Abstract
Esophageal leiomyosarcoma is a rare tumor that accounts for less than 1% of all malignant esophageal tumors. Esophageal leiomyosarcoma combined with squamous cell carcinoma is even rarer than solitary leiomyosarcoma. We experienced a case of leiomyosarcoma combined with squamous cell carcinoma that progressed very rapidly.
Keywords: Leiomyosarcoma, Carcinoma, Squamous cell, Esophagus, Sarcoma
Core tip: We performed esophagectomy with esophagogastrostomy to resect the tumor. Pathological examination of the surgical specimen revealed that it was combined with squamous cell carcinoma. Combined carcinoma should therefore be considered when leiomyosarcoma shows rapid progression.
INTRODUCTION
Leiomyosarcoma of the esophagus is a rare malignant tumor, accounting for less than 1% of all malignant esophageal tumors[1-3]. Esophageal leiomyosarcoma combined with squamous cell carcinoma is even rarer than solitary leiomyosarcoma. Simultaneous esophageal leiomyosarcoma and squamous cell carcinoma were first described by Ovens et al[4] in 1951. Leiomyosarcomas are characterized by slow growth and late metastases, and hence have a better prognosis than squamous cell carcinomas of the esophagus[5,6]. However, we experienced a case of leiomyosarcoma combined with squamous cell carcinoma that progressed very rapidly. We report this case and review the literature.
CASE REPORT
A 72-year-old male visited to our hospital suffering from chest pain that had been present for 1 mo. The patient had been diagnosed with colon cancer and received laparoscopic surgery 1 year prior. The physical examination was unremarkable. He was admitted to the cardiology department, and received electrocardiogram and cardiac single photon emission computed tomography, but no cardiac problem was found. Endoscopic examination demonstrated a stalked intraluminal polypoid mass in the mid esophagus, 30 cm from the incisor (Figure 1). The tumor was large enough to fill the esophageal lumen, but allowed passage of a gastrofiberscope (Q260, Olympus, Tokyo, Japan) to the distal part of the esophagus. An endoscopic biopsy was performed, and the patient was suspected of leiomyoma and leiomyosarcoma. A computed tomography scan showed a large, well enhancing soft tissue mass in the mid esophagus (Figure 2), but no regional lymph node enlargement or liver metastasis. Positron emission tomography/computed tomography (PET-CT) showed intense segmental F-18 fluorodeoxyglucose (FDG) uptake [Standardized Uptake Value (SUV) max 17.3] at the mid-thoracic esophagus. Compared with the previous PET-CT for colon cancer follow-up from 3 mo prior, there was only physiologic FDG uptake at the esophagus (Figure 3). The patient underwent surgery; an esophagectomy with esophagogastrostomy. Macroscopically, the resected specimen was a polypoid tumor measuring 9.8 cm × 5.0 cm × 2.5 cm (Figure 4). Histopathologically, the tumor consisted of pleomorphic spindle cells with mitosis and cell necrosis compatible with leiomyosarcoma (Figure 5A). Tumor invasion involved the muscularis propria, submucosa, and mucosa. Nine regional lymph nodes were free of metastasis. An immunohistochemical examination stained positive for smooth muscle actin, but negative for cytokeratin and S-100 protein (Figure 5B). These were stained by an automated Ventana immunohistochemical/in situ hybridization staining platforms machine (BenchMark XT). Squamous severe dysplasia and focal stratified squamous epithelial invasion into the lamina propria was also noted in the mucosa (Figure 5C). We diagnosed the patient with leiomyosarcoma combined with squamous cell carcinoma.
Figure 1.
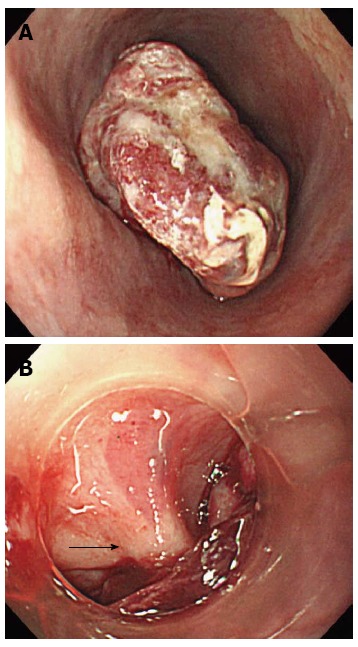
Endoscopic finding. A: Intraluminal polypoid mass; B: Stalk of the mass (arrow).
Figure 2.
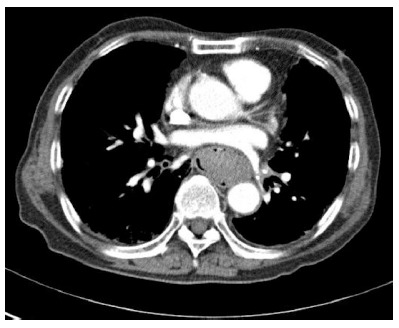
Computed tomography scan showed a large, homogeneously enhancing soft tissue mass.
Figure 3.
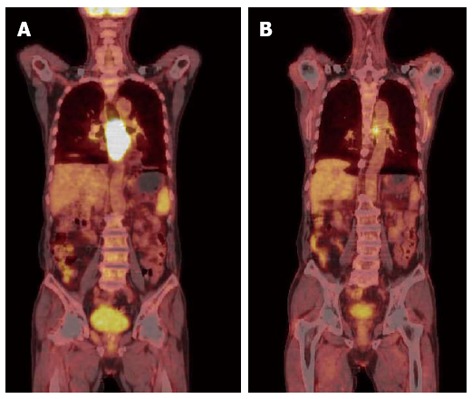
Positron emission tomography/computed tomography. A: Positron emission tomography/computed tomography (PET-CT) showed intense segmental fluorodeoxyglucose uptake (SUV max 17.3) at mid esophagus; B: PET-CT performed at 3 mo ago.
Figure 4.
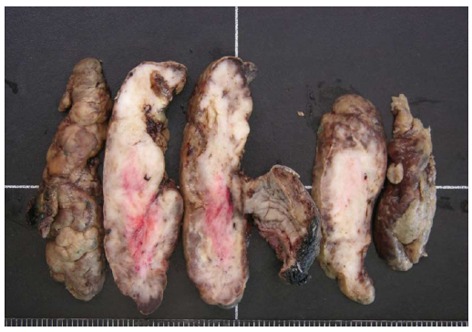
Resected specimen measured about 9.8 cm × 5.0 cm × 2.5 cm.
Figure 5.
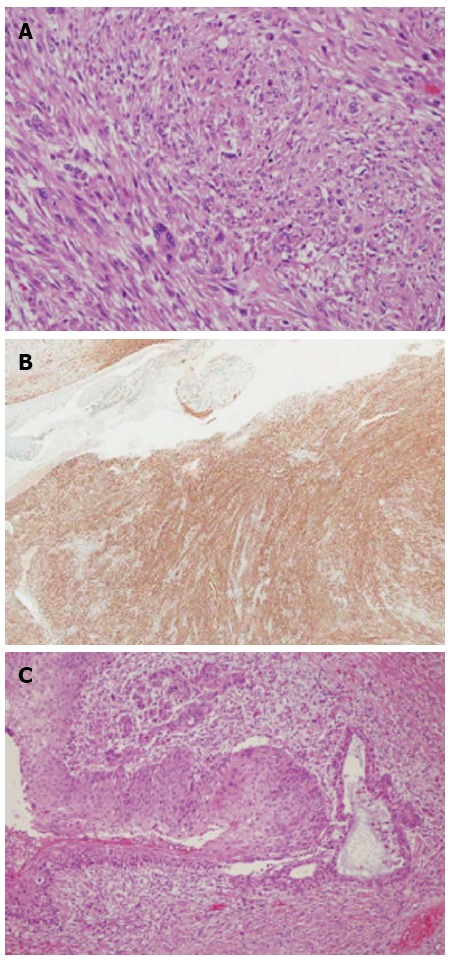
Pathologic images. A: Pleomorphic spindle cells showing mitosis and cell necrosis compatible with leiomyosarcoma [hematoxylin and eosin (HE) stain, × 200]; B: Immunohistochemical stain was positive for smooth muscle actin (× 12); C: Squamous severe dysplasia and focal stratified squamous epithelial invasion into lamina propria was noted in mucosa (HE stain, × 100).
In the post-operative period, the patient recovered uneventfully and was discharged 18 d after operation. No adjuvant radiotherapy or chemotherapy was administered. At the last follow up visit to our hospital 2 mo after surgery, the patient was in good condition without any recurrence or distant metastasis.
DISCUSSION
Leiomyosarcoma is a high grade, smooth muscle soft tissue tumor that can occur in any tissue containing smooth muscle fibers. A leiomyosarcoma combined with squamous cell carcinoma is an extremely rare disease of the esophagus, with very few such cases described[4,5,7-9]. Leiomyosarcomas are most commonly located in the middle and lower thoracic esophagus because smooth muscle predominates in that area[10]. Esophageal leiomyosarcomas are typically divided into two types: the polypoid type in 60% of cases and the infiltrative type in 40% of cases[11,12]. Our case was the polypoid type. The prognosis of esophageal leiomyosarcoma is better than esophageal squamous cell carcinoma because of its characteristics of slow growth and late metastases[5,6]. Patients with polypoid and intramural tumors, tumors in an intrathoracic location, and well-differentiated tumors have a better prognosis than patients with infiltrating lesions, tumors in cervical locations, and poorly differentiated tumors[13,14]. Koga et al[13] reported a case of esophageal leiomyosarcoma that grew rapidly and had a poor prognosis. We think this case is unique because the tumor had good prognostic factors, such as the polypoid type and intrathoracic location, but it grew very rapidly and was combined with squamous cell carcinoma. Eroğlu et al[7] suggested that mutability or metaplasia between mesenchymal and epithelial tissues or multipotent stem cells with the ability to undergo biphasic differentiation toward mesenchymal and epithelial elements could be a mechanism of this combined malignancy. It is possible that these are separate entities that have arisen independently and combined squamous cell carcinoma may affect the growth of leiomyosarcoma by cytokines or growth factors.
The role of FDG-PET-CT in the diagnosis of leiomyosarcoma was reported recently[15-17]. Our case showed intense FDG uptake on PET-CT. The standard treatment is esophagectomy, but the role of adjuvant radiotherapy or chemotherapy is controversial with some authors[2,6,14,18]. In our case, the leiomyosarcoma grew exceptionally rapidly and was combined with squamous cell carcinoma, so further research will be needed to reveal the relationship between leiomyosarcoma and squamous cell carcinoma.
Footnotes
P- Reviewer Yeudall WA S- Editor Zhai HH L- Editor Rutherford A E- Editor Zhang DN
References
- 1.Almeida JM. Leiomyosarcoma of the esophagus. Chest. 1982;81:761–763. doi: 10.1378/chest.81.6.761. [DOI] [PubMed] [Google Scholar]
- 2.Choh JH, Khazei AH, Ihm HJ. Leiomyosarcoma of the esophagus: report of a case and review of the literature. J Surg Oncol. 1986;32:223–226. doi: 10.1002/jso.2930320409. [DOI] [PubMed] [Google Scholar]
- 3.Galandiuk S, Hermann RE, Cosgrove DM, Gassman JJ. Cancer of the esophagus. The Cleveland Clinic experience. Ann Surg. 1986;203:101–108. doi: 10.1097/00000658-198601000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ovens JM, Russell WO. Concurrent leiomyosarcoma and squamous carcinoma of the esophagus. AMA Arch Pathol. 1951;51:560–564. [PubMed] [Google Scholar]
- 5.Camishion RC, Gibbon JH, Templeton JY. Leiomyosarcoma of the esophagus: review of the literature and report of two cases. Ann Surg. 1961;153:951–956. doi: 10.1097/00000658-196106000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Levine MS, Buck JL, Pantongrag-Brown L, Buetow PC, Hallman JR, Sobin LH. Leiomyosarcoma of the esophagus: radiographic findings in 10 patients. AJR Am J Roentgenol. 1996;167:27–32. doi: 10.2214/ajr.167.1.8659399. [DOI] [PubMed] [Google Scholar]
- 7.Eroğlu A, Kürkçüoğlu C, Karaoğlanoğlu N, Erdoğan F, Polat P. Simultaneous leiomyosarcoma and squamous cell carcinoma of the esophagus: report of a new case. Dis Esophagus. 2001;14:245–246. doi: 10.1046/j.1442-2050.2001.00194.x. [DOI] [PubMed] [Google Scholar]
- 8.Gaede JT, Postlethwait RW, Shelburne JD, Cox JL, Hamilton WF. Leiomyosarcoma of the esophagus. Report of two cases, one with associated squamous cell carcinoma. J Thorac Cardiovasc Surg. 1978;75:740–746. [PubMed] [Google Scholar]
- 9.Rella AJ, Farrell JT, Comer JV. Concurrent leiomyosarcoma and squamous cell carcinoma of esophagus. N Y State J Med. 1965;65:1254–1256. [PubMed] [Google Scholar]
- 10.Zhang BH, Zhang HT, Wang YG. Esophageal leiomyosarcoma: clinical analysis and surgical treatment of 12 cases. Dis Esophagus. 2012:Epub ahead of print. doi: 10.1111/j.1442-2050.2012.01444.x. [DOI] [PubMed] [Google Scholar]
- 11.Hatch GF, Wertheimer-Hatch L, Hatch KF, Davis GB, Blanchard DK, Foster RS, Skandalakis JE. Tumors of the esophagus. World J Surg. 2000;24:401–411. doi: 10.1007/s002689910065. [DOI] [PubMed] [Google Scholar]
- 12.Patel SR, Anandarao N. Leiomyosarcoma of the esophagus. N Y State J Med. 1990;90:371–373. [PubMed] [Google Scholar]
- 13.Koga H, Iida M, Suekane H, Aoyagi K, Yao T, Kimura Y, Masuda N, Fujishima M. Rapidly growing esophageal leiomyosarcoma: case report and review of the literature. Abdom Imaging. 1995;20:15–19. doi: 10.1007/BF00199635. [DOI] [PubMed] [Google Scholar]
- 14.Rocco G, Trastek VF, Deschamps C, Allen MS, Miller DL, Pairolero PC. Leiomyosarcoma of the esophagus: results of surgical treatment. Ann Thorac Surg. 1998;66:894–896; discussion 897. doi: 10.1016/s0003-4975(98)00684-5. [DOI] [PubMed] [Google Scholar]
- 15.Grover RS, Kernstine K, Krishnan A. A case of diffuse large B-cell lymphoma in association with paraesophageal leiomyoma: highlighting false-positivity of PET scan and importance of tissue diagnosis. J Natl Compr Canc Netw. 2012;10:577–581. doi: 10.6004/jnccn.2012.0059. [DOI] [PubMed] [Google Scholar]
- 16.Kao YH, Saad U, Tan AE, Magsombol BM, Padhy AK. Fluorine-18-fluorodeoxyglucose PET/CT for the evaluation of suspected recurrent uterine leiomyosarcomas. Acta Radiol. 2011;52:463–466. doi: 10.1258/ar.2011.100509. [DOI] [PubMed] [Google Scholar]
- 17.Manohar K, Mittal BR, Kashyap R, Bhattacharya A, Kakkar N, Mete UK. F-18 fluorodeoxy glucose positron emission tomography/computed tomography findings in a rare case of penile leiomyosarcoma. J Clin Imaging Sci. 2011;1:58. doi: 10.4103/2156-7514.90955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perch SJ, Soffen EM, Whittington R, Brooks JJ. Esophageal sarcomas. J Surg Oncol. 1991;48:194–198. doi: 10.1002/jso.2930480311. [DOI] [PubMed] [Google Scholar]


