Abstract
Background
Previous work has shown that inhibition of fear is impaired in posttraumatic stress disorder (PTSD) resulting from both civilian and combat trauma. The purpose of the present study was to investigate the inhibition of learned fear in traumatized individuals diagnosed with either acute stress disorder (ASD) or PTSD. This is the first study to use a conditioned inhibition paradigm with traumatized individuals within a month of trauma exposure. We hypothesized that impaired fear inhibition would be evident in PTSD, but not ASD.
Method
Using established translational, psychophysiological methods including fear-potentiated startle, and skin conductance, we examined fear acquisition, stimulus discrimination, and the transfer of learned safety in a Croatian population with ASD or PTSD. This cross-sectional study included three age-matched groups: healthy nontrauma controls (n = 27), a group with chronic PTSD (10 or more years since trauma exposure, n = 24), and a group with ASD (30 days or less since trauma exposure, n = 27).
Results
The presence of trauma-related psychopathology, whether acute or chronic, was associated with an impaired ability to transfer learned safety based on fear-potentiated startle measures, while healthy control subjects showed significant fear inhibition in the presence of the safety cue compared to the danger cue, F(1,26) = 12.64, P = .001.
Conclusions
These data expand our previously observed findings of PTSD-associated fear inhibition deficits by demonstrating that trauma-related impairments in safety learning are evident within 30 days of trauma exposure.
Keywords: anxiety disorders, biological markers, PTSD, startle, trauma
INTRODUCTION
Exposure to an event that causes extreme fear, horror, or helplessness, such as combat exposure, violent assault, or major disaster[1] can result in trauma-related anxiety disorders such as posttraumatic stress disorder (PTSD), considered the fourth most common psychiatric diagnosis.[2] PTSD is characterized by three primary symptom clusters following a traumatic experience (DSM-IV Criterion A; e.g. combat exposure, motor vehicle accident, major disaster).[3] The first cluster of symptoms (DSM-IV Criterion B) includes re-experiencing of the traumatic event through intrusive thoughts, nightmares, flashbacks, and related phenomena that are often produced by reminders of the traumatic event. The second cluster (DSM-IV Criterion C) is characterized by avoidance symptoms including loss of interest in social situations and emotional detachment. The third cluster (DSM-IV Criterion D) includes psychophysiological reactivity in response to trauma-related stimuli including exaggerated startle, hypervigilance, elevated perspiration, and shortness of breath.[1] Time elapsed since trauma is an important diagnostic criterion because in many cases the initial response to trauma may resolve itself within 1 month’s time. In order to aid in the early identification of potentially vulnerable individuals who might develop PTSD, the diagnosis of acute stress disorder (ASD) was introduced in 1994 in the DSM-IV.[4] This disorder has the same symptoms as PTSD, except that it is diagnosed within a month of trauma exposure, and has a greater focus on dissociative symptoms.[4] Given that exaggerated startle and related hyperarousal symptoms are shared between ASD and PTSD, the current study was designed to investigate whether the time elapsed since trauma exposure affects inhibition of fear responses, an impairment previously observed in combat and civilian PTSD.[5, 6] A study of Israeli trauma patients found that some psychophysiological markers such as increased heart rate and startle responses were not evident in the first months posttrauma, but developed by 4 months after trauma.[7] Similarly, our previous study of Vietnam veterans with chronic PTSD indicated that fear inhibition was impaired in those who continued to present high levels of symptoms more than 30 years after trauma exposure, but not in those veterans who showed improvement.[5] Based on these previous findings, we hypothesized that fear inhibition would be impaired in chronic PTSD, but not in ASD patients.
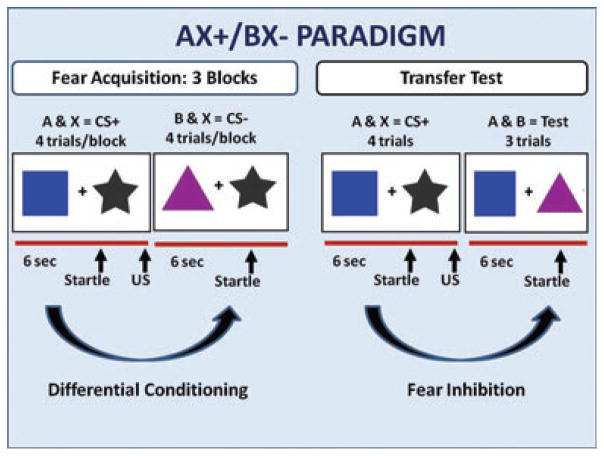
We have recently developed an experimental paradigm that allows for the independent evaluation of fear potentiation and fear inhibition in humans.[8] The procedure, referred to as a conditional discrimination (abbreviated as AX+/BX−, see Fig. 1), was translated from a rodent model of fear inhibition[9] based on early learning theory experiments.[10, 11] In this paradigm, the participants learn that A and X together predict the delivery of an aversive airblast (i.e. danger signal), whereas the B and X compound cue predicts the absence of the airblast (i.e. safety signal). Next, the presentation of A and B together reduces fear responses as the inhibitory properties of stimulus B are transferred to stimulus A. Thus, the AB trials are referred to as “Transfer Test” trials, and measure fear inhibition. Our previous studies of traumatized populations using this paradigm have shown that PTSD is associated with impaired fear inhibition.[5] However, the trauma exposure in our previous work occurred many years prior to our assessment. Therefore, it is possible that impaired fear inhibition develops as a result of chronic PTSD, and is most evident in those with severe symptoms that persist long after trauma.
Figure 1.
Schematic representation of the AX+/BX− experimental paradigm.
In the current study, we examined whether impaired inhibition was evident soon after trauma exposure. Our study population consisted of traumatized Croatian civilians and combat veterans. The Regional Center for Psychotrauma in Croatia found 15% prevalence of current PTSD in veterans from the Croatian war that ended in 1995.[12] We hypothesized transfer of safety would be related to the recency of trauma exposure, in that the patients with the longest time since trauma exposure would have the most difficulty inhibiting fear.
MATERIALS AND METHODS
PARTICIPANTS
The study included 78 participants: 51 of which were treated at the University Hospital Dubrava, Croatia, for a diagnosis of PTSD (n = 24), or ASD (n = 27), and 27 healthy controls. Trauma exposure was assessed in all participants using the Life Events Checklist (LEC,[13] see description below). All PTSD patients were combat veterans of the Croatian war (1991–1995) and their PTSD diagnosis was due to a combat-related index trauma. The ASD patients were recruited within 30 days of trauma exposure and their ASD diagnosis was due to a civilian trauma. Of the 27 ASD patients, 16 had experienced a violent assault, and 11 had experienced a motor vehicle accident. The healthy controls did not have any history of trauma exposure. Participants were recruited for the study from 2005 to 2010. All subjects were screened with an audiometer (Grason-Stadler, Model GS1710); and were required to detect tones at 30-dB (A) sound pressure level (SPL) at frequencies ranging from 250 to 4,000 Hz. Participants were informed of the research study and signed an informed consent form approved by the Committee for Ethical Conduct of Research, University Hospital Dubrava, Zagreb, Croatia.
Inclusion Criteria
PTSD group: Confirmed diagnosis of PTSD by the Clinician-Administered PTSD Scale (CAPS[14]).
ASD group: confirmed diagnosis of ASD by the Acute Stress Disorder Interview (ASDI[15]).
Exclusion Criteria
Current substance abuse or dependence, suicidal ideation, head injury or neurological disorder, psychotic and bipolar symptoms, hearing or visual impairment (determined by audiometer as described above), liver or kidney disease, and cardiovascular disease. In addition, the healthy control group did not meet any DSM-IV criteria on the Mini-International Neuropsychiatric Interview (MINI[16], Croatian version). All psychiatric evaluations were conducted by experienced clinicians at the University Hospital Dubrava.
EXPERIMENTAL DESIGN
Fear-potentiated startle and inhibition of fear-potentiated startle were assessed using the AX+/BX− conditional discrimination paradigm.[8] Figure 1 shows a schematic of the experimental design. Each conditioned stimulus (CS) was a compound of two shapes presented simultaneously on a computer monitor. The AX+ compound served as the reinforced stimulus (CS+), and the BX− compound served as the nonreinforced stimulus (CS−). For any given pair, the cues differed on both color and shape (and were counterbalanced across subjects). Each compound CS had one novel cue (A or B) and one common cue “X.” The fear inhibition test stimulus was a compound of the previously conditioned A and B cues that was used to determine transfer of safety (by B) to the danger cue.[8, 9] The unconditioned stimulus (US) was a 250-ms airblast with an intensity of 140 psi directed to the larynx. The startle probe was a 108-dB (A) SPL, 40-ms burst of broadband noise with near instantaneous rise time, delivered binaurally through headphones (Maico, TDH-39-P). Both CSs were 6 s in duration, see Fig. 1.
The session began with a Habituation phase consisting of six noise-alone (NA) startle trials. Immediately following habituation, participants underwent the Fear Acquisition phase, which consisted of three blocks, each of which included four trials of each CS type and four NA trials for 12 trials per block. For the Transfer Test of fear inhibition, a block of three AB trials and three NA trials, followed by another AX+ block, was presented after the Fear Acquisition phase. All AX+ trials were reinforced with the US, whereas the BX− and AB trials were not reinforced. During AX+ trials, the 250-ms air-blast coterminated with the CS, and the startle probe preceded the airblast by 500 ms. The BX− trials terminated immediately after the presentation of the startle probe. The AB trials were designed the same way as the BX− trials. In all phases of the experiment, intertrial intervals were of randomized duration ranging from 9 to 22 s.
INTERVIEW MEASURES
LEC[13] is a measure of trauma exposure that was developed by the National Center for PTSD and distributed as part of the CAPS to assess for criterion A trauma. It assesses the degree of exposure to 16 trauma items. This instrument has high reliability, with mean kappa values for all items of .61, and a test–retest correlation of r = .82, P < .001. All three groups (ASD, PTSD, and controls) were assessed for trauma exposure using the LEC.
Mini-International Neuropsychiatric Interview (MINI[16])
The MINI is a short structured diagnostic interview for both DSM-IV and ICD-10 psychiatric disorders, validated with the Structured Clinical Interview for DSM. The present study used a Croatian translation of the MINI, which was administered to all participants.
Clinician-Administered PTSD Scale (CAPS[14])
The CAPS is a reliable, valid interview measure of PTSD based on DSM-IV that yields PTSD symptom frequency and intensity. It is the “gold standard” measure for PTSD diagnosis, with high reliability (κ’s above .75) and sensitivity (Cohen’s κ’s above .50).[17] The CAPS was administered to the PTSD patients to confirm diagnosis.
Acute Stress Disorder Interview (ASDI[15])
The ASDI is a structured interview for diagnosing ASD based on DSM-IV criteria. It has strong test–retest reliability (r = .88), and diagnostic agreement for presence (88%) and absence (94%) of ASD diagnosis is high. The ASDI possessed good internal consistency (r = .90), sensitivity (91%), and specificity (93%).[15] The ASDI was administered to the ASD group to confirm diagnosis.
PSYCHOPHYSIOLOGY MEASURES
Acoustic startle responses were measured using electromyographic (EMG) recordings and electrodermal activity (EDA) was measured using skin conductance responses (SCRs). These data were sampled at 1,000 Hz and amplified using the respective modules of the Biopac MP150 system (Biopac, Inc., Goleta, CA). The acquired data were filtered, rectified, and smoothed in MindWare software (MindWare Technologies, Inc., Gahanna, OH) and exported for statistical analyses using the SPSS 19.0 software suite. As previously described[6, 18] the eyeblink component of the startle response was measured by EMG activity recorded from two 5-mm Ag/AgCl electrodes placed over the orbicularis oculi muscle, approximately 1 cm under the pupil and 1 cm below the lateral canthus. The impedances for all participants were less than 6 kΩ. The EMG signal was filtered with low- and high-frequency cutoffs at 28 and 500 Hz, respectively. Startle magnitude was assessed as the peak amplitude of the EMG contraction 20–200 ms following the acoustic stimulus. EDA was measured using two Ag/AgCl electrodes on the hypothenar surface of the nondominant hand. The SCR was analyzed from EDA, which was defined as the average increase in skin conductance level (from a 1-s pre-CS onset baseline) from 3 to 6 s after the CS onset.[19] EMG and SCR were scored and edited for artifacts using MindWare EMG and EDA modules, respectively. Nonresponders were not excluded from the analyses, in order to capture individuals with low responses.
CONTINGENCY AWARENESS MEASURES
A response keypad (SuperLab, Cedrus Corp., San Pedro, CA) was used to collect trial-by-trial ratings of US expectancy similar to previously published methods.[5, 20] Each trial contained two shape components (e.g. A and X). Subjects were instructed to respond to each shape combination separately on each trial by pressing one of three buttons: the “+” key when they expected a shape combination to be followed by the airblast (DANGER), the “−” key when they did not expect a shape combination to be followed by the airblast (SAFETY), and the “0” key when they were uncertain of what to expect. Subject responses of “+” were scored as +1, responses of “0” were scored as 0, and responses of “−” were scored as −1.
DATA ANALYSIS
The group variables in the analyses included three groups: control, PTSD, and ASD. Fear potentiation of the startle response was measured by comparing startle magnitude on the NA trials and the AX+ trials using a two-way repeated-measures analysis of variance (RM-ANOVA) with the between-groups factor of group (control, PTSD, ASD) and within-subjects factor of trial type (NA, AX+).
Differential conditioning to AX+ and BX−, and fear inhibition to AB was measured by calculating percent potentiation for each CS type, in order to account for individual differences in startle magnitude as well as startle habituation. This value was derived as follows: Percent Startle Potentiation = 100 × (startle magnitude during CS trials − NA startle)/(NA startle). For differential conditioning, we compared the average percent potentiation to AX+ and BX− during Fear Acquisition. SCRs were square-root transformed and averaged for AX+ and BX− trials during Fear Acquisition. Response pad data were also averaged for the AX+ and BX− trial types in order to assess contingency awareness during Fear Acquisition. These variables were analyzed using a two-way RM-ANOVA with group and trial type (AX+, BX−).
Fear inhibition was measured by calculating percent potentiation of the startle response to AX+ and AB trials during the Transfer Test phase. SCR and response pad data during the Transfer Test phase were also analyzed. For these analyses, we also used a two-way RM-ANOVA with group and trial type (AXtest, AB). In all RM-ANOVAs, we used the Greenhouse–Geisser statistic with an alpha level of .05. Significant between-groups differences were followed up by post hoc Tukey HSD tests. Effects size is shown as partial eta squared (η2).
RESULTS
DEMOGRAPHIC AND CLINICAL DESCRIPTION
The three groups did not differ on age, mean (SD): control, 37.9 (8.9) years, PTSD, 40.0 (4.9) years, and ASD, 39.2 (12.0) years, F(2,77) = 0.36, ns. There was a differential distribution of sex across groups: the control group was 70% male population, the PTSD group included only males, but the ASD group was only 30% male population, χ2 = 32.2, P < .001. All participants were of Caucasian and Croatian nationality. The mean and SEM CAPS score for the PTSD patients was 56.4 (15.2) (highest possible score is 136[14]), and the mean and SEM ASDI score for the ASD patients was 15.1 (2.1) (highest possible score is 19[15]).
FEAR-POTENTIATED STARTLE
Fear-potentiated startle was measured by comparing startle magnitude on the NA trials and the AX+ trials using a two-way RM-ANOVA with the between groups factor of group (control, PTSD, ASD) and within subjects factor of trial type (NA, AX+). This analysis revealed a significant main effect of trial type (F(1,75) = 61.20, P < .001, η2 = 0.45), a main effect of group (F(2,75) = 10.12, P < .001, η2 = 0.21), and an interaction effect of the two variables (F(2,75) = 6.59, P = .002, η2 = 0.15). Comparison of NA to AX+ within each group showed that all groups had significant fear-potentiated startle responses, control (F(1,26) = 29.26, P < .001, η2 = 0.53), PTSD (F(1,23) = 17.86, P < .001, η2 = 0.44), and ASD (F(1,26) = 26.85, P < .001, η2 = 0.51). However, the startle magnitude on both trial types was greater for the ASD group compared to controls (P = .05) and PTSD subjects (P < .001). Given the differential distribution of men and women across the three groups, we repeated the analysis with the variable sex as a covariate. Although the main effect of trial type was still significant (F(1,74) = 15.00, P < .001, η2 = 0.17), there was no longer a significant main effect of group, and no interaction effect of trial type and group.
DIFFERENTIAL CONDITIONING
For differential conditioning, we compared AX+ and BX− during Fear Acquisition, using percent fear-potentiated startle (Fig. 2a), SCR (Fig. 2b), and US-expectancy ratings (Fig. 2c) as dependent measures. The analysis showed significant discrimination between AX+ and BX− on all measures: startle (F(1,75) = 37.34, P < .001, η2 = 0.33), SCR (F(1,75) = 14.28, P < .001, η2 = 0.16), and US expectancy (F(1,72) = 246.31, P < .0001, η2 = 0.78). US-expectancy data from three individuals (all ASD) were missing. However, there were no significant effects of group on any of the measures. The only variable that demonstrated an interaction effect of group and trial type was US expectancy; follow-up comparisons of trial type within each group showed significant discrimination between AX+ and BX− in all groups, controls (F(1,26) = 381.90, P < .0001, η2 = 0.94), PTSD (F(1,23) = 29.35, P < .001, η2 = 0.58), and ASD (F(1,23) = 60.89, P < .001, η2 = 0.73). We repeated the 2 × 3 RM-ANOVA with sex as a covariate, and again found a significant effect of trial type with startle (F(1,75) = 14.17, P < .001, η2 = 0.16), SCR (F(1,75) = 9.11, P = .003, η2 = 0.11), and US-expectancy ratings (F(1,72) = 120.17, P < .001, η2 = 0.64), and no effect of group on any of the variables.
Figure 2.
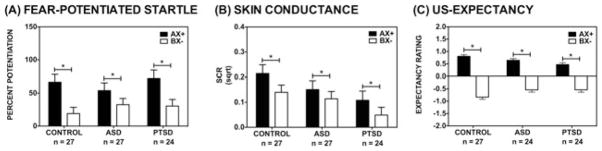
Differential conditioning between the reinforced danger cue (AX+), and the nonreinforced safety cue (BX−) measured by (A) fear-potentiated startle; (B) skin conductance response; and (C) US expectancy. There were significant effects of trial type with each dependent variable across all three groups.
TRANSFER TEST OF FEAR INHIBITION
For the Transfer Test of fear inhibition, we compared the AB trials to the AX+ trials during the test phase, with the dependent variables of fear-potentiated startle (Fig. 3a), SCR (Fig. 3b), and US-expectancy ratings (Fig. 3c). Using fear-potentiated startle, we did not find an overall main effect of trial type, group, or interaction effect. Using SCR, we also did not find a significant effect of trial type; however, there was a main effect of group (F(2,75) = 3.92, P = .02, η2 = 0.10), with the PTSD group having less SCR than controls (P = .02). Conversely, US expectancy was markedly higher for AX+test, than AB (F(1,72) = 119.01, P < .001, η2 = 0.62), but there was no effect of group or interaction with group.
Figure 3.
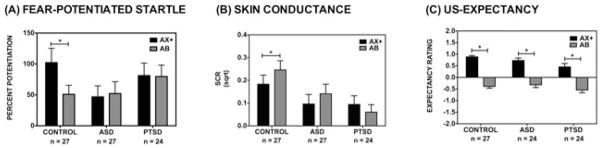
Fear inhibition between the reinforced danger cue (AX+), and the transfer of safety (AB) measured by (A) fear-potentiated startle; (B) skin conductance response; and (C) US expectancy. There was a significant effect of trial type in the control group (P = .001), but not in PTSD or ASD groups with fear-potentiated startle measures. With the SCR measure, there was also a significant effect of trial type in controls (P = .02), but neither trauma group. However, the effect in the controls was a greater SCR to the safety signal. All three groups showed a significant effect of trial type on the US-expectancy measure (all Ps < .001).
Given our a priori hypotheses that time since trauma would affect fear inhibition, we compared AX+test to AB within each group, using a RM-ANOVA with trial type across each dependent variable. This analysis revealed significant inhibition of fear-potentiated startle in controls (F(1,26) = 12.64, P = .001, η2 = 0.33), but not in the PTSD or ASD groups (both Fs < 1.00). With respect to SCR, the control group showed higher SCR to AB trials compared to AX+test (F(1,26) = 6.41, P = .003, η2 = 0.20), but neither the PTSD nor the ASD group showed an effect of trial type. Yet, all three groups demonstrated robust fear inhibition using US-expectancy measures: controls (F(1,26) = 135.95, P < .0001, η2 = 0.84), PTSD (F(1,23) = 24.51, P < .001, η2 = 0.52), and ASD (F(1,23) = 24.53, P < .001, η2 = 0.52).
In order to control for the effects of sex, we repeated the above analyses with the variable sex as a covariate. Again, we found that fear-potentiated startle was reduced to AB compared to AX+test trials in the control group (F(1,25) = 10.94, P = .003, η2 = 0.30), but not in the PTSD or the ASD groups. SCR was marginally higher in the AB trials than the AX+test trials in the control group (F(1,25) = 3.73, P = .07, η2 = 0.13), with no effect in the other two groups. US-expectancy ratings were still significantly lower to AB compared to AX+test trials after covarying for sex (F(1,73) = 48.52, P < .001, η2 = 0.48) and did not differ across groups.
DISCUSSION
The current study employed the AX+/BX− conditional discrimination paradigm to examine the effect of trauma recency on fear inhibition. Time elapsed since trauma was greater than 10 years in the PTSD group and 30 days or less in the ASD group. The psychiatrically healthy control group was not exposed to trauma. We found that all three groups showed significantly higher startle magnitude in the presence of the danger cue; however, across all trial types, startle magnitude was highest in the ASD group. We also found that all three groups showed significant discrimination between the reinforced cue (danger signal) and the non-reinforced cue (safety signal), on all response measures. However, transfer of fear inhibition in the presence of a safety signal was only found in the control group based on fear-potentiated startle responses. Both PTSD and ASD patients demonstrated impaired inhibition of fear-potentiated startle; therefore the data did not support our hypothesis that impaired inhibition develops over time and would only be evident in the PTSD group. SCR did not demonstrate transfer of fear inhibition in any group, while expectancy ratings showed robust fear inhibition in all groups.
In our previous studies using the AX+/BX− paradigm, we have found the PTSD patients show impaired transfer of fear inhibition,[5, 6] an experimental observation that may underlie the clinical expression and persistence of fear-related stress disorder symptoms. This is the first study to use this paradigm to examine the effect of time since trauma and one of the few translational studies to empirically compare acute and chronic posttraumatic stress responses (for discussion see Yehuda et al.[21]). As in our previous studies, the PTSD group showed impaired inhibition of fear-potentiated startle, despite showing fear conditioning and stimulus discrimination between the danger and safety cues similar to healthy controls. However, in contrast to our hypothesis that longer time since trauma would be related to impaired fear inhibition, the ASD group showed similar results as the PTSD group, in that they displayed normal fear conditioning and stimulus discrimination, but impaired transfer of safety to the AB trials. This finding underscores the deficit in generalizing safety cues, in that the patients were able to learn safety on the BX− trial, but could not apply it to a novel situation on the AB trial. Furthermore, similar to our prior studies of traumatized individuals, there was dissociation between psychophysiological measures and contingency awareness: the ASD and PTSD groups showed normal discrimination and transfer of inhibition based on their cognitive responses but not in their startle responses. This is in parallel to clinical observations of PTSD patients who can cognitively identify dangerous and safe cues (e.g. combat-related stimuli such as improvised explosive device explosions vs. domestic-related stimuli such as fireworks) but experience equivalent physiological levels of fear to both stimuli types.[22]
A novel component of the current study was the addition of SCR in the AX+/BX− paradigm. Although this measure showed discrimination between danger and safety cues, there was no transfer, even in the control group. In fact, the controls exhibited a significant increase in response to the AB transfer trials. Given that SCR is highly sensitive to novelty and arousal,[23] it may not be an appropriate index for the Transfer Test, which includes only three trials of a novel combination of CSs. In our prior studies, we have found that fear-potentiated startle may be more sensitive to measures of posttraumatic psychopathology than SCR.[19]
LIMITATIONS
A significant advantage of the current study is that the three groups did not differ in age; an important consideration given the large difference in time since trauma. However, there are key limitations to the study. First, in addition to the variable of time since trauma, the PTSD and ASD groups differ in type of trauma exposure. The PTSD group experienced only combat trauma, whereas all the ASD subjects experienced only civilian trauma. We have used the AX+/BX− paradigm in both trauma populations (i.e. Vietnam veterans with PTSD[5] and victims of inner-city violence[6] with PTSD), and have found that both have impaired transfer of fear inhibition. From a study design perspective, it is difficult to assess combat veterans within 30 days of trauma[24] and, as such, a direct longitudinal study of combat veterans with ASD and subsequent chronic PTSD may prove challenging. On the other hand, because we did not find differences between ASD and PTSD in fear inhibition in this instance, it seems that neither trauma type nor time since trauma had an effect, and thus were less likely to be confounded. This study suggests that fear inhibition is not developed as part of the chronic psychopathology of PTSD, but is present very early in the symptom presentation of trauma-related disorders.
Second, the distribution of men and women differed significantly among groups. The PTSD group contained only men, whereas the ASD and control groups included men and women. In an attempt to control for these differences, we repeated all significant analyses adding sex as a covariate. The only significant effect that was removed after covarying for sex, was increased startle magnitude in the ASD group. Our previous study examining baseline startle magnitude across menstrual cycle did not find any sex differences in startle magnitude,[25] suggesting that baseline startle levels may be associated with trauma recency. This would be consistent with an early review of the startle literature indicating that exaggerated startle was found in subjects with recent trauma, but not in most studies examining PTSD from trauma more than 10 years in the past.[26] Our own prospective study of traumatized individuals tested at 1 and 6 months post-trauma found that those who met criteria for PTSD at 6 months had much higher startle magnitude at 1 month compared to those who recovered.[27] On the other hand, a prospective study that examined psychophysiological responses to loud sounds for 4 months after trauma exposure found that eyeblink EMG gradually increased in individuals who met criteria for PTSD.[28] However, the auditory stimulus (500 ms) was much longer than the startle stimulus (40 ms) used in our studies, potentially evoking a sympathetic response. Several studies have found that increased heart rate in the months after trauma is predictive of PTSD,[28–30] suggesting sensitization of the sympathetic nervous system.
FUTURE DIRECTIONS
This study found that impaired fear inhibition is evident in the immediate aftermath of trauma and is not specific to chronic PTSD. A longitudinal prospective study of the same subjects within 30 days of trauma exposure tested again after an extended time since trauma would show whether impaired fear inhibition may be an early predictor of long-term sequelae. Another possibility is that impaired fear inhibition is a risk factor predating the trauma exposure; studies looking at inhibition pre- and posttrauma would focus on this issue. A study that examined extinction of conditioned fear (which involves inhibition of fear to the extinguished cue) before and after trauma exposure in firefighters found that deficient extinction pretrauma was a vulnerability for PTSD symptoms.[31] More studies of this type are necessary to assess impaired fear inhibition as a risk factor for trauma-related psychopathology.
CONCLUSION
In summary, an impaired ability to transfer learned safety is present in traumatized individuals soon after their traumatic experience and as a feature of chronic PTSD. Thus, effective clinical interventions for the fear-related symptoms of PTSDs, that often rely on the principles of fear learning and fear inhibition,[32] may require an increased focus on strengthening inhibitory processes while reducing robust excitatory fear memories that perpetuate PTSD symptoms such as re-experiencing and hyperarousal.
Acknowledgments
This research was supported by funding from NIMH (MH092576 to TJ; MH47840 to MD), NIDA (DA018294 to ED), DoD (CDMRP; #W81XWH-08–2-0170 to SDN), NARSAD, and the Croatian Ministry of Science, Education and Sport to DK-K. We also thank Slavica Esterajher for her assistance with patient recruitment and testing.
References
- 1.APA. Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 2.Breslau N, Peterson EL, Poisson LM, et al. Estimating post-traumatic stress disorder in the community: lifetime perspective and the impact of typical traumatic events. Psychol Med. 2004;34(5):889–898. doi: 10.1017/s0033291703001612. [DOI] [PubMed] [Google Scholar]
- 3.Association AP. (DSM-IV-TR) Diagnostic and Statistical Manual of Mental Disorders, Text Revision. 4. Washington, DC: American Psychiatric Press, Inc; 2000. [Google Scholar]
- 4.Bryant RA, Harvey AG. Acute stress disorder: a critical review of diagnostic issues. Clin Psychol Rev. 1997;17(7):757–773. doi: 10.1016/s0272-7358(97)00052-4. [DOI] [PubMed] [Google Scholar]
- 5.Jovanovic T, Norrholm SD, Fennell JE, et al. Posttraumatic stress disorder may be associated with impaired fear inhibition: relation to symptom severity. Psychiatry Res. 2009;167(1–2):151–160. doi: 10.1016/j.psychres.2007.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jovanovic T, Norrholm SD, Blanding NQ, et al. Impaired fear inhibition is a biomarker of PTSD but not depression. Depress Anxiety. 2010;27(3):244–251. doi: 10.1002/da.20663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shalev A, Peri T, Brandes D, et al. Auditory startle response in trauma survivors with posttraumatic stress disorder: a prospective study. Am J Psychiatry. 2000;157(2):255–261. doi: 10.1176/appi.ajp.157.2.255. [DOI] [PubMed] [Google Scholar]
- 8.Jovanovic T, Keyes M, Fiallos A, et al. Fear potentiation and fear inhibition in a human fear-potentiated startle paradigm. Biol Psychiatry. 2005;57(12):1559–1564. doi: 10.1016/j.biopsych.2005.02.025. [DOI] [PubMed] [Google Scholar]
- 9.Myers KM, Davis M. AX+, BX− discrimination learning in the fear-potentiated startle paradigm: possible relevance to inhibitory fear learning in extinction. Learn Mem. 2004;11(4):464–475. doi: 10.1101/lm.74704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wagner AR, Logan FA, Haberlandt K, et al. Stimulus selection in animal discrimination learning. J Exp Psychol. 1968;76:171–180. doi: 10.1037/h0025414. [DOI] [PubMed] [Google Scholar]
- 11.Rescorla RA, Wagner AR. A theory of Pavlovian conditioning: variations in the effectiveness of reinforcement and nonreinforcement. In: Black AH, Prokasy WF, editors. Classical Conditioning II: Current Theory and Research. New York, NY: Appleton-Century-Crofts; 1972. pp. 64–99. [Google Scholar]
- 12.Kozarić-Kovacić D, Borovecki A. Prevalence of psychotic comorbidity in combat-related post-traumatic stress disorder. Mil Med. 2005;170(3):223–226. doi: 10.7205/milmed.170.3.223. [DOI] [PubMed] [Google Scholar]
- 13.Gray MJ, Litz BT, Hsu JL, et al. Psychometric properties of the Life Events Checklist. Assessment. 2004;11(4):330–341. doi: 10.1177/1073191104269954. [DOI] [PubMed] [Google Scholar]
- 14.Blake DD, Weathers FW, Nagy LM, et al. The development of a clinician-administered PTSD scale. J Trauma Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- 15.Bryant RA, Harvey AG, Dang ST, et al. Assessing acute stress disorder: psychometric properties of a structured clinical interview. Psychol Assess. 1998;10(3):215–220. [Google Scholar]
- 16.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 17.Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychol Assess. 1999;11(2):124–133. [Google Scholar]
- 18.Norrholm SD, Jovanovic T, Olin IW, et al. Fear extinction in traumatized civilians with posttraumatic stress disorder: relation to symptom severity. Biol Psychiatry. 2011;69(6):556–563. doi: 10.1016/j.biopsych.2010.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Glover EM, Phifer JE, Crain DF, et al. Tools for translational neuroscience: PTSD is associated with heightened fear responses using acoustic startle but not skin conductance measures. Depress Anxiety. 2011;28(12):1058–1066. doi: 10.1002/da.20880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jovanovic T, Norrholm SD, Keyes M, et al. Contingency awareness and fear inhibition in a human fear-potentiated startle paradigm. Behav Neurosci. 2006;120(5):995–1004. doi: 10.1037/0735-7044.120.5.995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yehuda R, McFarlane AC, Shalev AY. Predicting the development of posttraumatic stress disorder from the acute response to a traumatic event. Biol Psychiatry. 1998;44(12):1305–1313. doi: 10.1016/s0006-3223(98)00276-5. [DOI] [PubMed] [Google Scholar]
- 22.Hoge CW. Once a Warrior Always a Warrior: Navigating the Transition from Combat to Home, Including Combat Stress, PTSD and mTBI. Guilford, CT: Globe Pequot Press; 2010. [Google Scholar]
- 23.Lang PJ, Bradley MM, Cuthbert BN. Emotion, motivation, and anxiety: brain mechanisms and psychophysiology. Biol Psychiatry. 1998;44:1248–1263. doi: 10.1016/s0006-3223(98)00275-3. [DOI] [PubMed] [Google Scholar]
- 24.Lee HJ, Goudarzi K, Baldwin B, et al. The combat experience log: a web-based system for the in theater assessment of war zone stress. J Anxiety Disord. 2011;25(6):794–800. doi: 10.1016/j.janxdis.2011.03.018. [DOI] [PubMed] [Google Scholar]
- 25.Jovanovic T, Szilagyi S, Chakravorty S, et al. Menstrual cycle phase effects on prepulse inhibition of acoustic startle. Psychophysiology. 2004;41(3):401–406. doi: 10.1111/1469-8986.2004.00166.x. [DOI] [PubMed] [Google Scholar]
- 26.Grillon C, Baas J. A review of the modulation of the startle reflex by affective states and its application in psychiatry. Clin Neurophysiol. 2003;114(9):1557–1579. doi: 10.1016/s1388-2457(03)00202-5. [DOI] [PubMed] [Google Scholar]
- 27.Kozarić-Kovačić D, Jambrošić-Sakoman A, Jovanovic T. Startle reactivity in acute stress disorder and posttraumatic stress disorder. Stud Health Technol Inform. 2011;167:194–198. [PubMed] [Google Scholar]
- 28.Shalev AY, Peri T, Brandes D, et al. Auditory startle response in trauma survivors with posttraumatic stress disorder: a prospective study. Am J Psychiatry. 2000;157:255–261. doi: 10.1176/appi.ajp.157.2.255. [DOI] [PubMed] [Google Scholar]
- 29.Kuhn E, Blanchard EB, Fuse T, et al. Heart rate of motor vehicle accident survivors in the emergency department, peritraumatic psychological reactions, ASD, and PTSD severity: a 6-month prospective study. J Trauma Stress. 2006;19(5):735–740. doi: 10.1002/jts.20150. [DOI] [PubMed] [Google Scholar]
- 30.Bryant RA. Longitudinal psychophysiological studies of heart rate: mediating effects and implications for treatment. Ann NY Acad Sci. 2006;1071:19–26. doi: 10.1196/annals.1364.002. [DOI] [PubMed] [Google Scholar]
- 31.Guthrie RM, Bryant RA. Extinction learning before trauma and subsequent posttraumatic stress. Psychosom Med. 2006;68:307–11. doi: 10.1097/01.psy.0000208629.67653.cc. [DOI] [PubMed] [Google Scholar]
- 32.Rothbaum BO, Davis M. Applying learning principles to the treatment of post-trauma reactions. Ann NY Acad Sci. 2003;1008:112–121. doi: 10.1196/annals.1301.012. [DOI] [PubMed] [Google Scholar]