor for Imaging with Sports Health and an editorial board member for Cartilage and Osteoarthritis and Cartilage, a consultant for Smith and Nephew and for Biomet, and received grants from General Electric Healthcare; Andrew J. Welland, MD, is a board member of the Journal of Bone and Joint Surgery - America and is a consultant for Acumed, LLC; and Struan H. Coleman is a consultant for Stryker.
References
- 1. Adson AW. Surgical treatment for symptoms produced by cervical ribs and the scalenus anticus muscle. Surg Gynecol Obstet. 1947;85:687-700 [PubMed] [Google Scholar]
- 2. Bast SC, Perry JR, Poppiti R, Vangsness CT, Weaver FA. Upper extremity blood flow in collegiate and high school baseball pitchers: a preliminary report. Am J Sports Med. 1996;24:847-851 [DOI] [PubMed] [Google Scholar]
- 3. Bast SC, Weaver FA, Perese S, Jobe FW, Weaver DC, Vangsness CT., Jr The effects of shoulder laxity on upper extremity blood flow in professional baseball pitchers. J Shoulder Elbow Surgery. 2011;20:461-466 [DOI] [PubMed] [Google Scholar]
- 4. Bigliani LU, Codd TP, Connor PM, Levine WN, Littlefield MA, Hershon SJ. Shoulder motion and laxity in the professional baseball player. Am J Sports Med. 1997;25:609-613 [DOI] [PubMed] [Google Scholar]
- 5. Bigliani LU, Pollock RG, Soslowsky LJ, Flatow EL, Pawluk RJ, Mow VC. Tensile properties of the inferior glenohumeral ligament. J Orthop Res. 1992;10:187-197 [DOI] [PubMed] [Google Scholar]
- 6. Charon JP, Milne W, Sheppard DG, Houston JG. Evaluation of MR angiographic technique in the assessment of thoracic outlet syndrome. Clin Radiol. 2004;59:588-595 [DOI] [PubMed] [Google Scholar]
- 7. Crockett HC, Gross LB, Wilk KE, et al. Osseous adaptation and range of motion at the glenohumeral joint in professional baseball pitchers. Am J Sports Med. 2002;30:20-26 [DOI] [PubMed] [Google Scholar]
- 8. Drakos MC, Rudzki JR, Allen AA, Potter HG, Altchek DW. Internal impingement of the shoulder in the overhead athlete. J Bone Joint Surg Am. 2009;91:2719-2728 [DOI] [PubMed] [Google Scholar]
- 9. Duwayri YM, Emery VB, Driskill MR, et al. Positional compression of the axillary artery causing upper extremity thrombosis and embolism in the elite overhead throwing athlete. J Vasc Surg. 2011;53:1329-1340 [DOI] [PubMed] [Google Scholar]
- 10. Esposito MD, Arrington JA, Blackshear MN, Murtagh FR, Silbiger ML. Thoracic outlet syndrome in a throwing athlete diagnosed with MRI and MRA. J Magn Reson Imaging. 1997;7:598-599 [DOI] [PubMed] [Google Scholar]
- 11. Fleisig GS, Andrews JR, Dillman CJ, Escamilla RF. Kinetics of baseball pitching with implications about injury mechanisms. Am J Sports Med. 1995;23:233-239 [DOI] [PubMed] [Google Scholar]
- 12. Kvitne RS, Jobe FW. The diagnosis and treatment of anterior instability in the throwing athlete. Clin Orthop Relat Res. 1993;(291):107-123 [PubMed] [Google Scholar]
- 13. Osbahr DC, Cannon DL, Speer KP. Retroversion of the humerus in the throwing shoulder of college baseball pitchers. Am J Sports Med. 2002;30:347-353 [DOI] [PubMed] [Google Scholar]
- 14. Ouellette H, Labis J, Bredella M, Palmer WE, Sheah K, Torriani M. Spectrum of shoulder injuries in the baseball pitcher. Skeletal Radiol. 2008;37:491-498 [DOI] [PubMed] [Google Scholar]
- 15. Remy-Jardin M, Remy J, Masson P, et al. Helical CT angiography of thoracic outlet syndrome: functional anatomy. AJR Am J Roentgenol. 2000;174:1667-1674 [DOI] [PubMed] [Google Scholar]
- 16. Stapleton CH, Green DJ, Cable NT, George KP. Flow-mediated dilation and intima-media thickness of the brachial and axillary arteries in individuals with and without inducible axillary artery compression. Ultrasound Med Biol. 2009;35:1443-1451 [DOI] [PubMed] [Google Scholar]
- 17. Stapleton CH, Herrington L, George K. Anterior translation at the glenohumeral joint: a cause of axillary artery compression? Am J Sports Med. 2008;36:539-544 [DOI] [PubMed] [Google Scholar]
- 18. van de Pol D, Kuijer PP, Langenhorst T, Maas M. High prevalence of self-reported symptoms of digital ischemia in elite male volleyball players in the Netherlands: a cross-sectional national survey. Am J Sports Med. 2012;40:2296-2302 [DOI] [PubMed] [Google Scholar]
- 19. Wright IS. The neurovascular syndrome produced by hyperabduction of the arms: the immediate changes produced in 150 normal controls, and the effects on some persons of prolonged hyperabduction of the arms, as in sleeping, and in certain occupations. Am Heart J. 1945;29(1):1-19 [Google Scholar]
- 20. Wyland DJ, Pill SG, Shanley E, et al. Bony adaptation of the proximal humerus and glenoid correlate within the throwing shoulder of professional baseball pitchers. Am J Sports Med. 2012;40:1858-1862 [DOI] [PubMed] [Google Scholar]