Abstract
Background:
Field expedient screening tools that can identify individuals at an elevated risk for injury are needed to minimize time loss in American football players. Previous research has suggested that poor dynamic balance may be associated with an elevated risk for injury in athletes; however, this has yet to be examined in college football players.
Hypothesis:
To determine if dynamic balance deficits are associated with an elevated risk of injury in collegiate football players. It was hypothesized that football players with lower performance and increased asymmetry in dynamic balance would be at an elevated risk for sustaining a noncontact lower extremity injury.
Study Design:
Prospective cohort study.
Methods:
Fifty-nine collegiate American football players volunteered for this study. Demographic information, injury history, and dynamic balance testing performance were collected, and noncontact lower extremity injuries were recorded over the course of the season. Receiver operator characteristic curves were calculated based on performance on the Star Excursion Balance Test (SEBT), including composite score and asymmetry, to determine the population-specific risk cut-off point. Relative risk was then calculated based on these variables, as well as previous injury.
Results:
A cut-off point of 89.6% composite score on the SEBT optimized the sensitivity (100%) and specificity (71.7%). A college football player who scored below 89.6% was 3.5 times more likely to get injured.
Conclusion:
Poor performance on the SEBT may be related to an increased risk for sustaining a noncontact lower extremity injury over the course of a competitive American football season.
Clinical Relevance:
College football players should be screened preseason using the SEBT to identify those at an elevated risk for injury based upon dynamic balance performance to implement injury mitigation strategies to this specific subgroup of athletes.
Keywords: injury screening, field testing, Star Excursion Balance Test
American football traditionally has one of the highest injury rates in comparison with other team sports.8,9,20 Risk factors for injury during football that have been previously identified include competition level,8,19 time of season,8 playing surface,14 player position,19 playing experience,21 and prior injury.19 Unfortunately, few of these factors are modifiable to alter injury risk. Some modifiable factors traditionally associated with injury risk in football include body mass index (BMI), strength, and flexibility.3,11,12,22 Previous research in football players has suggested that strength alone is not related to an elevated risk of injury, while findings for BMI are inconclusive.21,25 Recently, functional testing protocols that examine multiple domains of body-relative movements have been able to predict professional football players at increased risk for injury.11 However, this study did not examine tests that require a greater degree of dynamic balance (ie, single limb balance at the limit of stability), which may provide insight into additional injury risk in American football players.
Dynamic balance performance has previously been associated with increased injury risk in varied populations.2,13,17 Previous work by Plisky et al17 observed that high school basketball players who exhibited asymmetry (>4 cm) or low performance (lower one-third of population) on the Star Excursion Balance Test (SEBT) were at an elevated risk for lower extremity injury. In addition, poor performance in the posterolateral direction of the SEBT is a strong predictor of ankle sprains in recreational adults.14 Not surprisingly, poor performance in dynamic balance has been observed in patients with a history of injury. Individuals with a history of chronic ankle instability perform worse on the SEBT in comparison with uninjured controls.5,18 Likewise, patients with a history of an anterior cruciate ligament (ACL) tear perform worse on the SEBT when compared with controls.4 As a result, it appears as if dynamic balance is related to increased injury risk and that following injury, changes in dynamic balance occur that decrease dynamic balance ability. However, these relationships have yet to be established in American football players.
Because of the high injury rates in American football, preparticipation screening for athletes at an elevated risk of injury may be helpful to develop individualized prospective plans of rehabilitation for at-risk players. Dynamic balance screening may provide additional information to identify American football players at an elevated risk for injury. Therefore, the purpose of this study was to examine how preseason performance of dynamic balance, using the SEBT, is related to lower extremity injuries in a small cohort of college-level American football players. It was expected that individuals who perform poorly on the dynamic balance test or exhibit asymmetry for a given reach direction will be at an elevated risk for injury.
Methods
Subjects and Setting
This study was approved by the institutional review board at the location where the testing occurred. Prior to the athlete’s season, each subject completed a survey that included demographics, history of previous injury, and current medical restrictions. Informed consent was obtained from each subject prior to data collection. Ninety-eight male collegiate American football players were recruited from the active roster of the football team, with 39 players being excluded from the study. Subjects were excluded if they declined to participate (n = 31) or failed to meet the inclusion criteria (n = 8) (Figure 1). Inclusion criteria consisted of: (1) no musculoskeletal injury (eg, postoperative conditions, musculotendinous, ligamentous, or bony defects) within 6 months of the start of the study and (2) no musculoskeletal pain at the time of testing (0 on a 0-10 numeric pain scale). As a result, 59 male collegiate American football players participated in the study. These 59 athletes had a mean age of 19.4 ± 1.1 years, height of 1.81 ± 0.05 m, and mass of 95.4 ± 18.4 kg. All athletes were currently participating in activities associated with American football training and were free of pain during their current athletic activities.
Figure 1.
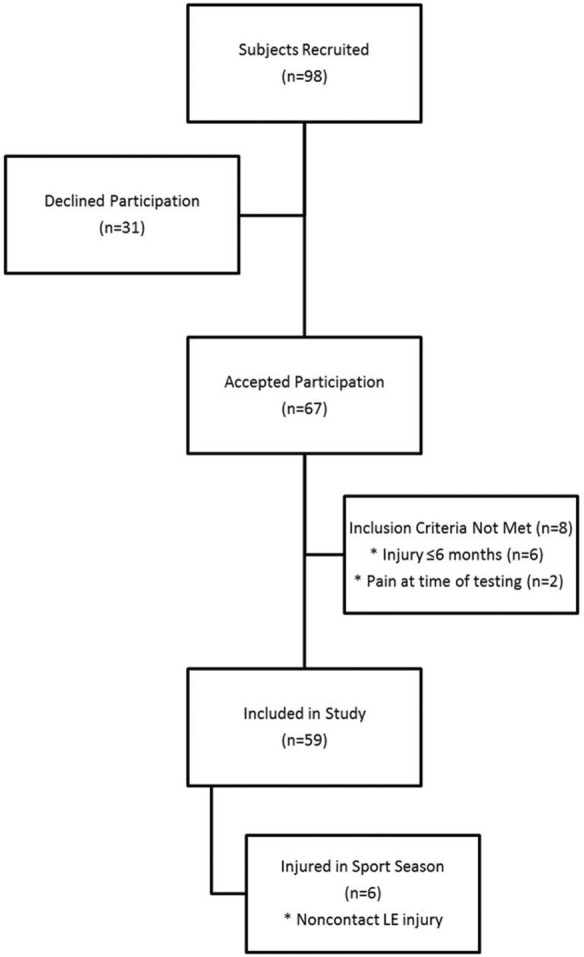
Flow diagram indicating selection of subjects in the study and injuries incurred. LE, lower extremity.
Lower Quarter Y-Balance Testing Protocol
All athletes’ dynamic balance was tested using the SEBT, as performed using the Lower Quarter Y-Balance Test protocol (YBT-LQ), at the beginning of the team’s preseason training. The YBT-LQ examines lower extremity reach of the contralateral leg while maintaining unilateral stance (Figure 2).15,16 Plisky and colleagues demonstrated excellent reliability using a standardized protocol for the YBT-LQ, which was followed for the current study. The YBT-LQ examines unilateral reach in 3 different directions of the SEBT: anterior, posteromedial, and posterolateral. To perform the YBT-LQ, each subject stands with the right foot on the center foot plate and the most distal aspect of the subject’s barefoot at the starting line.16 Three trials were completed in each direction (anterior, posteromedial, posterolateral) following the standardized warm-up practice trials.16 The same process was repeated using the contralateral limb as the stance limb. Per the YBT-LQ protocol, a trial was discarded if the subject (1) failed to maintain unilateral stance, (2) touched down on the reaching foot, or (3) failed to return to the starting position. Performance for all trials was recorded, and the maximum reach score for each reach direction was extracted for data analysis. Differences in the maximum reach for left and right leg were compared to examine reach asymmetry for each direction. The composite score on the test was calculated by averaging the maximum scores for each reach direction after the maximum scores were normalized to limb length.
Figure 2.
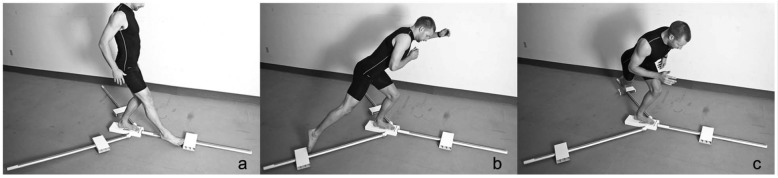
(a-c) Lower Quarter Y-Balance Test reach directions.
Injury Surveillance Protocol
Over the course of a single American football season, all athletes were monitored for lower extremity noncontact injuries. All injuries were tracked with a standardized software system (Sports Injury Monitoring System [SIMS], Flantech, Iowa City, Iowa). Based on prior research, an injury definition was modified and defined as noncontact lower extremity trauma that required medical intervention and resulted in time loss of more than 1 day from participation in sports-related activities.17 The primary rationale for adopting this injury definition was because of the limited prospective studies that specifically included a noncontact mechanism. Two certified athletic trainers recorded the injury, date of injury, diagnosis, time lost, and date of return to unrestricted participation into the SIMS software program. These injury reports were submitted to the primary investigator to ensure accuracy. If a discrepancy was observed by the research team, a meeting was scheduled to discuss the results. To maintain privacy, all athletes were provided an individualized identification code for monthly report generation from the SIMS software. These reports were then provided to the research team to maintain the subject’s privacy and confidentiality.
Statistical Analysis
All statistical analyses were conducted using SPSS version 16.0 (IBM, Armonk, New York). To identify factors associated with an elevated injury risk, a receiver operator characteristic (ROC) curve was developed, and the cut-off point was established at the score that maximized sensitivity and specificity. After the cut-off point was established, a 2 × 2 table was created to calculate relative risk. This process was completed for YBT-LQ composite score, asymmetry for each reach direction, and prior injury.
Results
Six of 59 American football players sustained a noncontact injury to the lower extremity over the course of the season. An analysis of the injury incidence revealed that ankle sprain and hamstring strain were the most common isolated injuries observed, and muscles that crossed the hip joint were the most commonly injured muscle groups (Table 1).
Table 1.
Type and frequency of noncontact lower extremity injuries observed
| Injury Type | Injury Frequency | Time Loss From Injury (range in days) |
|---|---|---|
| Ankle sprain | 2 | 3-52 |
| Tibial stress reaction | 1 | 2 |
| Hamstring strain | 2 | 1-10 |
| Groin/adductor strain | 1 | 38 |
ROC curve analysis revealed that a cut-off point of 89.6% limb length maximized sensitivity (100.0%) and specificity (71.7%) (Table 2). At this cut-off point, all athletes who developed a noncontact lower extremity injury were identified, along with 15 athletes who did not get injured (positive likelihood ratio: 3.5, 95% confidence interval [CI], 2.4-5.3). ROC analysis for reach asymmetry on the SEBT and previous injury did not assist with identifying athletes at risk for an injury during the upcoming season. The positive likelihood ratio from the current study in combination with expected incidence moved the risk of injury during a football season from 37.7%, based on prior research, to 68.1% for this given dynamic balance cut-off point (Figure 3).
Table 2.
Lower Quarter Y-Balance Test cut-off point and noncontact lower extremity injury occurrence
| YBT-LQ Composite Reach Cut-off Score | Noncontact LE Injury Present (+) | Noncontact LE injury Absent (–) |
|---|---|---|
| (+) YBT-LQ (<89% LL) | 6 (true positive result) | 15 (false positive result) |
| (–) YBT-LQ (≥89% LL) | 0 (false negative result) | 38 (true negative result) |
YBT-LQ, Lower Quarter Y-Balance Test; LE, lower extremity; LL, limb length.
Figure 3.
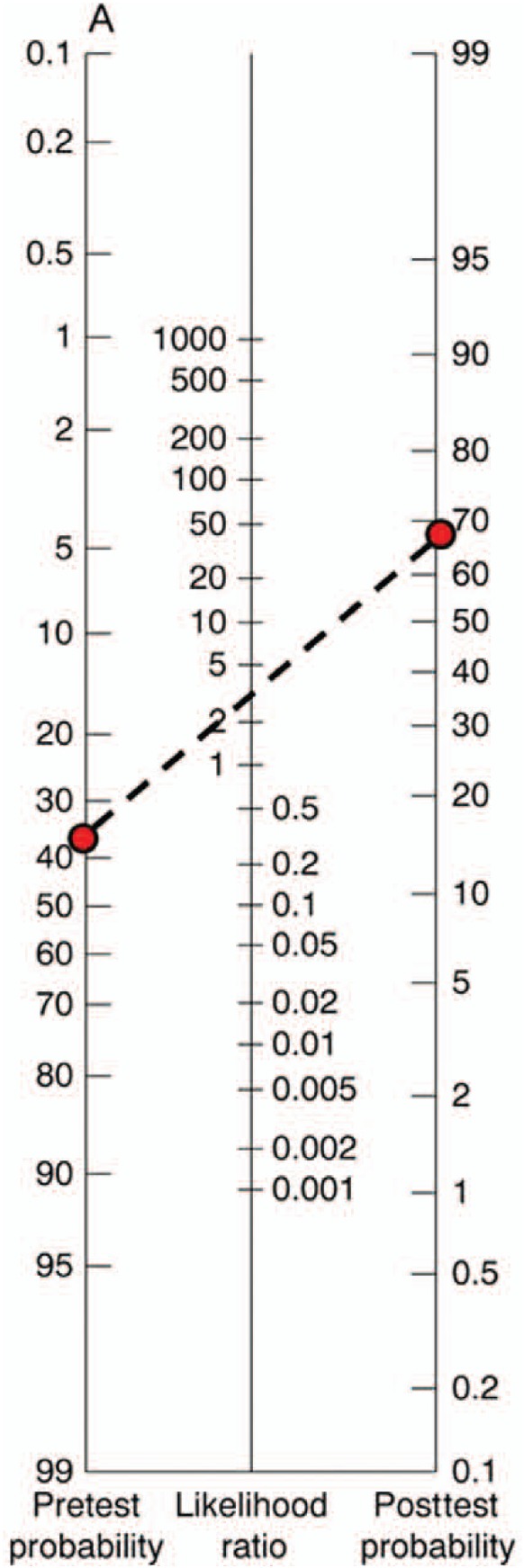
Likelihood ratio nomogram showing how the SEBT cut-off point changes the probability of sustaining a lower extremity noncontact injury. A YBT-LQ composite reach score of <89 cm increases the probability from 37.7% to 68.0%. SEBT, Star Excursion Balance Test; YBT-LQ, Lower Quarter Y-Balance Test.
Discussion
Currently, there is a paucity of literature identifying movement-related testing that screens for American football players at an elevated risk for injury.11,21,25 The results of this study suggest that an easily administered dynamic balance test during preseason was successful in identifying players who sustained an injury over the course of the season.
The findings of the current study support the hypothesis that poorer performance on dynamic balance tests is associated with an elevated injury risk.2,13,17 However, prior to the current study, this construct had not been established in American football players. The results of this study suggest that poor dynamic balance performance, as determined on the SEBT using the YBT-LQ protocol, is associated with an increased risk for a noncontact lower extremity injury in college football players. The current study adds to the external validity of the SEBT as a potential successful injury prediction tool.
During the current study, football players who had a composite SEBT score of less than 89% were at an elevated risk of injury. Athletes with a positive SEBT result (<89% limb length composite score) had a substantially shifted probability of sustaining a noncontact lower extremity injury (37.7%-68.1%). The high sensitivity (100%) indicates that when the SEBT was used with this population, it helped to rule out the increased risk of sustaining a noncontact lower extremity injury, and thus, it may be considered a helpful injury screening tool in the collegiate football athlete. The results of this study are consistent with previous work on the SEBT in high school female basketball players.13 The prior study observed that female players that scored in the lower third (<94% leg length) were 6.5 times as likely to sustain a musculoskeletal injury. Plisky et al17 observed that >4 cm asymmetry on the anterior reach was associated with an elevated injury risk. The current study did not observe a significant change in the noncontact lower extremity injury risk as a result of reach direction asymmetries. It is important to note that the cut-off point for elevated injury risk in the current study in college football players was different than the risk cut-off point in the high school basketball players (effect size = 0.71). This finding suggests that there may be a need for population-specific cut-off points to be developed to screen for injury risk in athletes during preseason.
In contrast to our findings, one of the most consistent risk factors for injury across epidemiologic studies in sports is previous injury; however, this was not observed in the present study.7,23,24,26 One potential explanation for this conflicting finding could be the study’s inclusion criteria of no injury in the past 6 months. Another possible explanation is our injury definition, which was specific to noncontact lower extremity injuries. The authors chose to adopt a more specific definition of injury focusing on the noncontact mechanism based on reports that suggest that neuromuscular control is a modifiable intrinsic risk factor.6,10 Finally, this relationship may reach significance in a larger sample study; however, it was underpowered in this smaller cohort.
The primary limitation of the current study is limited external validity due to the specific population examined. This limitation is lessened because of the prior finding of poor dynamic balance being associated with noncontact injury in high school basketball players and in a general recreational population.2,17 Another limitation of the current study was the high false positive rate. However, even with the false positive rate, the number of athletes identified at an elevated injury risk provided a more manageable number for intervention development as opposed to developing individualized programs for each member of the team. It is possible that the addition of other screening tests to develop a multifactorial injury assessment may reduce the number of false positives. Exclusion criteria should have included athletes with a previous injury up to 1 year prior to the study to improve the robustness of this variable since prior research has observed movement deficits up to this point in time. Finally, the small sample size of the study limits the breadth of the external validity. It is necessary to reproduce this study in a larger population to validate the findings of this initial work. Future studies should examine similar constructs across multiple institutions and multiple populations to maximize the external validity of the findings of such a study. These studies should also examine athlete exposures as well as look at multifactorial models for injury prediction.
Current models of screening for the readiness of participation typically do not include movement-based measures associated with an elevated risk for musculoskeletal injury.1 This is often due to the fact that screening measures are required to be sport, sex, and age specific. The results of this study, in combination with prior work, suggest that the SEBT may be an effective screening test in multiple sports since the test requires unilateral stance performance at the limit of stability, which may likely incorporate a number of the components of motor control that are common requirements for all sports. The YBT-LQ protocol of the SEBT takes 5 minutes to administer following adequate warm-up trials, which can be performed in a group setting,18 thus minimizing the time cost associated with integrating the test. It would seem beneficial to add the SEBT into a preseason screening to identify athletes who are at an elevated risk for sustaining a noncontact musculoskeletal injury. Since the SEBT is predictive of injury and identifies deficits with knee and ankle injury, it may be useful in return-to-sport testing.
Conclusion
The SEBT, using the YBT-LQ protocol, may be a time-efficient method to identify college football players at risk for developing a noncontact musculoskeletal injury to the lower extremity.
Acknowledgments
The authors thank Jessica Fry and Ellen Pitman for their technical assistance and data entry for this article and the Sports Medicine Departments of Lebanon Valley College for their role in injury surveillance throughout this study.
Footnotes
The following authors declared potential conflicts of interest: Kyle B. Kiesel, PT, PhD, ATC, has ownership in Move2perform LLC; and Phillip J. Plisky, PT, DSc, ATC, has received grants or has grants pending from the Henry M. Jackson Foundation and has received payment for lectures and has patents pending for Move2Perform, LLC and FunctionalMovement, LLC.
References
- 1. Carek PJ, Hunter L. The preparticipation physical examination for athletics: a critical review of current recommendations. J Med Liban. 2001;49:292-297 [PubMed] [Google Scholar]
- 2. de Noronha M, Franca LC, Haupenthal A, Nunes GS. Intrinsic predictive factors for ankle sprain in active university students: a prospective study [published online January 20, 2012]. Scan J Med Sci Sports. 10.1111/j.1600-0838.2011.01434.x [DOI] [PubMed] [Google Scholar]
- 3. Gomez JE, Ross SK, Calmbach WL, Kimmel RB, Schmidt DR, Dhanda R. Body fatness and increased injury rates in high school football linemen. Clin J Sports Med. 1998;8:115-120 [DOI] [PubMed] [Google Scholar]
- 4. Herrington L, Hatcher J, Hatcher A, McNicholas M. A comparison of Star Excursion Balance Test reach distances between ACL deficient patients and asymptomatic controls. Knee. 2009;16:149-152 [DOI] [PubMed] [Google Scholar]
- 5. Hertel J, Braham RA, Hale SA, Olmsted-Kramer LC. Simplifying the Star Excursion Balance Test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther. 2006;36:131-137 [DOI] [PubMed] [Google Scholar]
- 6. Hewett TE, Myer GD, Ford KR. Reducing knee and anterior cruciate ligament injuries among female athletes; a systematic review of neuromuscular training interventions. J Knee Surg. 2005;18:82-88 [DOI] [PubMed] [Google Scholar]
- 7. Hjelm N, Werner S, Renstrom P. Injury risk factors in junior tennis players: a prospective 2-year study. Scand J Med Sci Sports. 2012;22:40-48 [DOI] [PubMed] [Google Scholar]
- 8. Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train. 2007;42:311-319 [PMC free article] [PubMed] [Google Scholar]
- 9. Kerr ZY, Collins CL, Fields SK, Comstock RD. Epidemiology of player-player contact injuries among US high school athletes, 2005-2009. Clin Pediatr (Phila). 2011;50:594-603 [DOI] [PubMed] [Google Scholar]
- 10. Kiesel KB, Plisky PJ, Butler RJ. Functional movement test scores improve following an off-season intervention program in professional football players. Scand J Med Sci Sports. 2009;21:287-292 [DOI] [PubMed] [Google Scholar]
- 11. Kiesel K, Plisky PJ, Voight ML. Can serious injury in professional football be predicted by a preseason functional movement screen. N Am J Sports Phys Ther. 2007;2:147-158 [PMC free article] [PubMed] [Google Scholar]
- 12. Krivickas L, Feinberg J. Lower extremity injuries in collegiate athletes: relation between ligamentous laxity and muscle tightness. Arch Phys Med Rehabil. 1996;77:1139-1143 [DOI] [PubMed] [Google Scholar]
- 13. McGuine T. Sports injuries in high school athletes: a review of injury-risk and injury-prevention research. Clin J Sports Med. 2006;16:488-499 [DOI] [PubMed] [Google Scholar]
- 14. Meyers MC. Incidence, mechanisms, and severity of game-related college football injuries on FieldTurf versus natural grass: a 3-year prospective study. Am J Sports Med. 2010;38:687-697 [DOI] [PubMed] [Google Scholar]
- 15. Plisky PJ, Gorman PP, Butler RJ, Keisel KB, Rauh MJ. Comparison of performance on the Star Excursion Balance Test by sport, competition level, and gender. Paper presented at Combined Sections Meeting of the American Physical Therapy Association; 2009; Las Vegas, NV [Google Scholar]
- 16. Plisky PJ, Gorman PP, Butler RJ, Kiesel KB, Underwood FB, Elkins B. The reliability of an instrumented device for measuring components of the Star Excursion Balance Test. N Am J Sports Phys Ther. 2009;4:92-99 [PMC free article] [PubMed] [Google Scholar]
- 17. Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther. 2006;36:911-919 [DOI] [PubMed] [Google Scholar]
- 18. Sefton J, Hicks-Little C, Hubbard T, et al. Sensorimotor function as a predictor of chronic ankle instability. Clin Biomech (Bristol, Avon). 2009;24:451-458 [DOI] [PubMed] [Google Scholar]
- 19. Shankar PR, Fields SK, Collins CL, Dick RW, Comstock RD. Epidemiology of high school and collegiate football injuries in the United States, 2005-2006. Am J Sports Med. 2007;35:1295-1303 [DOI] [PubMed] [Google Scholar]
- 20. Swenson DM, Henke NM, Collins CL, Fields SK, Comstock RD. Epidemiology of United States high school sports-related fractures, 2008-09 to 2010-11. Am J Sports Med. 2012;40:2078-2084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Turbeville SD, Cowan LD, Owen WL, Asal NR, Anderson MA. Risk factors for injury in high school football players. Am J Sports Med. 2003;31:974-980 [DOI] [PubMed] [Google Scholar]
- 22. Tyler TF, McHugh MP, Mirabella MR, Mullaney MJ, Nicholas SJ. Risk factors for noncontact ankle sprains in high school football players: the role of previous ankle sprains and body mass index. Am J Sports Med. 2006;34:471-475 [DOI] [PubMed] [Google Scholar]
- 23. Venturelli M, Schena F, Zanolla L, Bishop D. Injury risk factors in young soccer players detected by a multivariate survival model. J Sci Med Sport. 2011;14:293-298 [DOI] [PubMed] [Google Scholar]
- 24. Wen DY. Risk factors for overuse injuries in runners. Curr Sports Med Rep. 2007;6:307-313 [PubMed] [Google Scholar]
- 25. Yard E, Comstock D. Injury patterns by body mass index in US high school athletes. J Phys Act Health. 2011;8:182-191 [DOI] [PubMed] [Google Scholar]
- 26. Zazulak BT, Hewett TE, Reeves NP, Goldberg B, Cholewicki J. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiological study. Am J Sports Med. 2007;35:1123-1130 [DOI] [PubMed] [Google Scholar]


