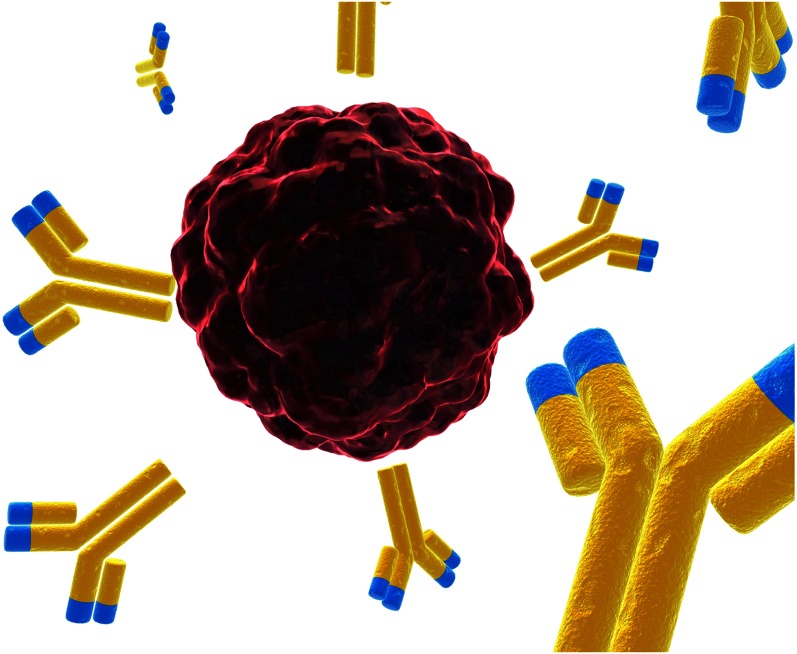
Antibodies (yellow and blue) can be engineered to carry a cytotoxic drug and deposit it in the target cell. © iStockphoto.com/Eraxion.
Ideally, targeted therapies attack diseased cells while leaving healthy ones alone. It’s a strategy that could result in more effective treatments for cancer (or other diseases) with fewer toxic side effects than traditional chemotherapies. A burgeoning class of targeted therapies, called antibody–drug conjugates (ADC), deliver dual therapies in a single, cancer cell-killing package.
An ADC contains two parts: a monoclonal antibody and a small amount of a highly potent cytotoxic drug, linked to the antibody. Like a key sliding into a lock, the ADC’s antibody binds with a particular receptor on the target cell’s surface. Then the linkage breaks, and the ADC releases a lethal toxin into the cell.
Monoclonal antibodies are laboratory-made imitators of the body’s own immune system, and researchers are looking for ways to specifically match the antibodies to those found on diseased cells. Monoclonal antibodies have already been used to treat autoimmune diseases and as cancer therapies in drugs, such as Cetuximab (brand name Erbitux), used to treat metastatic colorectal cancer and head and neck cancers, and Trastuzumab (brand name Herceptin), prescribed to treat some breast and gastric cancers. Both drugs are designed to block a diseased cell’s ability to receive certain chemical signals that tell it to grow. The second part of the ADC is the potent drug attached to the monoclonal antibody.
In 2011, brentuximab vedotin (brand name Adcetris) became the first Food and Drug Administration (FDA)-approved ADC and, remarkably, the first new FDA-approved therapy for Hodgkin lymphoma in more than three decades (1). (Adcetris is also the first therapy specifically approved for anaplastic large-cell lymphoma.) The phase II clinical trial was small but promising: of 102 Hodgkin lymphoma patients treated with the new drug, 32% had complete remission for 20.5 months on average, which meant all detectable traces of the tumor disappeared during that time. An additional 40% of patients had partial remission—where the tumor shrank by more than half—for 3.5 months on average (2). The antibody in Adcetris is nearly ineffective on its own, and its potent poison is far too toxic to be used on its own. Only in combination do the two parts safely give the drug its punch.
Other ADCs are coming down the pipeline. In February 2013, the FDA approved ado-trastuzumab emtansine (brand name Kadcyla) for patients with metastatic HER2-positive breast cancer. The drug uses the Herceptin antibody to deliver a chemotherapeutic drug that’s being investigated in other ADCs as well. In clinical trials, the drug provided benefits even to those patients whose disease has become resistant to Herceptin acting alone (3).
Early clinical studies suggest evidence for optimism, but many hurdles remain. Researchers face pressure both inside and outside the laboratory. Inside, researchers have to find the right combination of drugs and a stable conjugate to use as a linker, as well as antibodies that flag cancer cells while leaving healthy cells alone. Outside the laboratory, researchers must identify the subgroup of cancer patients most likely to respond favorably. History offers a warning, too: In 2000, the FDA approved an ADC called Mylotarg for patients with acute myeloid leukemia. However, in June 2010 the drug’s manufacturer, Pfizer, pulled the drug after follow-up studies showed that the drug did not extend survival and was associated with a high rate of fatal toxicity (4).
References
- 1. FDA (2011) FDA news release: “FDA approves Adcetris to treat two types of lymphoma.” Available at www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm268781.htm. Accessed September 15, 2012.
- 2.Younes A, et al. Results of a pivotal phase II study of brentuximab vedotin for patients with relapsed or refractory Hodgkin’s lymphoma. J Clin Oncol. 2012;30(18):2183–2189. doi: 10.1200/JCO.2011.38.0410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Verma S, et al. EMILIA Study Group Trastuzumab emtansine for HER2-positive advanced breast cancer. N Engl J Med. 2012;367(19):1783–1791. doi: 10.1056/NEJMoa1209124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. FDA (2010) FDA news Release: “Pfizer voluntarily withdraws cancer treatment Mylotarg from U.S. market.” Available at www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm216448.htm. Accessed September 15, 2012.