Abstract
A 44 year old female patient presented with multiple, painful, relapsing, nodules, plaques with sinuses discharging pus and scars in apocrine gland bearing region since past 17 years. These lesions were clinically and histopathologically suggestive of hidradenitis suppurativa. Our patient was not aware about the flexural pigmentary lesions, comedones and pitted scars which were also clinically and histopathologically suggestive of Dowling–Degos disease.
We are reporting a rare interesting association of Dowling Degos disease and hidradenitis suppurativa which is not reported in Indian literature till date.
Keywords: Association, Dowling-Degos disease, hidradenitis suppurativa
INTRODUCTION
Dowling-Degos disease (DDD) was first described by Dowling and Freudenthal in 1938,[1] then by Degos and Ossipowski in 1954.[2] It is characterized by a reticulate pigmentation of the flexures with prominent comedone like lesions and pitted scars.[3,4,5] The disease runs in families and has an autosomal-dominant mode of transmission with female preponderance.
DDD, or dark dot disease, is a rare pigmentary genodermatosis that has been associated with hidradenitis suppurativa (HS).[5]
HS is a chronically relapsing inflammatory disease that is characterized by recurrent draining sinuses and abscesses occurring predominantly in skin folds that carry terminal hairs and apocrine glands.[6]
HS is widely considered to occur more frequently in females than in males, with a ratio as high as 2–5:1.[7,8] The onset of HS peaks in individuals aged 11–50 years, with an average patient age of 23 years.[8] HS has a predilection for terminal hair follicles and apocrine sweat glands bearing region like axillary, inguinal and perineal regions. Clinically, it is characterized by painful, tender erythematous papules and nodules, abscesses that burst open leading to sinus formation. A deep-seated lesion heals with scarring. The disease has a recurrent and chronic course.
We are reporting a rare interesting association of Dowling-Degos disease (DDD) and HS that is not reported in the Indian literature till date.
CASE REPORT
A 44-year-old female patient presented with multiple painful, tender nodular lesions and plaques with multiple sinuses discharging pus involving the buttocks, inner aspect of upper thigh, perianal region and both upper legs since the past 4 years but which aggravated since 1 month. The patient had similar lesions on and off since the past 17 years. There was no history of similar lesions in any family members. Two years back, she was diagnosed as a case of scrofuloderma and had received anti-tubercular treatment for 6 months. The patient frequently took systemic antibiotics for the skin lesions with only temporary relief.
Cutaneous examination revealed multiple tender nodules and plaques with multiple sinuses discharging pus involving the buttocks, inner aspect of upper thigh, anogenital region [Figures 1 and 2] and both upper legs. Few plaques over the leg revealed crusting [Figure 3]. Post inflammatory atrophic scarring was seen over the lower abdomen and inner aspect of the right thigh [Figure 2]. Bilateral tender inguinal lymphadenopathy was present. The patient also had asymptomatic, multiple, symmetrical, dark brown pigmented macules over the axillae [Figures 4 and 5] and groins. Scattered comedo-like lesions (dark dot follicles) were seen over the abdomen, thighs [Figure 6], back and upper extremity. The patient had multiple discrete pitted scars over the face [Figure 7], back and axillae.
Figure 1.

Multiple nodules and plaques with sinuses discharging pus involving the buttocks
Figure 2.

Nodules, plaques and scars involving the inner aspect of the upper thigh and anogenital region
Figure 3.

Crusted plaque over the right leg
Figure 4.

Multiple dark brown pigmented macules and comedo like lesions (dark dot follicle) involving the right axilla
Figure 5.

Multiple dark brown pigmented macules and comedo (dark dot follicle) involving the left axilla
Figure 6.

Scattered comedo-like lesions (dark dot follicles) involving the right thigh
Figure 7.

Multiple discrete pitted scars over the face
Investigations revealed normal blood counts, liver and renal function tests, but the erythrocyte sedimentation rate was raised. Blood glucose levels were normal. Mantoux test was negative. Pus for gram staining and culture sensitivity revealed gram positive Staphylococcus aureus. Enzyme-linked immunosorbent assay test for human immunodeficiency virus-1 and 2 was negative. Biopsy from the nodular lesion revealed neutrophilic and histiocytic infiltration around the pilosebaceous apocrine units [Figure 8]. Histopathology from the pigmented lesion revealed irregular epidermis, acanthosis and elongation of rete ridges with increased basal melanin pigmentation [Figure 9].
Figure 8.
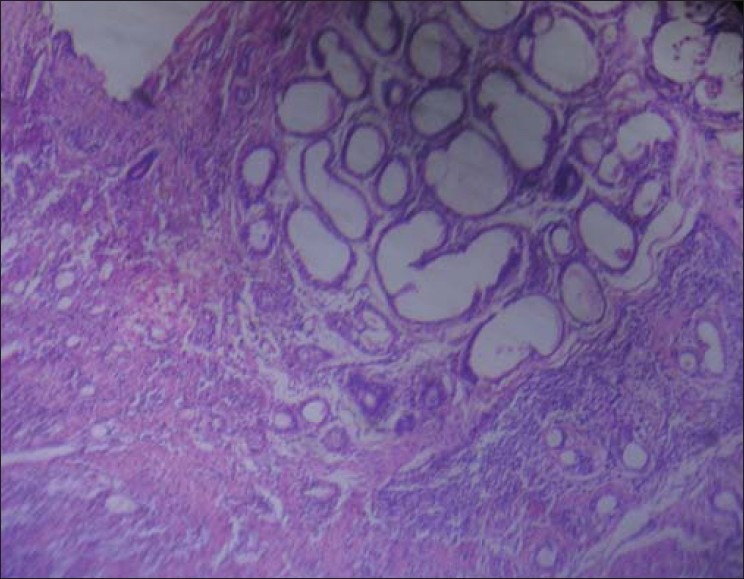
Neutrophilic and histiocytic infiltration around the pilosebaceous apocrine units (H & E, 10X)
Figure 9.
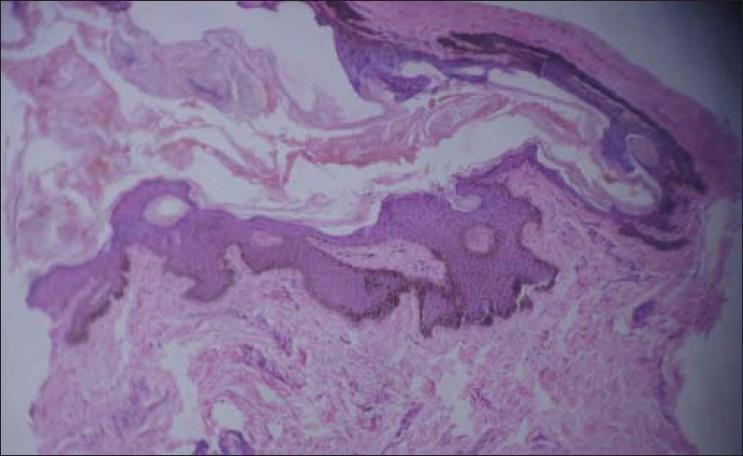
Irregular epidermis, acanthosis and elongation of rete ridges with increased basal melanin pigmentation (H & E, 10X)
DISCUSSION
Our case was a female patient with onset of lesions at the age of 27 years. The patient had chronic relapsing multiple painful nodules, plaques with sinuses discharging pus and multiple scars in the aprocrine gland-bearing region. These lesions were clinically and histopathologically suggestive of HS. Our patient was not aware of the flexural pigmentary lesions, comedones and pitted scars, which were also clinically and histopathologically suggestive of DDD.
A number of diseases have been described to coexist with HS. It has been associated with pigmentary disorders of skin folds (Dowling-Degos and Kitamura's disease), rheumatologic diseases, neutrophilic diseases, cutaneous and other malignancies (squamous cell carcinoma, epidermal cysts, keratoacanthoma).
Loo et al,[3] illustrated the rare association between HS and DDD.
Furthermore, the association of HS, DDD and multiple epidermal cysts has not been described before, but their co-existence in the same patient was likely to reflect the same follicular anomaly.
It is possible that a single underlying defect of follicular proliferation may account for the co existence of these conditions.
Fenske et al,[4] reported a case in which one patient had DDD, HS and multiple keratoacanthomas. Abnormal epithelial proliferation involving mainly the pilosebaceous apparatus has been recognized in all three conditions. They speculated that a single underlying defect in follicular epithelial proliferation, characterized by variable expressivity, accounts for the co-existence of these clinically distinct disorders of follicular derivation.
Li et al,[5] described a patient with HS in association with DDD and perianal squamous cell carcinomas.
Evidence of a true causal relationship between HS and these diseases is weak. Association may be due to co-occurrence rather than a truly common pathogenic mechanism or a gene linkage.
There is paucity of reports in the literature regarding the association of HS and DDD. To the best of our knowledge, there is not a single Indian report of association of DDD and HS.
Footnotes
Source of Support: Nil
Conflict of Interest: NIL
REFERENCES
- 1.Dowling G, Freudenthal W. Acanthosis nigricans. Br J Dermatol. 1938;50:467–71. doi: 10.1177/003591573803100964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Degos R, Ossipowski B. Dermatose pigmentaire reticule des plis. Ann Dermatol Syphilol. 1954;81:147–51. [PubMed] [Google Scholar]
- 3.Loo WJ, Rytina E, Todd PM. Hidradenitis suppurativa, Dowling- Degos and multiple epidermal cysts: A new follicular occlusion triad. Clin Exp Dermatol. 2004;29:622–4. doi: 10.1111/j.1365-2230.2004.01631.x. [DOI] [PubMed] [Google Scholar]
- 4.Fenske NA, Groover CE, Lober CW, Espinoza CG. _Dowling-Degos disease, hidradenitis suppurativa, and multiple keratoacanthomas. A disorder that may be caused by a single underlying defect in pilosebaceous epithelial proliferation. J Am Acad Dermatol. 1991;24:888–92. [PubMed] [Google Scholar]
- 5.Li M, Hunt MJ, Commens CA. _Hidradenitis suppurativa, Dowling Degos disease and perianal squamous cell carcinoma. Aust J Dermatol. 1997;38:209–11. doi: 10.1111/j.1440-0960.1997.tb01700.x. [DOI] [PubMed] [Google Scholar]
- 6.Jansen T, Plewig G. Acne inversa. Int J Derm. 1998;37:96–100. doi: 10.1046/j.1365-4362.1998.00414.x. [DOI] [PubMed] [Google Scholar]
- 7.Jemec GB, Heidenheim M, Nielsen NH. Hidradenitis suppurativa-characteristics and consequences. Clin Exp Dermatol. 1996;21:419–23. doi: 10.1111/j.1365-2230.1996.tb00145.x. [DOI] [PubMed] [Google Scholar]
- 8.von der Werth JM, Williams HC. The natural history of hidradenitis suppurativa. J Eur Acad Dermatol Venereol. 2000;14:389–92. doi: 10.1046/j.1468-3083.2000.00087.x. [DOI] [PubMed] [Google Scholar]


