Abstract
Two-micron (thulium) laser resection of the prostate-tangerine technique (TmLRP-TT) is a transurethral procedure that uses a thulium laser fiber to dissect whole prostatic lobes off the surgical capsule, similar to peeling a tangerine. We recently reported the primary results. Here we introduce this procedure in detail. A 70-W, 2-μm (thulium) laser was used in continuous-wave mode. We joined the incision by making a transverse cut from the level of the verumontanum to the bladder neck, making the resection sufficiently deep to reach the surgical capsule, and resected the prostate into small pieces, just like peeling a tangerine. As we resected the prostate, the pieces were vaporized, sufficiently small to be evacuated through the resectoscope sheath, and the use of the mechanical tissue morcellator was not required. The excellent hemostasis of the thulium laser ensured the safety of TmLRP-TT. No patient required blood transfusion. Saline irrigation was used intraoperatively, and no case of transurethral resection syndrome was observed. The bladder outlet obstruction had clearly resolved after catheter removal in all cases. We designed the tangerine technique and proved it to be the most suitable procedure for the use of thulium laser in the treatment of benign prostatic hyperplasia (BPH). This procedure, which takes less operative time than standard techniques, is safe and combines efficient cutting and rapid organic vaporization, thereby showing the great superiority of the thulium fiber laser in the treatment of BPH. It has been proven to be as safe and efficient as transurethral resection of the prostate (TURP) during the 1-year follow-up.
Keywords: benign prostatic hyperplasia, laser surgery, prostatectomy, tangerine technique, thulium
Introduction
Symptomatic benign prostatic hyperplasia (BPH) is a common problem for aged men. At present, transurethral resection of the prostate (TURP) is the standard surgical treatment. However, the high rate of complications associated with TURP is a major drawback of this procedure. In 1994, Gilling et al. 1, 2 introduced the use of the holmium laser (Ho:YAG) for prostate resection. Use of the Ho:YAG to resect, ablate or enucleate the prostate reduced the complications in the treatment of BPH. Although its safety and efficacy are well-known, the Ho:YAG laser has some limitations, such as its thermal damage zone, which is around 400–500 μm wide 3.
The 2-μm (thulium) laser is a new surgical laser with optional continuous- or pulse-wave modes and a wavelength tunable from 1.75 to 2.22 μm. It has many advantages over the Ho:YAG, including improved spatial beam quality, more precise tissue incision and operation in optional continuous- or pulse-wave modes 4. An earlier study of canine models and human cadavers indicated that the 2-μm (thulium) laser could cause rapid vaporization and coagulation of the prostate 5. On the basis of its cut and ablation characteristics at 50 W, we designed a 2-μm (thulium) laser resection of the prostate-tangerine technique (TmLRP-TT), and the preliminary results in terms of therapeutic efficacy and safety have been reported 6. Recently, the application of a 70-W laser has achieved a significant increase in the speed of the procedure. As more and more surgeons are interested in this technique, in this article we describe it in detail.
Materials and methods
Patients
Symptomatic BPH patients were enrolled with informed consent regarding TmLRP-TT. The symptoms were evaluated according to the international prostate symptom score (IPSS). All patients underwent digital rectal examinations. The mean peak urinary flow rate (Qmax) was tested, and the mean volume of the prostate was estimated by transrectal ultrasound (TRUS, W × H × L × 0.52). The serum total prostate-specific antigen (tPSA) was also tested, and patients with a PSA level above 4 μg/L underwent transrectal ultrasound-guided biopsies to prove the diagnosis of BPH.
Equipment
When receiving spinal anesthesia, all patients were in the lithotrity position. A 2-μm (thulium) laser with a maximum average power of 50 W (it has since been raised to 70 W) and a wavelength of 2 013 nm (LISA laser products OHG, Katlenburg-Lindau, Germany) was used in continuous-wave mode for the procedure. The energy was delivered through 550 μm end-firing PercuFib fibers. The laser fibers were introduced through a Karl Storz 26-Fr continuous flow resectoscope. Saline irrigation was used in all the cases, with an irrigation pressure of 40–60 cm.
Two-micron (thulium) laser resection of the prostate–tangerine technique (Supplementary Video)
Step 1: Resection of the median lobe
The resectoscope is placed into the bladder to estimate the range between bladder neck and verumontanum, and also to ascertain the size and configuration of the prostate.
The first incision is made at the bladder neck directly at the 6 o'clock position (Figure 1). The depth must be sufficiently increased to expose the surgical capsule. As with TURP and Ho:YAG enucleation of the prostate (HoLEP), the surgical capsule serves as a very important guide that will conveniently and clearly help us to dissect the remaining tissue. Then, the incision is lengthened distally from the neck to the verumontanum. When we perform the incision, we combine the experience of Gilling 7 with our own 6. We keep the 2-μm (thulium) laser fiber close to the end of the resectoscope so that we can use the beak of the resectoscope to assist in the separation of tissue and to identify the smooth fibrous layer of the capsule during the incision.
Figure 1.
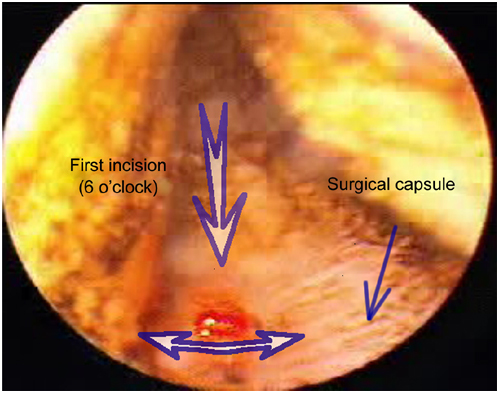
Resection of the median lobe: the first incision is made at the bladder neck directly at the 6 o'clock position. The depth must be sufficiently increased to expose the surgical capsule. Then the incision is lengthened distally from the neck to the verumontanum.
The second and third incisions are made at 5 and 7 o'clock positions, respectively. The two incisions must be kept parallel with the first incision and must be sufficiently deep to reach the capsule. The three incisions divide the median lobe into two pieces of the capsule.
Next, join the incision at 5 and 6 o'clock positions at the level just proximal to the verumontanum and sweep the laser fiber in a transverse cutting motion. Resections will develop deep along the plane of the surgical capsule toward the bladder neck until the left half of the median lobe is detached back into the bladder in a small piece. Resection of the area between 6 and 7 o'clock is carried out in the same way. If the median lobe is extremely enlarged, the two major pieces will be cut and vaporized into fragments of around 1 cm3 before they detach from the bladder (Figure 2).
Figure 2.
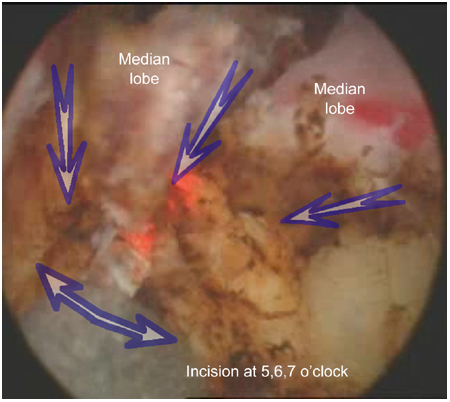
Resection of the median lobe: sweep the laser fiber in a transverse cutting motion along the plane of the surgical capsule toward the bladder neck until the left half of median lobe is detached back into the bladder in a small piece. If the median lobe is extremely enlarged, then two major pieces will be cut and vaporized into fragments of around 1 cm3 before their detachment from the bladder.
The 2-μm (thulium) laser is able to cut the tissue and coagulate small vessels simultaneously. If there is a larger bleeding vessel, we draw the fiber tip away from the tissue, which acts to defocus the laser, enabling us to achieve absolute hemostasis, which can afford clear visibility in the operation. However, take care not to burn the tissue at the 5 or 7 o'clock position. If new users are not very familiar with the sweeping motion, they may perforate the capsule and injure the outer erectile nerve.
Step 2: Resection of the lateral lobes
Resection marks are made at the 3, 1, 9 and 11 o'clock sites at the apex. The resection of the left lobe includes two continuous steps.
First, make a large cutting curve laterally from the 5 o'clock incision to the 3 and 1 o'clock resection marks of the apex (Figure 3). The depth of the incision must be the same as that of the initial bladder neck incision. Second, insert the fiber into the prostate tissue and make a transverse incision at the 3 o'clock position from the capsule toward the urethra. The fiber vibrates, and greatly increases the efficiency of the vaporization and the resection rate (Figure 4). The two incision strokes are repeated, together, from the apex toward the proximal bladder neck.
Figure 3.
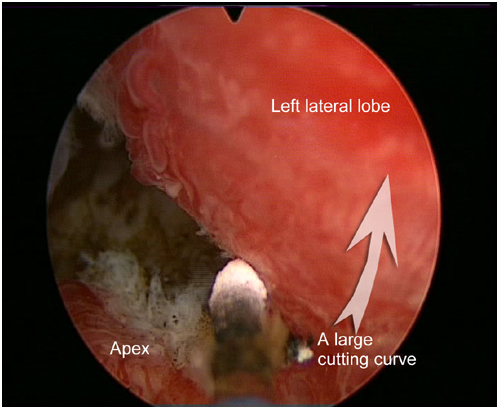
Resection of the lateral lobes: first, a large cutting curve is made laterally from the 5 o'clock incision to the 3 and 1 o'clock resection marks of the apex.
Figure 4.
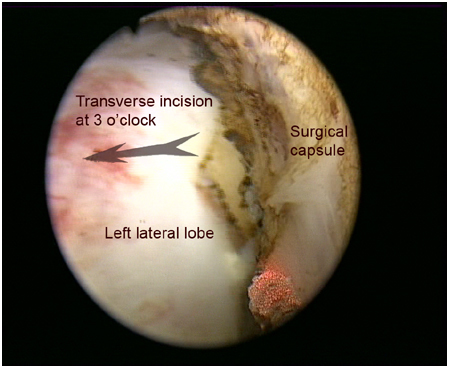
Resection of the lateral lobes: insert the fiber into the prostate tissue and make a transverse incision at the 3 o'clock position from the capsule toward the urethra direction. The fiber vibrates, and greatly increases the efficiency of the vaporization and the resection rate.
The tissue of the prostate is simultaneously resected and vaporized 8. We control the speed of laser fiber sweeping through the tissue to adjust the degree of vaporization. Finally, the left lobe is vaporized into two pieces, dissected away from the capsule, and pushed into the bladder. If the left lobe is extremely enlarged, we may add landmarks and transverse incisions at 2 and 4 o'clock positions. The pieces are sufficiently small to be evacuated through the resectoscope sheath, and the use of the mechanical tissue morcellator is not required.
The resection of the right lobe is achieved in the same way. The entire procedure is like peeling a tangerine, which is why it is named the tangerine technique.
Step 3: Resection of the anterior tissue
The incision is made at the bladder neck, directly at the 12 o'clock position, and then performed distally to the apex (Figure 5). It must be sufficiently deep to reach the surgical capsule. A small cutting curve is made on the capsule plane from the 1 o'clock incision to the 12 and 11 o'clock resection marks at the apex and then extended in a retrograde direction.
Figure 5.
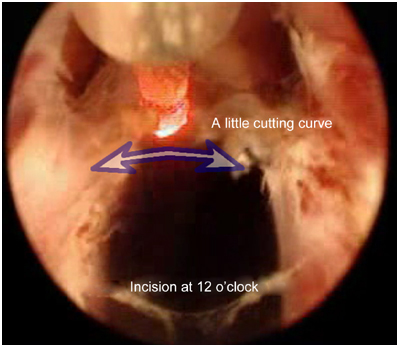
Resection of the anterior tissue: the incision is made at the bladder neck directly at the 12 o'clock position and then carried out distally to the apex. A small cutting curve is made on the capsule plane from the 1 o'clock incision to the 12 and 11 o'clock resection marks at the apex and is then developed in a retrograde direction.
Step 4: Slick the apex and the surface of the prostate
Fasten the laser fiber to the resectoscope and then quickly move the laser handle to resect the residual tissue and smoothen the cutting surface of the prostate (Figure 6). Especially at the apex, it is possible to increase the speed of laser probe movement to enhance the vaporizing effect and reduce heat penetration. The shallow penetration of the laser and the precise cutting provide less opportunity for causing damage to the sphincter of the urethra. Finally, retrieve the tissue pieces from the bladder using a modified grasping forceps technique or an Ellik. Leave a 22-Fr triple catheter for urine drainage.
Figure 6.
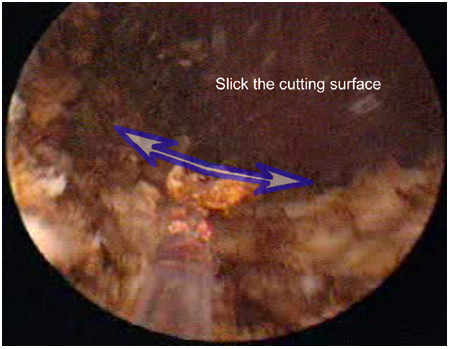
Smoothen the surface of the prostate: quickly move the laser handle to resect the residual tissue and slick the cutting surface of the prostate.
Postoperative care
In total, 500 mg of levofloxacin is administered 1 h before the operation and once a day until catheter removal.
The catheters are removed 1–3 days after the operation in the absence of bladder irrigation. The feasibility of catheter removal and suitability for discharge are assessed between 7:00 and 10:00 hours each postoperative day. Catheters are removed if the urine's color is satisfactorily light. If the catheter cannot be removed, the patient remains in the hospital another night and is reassessed the following day.
Results
No significant bleeding was observed at any stage of the procedure and no significant changes in the hematocrit were observed, suggesting that the TmLRP-TT was a nearly bloodless procedure. Although some patients experienced transient urgency after the removal of the catheter, no severe hematuria, dysuria, incontinence or acute urinary retention occurred in any patient. No patient needed recatheterization. Preoperative and perioperative parameters were also evaluated during the 1-year follow-up. All complications were recorded. Compared with the baseline, there were highly significant improvements in each parameter, including IPSS, quality of life scores (QoLs), Qmax, and post-void residual urine (PVR). Bladder outlet obstruction had clearly resolved by the 1-year follow-up visit 6.
Discussion
The tangerine technique is an almost bloodless procedure with high efficacy for treating symptomatic BPH, with little perioperative morbidity. TmLRP-TT is superior to TURP in safety and is equally efficacious 6.
The thulium laser may have several advantages over the Ho:YAG, including improved spatial beam quality, more precise tissue incision and operation in continuous-/pulse-wave modes. First, the center wavelength of the thulium laser is tunable between 1.75 and 2.22 μm, allowing the wavelength to exactly match the 1.92 μm water absorption peak in the tissue. Higher absorption of the laser radiation at the thulium wavelength results in more efficient and rapid tissue cutting. Second, unlike HoLEP, which is carried out in a pulsed mode, TmLRP-TT is carried out in a continuous-wave mode. As a result, the hemostasis of TmLRP-TT is much better than that of HoLEP. The excellent hemostasis and accurate incision of the 2-μm (thulium) laser ensures the safety of TmLRP-TT. The thulium laser has been proven to be efficacious for the vaporesection of the prostate in another study 9.
Our experience with this novel technique showed the following aspects of optimal performance of the TmLRP-TT: (1) multiple incisions and resection of the median lobe are the key steps, (2) step-by-step resection provides clear endo-anatomic vision to ensure precise incision, (3) incisions at multiple positions enable cutting the prostate adenoma into small pieces, which makes the procedure possible without using the morcellator, thereby decreasing the complication morbidity and cost, and (4) using saline for irrigation makes the serum sodium concentrations quite stable.
Conclusions
In this study, we designed what we call the tangerine technique to completely resect the prostatic adenoma in BPH patients without the help of a morcellator. This procedure, which needs less operative time and possesses high safety, combines efficient cutting and rapid vaporization and shows the great superiority of the 2-μm (thulium) laser in the treatment of BPH.
Supplementary Information accompanies the paper on Asian Journal of Andrology website (http://www.nature.com/aja).
Supplementary Information
References
- Gilling PJ, Cass CB, Malcolm AR, Fraundorfer MR. Combination holmium and Nd:YAG laser ablation of the prostate: initial clinical experience. J Endourol. 1995;9:151–3. doi: 10.1089/end.1995.9.151. [DOI] [PubMed] [Google Scholar]
- Gilling PJ, Cass CB, Cresswell MD, Malcolm AR, Fraundorfer MR. The use of the holmium laser in the treatment of benign prostatic hyperplasia. J Endourol. 1996;10:459–61. doi: 10.1089/end.1996.10.459. [DOI] [PubMed] [Google Scholar]
- Fried NM. Potential applications of the erbium:YAG laser in endourology. J Endourol. 2001;15:889–94. doi: 10.1089/089277901753284080. [DOI] [PubMed] [Google Scholar]
- Fried NM, Murray KE. High-power thulium fiber laser ablation of urinary tissues at 1.94 μm. J Endourol. 2005;19:25–31. doi: 10.1089/end.2005.19.25. [DOI] [PubMed] [Google Scholar]
- Fried NM. High-power laser vaporization of the canine prostate using a 110 W Thulium fiber laser at 1.91 μm. Lasers Surg Med. 2005;36:52–6. doi: 10.1002/lsm.20126. [DOI] [PubMed] [Google Scholar]
- Xia SJ, Zhuo J, Sun XW, Han BM, Shao Y, et al. Thulium laser versus standard transurethral resection of the prostate: a randomized prospective trial. Eur Urol. 2008;53:382–9. doi: 10.1016/j.eururo.2007.05.019. [DOI] [PubMed] [Google Scholar]
- Gilling P. Holmium laser enucleation of the prostate (HoLEP) BJU Int. 2008;101:131–42. doi: 10.1111/j.1464-410X.2007.07341.x. [DOI] [PubMed] [Google Scholar]
- Bach T, Herrmann TR, Ganzer R, Burchardt M, Gross AJ. RevoLix vaporesection of the prostate: initial results of 54 patients with a 1-year follow-up. World J Urol. 2007;25:257–62. doi: 10.1007/s00345-007-0171-x. [DOI] [PubMed] [Google Scholar]
- Wendt-Nordahl G, Huckele S, Honeck P, Alken P, Knoll T, et al. Systematic evaluation of a recently introduced 2-microm continuous-wave thulium laser for vaporesection of the prostate. J Endourol. 2008;22:1041–5. doi: 10.1089/end.2007.0421. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


