Abstract
Infertility is a couple based fecundity impairment, though population level research is largely based upon information reported by female partners. Of the few studies focusing on male partners, most focus on the utilization of infertility services rather than efforts to estimate the prevalence and determinants of infertility as reported by male partners. Data from a nationally-representative sample of men aged 15–44 years who participated in the 2002 National Survey of Family Growth (NSFG) were used to estimate the prevalence of infertility and determinants of longer time-to-pregnancy (TTP) using the novel current duration approach. Using backward recurrence time parametric survival methods, we estimated infertility prevalence (TTP > 12 months) and time ratios (TR) associated with TTP as derived from males’ reported current duration of their pregnancy attempt. The estimated prevalence of infertility was 12.0% (95% CI: 7.0, 23.2). Longer TTP was associated with older male age (35–45 vs. 17–24 years) (TR: 2.49; 95% CI: 1.03, 6.03), biological childlessness (TR: 1.53; 95% CI: 1.07, 2.19), and lack of health insurance (TR: 1.73; 95% CI: 1.02, 2.94) after controlling for the differences in couples’ age and other socioeconomic factors. The prevalence of infertility based on male reporting is consistent with estimates of infertility in the United States found in prospective cohort studies and current duration studies based on female reporting. Our findings suggest that males can reliably inform about couple infertility. Interventions and services aimed at reducing couple infertility should include attention to male factors associated with longer TTP identified in this study.
INTRODUCTION
Infertility is defined as the inability of couples to conceive a clinical pregnancy after 12 months or more of unprotected intercourse (Practice Committee of the American Society for Reproductive Medicine, 2013). Beyond just pregnancy or its absence, infertility has significant public health consequences, including psychological distress (Bak et al., 2012), social stigmatization (Slade et al., 2007), economic constraints (Wu et al., 2013), and later onset adult diseases in both men and women (Jensen et al., 2009; Merritt et al., 2013). Male factors are estimated to account for approximately 20% of couple infertility with another 30–40% presenting with reproductive abnormalities in both partners (Thonneau et al., 1991; Anderson et al., 2009). In particular, men with a history of infertility or poor semen quality are more likely to be at increased risk of testicular cancer (Baker et al., 2005; Rives et al., 2012; Jorgensen et al., 2011) and a shorter life expectancy (Jensen et al., 2009). In addition, generational effects are reported to be associated with poorer semen quality. For example, boys born with hypospadias were reported to have fathers with poorer semen quality relative to unaffected boys (Asklund et al., 2007). Despite the contribution and consequences of infertility for men, our population-based understanding of infertility is often limited to a female perspective.
A more complete understanding of infertility in the population is achieved when information from both male and female partners is considered. Much of the available data on infertility in the United States is derived from the National Survey of Family Growth (NSFG), which was conducted periodically before implementing a continuous sampling design in 2006 (Groves et al., 2009). Current estimates of infertility in the United States are not derived from direct querying of NSFG survey participants; rather, they rely upon a constructed measure derived from females’ responses to a series of questions on sexual activity, contraceptive use, and pregnancy status in the past 12 months (Chandra et al., 2005). Recently, Thoma and colleagues applied the current duration approach (Keiding et al., 2002; Slama et al., 2012; Slama et al., 2006; Keiding et al., 2012) to derive a time-to-pregnancy (TTP) distribution for estimating the prevalence of infertility in a nationally-representative cross-sectional sample of females in the U.S. (Thoma et al., 2013). Using this approach, the prevalence of infertility was found to be considerably higher than that derived from the constructed approach (16% and 7%, respectively), but consistent with other U.S. prospective cohort studies with preconception enrollment (range: 12–27%) considered the gold standard for measuring TTP (Buck Louis et al., 2009; Buck Louis et al., 2011; Tietze, 1968; Zinaman et al., 1996).
In 2002, the NSFG began interviewing men in recognition of the need to obtain reliable data from males on fertility, fatherhood and childrearing, and sexual behaviors (Martinez et al., 2006). To date, much of the infertility research utilizing the data on males has focused on medical care seeking behaviors for infertility services. For example, Anderson and colleagues (Anderson et al., 2009) estimated that approximately 7.5% of sexually active men aged 15–44 years have ever sought medical care (with their partner) for help in becoming pregnant, of which 2.2% reported seeking care in the past year. Use of infertility services as reported by men was higher among college-educated, older, and married men than referent groups (Anderson et al., 2009; Hotaling et al., 2012). However, these findings characterize the experiences of men who have access to or seek infertility services and, thereby, characterize only a subsample of infertile men in the United States.
Evidence suggests that males may more accurately report their characteristics, attitudes, and behaviors than female proxies (Martinez et al., 2006). The secular pattern of an increasing percentage of births fathered by cohabitating males (i.e., 18.2% in 2002 to 25.4% in 2006–2010) further underscores the need for estimating infertility inclusive of the male partner (Martinez et al., 2012). Moreover, the reliability of TTP as reported by male in comparison to female partners is reported to have moderate (r = 0.62) to high (r = 0.84) reliability (Nguyen & Baird, 2005; Coughlin et al., 1998). In response to these data gaps and in keeping with the couple dependent nature of human reproduction, the objectives of this study were to estimate the prevalence of infertility and determinants of longer TTP using the current duration approach in a nationally representative sample of males aged 15–44 years from the 2002 NSFG.
MATERIALS AND METHODS
Design and study population
The study population comprised 4,928 male respondents aged 15–44 years who participated in the 2002 cycle of the National Survey of Family Growth (NSFG) (www.cdc.gov/nchs/nsfg.htm). The NSFG sample is derived from a stratified multi-stage area probability sampling of 121 geographic areas in the United States to ensure national representativeness of males with oversampling on teenagers (ages 15–19 years), and black and Hispanic men (Groves et al., 2005). The response rate for males in the NSFG was 78%. Research Ethics Review Boards at the Centers for Disease Control and Prevention, National Centers for Health Statistics, and the University of Michigan reviewed and approved the NSFG.
Data collection and operational definitions
Trained interviewers conducted in-person interviews in participants’ households using Computer-Assisted Interviewing (CAI) techniques. Information was collected on sociodemographic characteristics, health history, sexual behaviors and attitudes, fatherhood, birth expectations, and characteristics of current and former wives or cohabiting partners. Potentially sensitive information (e.g., income, sexually transmitted infections) was obtained through Audio Computer Assisted Self-Interviewing (ACASI) techniques. Interviews for males averaged 60 minutes in length with approximately 20 minutes for the ACASI portion.
For study purposes, we defined infertility as requiring greater than 12 months for pregnancy as estimated from a current duration approach (Slama et al., 2012). Specifically, this approach required use of two survey questions that were asked separately for male respondents who were married or cohabiting (n1), or who were in a current sexually active relationship with at least one partner in the past year (n2) (n = n1 + n2 = 2,840; 57.6%) as illustrated in Figure 1. Respondents who were sexually active in the past 12 months with a female partner who was not known to be physically unable to have a child (n = 2,315; 47.0%) were asked about their partner’s current pregnancy status. Men were considered to be in a relationship that was “at risk of pregnancy” if they were sexually active in the past year, reported that their partner was physically able to have a child (to their knowledge) but not currently pregnant (n = 2,179; 44.2%). Men who were considered to be in a relationship “at risk of pregnancy” were then asked “Are you and your (wife/partner) currently trying to get pregnant?” of which 157 (3.2%) men responded “Yes” and, thereby, were eligible for the current duration analysis. Eligible men were then asked, “How long have you and she been trying to get pregnant (in months)?” Responses to these questions were used to determine their duration of current pregnancy attempt. All men who reported they were currently trying for pregnancy provided information on their current duration of attempt (i.e., no missing responses among eligible respondents).
FIGURE 1.
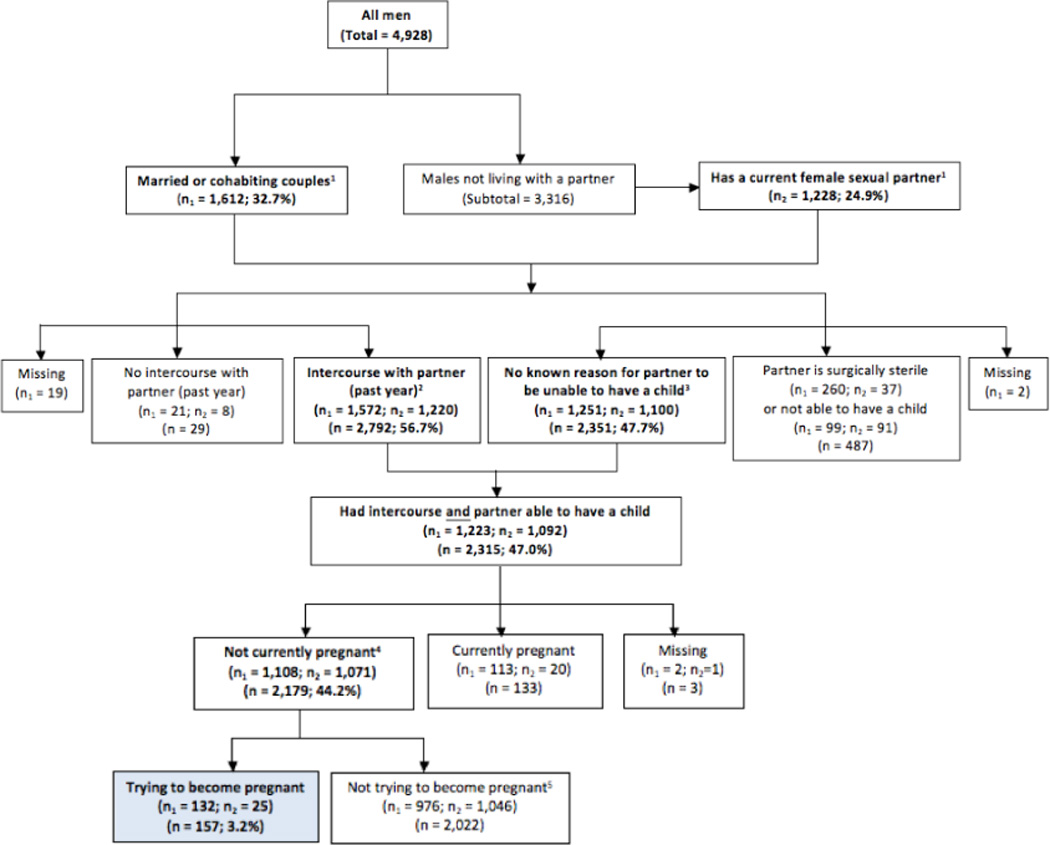
Flow chart of men surveyed in the National Survey of Family Growth based on their eligibility for the current duration analysis.
Footnotes
1 n1 pertains to men who reported they were married or living with a partner of the opposite sex; n2 pertains to men with a recent (past 12 months) sexual partner who were not married or cohabiting, or who’s last partner was not the respondents wife who had died; n pertains to the total number of men with a current partner from each respective category (n = n1+n2).
2 Includes n1 = 13 and n2 = 2 responding “Don’t Know” to the respective category.
3 Includes n2 = 18 responding “Don’t Know” to the respective category; n2 = 3 men reporting vasectomy as method of contraception at last sex.
4 Includes n1 = 8 and n2 = 3 responding “Don’t Know” or “Refuse” to the respective category.
5 Includes n1 = 3 and n2 = 1 responding “Don’t Know” or “Refuse” to the respective category.
All other covariates were defined based upon the survey questions (www.cdc.gov/nchs/nsfg/nsfg_cycle6.htm). Sociodemographic characteristics included categorical terms for male age, relationship status, self-identified race and ethnicity, years of education completed, household family income, and health insurance coverage. Family income was computed relative to the 2001 poverty levels and then categorized into percent of poverty level. Health insurance was categorized as none or any (public or private) based on any mention of private insurance or Medicaid, public, government, state, or military health care. The partner’s age was obtained by direct report or by subtracting the date of interview from the partner’s birthdate. Respondents who reported they or their partners were currently receiving “medical help to become pregnant” or who had a recent medical visit within the reported duration of current pregnancy attempt, and reported ever using infertility treatment (i.e., not advice or testing) were regarded as current users of infertility treatment. Ever having fathered a biological child (yes/no) was determined from the number of biological children computed across responses for all current and past relationships.
Statistical analyses
Descriptive characteristics for the three groups of men as defined by their eligibility for inclusion in the current duration sample were assessed using a design-based F-test to account for the survey design (Table 1). Specifically, the groups were: Group 1) men in a relationship that is at risk of pregnancy and who were trying to become pregnant (i.e., eligible for the current duration analysis) (n = 157); Group 2) men in a relationship that is at risk of pregnancy but who were not trying to become pregnant (n = 2,022); and Group 3) men not in a relationship or who were in a relationship that was not at risk of pregnancy (n = 2,749).
Table 1.
Descriptive characteristics of males by inclusion in the current duration sample
| Current duration eligibility | |||||||
|---|---|---|---|---|---|---|---|
| Yes (group 1)a | No (group 2)b | No (group 3)c | |||||
| Characteristics | n | Weighted % |
n | Weighted % |
n | Weighted % |
p-value |
| Totald | 157 | 4.26 | 2,022 | 45.8 | 2,749 | 49.94 | - |
| Sociodemographic | |||||||
| Age at interview | |||||||
| 15–24 years | 25 | 11.6 | 727 | 26.8 | 1,307 | 40.2 | <0.001 |
| 25–34 | 85 | 55.0 | 717 | 38.0 | 630 | 23.9 | |
| 35–45 | 47 | 33.4 | 578 | 35.2 | 812 | 35.9 | |
| Relationship status | |||||||
| Married | 110 | 83.3 | 723 | 54.5 | 401 | 27.4 | <0.001 |
| Cohabiting | 22 | 9.1 | 253 | 13.6 | 103 | 5.3 | |
| Not cohabiting | 25 | 7.6 | 1,046 | 31.9 | 2,245 | 67.3 | |
| Race and Hispanic origin | |||||||
| Non-Hispanic white | 63 | 56.0 | 1,024 | 67.1 | 1,514 | 64.6 | <0.004 |
| Non-Hispanic black | 37 | 13.3 | 400 | 11.0 | 493 | 12.6 | |
| Non-Hispanic other | 7 | 6.7 | 97 | 4.2 | 170 | 7.7 | |
| Hispanic | 50 | 24.0 | 501 | 17.7 | 572 | 15.1 | |
| Education | |||||||
| 0–11 years completed | 43 | 18.3 | 494 | 19.8 | 1,044 | 35.9 | <0.001 |
| 12 | 30 | 19.0 | 549 | 26.7 | 714 | 27.6 | |
| 13–15 | 47 | 30.1 | 555 | 27.5 | 580 | 21.3 | |
| 16+ | 37 | 32.6 | 424 | 26.1 | 411 | 15.2 | |
| Family incomee | |||||||
| ≥ 300% poverty level | 78 | 53.9 | 1,020 | 52.4 | 1,211 | 43.9 | <0.001 |
| 150–299% | 46 | 30.5 | 565 | 27.9 | 791 | 29.7 | |
| < 150% | 33 | 15.6 | 437 | 19.7 | 747 | 26.4 | |
| Health insurance | |||||||
| Any | 120 | 84.5 | 1,576 | 80.2 | 2,151 | 79.5 | <0.48 |
| None | 37 | 15.5 | 446 | 19.8 | 598 | 20.5 | |
| Reproductive History | |||||||
| Fathered biological child | |||||||
| Yes | 81 | 57.8 | 960 | 74.6 | 690 | 32.6 | <0.001 |
| No | 76 | 42.2 | 1,062 | 25.4 | 2,059 | 67.4 | |
| Medical treatment for pregnancy (at interview)f |
|||||||
| Never | 126 | 74.1 | 1,984 | 97.1 | 2,705 | 97.4 | <0.001 |
| Current treatment | 11 | 9.6 | 0 | 0 | 2 | 0.2 | |
| Past treatment | 20 | 16.3 | 38 | 2.9 | 42 | 2.4 | |
Note: All percentages and p-value estimates account for survey design.
Group 1: Men who were eligible for the current duration analysis, given they were at risk of pregnancy (i.e. sexually active with a partner in the past year who was not sterile and not pregnant) and reported they and their partner were attempting pregnancy at the time of interview.
Group 2: Men who were at risk of pregnancy, but who reported they were not attempting pregnancy at the time of interview.
Group 3: Men who were either not in a relationship or in a relationship not at risk of pregnancy.
Weighted row percentages; all other values are column percentages.
Family income relative to the 2001 poverty levels defined by the U.S. Census Bureau.
Based on self-reported current or ever use of medical help for pregnancy and type of services sought.
The current duration approach was used to estimate the prevalence of infertility (TTP > 12 months) and median TTP for all eligible men (n = 157). Briefly, this approach yields an estimate of the total duration of pregnancy attempt (i.e., estimated TTP), which is unobserved but estimated from the observed current duration of pregnancy attempt at the time of interview using parametric survival methods (Keiding et al., 2002; Keiding et al., 2012). Under this framework, men with longer durations of pregnancy attempt are more likely to be over-represented in the sample (i.e., length-biased sample). However, this sampling bias is accounted for in the current duration methods to provide unbiased results under the assumptions of stationarity (i.e., the start of pregnancy attempts are uniform over time) and independence of observations. To estimate a TTP distribution, we assumed a generalized gamma distribution, which is well-suited to distributions with a long right tail (e.g., income or TTP). In fitting the model, we censored observations at 30 months and interpreted observations representing less than 1 month of trying as 0.25. Ninety-five percent confidence intervals were calculated from bootstrapped samples with 1000 iterations (Efron & Tibshirani, 1993). A weighted maximum likelihood analysis was conducted to account for the oversampling of teenagers and black/Hispanic men in the survey to ensure generalizability of our results to the U.S. population. Analyses to estimate TTP distributions and infertility prevalence were implemented in R (R Development Core Team, 2012).
Unadjusted and adjusted associations between sociodemographic characteristics and the total (unobserved) duration of pregnancy attempt were estimated using backward recurrence time survival methods (Yamaguchi, 2003). Specifically, we used weighted accelerated-failure-time (AFT) regression models censored at a TTP of 30 months and accounted for potential clustering due to the sample design (Keiding et al., 2011). These methods allow for the estimation of time ratio (TR) associations between sociodemographic characteristics and the (unobserved) TTP. TRs can be interpreted as the ratio of median values of the total duration of pregnancy attempt across characteristics, such that a ratio greater than 1 indicates a longer median TTP while a TR less than 1 denotes a shorter median TTP. AFT models were adjusted for age (categorical), difference between partners’ ages (years, continuous) given the correlation between couples’ ages (r=0.64), relationship status (categorical), racial and ethnic self-identification (categorical), education (categorical), poverty level (categorical), health insurance (any versus none), and history of having fathered a biological child (yes versus no). Prior to running AFT models, eight missing observations for partner age only were imputed using multiple imputation techniques (Schafer, 1999). All regression analyses accounted for the survey weights and were performed using Stata, version 11 (StataCorp, College Station, TX).
The robustness of these estimates was assessed in sensitivity analyses. We varied inclusion criteria in restricted analyses to assess men who had not initiated infertility treatment during the current duration attempt, in recognition that treatment may modify the probability of pregnancy (Keiding et al., 2012), and men who had not fathered a biological child, which may modify the persistency of trying for pregnancy (Basso et al., 2000). Finally, we assessed the combined effects of partners’ ages (≥ 35 years versus < 35 years) on TTP, given evidence that both may exert an effect on the probability of pregnancy during the fertile window and TTP (Dunson et al., 2002; Dunson et al., 2004). Additional parametric assumptions were employed to assess the performance of our methods for estimating TTP using a Pareto distribution in place of a generalized gamma and using data grouped across suitable intervals (see Supplementary Information) to account for the common issue of digit preference observed in this study and other retrospective TTP data (Joffe et al., 1993).
RESULTS
Descriptive characteristics of men by the three groups (Group 1- at risk of and trying for pregnancy, Group 2 - at risk of and not trying for pregnancy, and Group 3 - not at risk of pregnancy) revealed important differences. Overall, statistically significant differences were found across groups for all sociodemographic characteristics with the exception of health insurance status. The current duration group (Group 1) had a higher percentage of men who were between the ages of 25 to 34 years (55.0%), married (83.3%), Hispanic ethnicity (24.0%), educational attainments ≥ 16 years (32.6%), had not previously fathered a biological child (42.2%), and had ever used fertility treatment (25.9%) compared to either Group 2 or Group 3.
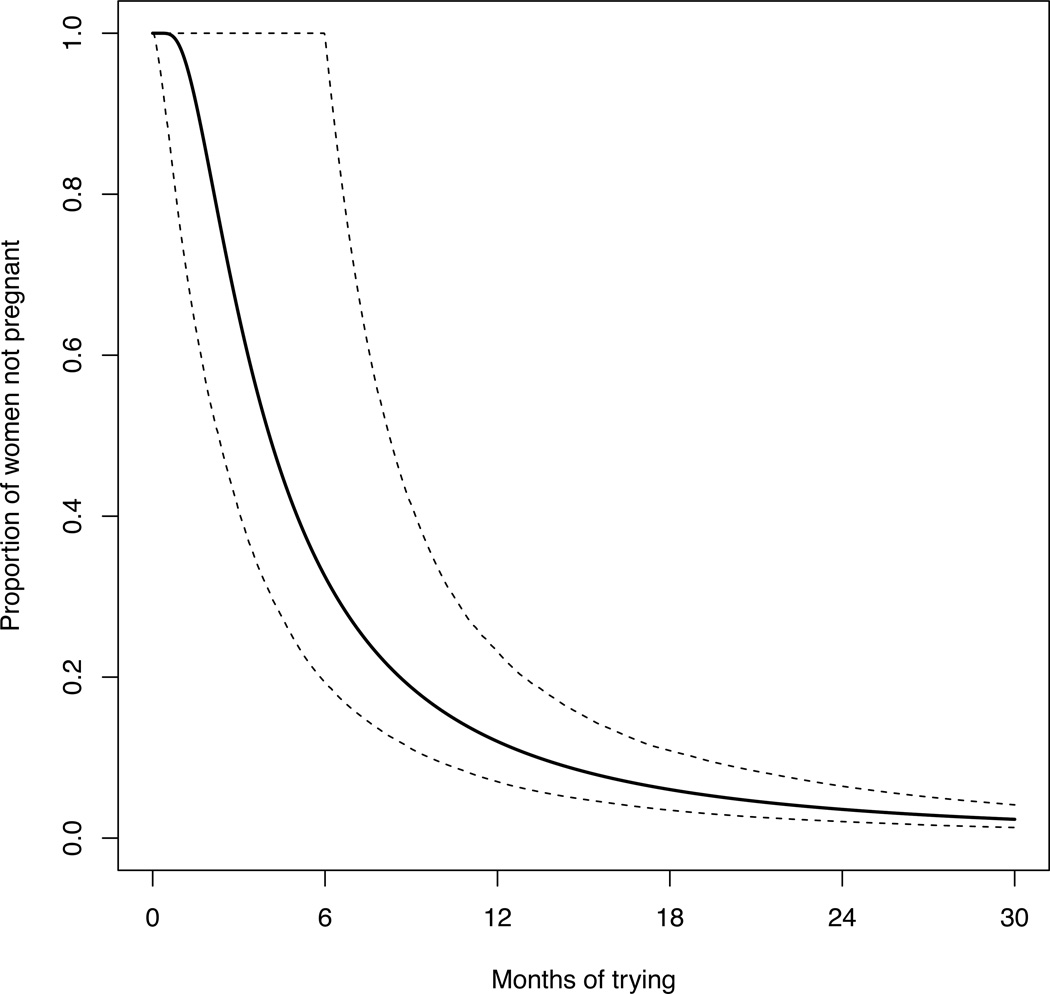
Figure 2 shows the estimated survival function of the total duration of sexually active couples not yet pregnant by their months of trying, as determined from male respondents. Among all men in the current duration sample, the prevalence of infertility was 12.0% (95% CI: 7.0, 23.2) and the median estimated TTP was 4.3 months (95% CI: 2.3, 8.2). The estimated probability of pregnancy at 3, 6, 12, and 24 months is 0.65, 0.33, 0.12, 0.04, respectively.
FIGURE 2.
Estimation of the proportion of couples not yet pregnant as a function of the number of months trying for pregnancy as reported by males (n = 157) in the National Survey of Family Growth. The solid curve is the weighted survival function censored at 30 months for the time until pregnancy or end of attempt and the dashed curves indicate 95% confidence intervals (CI).
In subgroup analyses, the prevalence of infertility increased to 14.0% (95% CI: 6.0, 25.6) with a median estimated TTP of 5.6 months (95% CI: 3.0, 8.4) for male participants who had not fathered a biological child. Among men reporting not having sought infertility treatment, infertility prevalence was 9.4% (95% CI: 5.2, 17.2) with a median TTP of 4.1 months (95% CI: 2.3, 7.9). Minimal change was seen when using a Pareto distribution, in place of the generalized gamma distribution, with a prevalence of 10.6% (95% CI: 3.9, 22.6) or when performing grouped analyses to account for digit preference (see Supporting Information).
A statistically significant longer estimated TTP was found for older age groups (TR25–34: 1.52; 95% CI: 1.00, 2.32; TR35–45: 2.49; 95% CI: 1.03, 6.03) compared to age group 17–24 years, not having a form of health insurance (TR: 1.73; 95% CI: 1.02, 2.94) compared to any insurance, and not having fathered a biological child (TR: 1.53; 95% CI: 1.07, 2.19) compared to having fathered a biological child. When looking at the combined ages of males and female partners, significant associations were only found for the group of males 35+ years and females < 35 years (TR: 2.78; 95% CI: 1.52, 5.09; n = 13), but not for males < 35 years and females 35+ years (TR: 0.85; 95% CI: 0.44, 1.65; n = 10) or males and females both aged 35+ years (TR: 1.43; 95% CI: 0.54, 3.81; n = 30) when compared to the reference group of males and females < 35 years of age (nref = 96; 64% of current duration sample).
DISCUSSION
In this nationally representative cross-sectional sample of men aged 15–44 years, the prevalence of current infertility based on a current duration approach was approximately 12% (95% CI: 7, 23); however, prevalence estimates ranged from 9 to 14% based on sensitivity analyses of inclusion criteria and modeling assumptions. Our infertility prevalence estimates based upon male report are consistent with other U.S. estimates based on female reporting applying a current duration approach (15.5%; 95% CI: 8.6, 27.5%) (Thoma et al., 2013), and the range reported from prospective cohort studies with preconception enrollment of couples observed over 12 months of trying (range: 12–27%) (Buck Louis et al., 2009; Buck Louis et al., 2011; Tietze, 1968; Zinaman et al., 1996). Older age and biological childlessness were associated with longer TTP in this study of male determinants as well as in previous studies of female determinants (Thoma et al., 2013). These findings underscore reliable reporting by male respondents and the importance of assessing partner characteristics when assessing couple fecundity.
Our infertility prevalence estimate is notably higher than the reported 2.2% of men who sought medical help to become pregnant with their partner in the past year from the 2002 NSFG (Anderson et al., 2009). The latter figure may reflect a more selective population due to care-seeking behaviors and access to care for infertility services, whereas our infertility prevalence estimate suggests the potential demand for medical services for infertility may be considerably higher. Prior studies on men reporting care seeking (with their partners) for help to become pregnant were more likely to be older, married, and have a college degree or higher than their corresponding reference groups (Anderson et al., 2009; Hotaling et al., 2012). Unlike age, which was a risk factor for both outcomes (infertility or infertility service use), we found no association between education and marital status with longer TTP in our study. Such discrepancies suggest that these factors may have more to do with care seeking behaviors rather than infertility, per se. The literature also reflects contrasting sociodemographic patterns for females in relation to infertility and use of medical services for infertility. For example, family income, health insurance status, and having a college or higher degree were associated with infertility service use in females (Chandra & Stephen, 2010); however, they were not associated with a longer estimated TTP (Thoma et al., 2013). These socioeconomic discrepancies in infertility service utilization are also observed in France (Moreau et al., 2010), where national access to infertility coverage is provided, and among states in the U.S. providing infertility insurance mandates (Bitler & Schmidt, 2006).
Compared to traditional population-based methods estimating infertility (yes/no), the current duration method provides a more sensitive indicator of fecundity and its risk factors by assessing the total TTP distribution. This study supports an association between older male age and a longer TTP, which may be due to age related hormonal changes in semen quality that may arise either directly or indirectly via changes in general health status (Stewart & Kim, 2011; Sartorisius et al., 2012). Of note is the equivocal literature regarding the relation between advanced paternal age and fecundity, with some studies showing an association with reductions in fecundity (Ford et al., 2000; Dunson et al., 2004; Dunson et al., 2002) while others do not (Mutsaerts et al., 2012; Olsen, 1990; Jensen et al., 2000). A further advantage of the current duration approach over pregnancy-based retrospective TTP studies (Ford et al., 2000; Olsen, 1990) is our ability to assess childless men and women, which we found to be associated with longer TTP. Notably, in comparison to men with health insurance, those without it had a longer TTP, which may be attributable to delays in access to care for conditions affecting fecundity. This finding may mark an unmet need for reproductive and preconception health services for uninsured men. However, other studies are needed to corroborate these trends.
Our estimated infertility prevalence in males (12%) may be underestimated in relation to the estimated 16% for female reporting in the 2002 NSFG, a study that also utilized the current duration approach (Thoma et al., 2013). However, our finding is consistent with an earlier study that reported shorter TTPs for male than female partners (Nguyen & Baird, 2005; Coughlin et al., 1998). Our prevalence estimate is not biased by the exclusion of males whose partners are already pregnant, given that by design the current duration approach relies only upon recurrence times for individuals currently trying to become pregnant. This is a unique feature of the method, and one that makes is well suited for cross-sectional survey research such as the NSFG. Additional potential limitations inherent in our study are the temporality of characteristics associated with infertility, the retrospective reporting of time at risk for pregnancy and our inability to better characterize men by infertility treatment-seeking behavior. This latter limitation reflects the cross-sectional nature of the NSFG survey rather than longitudinal follow up over 12 months.
Conclusion
In sum, we found that approximately 9% to 14% of reproductive-aged U.S. men may be experiencing couple infertility based on a current duration approach. The consistency of these estimates with those reported by women applying this approach or with the gold standard of prospective cohorts suggests that males are able to provide reliable information on couple infertility. In light of the forthcoming U.S. National Public Health Action Plan for Detection, Prevention, and Management of Infertility (www.cdc.gov/reproductivehealth/Infertility/PublicHealth.htm), our findings underscore the importance of including men in research focusing on infertility in keeping with the couple dependent nature of human reproduction.
Supplementary Material
Table 2.
Time ratios (TR) and 95% confidence intervals (CI) for the association between descriptive characteristics of male partners and total duration of pregnancy attempt
| Characteristics | Weighted Mean CDa |
Unadjusted TR (95% CI) |
Adjustedb TR (95% CI) |
|---|---|---|---|
| Total | 12.5 | - | - |
| Age at interview | |||
| 17–24 years | 5.3 | 1.00 | 1.00 |
| 25–34 | 9.2 | 1.42 (1.04, 1.94) | 1.52 (1.00, 2.32) |
| 35–45 | 20.3 | 2.03 (0.94, 4.39) | 2.49 (1.03, 6.03) |
| Relationship status | |||
| Married | 12.7 | 1.00 | 1.00 |
| Cohabiting | 14.6 | 0.98 (0.53, 1.79) | 1.30 (0.78, 2.17) |
| Not cohabiting | 7.6 | 0.92 (0.64, 1.33) | 1.15 (0.68, 1.94) |
| Race and Hispanic origin | |||
| Non-Hispanic white | 11.4 | 1.00 | 1.00 |
| Non-Hispanic black | 8.7 | 0.99 (0.53, 1.79) | 1.02 (0.62, 1.68) |
| Non-Hispanic other | 18.8 | 1.49 (0.83, 2.68) | 1.28 (0.56, 2.96) |
| Hispanic | 15.2 | 0.80 (0.52, 1.23) | 0.88 (0.55, 1.40) |
| Education | |||
| 0–11 years completed | 11.5 | 1.00 | 1.00 |
| 12 | 10.0 | 0.94 (0.62, 1.43) | 0.77 (0.47, 1.26) |
| 13–15 | 14.3 | 1.26 (0.86, 1.85) | 1.08 (0.66, 1.75) |
| 16+ | 12.8 | 1.47 (0.90, 2.40) | 1.24 (0.68, 2.27) |
| Family incomec | |||
| ≥ 300% poverty level | 12.3 | 1.00 | 1.00 |
| 150 -- 299% | 13.7 | 1.04 (0.69, 1.57) | 1.40 (0.91, 2.13) |
| < 150% | 10.5 | 0.75 (0.50, 1.13) | 0.81 (0.49, 1.35) |
| Health insurance | |||
| Any | 10.5 | 1.00 | 1.00 |
| None | 23.1 | 1.11 (0.67, 1.83) | 1.73 (1.02, 2.94) |
| Fathered a biological child | |||
| Yes | 10.0 | 1.00 | 1.00 |
| No | 15.7 | 1.22 (0.89, 1.69) | 1.53 (1.07, 2.19) |
Values are weighted means of reported current duration (CD) of pregnancy attempt in months used to estimate total duration of pregnancy attempt (time-to-pregnancy, TTP).
Adjusted for all male characteristics in the table and age difference between female partner and male respondent age (TR: 0.98; 95% CI: 0.95, 1.00; p-value = 0.08).
Family income relative to the 2001 poverty levels defined by the U.S. Census Bureau.
ACKNOWLEDGEMENTS
The 2002 National Survey of Family Growth (NSFG) was conducted by the Centers for Disease Control and Prevention’s (CDC) National Center for Health Statistics (NCHS) with the support and assistance of a number of other organizations and individuals, with the participation and funding support of the following programs of the U.S. Department of Health and Human Services:
Eunice Kennedy Shriver National Institute for Child Health and Human Development (NICHD), National Institutes of Health (NIH)
Office of Population Affairs
CDC’s National Center for Health Statistics (CDC/NCHS)
CDC’s Division of HIV/AIDS Prevention (CDC/DHAP)
CDC’s Division of Sexually Transmitted Disease Prevention (CDC/DSTDP)
CDC’s Division of Reproductive Health (CDC/DRH)
Office of the Assistant Secretary for Planning and Evaluation (OASPE)
Children’s Bureau of the Administration for Children and Families.
The analysis and writing of this paper was supported by the Intramural Research Program, NICHD, NIH.
Footnotes
Author disclosure statement:
J.F.L has nothing to disclose. D.N.S. has nothing to disclose. M.E.T has nothing to disclose. A.C.M has nothing to disclose. R.B.K. has nothing to disclose. A.C.T. has nothing to disclose. R.S. has nothing to disclose. N.K. has nothing to disclose. G.M.L has nothing to disclose.
Author contribution statement:
JFL acquired and compiled the data; JFL, MET, DNS, ACM, NK analyzed the data; JFL, MET, DNS, ACM, RBK, RS, NK, GML wrote the paper. MET, RBK, and GML conceptualized the research question. All authors approved the final manuscript for publication.
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article:
Supplementary Methods
Figure S1. Frequency of reported current duration of pregnancy attempt
Figure S2. Estimation of the density of current duration of pregnancy attempt using grouped and reported data
Figure S3. Estimated survival curves for time-to-pregnancy using grouped and reported data
Table S1. Estimated infertility prevalence based on grouped and reported data
REFERENCES
- Anderson JE, Farr SL, Jamieson DJ, Warner L, Macaluso M. Infertility services reported by men in the United States: national survey data. Fertil. Steril. 2009;91(6):2466–2470. doi: 10.1016/j.fertnstert.2008.03.022. [DOI] [PubMed] [Google Scholar]
- Asklund C, Jorgensen N, Skakkebaek NE, Jensen TK. Increased frequency of reproductive health problems among fathers of boys with hypospadias. Hum. Reprod. 2007;22(10):2639–2646. doi: 10.1093/humrep/dem217. [DOI] [PubMed] [Google Scholar]
- Bak CW, Seok HH, Song SH, Kim ES, Her YS, Yoon TK. Hormonal imbalances and psychological scars left behind in infertile men. J. Androl. 2012;33(2):181–189. doi: 10.2164/jandrol.110.012351. [DOI] [PubMed] [Google Scholar]
- Baker JA, Buck GM, Vena JE, Moysich KB. Fertility patterns prior to testicular cancer diagnosis. Cancer Causes Control. 2005;16(3):295–299. doi: 10.1007/s10552-004-4024-2. [DOI] [PubMed] [Google Scholar]
- Basso O, Juul S, Olsen J. Time to pregnancy as a correlate of fecundity: differential persistence in trying to become pregnant as a source of bias. Int. J Epidemiol. 2000;29(5):856–861. doi: 10.1093/ije/29.5.856. [DOI] [PubMed] [Google Scholar]
- Bitler M, Schmidt L. Health disparities and infertility: impacts of state-level insurance mandates. Fertil. Steril. 2006;85(4):858–865. doi: 10.1016/j.fertnstert.2005.11.038. [DOI] [PubMed] [Google Scholar]
- Buck Louis GM, Dmochowski J, Lynch C, Kostyniak P, McGuinness BM, Vena JE. Polychlorinated biphenyl serum concentrations, lifestyle and time-to-pregnancy. Hum. Reprod. 2009;24(2):451–458. doi: 10.1093/humrep/den373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buck Louis GM, Schisterman EF, Sweeney AM, Wilcosky TC, Gore-Langton RE, et al. Designing prospective cohort studies for assessing reproductive and developmental toxicity during sensitive windows of human reproduction and development--the LIFE Study. Paediatr. Perinat. Epidemiol. 2011;25(5):413–424. doi: 10.1111/j.1365-3016.2011.01205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Fertility, family planning, and reproductive health of U.S. women: data from the 2002 National Survey of Family Growth. Vital Health Stat. 2005;23(25):1–160. [PubMed] [Google Scholar]
- Chandra A, Stephen EH. Infertility service use among U.S. women: 1995 and 2002. Fertil. Steril. 2010;93(3):725–736. doi: 10.1016/j.fertnstert.2008.10.049. [DOI] [PubMed] [Google Scholar]
- Coughlin MT, LaPorte RE, O'Leary LA, Lee PA. How accurate is male recall of reproductive information? Am. J. Epidemiol. 1998;148(8):806–809. doi: 10.1093/oxfordjournals.aje.a009702. [DOI] [PubMed] [Google Scholar]
- Dunson DB, Baird DD, Colombo B. Increased infertility with age in men and women. Obstet. Gynecol. 2004;103(1):51–56. doi: 10.1097/01.AOG.0000100153.24061.45. [DOI] [PubMed] [Google Scholar]
- Dunson DB, Colombo B, Baird DD. Changes with age in the level and duration of fertility in the menstrual cycle. Hum. Reprod. 2002;17(5):1399–1403. doi: 10.1093/humrep/17.5.1399. [DOI] [PubMed] [Google Scholar]
- Efron B, Tibshirani RJ. An introduction to the bootstrap. London: Chapman & Hall; 1993. [Google Scholar]
- Ford WC, North K, Taylor H, Farrow A, Hull MG, Golding J. Increasing paternal age is associated with delayed conception in a large population of fertile couples: evidence for declining fecundity in older men. The ALSPAC Study Team (Avon Longitudinal Study of Pregnancy and Childhood) Hum. Reprod. 2000;15(8):1703–1708. doi: 10.1093/humrep/15.8.1703. [DOI] [PubMed] [Google Scholar]
- Groves RM, Benson G, Mosher WD, Rosenbaum J, Granda P, et al. Plan and operation of Cycle 6 of the National Survey of Family Growth. Vital Health Stat. 2005;1(42):1–86. [PubMed] [Google Scholar]
- Groves RM, Mosher WD, Lepkowski JM, Kirgis NG. Planning and development of the continuous National Survey of Family Growth. Vital Health Stat. 2009;1(48):1–64. [PubMed] [Google Scholar]
- Hotaling JM, Davenport MT, Eisenberg ML, VanDenEeden SK, Walsh TJ. Men who seek infertility care may not represent the general U.S. population: data from the National Survey of Family Growth. Urology. 2012;79(1):123–127. doi: 10.1016/j.urology.2011.09.021. [DOI] [PubMed] [Google Scholar]
- Jensen TK, Jacobsen R, Christensen K, Nielsen NC, Bostofte E. Good semen quality and life expectancy: a cohort study of 43,277 men. Am. J. Epidemiol. 2009;170(5):559–565. doi: 10.1093/aje/kwp168. [DOI] [PubMed] [Google Scholar]
- Jensen TK, Scheike T, Keiding N, Schaumburg I, Grandjean P. Selection bias in determining the age dependence of waiting time to pregnancy. Am. J. Epidemiol. 2000;152(6):565–572. doi: 10.1093/aje/152.6.565. [DOI] [PubMed] [Google Scholar]
- Joffe M, Villard L, Li Z, Plowman R, Vessey M. Long-term recall of time-to-pregnancy. Fertil. Steril. 1993;60(1):99–104. doi: 10.1016/s0015-0282(16)56044-0. [DOI] [PubMed] [Google Scholar]
- Jorgensen N, Vierula M, Jacobsen R, Pukkala E, Perheentupa A, et al. Recent adverse trends in semen quality and testis cancer incidence among Finnish men. Int. J. Androl. 2011;34(4 Pt 2):e37–e48. doi: 10.1111/j.1365-2605.2010.01133.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keiding N, Fine JP, Hansen OH, Slama R. Accelerated failure time regression for backward recrrence times and current durations. Statistics and Probability Letters. 2011;81:724–729. [Google Scholar]
- Keiding N, Hansen OK, Sorensen D, Slama R. The Current Duration Approach to Estimating Time to Pregnancy. Scandinavian Journal of Statistics. 2012;39(2):185–204. [Google Scholar]
- Keiding N, Kvist K, Hartvig H, Tvede M, Juul S. Estimating time to pregnancy from current durations in a cross-sectional sample. Biostatistics. 2002;3(4):565–578. doi: 10.1093/biostatistics/3.4.565. [DOI] [PubMed] [Google Scholar]
- Martinez G, Daniels K, Chandra A. Fertility of Men and Women Aged 15–44 Years in the United States: National Survey of Family Growth, 2006–2010. Hyattsville, MD: Rep. 51, National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- Martinez GM, Chandra A, Abma JC, Jones J, Mosher WD. Fertility, contraception, and fatherhood: data on men and women from cycle 6 (2002) of the 2002 National Survey of Family Growth. Vital Health Stat. 2006;23(26):1–142. [PubMed] [Google Scholar]
- Merritt MA, De Pari M, Vitonis AF, Titus LJ, Cramer DW, Terry KL. Reproductive characteristics in relation to ovarian cancer risk by histologic pathways. Hum Reprod. 2013;28(5):1406–1417. doi: 10.1093/humrep/des466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreau C, Bouyer J, Ducot B, Spira A, Slama R. When do involuntarily infertile couples choose to seek medical help? Fertil. Steril. 2010;93(3):737–744. doi: 10.1016/j.fertnstert.2008.10.011. [DOI] [PubMed] [Google Scholar]
- Mutsaerts MA, Groen H, Huiting HG, Kuchenbecker WK, Sauer PJ, et al. The influence of maternal and paternal factors on time to pregnancy--a Dutch population-based birth-cohort study: the GECKO Drenthe study. Hum. Reprod. 2012;27(2):583–593. doi: 10.1093/humrep/der429. [DOI] [PubMed] [Google Scholar]
- Nguyen RH, Baird DD. Accuracy of men's recall of their partner's time to pregnancy. Epidemiology. 2005;16(5):694–698. doi: 10.1097/01.ede.0000173038.93237.b3. [DOI] [PubMed] [Google Scholar]
- Olsen J. Subfecundity according to the age of the mother and the father. Dan. Med. Bull. 1990;37(3):281–282. [PubMed] [Google Scholar]
- Practice Committee of the American Society for Reproductive Medicine. Definitions of infertility and recurrent pregnancy loss: a committee opinion. Fertil. Steril. 2013;99(1):63. doi: 10.1016/j.fertnstert.2012.09.023. [DOI] [PubMed] [Google Scholar]
- R Development Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2012. [Google Scholar]
- Rives N, Perdrix A, Hennebicq S, Saias-Magnan J, Melin MC, et al. The semen quality of 1158 men with testicular cancer at the time of cryopreservation: results of the French National CECOS Network. J. Androl. 2012 doi: 10.2164/jandrol.112.016592. [DOI] [PubMed] [Google Scholar]
- Sartorius G, Spasevska S, Idan A, Turner L, Forbes E, Zamojska A, Allan CA, Ly LP, Conway AJ, McLachlan RI, Handelsman DJ. Serum testosterone, dihydrotestosterone and estradiol concentrations in older men self-reporting very good health: the healthy man study. Clin Endocrinol. 2012;77(5):755–763. doi: 10.1111/j.1365-2265.2012.04432.x. [DOI] [PubMed] [Google Scholar]
- Schafer JL. Multiple imputation: a primer. Stat. Methods Med. Res. 1999;8(1):3–15. doi: 10.1177/096228029900800102. [DOI] [PubMed] [Google Scholar]
- Slade P, O'Neill C, Simpson AJ, Lashen H. The relationship between perceived stigma, disclosure patterns, support and distress in new attendees at an infertility clinic. Hum. Reprod. 2007;22(8):2309–2317. doi: 10.1093/humrep/dem115. [DOI] [PubMed] [Google Scholar]
- Slama R, Ducot B, Carstensen L, Lorente C, de La RE, et al. Feasibility of the current-duration approach to studying human fecundity. Epidemiology. 2006;17(4):440–449. doi: 10.1097/01.ede.0000221781.15114.88. [DOI] [PubMed] [Google Scholar]
- Slama R, Hansen OK, Ducot B, Bohet A, Sorensen D, et al. Estimation of the frequency of involuntary infertility on a nation-wide basis. Hum. Reprod. 2012;27(5):1489–1498. doi: 10.1093/humrep/des070. [DOI] [PubMed] [Google Scholar]
- Stewart AF, Kim ED. Fertility concerns for the aging male. Urology. 2011;78(3):496–499. doi: 10.1016/j.urology.2011.06.010. [DOI] [PubMed] [Google Scholar]
- Thoma ME, McLain AC, Louis JF, King RB, Trumble AC, et al. Prevalence of infertility in the United States as estimated by the current duration approach and a traditional constructed approach. Fertil. Steril. 2013 doi: 10.1016/j.fertnstert.2012.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thonneau P, Marchand S, Tallec A, Ferial ML, Ducot B, et al. Incidence and main causes of infertility in a resident population (1,850,000) of three French regions (1988–1989) Hum. Reprod. 1991;6(6):811–816. doi: 10.1093/oxfordjournals.humrep.a137433. [DOI] [PubMed] [Google Scholar]
- Tietze C. Fertility after discontinuation of intrauterine and oral contraception. Int. J Fertil. 1968;13(4):385–389. [PubMed] [Google Scholar]
- Wu AK, Elliott P, Katz PP, Smith JF. Time costs of fertility care: the hidden hardship of building a family. Fertil. Steril. 2013 doi: 10.1016/j.fertnstert.2013.01.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamaguchi K. Accelerated Failure-Time Mover-Stayer Regression Models for the Analysis of Last-Episode Data. Sociological Methodology. 2003;33:81–110. [Google Scholar]
- Zinaman MJ, Clegg ED, Brown CC, O'Connor J, Selevan SG. Estimates of human fertility and pregnancy loss. Fertil. Steril. 1996;65(3):503–509. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.