Abstract
Background
Improving clinicians' interest, confidence, and commitment in using evidence-based treatment (EBT) is often an aim of training clinicians in EBT. However, the degree to which these areas actually improve through training and what their relationship is to treatment integrity is unknown.
Method
Using data from a multi-site study (Martino et al., 2010) comparing three methods of clinician training in motivational interviewing (MI), changes in interest, confidence, and commitment over time and their relationship to MI adherence and competence were assessed using mixed-effects regression models. Individual patterns of change were examined through cluster analysis.
Results
Interest, confidence, and commitment declined over time across training conditions with two distinct patterns: 76% clinicians largely maintained strong interest in MI over time with only slight decreases in confidence and commitment (the “maintainers”), while 24% began with lower initial interest, confidence, and commitment, which subsequently declined over time (the “decliners”). Interest and commitment were not associated with MI adherence and competence; confidence was associated with increased competence in the use of advanced MI strategies. However, decliners demonstrated greater use of MI-inconsistent techniques than maintainers overall (d = 0.28).
Conclusions
Training in MI may have an unintended consequence of diminishing clinicians' interest, confidence, or commitment in using MI in practice. While attitudinal variables in this study show mixed relationships to MI integrity, they may have some utility in identifying less enthusiastic participants, better preparing them for training, or tailoring training approaches to meet individual training needs.
Keywords: clinician training, treatment integrity, adherence, motivational interviewing, dissemination, implementation
1. INTRODUCTION
The capacity of clinicians to learn and use evidence-based treatments (EBT) might be affected by their enthusiasm or attitude toward the EBT in which they are being trained (Damschroder and Hagedorn, 2011). Enthusiasm, as demonstrated by the clinician's self-reported interest, confidence, and commitment in using EBT, could influence the extent to which they are able to deliver the treatment with integrity, namely with sufficient adherence (use of therapeutic strategies consistent with the targeted treatment and minimization of interventions that would undermine its implementation) and competence (the skill or quality of implementation; Waltz et al., 1993). Examining the effect of training on attitudinal variables is considered a key component in training evaluation research (Damschroder and Hagedorn, 2011; Fixsen et al., 2005; Simpson, 2009). In this study, we examine the effect of training on clinicians' interest, confidence, and commitment in using motivational interviewing (MI; Miller and Rollnick, 2012) to help clients change substance abuse and examine the relationship of these attitudinal variables to the clinicians' MI adherence and competence.
Rogers (2003) described a process by which individuals adopt new interventions, beginning with increased knowledge of the intervention and then using this knowledge to form a favorable or unfavorable attitude toward the intervention. As most clinician training efforts include the presentation of theoretical knowledge about the EBT (MI: Madson et al., 2009; other EBT: Rakovshik and Manus, 2010), clinicians may then be expected to form attitudes about the EBT as they learn more about it. Studies that have examined changes in clinician interest, confidence, and commitment in using EBT after training have had largely positive results, with significant increases in clinician self-reported interest (Martino et al., 2007), confidence and commitment in using MI (Martino et al., 2007; Miller and Mount, 2001; Shafer et al., 2004) and other EBT (Dimeff et al., 2009; Jacobson et al., 2012). However, Miller and Mount (2001) found decreased interest in learning MI after training; participants indicated they felt they had learned the skills and no longer needed further training.
While self-reported interest, confidence, and commitment may change with EBT training, they may not correspond well to observer ratings of clinicians' abilities to deliver the EBT with integrity (Miller et al., 2006). For example, clinician's self-rated proficiency in MI has shown weak or nonsignificant correlations to observer-rated measures of MI integrity (Miller and Mount, 2001; Miller et al., 2004; Shafer et al., 2004). Similarly, more detailed self-rating treatment integrity checklists completed by clinicians after an EBT session show poor correspondence to independent observer-rated fidelity measures of the same session (Carroll et al., 1998; Hartzler et al., 2007; Martino et al., 2009). Possibly, self-reported attitudinal variables such as interest, confidence, and commitment in using an EBT may change during training with little relationship to clinicians' EBT proficiency.
Alternatively, attitudinal variables may be related to clinicians' abilities to benefit from training (Ball et al., 2002; Miller et al., 2006). For example, McGovern and colleagues (2004) found that clinicians who endorsed a disease model of addiction as their primary orientation were more likely than clinicians who did not have this allegiance to use a twelve-step facilitation approach and less likely to use MI, cognitive behavioral therapy, or behavioral couples counseling. Similarly, Baer and colleagues (2009) and Sholomskas and colleagues (2005) found that clinicians who endorsed greater disease model beliefs about treatment showed fewer gains in MI and cognitive behavioral therapy skills, respectively, although Miller and colleagues (2004) did not find that clinician attitudinal variables affected MI training outcomes.
This study examines changes in clinicians' interest in learning, confidence in their ability, and commitment to using MI in clinical practice, using data from a multi-site trial comparing strategies for training community substance abuse clinicians in MI (Martino et al., 2010). We hypothesized that clinician interest, confidence, and commitment in using MI would increase during training, and that gains would be maintained at follow-up. Next, we examined the associations of these variables with observer-rated clinician MI adherence and competence in client sessions, including identifying individual patterns of clinician changes in self-reported MI interest, confidence, and commitment, and the manner in which these patterns might influence their use of this treatment approach.
2. METHOD
2.1 Participants
Ninety-two clinicians from 12 outpatient substance abuse programs in the State of Connecticut, USA participated in the original study (see Martino et al., 2010 for demographic details). All participants were required to be employed at least 20 hours per week, treat English-speaking substance-using clients, agree to provide audiotaped client sessions that demonstrated their MI integrity at each assessment time point, and provide written informed consent as approved by the Yale University School of Medicine Human Investigation Committee. Of the 92 participants, 91 (99%) provided ratings of interest, confidence, and commitment for at least two assessment points and provided the data for the present report. Retention rates were good, with 82% participants providing data at 12-week follow-up. Sample sizes per time points were: baseline = 91; post-workshop = 91; post-supervision = 84; and 12-week follow-up = 75. Collection of audiotaped sessions varied (73% – 96%) depending on clinician compliance, operator error, and equipment failure, with a total of 25 missing audiotaped sessions across time points.
2.2. Procedures
2.2.1. Training Conditions
Details about the original study's aims, methods, and results have been published previously (Martino et al., 2010). Treatment programs were randomly assigned to one of three training conditions: 1) self-study in which clinicians only received training materials; 2) expert in which clinicians received a 15-hour workshop and three monthly supervision sessions from an expert in MI; and 3) train-the-trainer in which clinicians received the workshop and supervision training from program-based trainers prepared by the MI expert. Clinicians received the training strategy to which their program had been randomly assigned (self-study = 30; expert-led = 32; train-the-trainer = 29).
2.2.2. Audiotaped Sessions
Clinicians audiotaped 40-minute sessions in which they conducted MI with clients who had substance use problems. Clinicians, not research staff, selected clients based on clinical judgment of the suitability of substituting MI for their routine practice and the client's willingness to be audiotaped (signed consent obtained). Prior to the session, a research assistant gave the clinician written instructions that asked the clinician to motivate the selected client to change his or her substance use. Recorded client sessions were obtained at baseline and within 2 weeks of subsequent assessment time points.
2.2.3. Rater Training
Audiotaped sessions were rated by twelve raters using the Independent Tape Rater Scale (described below). Raters received approximately 44 hours of training in seminars and through practicing rating tapes with expert feedback (see Martino et al., 2010 for details).
2.2.4. Assessments
All clinicians completed assessments at baseline, post 15-hour workshop, following the 12-week supervision study phase, and at a 12-week follow-up point during which study-supported training had ended.
2.3. Measures
2.3.1. Independent Tape Rater Scale (ITRS)
The ITRS (see Martino et al., 2008 for item descriptions and full psychometric report) assesses community program clinicians' adherence and competence using MI, strategies inconsistent with MI (e.g., providing unsolicited advice), and strategies common to drug counseling (e.g., case management). For each strategy, a 7-point Likert-type scale is used to reflect strategy frequency or extensiveness (adherence; 1 = not at all, to 7 = extensively) and the skill with which the strategy is used (competence; 1 = very poor, to 7 = excellent). In a prior study, confirmatory factor analyses of the ITRS items (Martino et al., 2008) supported a two-factor solution for MI consistent items reflecting five fundamental MI strategies (e.g., reflective listening) and five advanced MI strategies (e.g., discussing pros, cons, and ambivalence). The fundamental and advanced MI items are averaged to yield factor scores representing fundamental adherence, fundamental competence, advanced adherence, and advanced competence scores. In addition, for this study five MI-inconsistent adherence item scores (unsolicited advice, therapeutic authority, direct confrontation, emphasizing total abstinence, asserting disease concepts of addiction) were averaged to determine the relationship of training outcomes to this area. Intraclass correlation coefficients (ICC; Shrout and Fleiss, 1979) for the fundamental and advanced MI strategy adherence and competence scores showed good to excellent inter-rater reliability (adherence ICC: fundamental = 0.88 and advanced = 0.87; competence ICC: fundamental = 0.88 and advanced = 0.68) (Cicchetti, 1994). Inter-rater reliability estimates for the MI-inconsistent adherence score was excellent (ICC = .91).
2.3.2. Clinician Rulers
Clinicians rated their interest, confidence, and commitment in using MI in clinical practice (0 = not at all, to 10 = extremely). The rulers showed significant increases (pre-post) in each of these three dimensions in a prior MI training study (Martino et al., 2007).
2.3.3. Clinician Survey
This baseline survey (Ball et al., 2002) evaluated a broad array of clinician characteristics (e.g., demographic, educational and professional experiences, treatment allegiance), including recovery status. Treatment allegiance was assessed by asking clinicians to rate how well different addiction treatment approaches (e.g., twelve-step or disease concept; cognitive-behavioral; motivational interviewing) describe their own approach to treatment, using a 5-point Likert-type scale. Recovery status was assessed by asking clinicians if they considered themselves to be a person in recovery from drug or alcohol abuse (yes/no). The Clinician Survey has been used in several other MI trials documenting clinician characteristics (Ball et al., 2007; Carroll et al., 2006; 2009; Martino et al., 2011).
2.4. Data Analysis
We used mixed-effects regression models to test the hypotheses that clinician interest, confidence, and commitment in using MI would increase over time. Separate analyses were conducted for each self-reported outcome, with time (baseline, post-workshop, post-supervision, follow-up), training condition (self-study, expert-led, train-the-trainer), and their interaction entered as fixed factors and clinician as a random factor. Time was entered as a fixed categorical variable with four assessment time points and an AR1 covariance structure, assuming that performance at two adjacent points in time (e.g., baseline to post-workshop) would be more similar than performance at more distant points in time (e.g., baseline to post-supervision). Because the sample size precluded a four-level model (time, clinician, program site, training condition) that included program site as a factor, analyses with the effects of time, program site, and their interaction were run without training condition as a factor to examine the potential effects of program site on interest, confidence, and commitment.
Next, we examined the relationship of self-reported outcomes to clinician MI performance. We conducted separate mixed-effects regression models with clinician performance in MI (fundamental and advanced adherence and competence, MI-inconsistent behavior) as the outcome and time, training condition, and their interaction as fixed factors and clinician as a random factor. We then repeated these analyses with the addition of the clinician self-reported outcomes (interest, confidence, and commitment, each variable centered around its mean) as fixed-factor covariates, referred to the enhanced model. Chi-squares were calculated to compare the −2 log likelihood values for the respective basic and enhanced models. A significant chi-square comparison would indicate that the addition of the covariates improved the predictive value of the model (Tabachnick and Fidell, 2007).
Finally, we conducted exploratory analyses to identify patterns of individual change in interest, confidence, and commitment. Scores on interest, confidence, and commitment over time were subject to hierarchical cluster analysis, using Ward's method to establish initial clusters and squared Euclidian distance as the similarity measure. Agglomeration coefficients were evaluated for solutions of two to nine clusters and plotted as recommended by Morey and colleagues (1983). This method and interpretability were used to determine the number of clusters. A K-means cluster analysis was conducted using the specified number of clusters to cross-validate the groups and to allow for the inclusion of clinicians with missing data points. Cluster stability was tested through chi-square analysis on the percentage of cases assigned to the same cluster by both procedures. Descriptive analyses on the groups of clinicians identified through K-means clusters were conducted to examine clinician characteristics associated with patterns of change. As above, mixed-effects regression models for fundamental and advanced MI adherence and competence and MI-inconsistent behavior were repeated with cluster identity as an additional fixed factor in the model to determine whether a clinician's pattern of change in self-reported outcomes was associated with MI performance over time.
3. RESULTS
3.1. Change over time
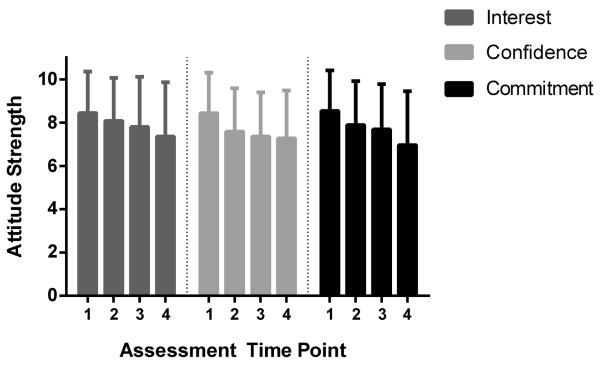
Table 1 displays the overall and respective mean values for interest, confidence, and commitment for each training condition. Each variable was high at baseline across conditions (between 8 to 9 out of 10) and significantly declined over time (Figure 1). Table 2 presents mixed-effects models for interest, confidence, and commitment and indicates change over time for each variable, with no significant differences by training condition. Analyses examining the potential effects of program site on interest, confidence, and commitment in relationship to time (available on request from the senior author) showed no significant site effects, consistent with the finding of a lack of significant site effects on clinician MI adherence and competence in the main trial (Martino et al., 2010).
Table 1.
Descnptives for interest, confidence, and commitment in using MI
| Baseline | Post-workshop | Post-supervision | 12-week Follow-up | ||
|---|---|---|---|---|---|
| Condition | M (SD) | M (SD) | M (SD) | M (SD) | |
| Interest | SS | 8.63 (1.90) | 8.47 (1.83) | 8.34 (2.41) | 7.64 (2.74) |
| EX | 8.59 (1.10) | 8.16 (1.46) | 8.03 (1.89) | 7.48 (1.98) | |
| TT | 8.07 (2.56) | 7.59 (2.51) | 6.78 (2.49) | 6.79 (2.94) | |
| All | 8.44 (1.92) | 8.08 (1.98) | 7.80 (2.31) | 7.36 (2.50) | |
| Confidence | SS | 8.63 (1.54) | 8.10 (1.85) | 7.90 (2.32) | 7.04 (2.70) |
| EX | 8.38 (1.66) | 7.38 (1.91) | 6.91 (1.67) | 7.19 (2.01) | |
| TT | 8.28 (2.39) | 7.28 (2.20) | 7.30 (2.01) | 7.68 (1.86) | |
| All | 8.43 (1.88) | 7.58 (2.00) | 7.36 (2.03) | 7.27 (2.21) | |
| Commitment | SS | 8.70 (1.44) | 7.80 (1.90) | 8.14 (2.34) | 6.92 (3.07) |
| EX | 8.78 (1.31) | 8.53 (1.14) | 7.91 (1.57) | 7.13 (1.96) | |
| TT | 8.10 (2.62) | 7.28 (2.67) | 6.83 (2.21) | 6.74 (2.54) | |
| All | 8.54 (1.87) | 7.89 (2.03) | 7.69 (2.09) | 6.96 (2.49) |
Note. Condition: SS = self-study. EX = expert-led training. TT = train-the-trainer. Ns are as follows: baseline N = 91, post-workshop N = 91, post-supervision N = 84, and 12-week follow-up N = 75.
Figure 1.
Mean interest, confidence, and commitment scores for all clinicians across assessment time points. Note. Interest, confidence, and commitment are rated on a Likert-type scale ranging from 0 (not at all) to 10 (extremely). Error bars represent standard deviation for each variable. The four bars for each domain represent assessment time points: 1 = baseline, 2 = post-workshop, 3 = post-supervision, and 4 = 12-week follow-up. Ns are as follows: baseline N = 91, post-workshop N = 91, post-supervision N = 84, and 12-week follow-up N = 75.
Table 2.
Mixed-effects models on interest, confidence, and commitment in using MI
| N. | Den. | ||||
|---|---|---|---|---|---|
| Source | df | df | F | p | |
| Interest | Intercept | 1 | 90.13 | 1710.55 | .00 |
| Condition | 2 | 90.02 | 1.82 | .17 | |
| Time | 3 | 162.98 | 6.59 | .00 | |
| Condition × Time | 6 | 162.18 | 0.70 | .65 | |
| Confidence | Intercept | 1 | 90.81 | 2684.22 | .00 |
| Condition | 2 | 90.53 | 0.83 | .44 | |
| Time | 3 | 208.59 | 7.83 | .00 | |
| Condition × Time | 6 | 201.26 | 1.16 | .33 | |
| Commitment | Intercept | 1 | 90.68 | 1977.29 | .00 |
| Condition | 2 | 90.50 | 2.00 | .14 | |
| Time | 3 | 155.83 | 11.49 | .00 | |
| Condition × Time | 6 | 154.90 | 1.29 | .26 |
Note. N. = numerator. Den. = denominator.
Condition: Training condition (self-study, expert-led training, train-the-trainer). All models run with AR1 covariance structure for time and random effects for clinician.
Note. N. = numerator. Den. = denominator.
Condition: Training condition (self-study, expert-led training, train-the-trainer). All models run with AR1 covariance structure for time and random effects for clinician.
3.2. Relationship to MI integrity
We conducted mixed-effects models for each of the five ITRS factors (fundamental and advanced MI adherence and competence; MI-inconsistent adherence) to evaluate the effects of time, training condition, and their interaction, using a Bonferroni-corrected α of .01 (.05/5), and then compared each model to the enhanced model incorporating interest, confidence, and commitment as covariates. Tables of analyses are available on request from the senior author. With few exceptions, models incorporating and excluding these covariates were not significantly different from each other, indicating the attitudinal variables were not significant predictors of MI integrity. However, in the case of advanced MI competence, the addition of the three covariates significantly improved model fit (Table 3). Confidence emerged as a significant predictor, with fixed-effect estimates indicating that increased confidence would be associated with slightly increased competence in the use of advanced MI strategies (t(253.84) = 3.94, p = .00, β = 0.10, SE β = 0.02, 95% CI = 0.05, 0.14).
Table 3.
Mixed-effects models on advanced MI strategy competence
| N. | Den. | ||||
|---|---|---|---|---|---|
| Source | df | df | F | p | |
| Basic | Intercept | 1 | 86.57 | 9329.34 | .00 |
| Condition | 3 | 184.37 | 6.81 | .00 | |
| Time | 2 | 85.88 | 8.44 | .00 | |
| Condition × Time | 6 | 186.70 | 1.89 | .09 | |
|
| |||||
| Enhanced | Intercept | 1 | 84.99 | 10011.31 | .00 |
| Condition | 3 | 186.34 | 7.90 | .00 | |
| Time | 2 | 88.59 | 11.56 | .00 | |
| Condition × Time | 6 | 187.89 | 1.91 | .08 | |
| Interest | 1 | 259.40 | 1.48 | .23 | |
| Confidence | 1 | 253.84 | 15.51 | .00 | |
| Commitment | 1 | 299.15 | 4.15 | .04 | |
|
| |||||
| Basic | −2 Log likelihood | 688.23 | |||
| Enhanced | −2 Log likelihood | 671.76 | |||
| χ2 comparison with df = 3 | 16.47 | .00 | |||
Note. Time entered as repeated measures factor with covariance structure (AR1). N. = numerator. Den. = denominator. Condition = self-study, expert-led training, train-the-trainer. Parameters estimated for basic model = 15. Parameters estimated for enhanced model = 18.
3.3. Patterns of individual change in interest, confidence, and commitment
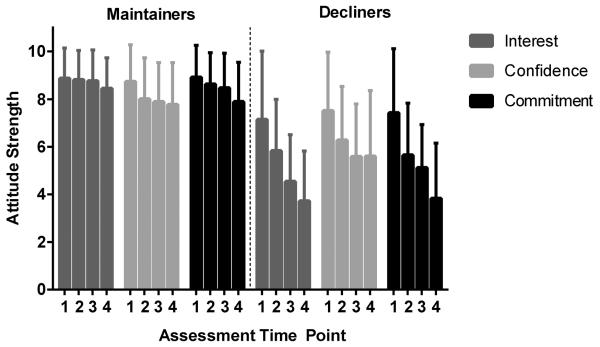
Hierarchical cluster analysis indicated a two-cluster solution. Cluster solutions of three or greater did not result in substantial reductions in agglomeration coefficients or improved cluster interpretability. This two-cluster solution was cross-validated with K-means cluster analysis. The overall agreement across clustering methods was 87% (χ2(1) = 26.34, p < .001). Two basic patterns emerged: (a) 69 (76%) “maintainers” who maintained strong interest in learning MI throughout the study and showed only a small decline in confidence and commitment over time, and (b) 22 (24%) “decliners” who started with lower interest, confidence, and commitment and declined steadily in each domain over time (see Figure 2).
Figure 2.
Mean interest, confidence, and commitment scores for maintainers and decliners across assessment time points. Note. Interest, confidence, and commitment are rated on a Likert-type scale ranging from 0 (not at all) to 10 (extremely). Error bars represent standard deviation for each variable. The four bars for each domain represent assessment time points: 1 = baseline, 2 = post-workshop, 3 = post-supervision, and 4 = 12-week follow-up. Ns are as follows: Maintainers: baseline N = 69, post-workshop N = 69, post-supervision N = 65, and 12-week follow-up N = 58. Decliners: baseline N = 22, post-workshop N = 22, post-supervision N = 19, and 12-week follow-up N = 17.
T-tests and chi-square analyses comparing the two groups showed that the decliners in comparison to maintainers were more likely to self-identify as being in recovery from a substance abuse problem, to have spent more years in recovery, and less likely to endorse allegiance to MI or CBT before receiving training (see Table 4). The two groups did not differ reliably on any other examined demographic, background, or study-related (e.g., study completion) variables.
Table 4.
Descriptive and comparative results for maintainers and decliners.
| Maintainers (n = 69) | Decliners (n = 22) | t | df | p | |
|---|---|---|---|---|---|
|
| |||||
| M (SD) | M (SD) | ||||
| Age | 44.62 (11.04) | 45.95 (11.82) | −0.48 | 89 | .63 |
| Years in clinical work | 9.13 (8.04) | 11.50 (9.09) | −1.17 | 89 | .25 |
| Years in alcohol / drug | 7.67 (6.92) | 9.95 (8.47) | −1.28 | 89 | .21 |
| Years education | 17.28 (2.57) | 17.41 (2.86) | −0.20 | 88 | .84 |
| Years held highest degree* | 8.89 (8.14) | 12.00 (11.02) | −1.22 | 29.14 | .23 |
| Years in recovery | 4.77 (7.49) | 9.20 (9.56) | −2.16 | 83 | .03 |
| Hours previous MI training Allegiance to | 1.07 (3.05) | 0.45 (1.74) | 0.90 | 88 | .37 |
| MI | 2.43 (1.08) | 1.62 (0.87) | 3.12 | 87 | .00 |
| CBT | 4.09 (0.84) | 3.55 (0.96) | 2.55 | 89 | .01 |
| 12step / disease concept* | 3.62 (1.00) | 3.68 (0.78) | −0.29 | 45.04 | .77 |
|
| |||||
| N (%) | N (%) | χ 2 | df | p | |
|
| |||||
| Female | 44 (64) | 15 (68%) | 0.14 | 1 | .80 |
| Ethnicity | 0.37 | 2 | .83 | ||
| Caucasian | 57 (83) | 18 (82) | - | - | - |
| African-American | 7 (10) | 3 (14) | - | - | - |
| Hispanic or other | 5 (7) | 1 (5) | - | - | - |
| In recovery | 20 (31) | 12 (60) | 5.57 | 1 | .03 |
| Masters or Doctoral degree | 42 (61) | 12 (55) | 0.28 | 1 | .63 |
| Community Treatment Program | - | - | 12.68 | 11 | .32 |
| Training condition | - | 0.29 | 2 | .87 | |
| Completed study | 58 (84) | 17 (77) | 0.53 | 1 | .52 |
Note.
equal variances not assumed. Treatment allegiance rated on a 5-point Likert scale (1 = not at all, 5 = very much). Percent within maintainers or percent within decliners is reported.
We conducted mixed-effects models for each of the ITRS factors (fundamental and advanced adherence and competence; MI-inconsistent behavior), with time, training condition, their interaction, and group (maintainer or decliner) as fixed factors, and clinician as a random factor. Given these were exploratory analyses, no Bonferroni correction was used (α = .05). Being a maintainer or decliner was not significantly associated with clinician ability to deliver MI with fundamental or advanced adherence or competence (all p > .05); tables of analyses available on request from the senior author. However, there was a significant group effect for MI-inconsistent adherence (t(85.21) = −2.10, p = .04, β = −0.21, SE β = 0.10, 95% CI −0.42, −0.01; Table 5). While MI-inconsistent adherence decreased over time for both maintainers and decliners, a post hoc univariate comparison indicated that across time points, decliners were likely to demonstrate more frequent MI-inconsistent behavior (estimated M = 1.97, SE = 0.09) than maintainers (estimated M = 1.76, SE = 0.05; F(1, 85.21) = 4.40, p = .04, d = 0.28).
Table 5.
Mixed-effects regression models on MI-inconsistent integrity ratings using maintainer or decliner status.
| N. | Den. | ||||
|---|---|---|---|---|---|
| Source | df | df | F | p | |
| Basic | Intercept | 1 | 84.07 | 1626.20 | .00 |
| Condition | 3 | 191.69 | 13.47 | .00 | |
| Time | 2 | 83.69 | 9.06 | .00 | |
| Condition × Time | 6 | 185.27 | 0.63 | .71 | |
|
| |||||
| Enhanced | Intercept | 1 | 85.95 | 1317.28 | .00 |
| Condition | 3 | 192.75 | 13.27 | .00 | |
| Time | 2 | 82.31 | 9.14 | .00 | |
| Condition × Time | 6 | 185.97 | 0.62 | .72 | |
| Status | 1 | 85.21 | 4.40 | .04 | |
|
| |||||
| Basic | −2 Log likelihood | 647.90 | |||
| Enhanced | −2 Log likelihood | 643.68 | |||
| χ2 comparison with df = 1 | 4.22 | <.05 | |||
Note. Time entered as repeated measures factor with covariance structure (AR1). N. = numerator. Den. = denominator. Condition = self-study, expert-led training, train-the-trainer. Status = maintainer or decliner. Parameters estimated for basic model = 15. Parameters estimated for enhanced model = 16.
4. DISCUSSION
This study examined changes in interest, confidence, and commitment in using MI over time in which clinicians received different types and intensities of MI training. Unexpectedly, clinicians' interest, confidence, and commitment declined over time, regardless of receiving only training materials for self-study or more intensive experiential workshops and follow-up supervision involving integrity rating-based feedback and coaching from either an expert or program-based clinician trainer. This apparently negative shift in attitude toward MI as a result of training bore little relationship to the integrity in which the clinicians used MI with their clients, with the exception that more clinician confidence in their use of MI was associated with greater advanced MI strategy competence. Closer examination of the data showed that 76% of clinicians maintained their interest in learning MI over time with only slight decreases in their confidence and commitment in using the approach. Twenty-four percent, however, began with lower levels of initial interest, confidence, and commitment in using MI, and they subsequently showed sharp declines in each of these areas as they were exposed to more training. In addition, this latter group showed greater use of MI-inconsistent techniques across assessment time points.
Why might have the clinicians' interest in improving their MI skills and confidence and commitment using MI declined over time across all training conditions? The initial high mean ratings on all three dimensions might suggest this declination occurred due to a regression to the mean in a highly motivated, self-selected group of clinicians who volunteered for a training study. Alternatively, clinicians' experiences applying MI after studying it themselves or learning it through workshops may have influenced their attitudes in that they may have realized MI was less compatible with their pre-existing ideas about addictions treatment than they had expected, or that it was harder to learn MI than they initially presumed. Miller and Moyers (2006) posited eight stages for sequentially building critical MI skill sets (e.g., client-centered counseling skills, drawing out client statements that support change, handling resistance). Clinicians attempting to use MI skills before all critical skill sets were fully consolidated may have encountered difficulties that fostered reductions in interest, confidence, and commitment to the intervention.
Despite the overall reductions in interest, confidence, and commitment, clinicians who received workshop training and supervision demonstrated growing MI adherence and competence (Martino et al., 2010). Clinicians who felt more confident delivered the advanced MI strategies (e.g., developing discrepancies, directly eliciting motivation for change, change planning) in a more skillful, fluid manner, consistent with theory that confidence or self-efficacy both influences and is influenced by the quality of performance (Bandura, 1977). However, confidence was unrelated to adherence to fundamental and advanced MI strategies, similar to most prior research findings (Hartzler et al., 2007; Miller and Mount, 2001; Miller et al., 2004). Interest and commitment to MI were likewise unrelated to MI adherence or competence. The main goal of training clinicians in any EBT is to help them increase their demonstrated ability to perform the treatment and ultimately improve their clients' outcomes, as indicated by the associations between therapist use of MI strategies, clients' motivation in session, and clients' subsequent reduction in drinking (Moyers et al., 2009). The finding that clinicians' interest, confidence, and commitment to MI were largely independent from their demonstrated use of MI-consistent and MI-inconsistent strategies suggests these attitudinal variables are distinct from clinicians' abilities to use MI and should be assessed separately.
Nonetheless, pre-existing clinician characteristics, including attitudes about an EBT, may influence the demonstration of EBT after training (Carpenter et al., 2012; Henggeler et al., 2008; Martino et al., 2011). In this study, a substantial minority of clinicians began this training with lower enthusiasm for MI, and their interest, confidence, and commitment declined sharply over time. While these clinicians did not differ from the majority group of “maintainers” in their ability to integrate MI-consistent techniques into their practice, they demonstrated more MI-inconsistent techniques over time, similar to results obtained by Miller and Mount (2001) when training probation officers to use MI. The training efforts used in this study might have increased these clinicians' resistance to learn MI, much as clinicians who prematurely push clients with insufficient readiness for change could provoke them to argue or act against it (Moyers and Martin, 2006). In addition, these clinicians may have had greater difficulty letting go of techniques that better fit their own beliefs about treatment or recovery (Baer et al., 2009), given that these clinicians were less likely to report an allegiance to MI before training and were more likely to be in recovery. Methods for preparing less enthusiastic clinicians for training in MI or other EBT to get the most out of training have received little attention in the literature. Individual clinicians' readiness to learn an EBT could be assessed prior to training and enhanced as a prelude to it if necessary (Barwick et al., 2012). Moreover, as more data accumulates about clinician variables, including attitudinal ones, and their relationships to training methods and outcomes, it could be used in the future to identify clinicians most likely to benefit from training in particular EBTs (Miller et al., 2006). Matching clinicians to EBT training preferences has the potential to maximize training outcomes and utilize training resources in the most cost-effective manner (Olmstead et al., 2011).
As noted above, clinicians' interest, confidence, and commitment to using MI were not strongly associated with MI adherence and competence. However, it is possible that their enthusiasm, as evidenced by these attitudinal variables, could affect their decision to use MI even if it has little bearing on the integrity of their implementation (Damschroder and Hagedorn, 2011). For example, Henggeler and colleagues (2008) showed that clinicians with more positive attitudes about behavior therapy were more likely to use contingency management after training. In addition, attitudinal variables might moderate other clinician training outcomes, such as the degree to which they continue to engage in activities to learn and master different EBT, which might then affect further skill enhancement and sustainability. The relationships between clinicians' interest, confidence, and commitment to EBT and their uptake of it in clinical practice or continued learning of treatment approaches over time remain important and under-explored implementation research areas.
Limitations of this study include: 1) clinician self-selection for study participation, which may have resulted in a highly motivated and interested group of clinicians at baseline and limits generalizability of these findings to clinicians who are willing to participate in an EBT training study; 2) the absence of client outcomes assessment such that the effects of clinician training outcomes on client outcomes could not be assessed; 3) use of only one treatment session per assessment time point to evaluate MI adherence and competence; 4) clinicians selecting clients with whom to demonstrate MI, potentially creating a bias in which clinicians could pick cases wherein they are more able to perform their best MI (Miller et al., 2004); 5) absence of a no-training control group that disallows examination of changes in attitudes or MI adherence and competence over time in the absence of any MI training efforts; and 6) potential for the repeated assessment of MI adherence and competence to affect performance over time. Finally, this study did not assess organizational variables (e.g., organizational support for MI implementation, penetration of MI practice across clinicians and agency programs), which additionally could have influenced the clinicians' enthusiasm for learning MI (Damschroder and Hagedorn, 2011).
This study joins others (Miller and Mount, 2001; Miller et al., 2004) in suggesting that clinicians' attitudes, such as their interest, confidence, and commitment to an EBT, show few associations with their ability to deliver the treatment with integrity. However, clinicians' attitudes may influence their ability to reduce EBT-inconsistent practices over time and may affect other important training outcomes such as the simple uptake of an approach or the degree to which clinicians continue to participate in training activities. Future training research should examine these issues, as well as pre-existing clinician-level predictors of EBT training outcomes, so that more fine-grained and effective clinician selection and training processes can be developed to best prepare the clinical workforce to deliver EBT effectively.
Role of Funding Source
Funding for this study was provided by the NIDA (R01 DA16970 awarded to Steve Martino, with additional support provided by R01 DA023230). Writing of this report was supported by the Office of Academic Affiliations, Advanced Fellowship in Mental Illness Research and Treatment, Department of Veterans Affairs, the Veterans Affairs Connecticut Healthcare System, and the Department of Veterans Affairs New England Mental Illness Research, Education, and Clinical Center (MIRECC). The NIDA, the Office of Academic Affiliations, Department of Veterans Affairs, Veterans Affairs Connecticut Healthcare System, and MIRECC had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication. Views expressed in this paper are those of the authors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors Suzanne Decker and Steve Martino designed this study and the statistical analytic approach, using data from a prior randomized controlled trial conducted by Steve Martino. Suzanne Decker conducted the statistical analyses and literature searches and wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Conflict of Interest No conflict declared.
REFERENCES
- Baer JS, Wells EA, Rosengren DB, Hartzler B, Beadnell B, Dunn C. Agency context and tailored training in technology transfer: a pilot evaluation of motivational interviewing training for community counselors. J. Subst. Abuse. Treat. 2009;37:191–202. doi: 10.1016/j.jsat.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ball SA, Bachrach K, DeCarlo J, Farentinos C, Keen M, McSherry T, Polcin D, Snead N, Sockriter R, Wrigley P, Zammarelli MA, Carroll KM. Characteristics, beliefs, and practices of community clinicians trained to provide manual-guided therapy for substance abusers. J. Subst. Abuse Treat. 2002;23:309–318. doi: 10.1016/s0740-5472(02)00281-7. [DOI] [PubMed] [Google Scholar]
- Ball SA, Martino S, Nich C, Frankforter TL, Van Horn D, Crits-Christoph P, Woody GE, Obert JL, Farentinos C, Carroll KM. Site matters: motivational enhancement therapy in community drug abuse clinics. J. Consult. Clin. Psychol. 2007;75:556–567. doi: 10.1037/0022-006X.75.4.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura AE. Self-efficacy: toward a unifying theory of behavioral change. Psychol. Rev. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Barwick MA, Bennett LM, Johnson SN, McGowan J, Moore JE. Training health and mental health professionals in motivational interviewing: a systematic review. Children Youth Serv. Rev. 2012;34:1786–1795. [Google Scholar]
- Carpenter KM, Cheng WY, Smith JL, Brooks AC, Amrhein PC, Wain RM, Nunes EV. “Old dogs” and new skills: how clinician characteristics relate to motivational interviewing skills before, during, and after training. J. Consult. Clin. Psychol. 2012;80:560–573. doi: 10.1037/a0028362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Ball SA, Nich C, Martino S, Frankforter TL, Farentinos C, Kunkel L, Mikulich-Gilbertson S, Morgenstern J, Obert JL, Polcin D, Snead N, Woody GE. Motivational interviewing to improve treatment engagement and outcome in individuals seeking treatment for substance abuse: a multisite effectiveness study. Drug Alcohol Depend. 2006;81:301–312. doi: 10.1016/j.drugalcdep.2005.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Martino S, Ball SA, Nich C, Frankforter T, Anez LM, Paris M, Suarez-Morales L, Szapocznik J, Miller WR, Rosa C, Matthews J, Farentinos C. A multisite randomized effectiveness trial of motivational enhancement therapy for Spanish-speaking substance users. J. Consult. Clin. Psychol. 2009;77:993–999. doi: 10.1037/a0016489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Rounsaville B. Utility of therapist session checklists to monitor delivery of coping skills treatment for cocaine abusers. Psychotherapy Res. 1998;8:307–320. [Google Scholar]
- Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol. Assess. 1994;6:284–290. [Google Scholar]
- Damschroder LJ, Hagedorn HJ. A guiding framework and approach for implementation research in substance use disorders treatment. Psychol. Addict. Behav. 2011;25:194–205. doi: 10.1037/a0022284. [DOI] [PubMed] [Google Scholar]
- Dimeff LA, Koerner K, Woodcock EA, Beadnell B, Brown MZ, Skutch JM, Paves AP, Bazinet A, Harned MS. Which training method works best? A randomized trial comparing three methods of training clinicians in dialectical behavior therapy skills. Behav. Res. Ther. 2009;47:921–930. doi: 10.1016/j.brat.2009.07.011. [DOI] [PubMed] [Google Scholar]
- Fixsen DL, Naoom SF, Blasé KA, Friedman RM, Wallace F. Implementation Research: A Synthesis of the Literature. University of South Florida, Louis de la Parte Florida Mental Health Institute, The National Implementation Research Network (FMHI Publication #231); Tampa, FL: 2005. [Google Scholar]
- Hartzler B, Baer JS, Dunn C, Rosengren DB, Wells E. What is seen through the looking glass: the impact of training on practitioner self-rating of motivational interviewing skills. Behav. Cogn. Psychother. 2007;35:431–445. [Google Scholar]
- Henggeler SW, Chapman JE, Rowland MD, Halliday-Boykins CA, Randall J, Shackelford J, Schoenwald SK. Statewide adoption and initial implementation of contingency management for substance-abusing adolescents. J. Consult. Clin. Psychol. 2008;76:556–567. doi: 10.1037/0022-006X.76.4.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson JM, Osteen P, Jones A, Berman A. Evaluation of the recognizing and responding to suicide risk training. Suicide Life Threat. Behav. 2012;42:471–485. doi: 10.1111/j.1943-278X.2012.00105.x. [DOI] [PubMed] [Google Scholar]
- Madson MB, Loignon AC, Lane C. Training in motivational interviewing: a systematic review. J. Subst. Abuse Treat. 2009;36:101–109. doi: 10.1016/j.jsat.2008.05.005. [DOI] [PubMed] [Google Scholar]
- Martino S, Ball SA, Nich C, Canning-Ball M, Rounsaville BJ, Carroll KM. Teaching community program clinicians motivational interviewing using expert and train-the-trainer strategies. Addiction. 2010;106:428–441. doi: 10.1111/j.1360-0443.2010.03135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martino S, Ball SA, Nich C, Frankforter TL, Carroll KM. Community program therapist adherence and competence in motivational enhancement therapy. Drug Alcohol Depend. 2008;96:37–48. doi: 10.1016/j.drugalcdep.2008.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martino S, Ball SA, Nich C, Frankforter TL, Carroll KM. Correspondence of motivational enhancement treatment integrity ratings among therapists, supervisors, and observers. Psychother. Res. 2009;19:181–193. doi: 10.1080/10503300802688460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martino S, Canning-Ball M, Carroll K, Rounsaville BJ. A criterion-based stepwise approach for training counselors in motivational interviewing. J. Subst. Abuse Treat. 2011;40:357–365. doi: 10.1016/j.jsat.2010.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martino S, Gallon S, Ball SA, Carroll KM. A step forward in teaching addiction counselors how to supervise motivational interviewing using a clinical trials approach. J. Teach. Addict. 2007;6:37–65. [Google Scholar]
- McGovern MP, Fox TS, Xie H, Drake RE. A survey of clinical practices and readiness to adopt evidence-based practices: dissemination research in an addiction treatment system. J. Subst. Abuse Treat. 2004;26:305–312. doi: 10.1016/j.jsat.2004.03.003. [DOI] [PubMed] [Google Scholar]
- Miller WR, Mount KA. A small study of training in motivational interviewing: does one workshop change clinician and client behavior? Behav. Cogn. Psychother. 2001;29:457–471. [Google Scholar]
- Miller WR, Moyers TB. Eight stages in learning motivational interviewing. J. Teach. Addict. 2006;5:3–17. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. Guilford Press; New York: 2012. [Google Scholar]
- Miller WR, Sorensen JL, Selzer JA, Brigham GS. Disseminating evidence-based practices in substance abuse treatment: a review with suggestions. J. Subst. Abuse Treat. 2006;31:25–39. doi: 10.1016/j.jsat.2006.03.005. [DOI] [PubMed] [Google Scholar]
- Miller W, Yahne C, Moyers T, Martinez J, Pirritano M. A randomized trial of methods to help clinicians learn motivational interviewing. J. Consult. Clin. Psychol. 2004;72:1050–1062. doi: 10.1037/0022-006X.72.6.1050. [DOI] [PubMed] [Google Scholar]
- Morey LC, Blashfield RK, Skinner HA. A comparison of cluster analysis techniques within a sequential validation framework. Multiv. Behav. Res. 1983;18:309–329. doi: 10.1207/s15327906mbr1803_4. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T. Therapist influence on client language during motivational interviewing sessions. J. Subst. Abuse Treat. 2006;30:245–251. doi: 10.1016/j.jsat.2005.12.003. [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Houck JM, Christopher PJ, Tonigan JS. From in-session behaviors to drinking outcomes: a causal chain for motivational interviewing. J. Consult. Clin. Psychol. 2009;77:1113–1124. doi: 10.1037/a0017189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olmstead T, Canning-Ball M, Carroll KM, Martino S. Cost and cost-effectiveness of three strategies for training clinicians in motivational interviewing. Drug Alcohol Depend. 2011;116:195–202. doi: 10.1016/j.drugalcdep.2010.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakovshik SG, McManus F. Establishing evidence-based training in cognitive behavioral therapy: a review of current empirical findings and theoretical guidance. Clin. Psycho. Rev. 2010;30:496–516. doi: 10.1016/j.cpr.2010.03.004. [DOI] [PubMed] [Google Scholar]
- Rogers EM. Diffusion of Innovations. Free Press; New York: 2003. [Google Scholar]
- Shafer MS, Rhode R, Chong J. Using distance education to promote the transfer of motivational interviewing skills among behavioral health professionals. J. Subst. Abuse Treat. 2004;26:141–148. doi: 10.1016/S0740-5472(03)00167-3. [DOI] [PubMed] [Google Scholar]
- Sholomskas DE, Syracuse-Siewart G, Rounsaville BJ, Ball SA, Nuro KF, Carroll KM. We don't train in vain: a dissemination trial of three strategies of training clinicians in cognitive-behavioral therapy. J. Consult. Clin. Psychol. 2005;73:106–115. doi: 10.1037/0022-006X.73.1.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol. Bull. 1979;2:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Simpson DD. Organizational readiness for stage-based dynamics of innovation implementation. Res Social Work Practice. 2009;19:541–51. [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5th ed Pearson; Upper Saddle River, NJ: 2007. [Google Scholar]
- Waltz J, Addis ME, Koerner K, Jacobson N, S. Testing the integrity of a psychotherapy protocol: assessment of adherence and competence. J. Consult. Clin. Psychol. 1993;61:620–30. doi: 10.1037//0022-006x.61.4.620. [DOI] [PubMed] [Google Scholar]