Abstract
Objective
To investigate long-term body mass index (BMI) changes with childbearing.
Design and Methods
Adjusted mean BMI changes were estimated by race-ethnicity, baseline BMI and parity using longitudinal regression models in 3943 young females over 10 and 25 year follow-up from the ongoing 1979 National Longitudinal Survey of Youth cohort. Results: Estimated BMI increases varied by group, ranging from a low of 2.1 BMI units for white, non-overweight nulliparas over the first 10 years to a high of 10.1 BMI units for black, overweight multiparas over the full 25-year follow-up. Impacts of parity were strongest among overweight multiparas and primaparas at ten years, ranges 1.4–1.7 and 0.8–1.3 BMI units, respectively. Among non-overweight women at 10 years, parity-related gain varied by number of births among black and whites but was unassociated in Hispanic women. After 25 years, childbearing significantly increased BMI only among overweight multiparous black women.
Conclusion
Childbearing is associated with permanent weight gain in some women, but the relationship differs by maternal BMI in young adulthood, number of births, race-ethnicity and length of follow-up. Given that overweight black women may be at special risk for accumulation of permanent, long-term weight after childbearing, effective interventions for this group are particularly needed.
Over half of U.S. women of childbearing age are overweight or obese, with the prevalence among Hispanics and non-Hispanic blacks reaching 70% (1). Pregnancy may contribute to obesity in women and serve as a potentially modifiable point for interventions (2). Moderate evidence suggests that excessive gestational weight gain increases postpartum weight retention up to 3 years after delivery, but results of longer investigations of parity and BMI in U.S. women are inconsistent, in part due to different study designs and follow up times (3). To our knowledge, no U.S. study of weight gain by parity has reported follow-up time of greater than 10 years and included Hispanic women. This paper compares BMI changes for nulliparous, primiparous and multiparous women in the United States 1979 National Longitudinal Survey of Youth (NLSY79) by race/ethnicity and baseline BMI, at 25 and 10 years after baseline.
METHODS
The NLSY79 is an ongoing nationally representative cohort born between 1957 and 1964. Detailed information on recruitment, sampling methods and study procedures have been published previously (http://www.bls.gov/nls) (4). The University of California, Berkeley Office for the Protection of Human Subjects waived the requirement for formal review because the dataset is unidentifiable and publicly available.
Of the 6061 enrolled NSY females, aged 14–21, in 1979, our analytical sample included 4015 nulliparous women with data collected on height and weight in 1981 and ≥ 1 non-pregnant follow-up weight measurement. After excluding 72 with missing baseline covariates, our sample of 3943 was less likely to be Hispanic or black, married, living in poverty at baseline, and have parents with 12 or fewer years of education. In 1990, 776 individuals were systematically dropped from follow up and an additional 752 women (19% of the original analytical sample) were lost to follow-up over 25 years. Table 1 shows that for each race-ethnicity group, parental education, the non-time varying baseline variable, remained consistent over time suggesting that loss to follow-up did not substantially change sample characteristics.
Table 1.
Demographic and Health-Related Characteristics of Analytical Samplea, According to Race/ethnicity in 1981, 1992, and 2006b, National Longitudinal Study of Youth.
| Characteristic | 1981 (N = 3943) | 1992 (N = 2649) | 2006 (N = 2415) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Whitec | Hispanic | Black | White | Hispanic | Black | White | Hispanic | Black | |
| 64.2d (2533) | 15.2 (601) | 20.5 (809) | 57.4 (1521) | 18.8 (499) | 23.7 (629) | 57.9 (1398) | 17.6 (426) | 24.5 (591) | |
| Mean (SD) | |||||||||
| Age, years | 20.1 (2.3) | 19.6 (2.2) | 19.6 (2.2) | 31.3 (2.1) | 30.9 (2.2) | 30.9 (2.1) | 44.9 (2.1) | 44.6 (2.2) | 44.6 (2.1) |
| Weight, kg | 57.8 (9.8) | 55.9 (8.9) | 60.8 (12.0) | 65.7 (14.6) | 65.7 (14.6) | 73.1 (17.5) | 72.8 (17.0) | 73.7 (16.8) | 82.2 (19.9) |
| Height, cm | 164.1 (6.8) | 159.8 (6.8) | 163.3 (8.0) | 164.3 (6.8) | 159.8 (6.7) | 163.4 (7.9) | 164.4 (6.7) | 159.9 (7.0) | 163.6 (8.0) |
| Body Mass Indexf | 21.5 (3.4) | 21.9 (3.3) | 22.9 (4.6) | 24.3 (5.3) | 25.7 (5.6) | 27.4 (6.7) | 26.9 (6.1) | 30.8 (7.6) | 28.8 (6.5) |
| % (n) | |||||||||
| <18.5 | 9.7 (247) | 7.6 (46) | 8.4 (68) | 3.1 (47) | 1.0 (5) | 3.5 (22) | 0.8 (11) | 0.2 (1) | 0.8 (5) |
| 18.5–24.9 | 76.5 (1937) | 71.6 (430) | 68.0 (550) | 59.0 (898) | 45.8 (229) | 34.3 (216) | 39.5 (552) | 23.0 (98) | 17.8 (105) |
| 25.0–29.9 | 10.0 (252) | 17.3 (104) | 15.7 (127) | 23.3 (355) | 30.3 (151) | 28.6 (180) | 29.7 (416) | 35.7 (152) | 30.3 (179) |
| ≥30 | 3.8 (96) | 3.5 (21) | 7.9 (64) | 14.5 (221) | 22.9 (114) | 33.5 (211) | 30.0 (419) | 41.1 (175) | 51.1 (302) |
| Parity | |||||||||
| 0 | 100 (2533) | 100 (601) | 100 (809) | 40.7 (619) | 35.3 (176) | 40.5 (255) | 22.3 (311) | 18.8 (80) | 28.6 (169) |
| 1 | 0 (0) | 0 (0) | 0 (0) | 23.2 (353) | 23.0 (115) | 23.9 (150) | 18.5 (259) | 17.1 (73) | 21.5 (127) |
| ≥2 | 0 (0) | 0 (0) | 0 (0) | 36.1 (549) | 41.7 (208) | 35.6 (224) | 59.2 (828) | 64.1 (273) | 49.9 (295) |
| Marital status | |||||||||
| Never married | 83.3 (2110) | 86.5 (520) | 93.6 (757) | 19.3 (294) | 27.9 (129) | 46.1 (290) | 8.0 (112) | 16.0 (68) | 31.3 (185) |
| Has married | 16.7 (423) | 13.5 (81) | 6.4 (52) | 80.7 (1227) | 72.1 (360) | 53.9 (339) | 92.0 (1286) | 84.0 (358) | 68.7 (406) |
| Parental educatione | |||||||||
| < 12 years | 18.5 (470) | 54.9 (330) | 40.4 (327) | 15.8 (240) | 54.7 (273) | 41.2 (259) | 15.5 (216) | 55.2 (235) | 41.8 (247) |
| 12 years | 42.8 (1083) | 27.5 (165) | 35.7 (289) | 44.0 (670) | 28.3 (141) | 36.6 (230) | 43.7 (611) | 27.9 (119) | 35.5 (210) |
| > 12 years | 38.7 (980) | 17.6 (106) | 23.9 (193) | 40.2 (611) | 17.0 (85) | 22.2 (140) | 40.8 (571) | 16.9 (72) | 22.7 (134) |
| Family poverty status | |||||||||
| Not in poverty | 86.7 (2195) | 75.5 (454) | 68.0 (550) | 92.7 (1410) | 84.4 (421) | 76.9 (484) | 92.4 (1292) | 85.9 (366) | 80.9 (478) |
| In poverty | 13.3 (338) | 24.5 (147) | 32.0 (259) | 7.3 (421) | 15.6 (78) | 23.1 (145) | 7.6 (106) | 14.1 (60) | 19.1 (113) |
Results in this table were for the unweighted analytic sample.
The analytical sample used for this table included women with complete data at baseline. For 1992 and 2006, the results describe the subset of women with available weight for that year.
White ethnicity includes other categories.
Mean (standard deviation) or percent (n).
Parental education was defined as the highest level of education achieved by either parent.
Weight (kg)/height (m)2
To address systematic underestimation of self-reported weight and height, we analyzed the data with and without regression calibration based on NHANES (5). Women were categorized by baseline age and BMI; non-overweight (≥ 20 years old: BMI < 25 kg/m2; < 20 years old: BMI < 85th percentile) and overweight (≥ 20 years old: BMI = 25 kg/m2; < 20 years old: BMI = 85th percentile). (6,7) Parity (number of live births 0,1 or ≥ 2) after baseline was calculated from the NLSY79 Child and Young Adult survey (8).
The NLSY79 categorizes self-reported race/ethnicity as non-Hispanic black, Hispanic, and non-Hispanic white/other (less than 6% classified as Asian, Pacific Islander, Native American, and other). Potential confounding variables were chosen a priori and included the highest grade completed by either parent (<12 years, 12 years, >12 years) and time-varying poverty status (dichotomized variable determined by total family income and participation in public assistance programs) and marital status (never married or married).
We used a regression model to examine our primary outcome of the mean BMI change from baseline. A quadratic term for age was included to reflect the non-linear shape of the BMI-age relationship. Time-dependent parity groups were included to estimate changes associated with childbearing. To account for repeated measures in our data, we used generalized estimating equations (GEE) to estimate model coefficients and applied the NLSY79 custom sampling weights to make the sample nationally representative (4). Fully adjusted models include baseline and time-dependent covariates and several sets of a priori two-way interactions. Mean BMI at ages 20, 30, and 45 years was estimated for time-dependent parity groups by baseline BMI and race-ethnicity, assuming constant covariates.
RESULTS
Of the 2415 women followed the entire 25 years, 1855 had one or more births during the study period and 560 remained nulliparous. The prevalence of obesity between 1981 and 2006 increased from 3.8% to 30% (white/other), 3.5% to 41.1% (Hispanics) and 14.5% to 51.1% (blacks).(Table 1)
There were significant interactions in weight change between baseline BMI, parity category, and age at follow-up. Total adjusted BMI increases ranged from 2.1 kg/m2 (non-overweight white nulliparas) to 6.44 kg/m2 (overweight black multiparas) in the first 10 years; a similar pattern with greater magnitude (5.15 and 10.09 kg/m2, respectively) was seen after 25 years. Black women gained the significantly more weight than white women in each BMI and parity category, with Hispanic women falling in between.
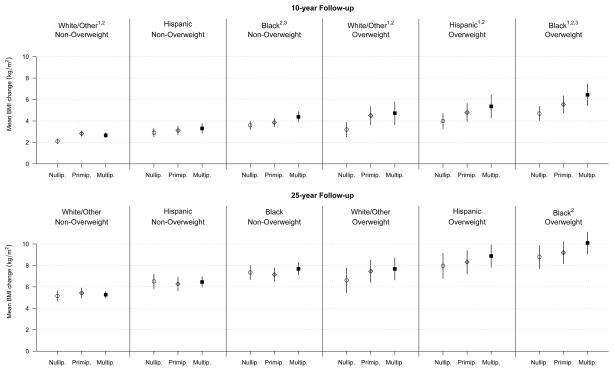
Figure 1 and Table 2 show that primparas and multiparas tended to have greater BMI increases than nulliparas. After ten years, BMI increased with childbearing in all three race-ethnicity groups that were overweight at baseline. The relationship was inconsistent for those not overweight at baseline, with modest but still significant BMI increases in white women and multiparous black women, but no increases in primiparous blacks or childbearing Hispanics. After 25 years, the only statistically significant increase in BMI associated with childbearing was observed in black multiparas who were overweight at baseline. Comparison of BMI changes within childbearing women suggest that generally primiparas gained similarly to multiparas, except black multiparas in both BMI groups gained significantly more weight than primiparas in the first 10 years.
Figure 1.
Ten and Twenty-five Year Average Body Mass Index Increasea for Parity Groups from Repeated Measures Linear Regression Modelb by Race and Baseline BMIc Groups.
Abbreviations: BMI, body mass index
1P < 0.05 (2-tailed Wald tests comparing BMI gain between primiparas and nulliparas).
2P < 0.05 (2-tailed Wald tests comparing BMI gain between multiparas and nulliparas).
3 P < 0.05 (2-tailed Wald tests comparing BMI gain between primiparas and multiparas).
a BMI increase was modeled for time-dependent follow-up live birth categories as the difference in BMI increase as compared to zero live births since baseline.
b Marginal longitudinal model adjusted for age, age2, poverty status, parental education, and marital status as well as two-way interactions between covariates of interest (race-ethnicity and baseline BMI) with follow-up parity groups and maternal age and between parity and maternal age.
c Baseline groups consist of baseline body mass index categories (Non-overweight, < 25; Overweight ≥ 25).
d Weight (kg)/height (m)2.
Table 2.
Ten and Twenty-five Year Average Body Mass Index Increase Attributable to Parity from Repeated Measures Linear Regression Modelb Stratified by Race and Baseline BMIc Groups
| BMI < 25 | BMI ≥ 25 | |||
|---|---|---|---|---|
| BMI Increased | 95% CI | BMI Increase | 95% CI | |
| 10 year Follow-up | ||||
| White/Other | ||||
| Nulliparous (referent) | ||||
| Primiparous | 0.72 | 0.52, 0.93 | 1.30 | 0.58, 2.02 |
| Multiparous | 0.56 | 0.35, 0.78 | 1.52 | 0.44, 2.60 |
| Hispanic | ||||
| Nulliparous (referent) | ||||
| Primiparous | 0.21 | −0.17, 0.59 | 0.79 | 0.02, 1.55 |
| Multiparous | 0.40 | −0.11, 0.91 | 1.36 | 0.25, 2.47 |
| Black | ||||
| Nulliparous (referent) | ||||
| Primiparous | 0.26 | −0.15, 0.67 | 0.84 | 0.10, 1.57 |
| Multiparous | 0.79* | 0.21, 1.36 | 1.74* | 0.69, 2.80 |
| 25 year Follow-up | ||||
| White/Other | ||||
| Nulliparous (referent) | ||||
| Primiparous | 0.28 | −0.28, 0.83 | 0.85 | −0.03, 1.73 |
| Multiparous | 0.12 | −0.36, 0.60 | 1.07 | −0.10, 2.25 |
| Hispanic | ||||
| Nulliparous (referent) | ||||
| Primiparous | −0.24 | −0.83, 0.35 | 0.34 | −0.54, 1.22 |
| Multiparous | −0.05 | −0.66, 0.57 | 0.91 | −0.26, 2.08 |
| Black | ||||
| Nulliparous (referent) | ||||
| Primiparous | −0.19 | −0.80, 0.43 | 0.39 | −0.47, 1.25 |
| Multiparous | 0.34 | −0.32, 1.00 | 1.30* | 0.18, 2.41 |
P < 0.05 (2-tailed Wald tests comparing weight gain between primiparas and multiparas.
BMI increase was modeled for time-dependent follow-up live birth categories as the difference in BMI increase as compared to zero live births since baseline.
Marginal longitudinal model adjusted for age, age2, poverty status, parental education, and marital status as well as two-way interactions between covariates of interest (race-ethnicity and baseline BMI) with follow-up parity groups and maternal age and between parity and maternal age.
Baseline groups consist of baseline body mass index categories (Normal, < 25; Overweight ≥ 25).
Weight (kg)/height (m)2.
DISCUSSION
Findings from this nationally representative cohort suggest that childbearing is associated with increased weight gain, but the strength of the relationship may vary considerably by baseline body size, race/ethnicity, parity, and length of follow-up.
Our results for 10 years after baseline agree with, extend and differ from previous studies. Consistent with other cohorts (9–12), white and black NLSY multiparous women who were overweight at baseline gained more weight than nulliparas; our study adds new knowledge that parity is also associated with increased gain in Hispanic women with these characteristics. In the non-overweight group, parity was not associated with BMI increase in Hispanic women; however, BMI did increase with childbearing for white women and for multiparous black mothers. Similar to results reported by the CARDIA study (12) and in contrast to data from the older National Health and Nutrition Examination Survey (11), we found that overall adjusted weight change in NLSY varied by race, but there was no evidence that black women gained more parity-associated weight than white women.
Previous evidence up to 10 years suggests that long-term maternal weight gain is established with the first birth and not increased with additional pregnancies (3,9,12). Our ten-year follow up results for white women and overweight Hispanic women confirm this view. However, the reverse was true for black mothers in both baseline BMI categories. Overall, these differences by baseline BMI, race/ethnicity and number of births over 10 years suggest a complexity that requires research to identify underlying mechanisms so that appropriate targeting and interventions can be applied.
Twenty-five years after baseline, parity was significantly associated with increased BMI in a single group: multiparous black women who were overweight at baseline. We identified no other studies comparing weight gain by childbearing with this length of follow-up, so these findings require confirmation in other samples.
The following limitations deserve mention. First, there was loss to follow up, but attrition was relatively low and our final sample reflected the baseline sample. Second, self-reported weight and height can underestimate BMI, but results did not change with regression calibration and our 10-year BMI and weight changes are similar to results of studies that measured weight and height (10,12). Third, other possible mediators (e.g., smoking, diet, physical activity, body composition, menopause) that may influence how parity affects BMI were unavailable in the NLSY79; however, many of our 10-year findings were consistent with the CARDIA results, which adjusted for diet, physical activity and waist circumference (12). Finally, we were unable to study high parity due to insufficient sample size.
Study strengths include a nulliparous comparison group; large subsamples of black and Hispanic mothers that allowed allow consideration of temporal trends, age and racial disparities and ability to adjust for a variety of potentially confounding variables. Our analysis of this prospective nationally representative cohort followed for 25 years is unique in estimating BMI change prospectively over the entire period of childbearing.
In summary, childbearing was associated with increased BMI over 10 years in women already overweight at baseline; increases were also observed in primiparous and multiparous normal weight and multiparous black though not Hispanic women. Body mass index increases after childbearing are concerning because increased adiposity contributes to adverse outcomes in subsequent pregnancies (2,13) and is a risk factor for development of chronic conditions, such as cardiovascular disease (14). Pregnant women and new mothers may be more health conscious and have greater contact with the health care system. The perinatal period should be a focus for interventions to prevent or reduce excessive weight gain during, after or between pregnancies (2,15), particularly for multiparous women who begin pregnancy overweight. Given that black women in this category may be at special risk for accumulation of permanent, long-term weight after childbearing, effective interventions for this group are particularly needed.
What is already known about this subject
Five US studies have compared long-term adult weight (Kg or BMI) change by parity, baseline BMI and race-ethnicity suggest that women with high baseline BMI (>25) and those with more than one birth are more likely to gain weight after childbearing.
However, differences by race-ethnicity and between primiparas and multiparas are less clear.
To our knowledge, no studies have compared childbearing and non-childbearing women for longer than 25 years in a diverse cohort and none include Hispanics.
What this study adds
In this nationally representative cohort, we confirm that white, black and Hispanic multiparous women with high BMI before pregnancy are more likely to gain weight with childbearing 10 years after baseline.
Parity is associated with significantly increased BMI in normal weight women as well, though results are less consistent by race and number of births, and Hispanic women did not gain significantly with childbearing.
To our knowledge this is the first study to report a 25-year follow-up. At 25 years, only black women who were overweight at baseline and delivered more than 1 child gained significantly more weight than those not giving birth.
Acknowledgments
BA and BH designed the study, analyzed the data and drafted the manuscript with BH responsible for data management and statistical analysis. ED and DR contributed to data analysis and interpretation. All authors were involved in writing the paper and had final approval of the submitted and published versions. The authors also acknowledge Allison Lindquist, MPH for her contribution to the literature review, Claire Margerision-Zilko, PhD for her contribution to data management and Alan Hubbard, Phd for statistical consultation.
Footnotes
Conflict of Interest
All authors declare no conflicts of interest.
Contributor Information
Barbara Abrams, University of California Berkeley, School of Public Health.
Brianna Heggeseth, University of California Berkeley, Department of Statistics.
David Rehkopf, Stanford University, School of Medicine.
Esa Davis, University of Pittsburgh, Division of General Internal Medicine.
References
- 1.Flegal KM, Carroll MD, Ogden CL, Curtin L. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010;303(3):235–41. doi: 10.1001/jama.2009.2014. [DOI] [PubMed] [Google Scholar]
- 2.Rasmussen KM, Yaktine AL, editors. Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines. Weight Gain During Pregnancy: Reexamining the Guidelines. Washington (DC): National Academies Press (US); 2009. [PubMed] [Google Scholar]
- 3.Gunderson EP. Childbearing and obesity in women: weight before, during, and after pregnancy. Obstet Gynecol Clin North Am. 2009;36(2):317–32. doi: 10.1016/j.ogc.2009.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Center for Human Resource Research. NLSY79 User’s Guide. Columbus: Center for Human Resource Research, Ohio State University; 2008. [Google Scholar]
- 5.Cawley J, Burkhauser RV. Working Paper no 12291. Cambridge, MA: National Bureau of Economic Research; 2006. Beyond BMI: The value of more accurate measures of fatness and obesity in social science research. [Google Scholar]
- 6.World Health Organization. [Accessed December 6, 2012];WHO: Global Database on Body Mass Index. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html)
- 7.US Centers for Disease Control and Prevention. Defining Childhood Overweight and Obesity. Atlanta: [Accessed June 2 2010]. ( http://www.cdc.gov/obesity/childhood/defining.html) [Google Scholar]
- 8.Bureau of Labor Statistics; U.S. Department of Labor and National Institute for Child Health and Human Development, editor. Children of the NLSY79, 1979–2002. Columbus: Center for Human Resource Research, The Ohio State University; 2002. [Google Scholar]
- 9.Rosenberg L, Palmer JR, Wise LA, Horton N, Kumanyika SK, Adams-Campbell L. A prospective study of the effect of childbearing on weight gain in African-American women. Obes Res. 2003;11(12):1526–35. doi: 10.1038/oby.2003.204. [DOI] [PubMed] [Google Scholar]
- 10.Wolfe WS, Sobal J, Olson CM, Frongillo EA, Williamson DF. Parity-associated weight gain and its modification by sociodemographic and behavioral factors: a prospective analysis in US women. Obes Res. 1997;5(2):131–41. doi: 10.1002/j.1550-8528.1997.tb00653.x. [DOI] [PubMed] [Google Scholar]
- 11.Williamson DF, Madans J, Pamuk E, Flegal K, Kendrick J, Serdula M. A prospective study of childbearing and 10-year weight gain in US white women 25 to 45 years of age. Int J of Obes Relat Metab Disord. 1994;18(8):561–9. [PubMed] [Google Scholar]
- 12.Gunderson EP, Murtaugh MA, Lewis CE, Quesenberry CP, West DS, Sidney S. Excess gains in weight and waist circumference associated with childbearing: The Coronary Artery Risk Development in Young Adults Study (CARDIA) Int J of Obes Relat Metab Disord. 2004;28(4):525–35. doi: 10.1038/sj.ijo.0802551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Villamor E, Cnattingius S. Interpregnancy weight change and risk of adverse pregnancy outcomes: a population-based study. Lancet. 2006;368(9542):1164–70. doi: 10.1016/S0140-6736(06)69473-7. [DOI] [PubMed] [Google Scholar]
- 14.Norman JE, Bild D, Lewis CE, Liu K, West DS. The impact of weight change on cardiovascular disease risk factors in young black and white adults: the CARDIA study. Int J Obes Relat Metab Disord. 2003;27(3):369–76. doi: 10.1038/sj.ijo.0802243. [DOI] [PubMed] [Google Scholar]
- 15.Phelan S. Pregnancy: a “teachable moment” for weight control and obesity prevention. Am J Obstet Gynecol. 2010;202:135.e1–8. doi: 10.1016/j.ajog.2009.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]