Abstract
A new paradigm for an effective delivery of therapeutics into cancer cells is presented. Degradable porous silicon carriers, which are tailored to carry and release a model anti-cancer drug, are biolistically bombarded into in-vitro cancerous targets. We demonstrate the ability to launch these highly porous microparticles by a pneumatic capillary gene gun, which is conventionally used to deliver cargos by heavy metal carriers. By optimizing the gun parameters e.g., the accelerating gas pressure, we have successfully delivered the porous carriers, to reach deep targets and to cross a skin barrier in a highly spatial resolution. Our study reveals significant cytotoxicity towards the target human breast carcinoma cells following the delivery of drug-loaded carriers, while administrating empty particles results in no effect on cell viability. The unique combination of biolistics with the temporal control of payload release from porous carriers presents a powerful and non-conventional platform for designing new therapeutic strategies.
Much effort is devoted to the development of new drug delivery methodologies, focusing on specificity and accuracy aspects. Biolistics has emerged in recent years as a promising non-invasive route for delivering payloads into both cells and tissue. In the biolistic method, originally developed by Klein and coauthors1 for gene expression manipulations, molecules are carried by heavy metal particles, accelerated to high speeds by flow of a gas and launched into the target tissue1. Payloads introduced into target cells by biolistics include DNA, RNA and different dyes2,3,4. This particle-mediated delivery was shown to be effective for delivery into target cells in internal layers of tissue, insensitive to the intrinsic permeability of the cell. Following the original setup, a new pneumatic capillary gene gun has been developed enabling highly localized targeting5,6,7. In this gene gun, the particles are injected into a continuous stream of high-speed Helium (He) in a capillary tube. The stream of He is completely diverted into a coaxial capillary to which vacuum is applied, while the particles continue in their trajectories (Figure 1-A). Due to the active vacuum suction, high He pressures can be applied with no evident gas shock damage to the targeted tissue. In previous studies, the active molecules were spontaneously released in physiological environment, while leaving their carriers intact6,7. In the present study we show for the first time the application of biolistics for highly controlled delivery of therapeutic payloads carried by degradable porous Si (PSi) particles8,9,10,11,12. The highly porous particles (65% porosity), tailored to carry and release a model anti-cancer drug13,14,15,16,17, are lighter (by at least ~2 fold) than the previously used heavy metal particles. Thus, accelerating them biolistically into the target is a challenge. In previous attempts to bombard porous particles (mesoporous silica nanoparticles synthesized by sol-gel) the intrinsic density of the particles was increased by incorporation of gold in addition to the cargo18,19,20. Here we successfully employ a modified version of the pneumatic capillary gene gun5, which allows application of high He pressures, to launch non-modified PSi drug carriers into two- and three-dimensional (2D, 3D) targets. The parameters of the gene gun system are set to adjust the particle penetration depth, demonstrating the ability to reach targets deeper than previously reported7 and to cross a skin barrier.
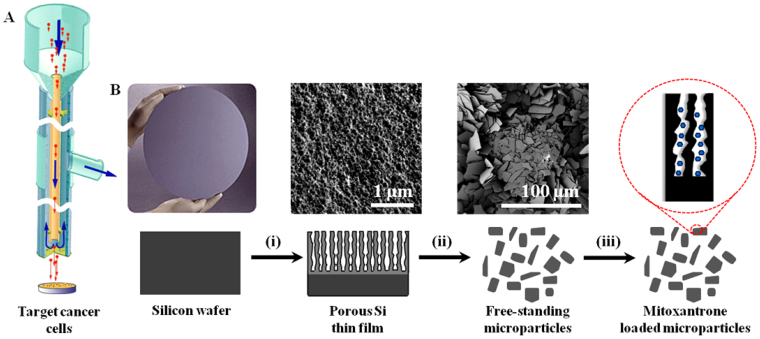
Figure 1.
(A) A schematic drawing of the biolistic set up system, modified from Shefi at el. 2006 [6]. (B) A representation of the preparation route of the PSi carriers: (i) Si substrate is subjected to electrochemical etching for 225 s at 15 mA/cm2, followed by (ii) lift-off of the porous layer from the bulk Si and ultrasonication, to produce particles ranging in size from 2 to 18 μm, and (iii) the anticancer drug, MTX, is loaded into the particles by physically adsorption.
The PSi particles are designed to carry and release Mitoxantrone dihydrochloride (MTX), an anthracenedione antitumor drug, which has shown a significant clinical effectiveness in the treatment of certain types of cancer, including metastatic breast cancer21,22. The MTX is loaded within the nanostructured PSi particles, which are fabricated by electrochemical etching of Si wafers, followed by ultrasonication (Figure 1-B). The drug release kinetics can be tuned by the PSi fabrication conditions, which determine the porosity and pores size, and the surface chemistry of the carriers23. The drug-loaded PSi carriers are delivered by the novel biolistic system into breast carcinoma cells (MDA-MB 231/GFP) in culture and into gels. The delivery of MTX-loaded PSi particles reveals significant cytotoxicity towards the target cells, while administration of empty particles (no drug) results in no effect on cell viability. Hence, demonstrating that cell death is solely induced by the released drug and not by the bombardment assay. Combination of biolistics with tunable PSi carriers presents a powerful non-conventional platform for the delivery of payloads in a highly controlled manner. This proof-of-concept study paves the way for designing new therapeutic strategies to allow both spatial and temporal control of payload release.
Results
Biolistic setup adjustment for PSi delivery
Porous Si is fabricated by electrochemical etching of single crystalline Si wafers in hydrofluoric acid (HF) electrolyte solutions (Figure 1-Bi). The selective dissolution of Si results in the formation of a porous nanostructure, where pore morphology and pore size can be tuned by controlling the anodization parameters (e.g., current density and electrolyte solution composition24,25). In this work, the etching conditions are adjusted to yield an approximately 2500 nm thick porous layer (porosity of 65% and surface area of ~450 m2/g) with a typical morphology of interconnecting cylindrical pores characterized by an average diameter of 30 ± 10 nm, as shown in the top-view high resolution scanning electron micrograph (Figure 1-Bi).
Following the electrochemical etching, the resulting freshly-etched porous films are lifted off from the bulk Si substrate, by applying an electropolishing current, after which the freestanding films are fractured into micron-size particles using an ultrasonic probe (amp. 55%, 30 min) (Figure 1-Bii). The resulting hydride terminated PSi particles are then loaded with the cargo by physical adsorption mechanism (Figure 1-Biii).
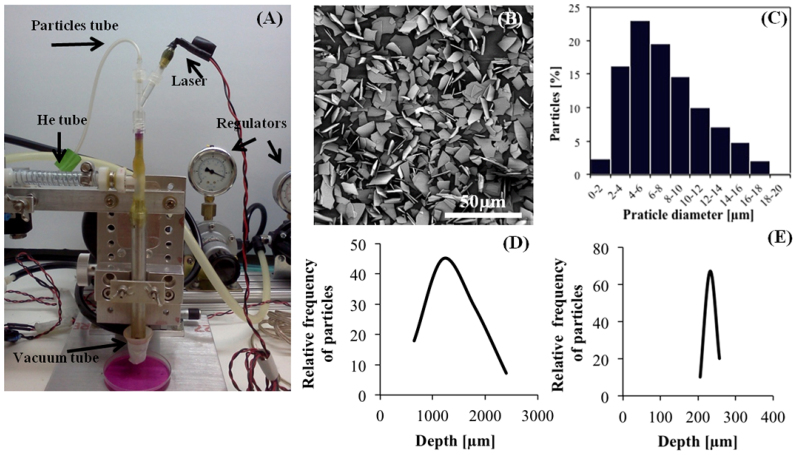
To adapt the gene gun for targeting 3D preparations and to adjust the ejection speed of the particles from the gun nozzle and their penetration depth, the PSi carriers are delivered into 2% agarose gel, emulating a soft tissue, using different sets of distances and pressures. In this process, the porous carriers are loaded directly into the ‘particle tube' of the gene gun (Figure 2-A) and accelerated by a minor He stream. Later on, this He stream merges with a major He stream that is accelerated through the ‘He tube'. We control the accelerating He pressures of both tubes using dedicated pressure regulators. The new gun set-up enables a wide range of He pressures, starting at 10/10 psi (particle tube pressure/He tube pressure) for targeting cells in culture, and up to 50/50 psi to achieve maximal penetration depths. The dosage is controlled by the loading method of the particles into the ‘particles tube' and the number of shots per load. In this study, one dose is referred as five biolistic shots following a single loading into the ‘particles tube' of the gun. We have calibrated and optimized the delivery parameters including the He pressure, distance and carriers dose for targeting cell cultures and 3D preparations. Prior to the bombardment, a laser beam, illuminating through the capillary tube, is used to define the targeted area (Figure 2-A). The PSi microparticles, ranging in size between 2-18 μm with 74 wt% of particles in the range of 2-10 μm (Figure 2-B and 2-C), are bombarded to a maximal penetration depth of ~2000 μm. A typical distribution of the penetration depths of the particles is depicted in Figure 2-D. Figure 2-E demonstrates the penetration depth distribution of uniform micron-size gold particles (1.6 μm) that are commonly practiced for biolistic delivery. The gold particles exhibit a narrower penetration depth distribution in comparison to the PSi particles, which are heterogeneous in structure and size. Surprisingly, the PSi particles have penetrated significantly deeper than the gold particles (2000 vs. 240 μm, respectively).
Figure 2.
(A) The biolistic setup. Particles are loaded into the ‘particles tube' (top left) in parallel to the laser inlet (top right) and are accelerated by controlled pressurized He. In the inner capillary tube the He stream with the particles merges with the gas flowing out the ‘He tube'. An active vacuum suction (bottom left) diverts the stream of He from the gun nozzle so only the particles are emerging out of the nozzle and target the sample. (B) HR-SEM micrographs of PSi microparticles. (C) Particle size distribution of PSi carriers, showing particles ranging in size from 2 to 18 μm. (D) A typical distribution curve of the number of PSi particles targeted to 2% agarose gel vs. the penetration depth (the number is normalized to total particles per shot), He pressures of 20/25 psi (particles/He tube)). (E) A typical distribution curve of the number of gold particles (1.6 μm) vs. penetration depth (similar bombardment conditions as in D).
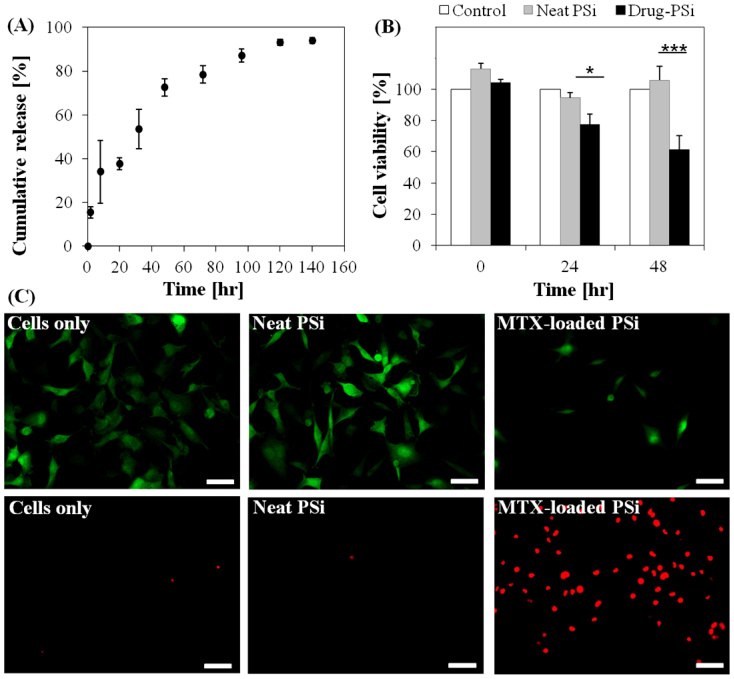
Biolistic delivery of PSi carriers to cancer cell models
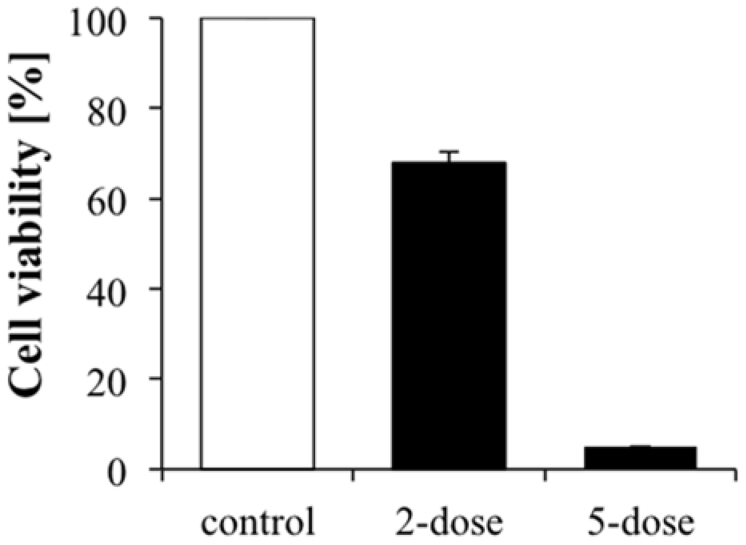
PSi particles were loaded with MTX as previously described23,26 showing an average loading of 31.4 ± 4.3 μg of MTX per mg of particles. The results of in-vitro drug release experiments, carried out in PBS (pH 7.4) while maintaining sink conditions, are presented in Figure 3-A. The PSi particles exhibit a sustained release of MTX over a period of 6 days, in which a minor burst release of 4% is observed within the first hour. A substantial release of 75% of the loaded drug is obtained within 48 h, after which a slower release rate is observed, lasting approximately 120 h. The cytotoxic effect of biolistically delivered MTX-loaded particles is studied using GFP-labeled breast carcinoma cells (MDA-MB-231/GFP). In order to rule out cell death caused by the delivery method (in comparison to the cytotoxic effect of the released anticancer drug), we study the viability of cells bombarded with empty (no drug) PSi microparticles as well. Cell viability experiments are performed at different time points of 0, 24, and 48 h after particle bombardment. PrestoBlue™ assay is used to quantify in-vitro cell viability. The results are summarized in Figure 3-B, revealing a profound drug-induced cell death. Immediately after the delivery (0 h), no statistically difference in cell viability is observed for all three preparations, demonstrating that the biolistic technique does not damage the targeted cells. The delivery of MTX-PSi carriers to the MDA-MB-231 cultures results in a decrease of 23 ± 6% in cell viability after 24 h. 48 h post-delivery, a significant cytotoxic effect is observed, with a decrease of 39 ± 9% in cell viability, compared to the control untreated cells. Notably, biolistic delivery of Neat-PSi particles demonstrates a consistent growth behavior similar to the control untreated cells. This result is also verified for additional cancer cell line cultures (neurobalstoma, SHSY-5Y), depicting no evident cell damage following administration of Neat-PSi particles (not shown). Furthermore, to rule out any cytotoxic effect due to the biolistic delivery assay we have characterized cell viability following a passive administration (no gun) of a similar dose of drug-loaded PSi. Indeed, we have confirmed that the cytotoxic effect on the MDA-MB-231 cell line is solely caused by the MTX drug released from the carriers. The fluorescence images of typical cultures of MDA-MB-231/GFP cells 24 h post the biolistic delivery assay, shown in Figure 3-C, reveal that the MTX released from the PSi carriers exhibit significant toxicity towards the cancer cells. In contrast, both control and Neat-PSi bombarded cultures display no evident effect on cell growth. To further confirm cell death, we have performed a Propidium Iodide (PI) staining of dead cells. The results of the PI staining show a significant number of dead cells following the MTX delivery whereas, only few dead cells are observed for the control cultures. The therapeutic efficacy of the biolistic delivery can be tailored and optimized by the number of bombardment cycles per culture. As can be seen in Figure 4, increasing the number of cycles, thus doses, significantly affects cell viability. Two-dose and five-dose bombardments lead to 32% and 95% cell death, respectively.
Figure 3.
(A) Cumulative percent of drug release from PSi particles into PBS (pH 7.4, 37°C) as a function of time. MTX release is expressed as percentage of the total MTX loaded. (B) Cell viability experiments over 48 h; the normalized percentage of cells, compared to control plates (white bars), following the biolistic delivery of neat PSi (gray bars) and drug-loaded PSi (black bars) immediately after delivery (0 h), and after 24 and 48 h. (n = 15). Data are the average percentage ± s.e.m of 4 independent experiments, *p < 0.01, one-tail t-test. (C) Upper panels: MDA-MB-231/GFP cells 24 h after treatment, GFP Ab labeling (green); (left) cells in a control, untreated culture, (middle) following delivery of neat PSi particles, and (right) after the delivery of MTX-loaded PSi particles. Lower panels: PI labeling indicating dead cells (red) in (left) a control untreated culture, (middle) following delivery of neat PSi particles, and (right) after the delivery of MTX-loaded PSi particles. Scale bar = 50 μm for upper panels, 100 μm for lower panels.
Figure 4. Different doses MTX–PSi carriers delivered into MDA-MB-231/GFP cell cultures.
A single dose is considered as five shots per loading. Between each dose the MTX–PSi carriers are reloaded. (n = 6).
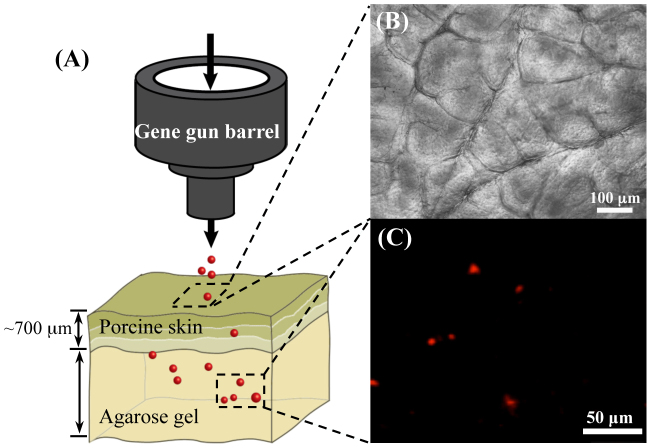
Delivery of PSi particles through a skin barrier
For further clinical applications it is important to demonstrate the feasibility of our biolistic methodology for non-invasive delivery of therapeutic cargos into tissues. Herein, we have designed an ex-vivo model system to mimic a skin barrier. We have bombarded fluorescently labeled PSi particles (see Supplementary Figure S1) through a freshly excised porcine skin into a 3D agarose gel. Porcine skin is used due to its structural and functional resemblance to human skin and its thickness differs greatly depending on the location27. The model includes the epidermis and dermis layers. The porcine skin (up to 700 μm thick) is placed on top of the gel, see Figures 5-A,B. The parameters of the bombardment process are adjusted to the 3D model system. We have applied high pressures of 40 psi in both He tubes to enable the delivery through the skin-barrier into deep layers. Obviously, the porcine skin barrier hinders particles penetration and results in a shift in the depth profile (in comparison to agarose gel), with a maximal penetration depth of ~1 mm.
Figure 5. Delivery of PSi particles into a 3D set-up: (A) A schematic diagram of a porcine skin placed atop 2% agarose gel.
PSi particles are delivered into the gel crossing the skin barrier. (B) The freshly excised porcine skin (3 × 3 cm2, 700 μm thick) is placed atop the agarose gel. (C) PSi particles labeled with Texas Red as detected in the gel using confocal microscopy, following biolistic delivery through the porcine skin. Particles/He pressures of 40/40 psi. Scale bar = 50 μm.
Discussion
In this study, a biolistic-mediated delivery method is developed to administrate an anti-cancer therapeutic into a breast cancer model. For the first time, nanostructured PSi carriers are successfully launched into two- and three-dimensional (2D, 3D) targets. PSi particles are characterized by high surface area, large free volume, biocompatible and biodegradable properties24,27,28. In recent years, these nanomaterials have emerged as a tunable platform for controlled delivery of therapeutic cargos such as small molecules, proteins and nanoparticles14,15,29,30,31,32,33,34. We have combined PSi carriers, designed to carry and release MTX, with a non-conventional biolistics technology for highly controlled anticancer therapeutics.
In attempt to extend the biolistic delivery methodology into a powerful therapeutic tool, we have used a novel gene gun setup5,6,7 to bombard the highly porous particles. We show that we can inject the PSi microparticles to penetrate deep into a 3D model by proper control over the bombardment conditions. The design of our gun allows the application of extremely high He pressures (used as the accelerating carrier medium) to launch the “airy” particles (65% porosity) with no spatial damage to the target. In the current setup, negative vacuum pressure (through the ‘vacuum tube', see Fig. 2A) is applied to divert the He flow from the target to prevent gas shock damages. It should be emphasized that bombardment of low-weight carriers is a major challenge. Previous studies by Martin-Ortigosa et al.18,19 have demonstrated an efficient biolistic-mediated delivery of porous silica particles into plants by increasing the density of the carries, using gold capping and plating techniques. Herein, we launched PSi microparticles (both empty and drug loaded) to depths of 2000 μm and through a skin barrier model. These bombardment conditions are also examined for the delivery of commercially available gold microparticles (commonly used in biolistic applications). In these experiments, the penetration depths are notably lower (240 μm) in comparison to the PSi penetration depth profile. However, it should be noted that these penetration values for the gold particles are superior to previous studies in which a maximum depth of 80 μm was achieved6.
Drug-loaded PSi particles, designed to exhibit a sustained release of MTX over several days, as shown in Figure 3-A, are launched into MDA-MB-231 cell cultures. Viability studies are carried out at different time points following the bombardment of the MTX-loaded PSi and Neat-PSi particles. At all studied time points, the viability of the cancer cells is not affected by the bombardment of the Neat-PSi particles. Thus, demonstrating that our biolistic administration methodology may potentially allow non-invasive injection of these porous carriers into diseased tissues. This result was also confirmed for a neurobalstoma cancer cell line. The targeted delivery of MTX-loaded PSi particles into cancer cells results in a profound cell death of about 40%, 48 h after the bombardment (Fig. 3-B,C). By administration of multiple doses, we have achieved a reduction of 95% in viable cancer cells, showing that we can control and optimize the efficacy of this biolistic-mediated therapeutic route.
We believe that the methodology presented in this work provides a new paradigm for an effective delivery of therapeutics into cancer cells. Moreover, the demonstration of an effective delivery of PSi carriers through the porcine skin model, may open a new therapeutic route for highly localized non-invasive treatment of skin carcinomas. The use of biolistics to administrate degradable PSi particles, which can practically be tailored to carry a variety of payloads with controlled release profiles, offers a generic approach for personalized nanomedicine.
Methods
Fabrication of porous Si carriers
Mesoporous Si films were fabricated form single-side polished p+ <100> silicon wafers (~1 mΩ-cm, B-doped, from Siltronix Corp, France) using an electrochemical etching process, in a 3:1 (v/v) solution of aqueous HF (48%, Merck, Germany) and ethanol (99.9%, Merck, Germany), at a constant current density of 15 mA/cm2 for 225 s. Si wafers with an exposed area of 6.16 cm2 were contacted on the backside with an aluminum foil and mounted in a Teflon etching cell; a platinum spiral coil was used as the counter-electrode. After etching, the surface of the wafer was rinsed with ethanol several times and dried under a dry nitrogen gas. The resulting porous films were removed from the bulk Si substrate by applying an electropolishing current density of 4 mA/cm2 for 3 min in an electrolyte solution of 3.3% HF in ethanol. The freestanding films were then placed in absolute ethanol and ultrasonically fractured, using an ultrasonic probe (Amp. 55%, 30 min, Vibracell 750 W, Sonics, USA), to produce particles ranging in size from 2 to 18 μm.
Note: All the materials were purchased from Sigma Aldrich Chemicals unless otherwise mentioned.
Texas red labeling of porous Si microparticles
Freshly-etched PSi microparticles were chemically modified using thermal hydrosilylation of undecylenic acid (≥95%), using microwave irradiation (Intelowave MS-204WS LG), to form undecanoic acid-terminated PSi (u-PSi). Briefly, 20 mg of microparticles were placed in an open Pyrex beaker containing 2 ml of undecylenic acid and were allowed to react for 6 min at 320 W. The resulting microparticles were thoroughly rinsed with acetone (Frutarom, Israel) and ethanol (99.9%, Merck) to remove unreacted species from the surface, and then dried under a stream of nitrogen gas.
For Texas red hydrazide (TRH) labeling, 2 mg of u-PSi microparticles were reacted for 2 h under orbital shaking with 150 μl of 0.052 M solution of N-(3-dimethylaminopropyl)-N2-ethylcarbodiimide hydrochloride (EDAC, ≥98.0%) and 200 μl of TRH solution (Invitrogen, USA), consisting of 0.3 mM TRH in N,N-Dimethyl formamide (DMF, Frutarom, Israel). Removal of unreacted TRH following labeling involved cycles of centrifugation (15,000 g for 5 min) and replacement of the supernatant with DMF and deionized water. This step was repeated several times till the red color of TRH had disappeared, after which the microparticles were dried under a stream of nitrogen gas.
Characterization of porous Si carriers
Physical and chemical characterization of PSi microparticles: (i) High-resolution scanning electron microscopy (HR-SEM) was performed using a Carl Zeiss Ultra Plus Field Emission SEM, at an accelerating voltage of 1 keV. (ii) Particle size and size distribution were determined using confocal laser scanning microscopy (LSM 700, Carl Zeiss, Germany) and image analysis software (Axio Vision Rel. 4.8 with auto measurements module). (iii) The specific surface area of the freshly-etched microparticles was determined by Nitrogen adsorption–desorption isotherms and the application of Brunauer–Emmett–Teller (BET) model (recorded at 77 K using a Micromeritics ASAP 2010 physisorption instrument, Norcross, GA). (iv) Surface modification and TRH labeling of the hydride terminated microparticles were characterized by attenuated total reflectance Fourier-transform infrared (ATR-FTIR) spectroscopy using a Thermo 6700 FTIR instrument equipped with a Smart iTR diamond ATR device.
Drug loading and release
MTX was physically adsorbed onto the freshly-etched (hydride terminated) PSi microparticles. MTX was dissolved in 200 μL of dimethyl sulfoxide (DMSO) to a final concentration of 9.66 × 10−3 M and 2 mg of PSi microparticles were soaked in the solution for 2 h, under orbital shaking. The microparticles were then separated from the solution, by centrifugation (15,000 g for 5 min), and rinsed with phosphate buffer solution (PBS) to remove excess drug, followed by drying under a stream of nitrogen gas.
Quantification of MTX loading within the PSi carriers was determined by completely dissolving the microparticles in an aqueous solution of 1 M sodium hydroxide (KOH), after which the absorbance of the solution was measured in the range 400–800 nm using a microplate reader (Varioskan Flash, Thermo Scientific, USA). The absorbance maximum at 596 nm was used to calculate the amount of the loaded MTX, based on a calibration curve.
In-vitro drug release studies were performed by incubating the MTX-loaded PSi particles in 2 ml of PBS. At designated time intervals aliquots were sampled and replaced with fresh PBS. MTX solutions were separated from microparticles by centrifugation, and the concentration of the released MTX in the sampled aliquots was determined by absorbance measurements at 612 nm (absorbance maximum), based on a calibration curve. MTX release is expressed as percentage of the total MTX loaded in the PSi carriers.
Cell culture
MDA-MB-231 human breast cancer cells were cultured in a humidified incubator at 37°C containing 5% CO2, and were routinely grown in 75 cm2 plastic tissue-culture flasks containing 10 ml of DMEM medium supplemented with 2 mM L-glutamine, 5% penicillin-streptomycin, 1% amphotericin and 10% heat-inactivated FBS. The medium was replaced every 2 days and the cells were split by adding 5 ml trypsin when reaching confluence of ~80%. A day before the biolistic assay the cells were split, counted and plated in 6 well cell-culture plates, 100,000 cells per well. Separate plates were prepared for each time point along the experiments (0 h, 16 h, 24 h, 48 h).
Biolistic assay
PSi particles were loaded into the setup ‘particles tube' using a mesh paper. The distance from the gun nozzle and the pressures in the ‘He tube' and ‘particle tube' were set to optimized values according to the target model and the required penetration depth. Vacuum was applied to the system, with a negative pressure of −25 psi. Prior the bombardment the medium was removed by a manual pipette and a laser beam was used to aim the targeted area within the well or gel model. For the delivery, a shot was generated by opening the valve for 0.3 s, causing the injection of a bolus of particles into the gun and out of the nozzle.
Cell viability assay
PrestoBlue™ reagent was used for quantitative measurements of cell death. The cell culture plates were treated biolistically, with drug-loaded and neat PSi particles at 0 h. Control plates were placed at the same atmosphere as the treated plates for the period of the experiment. At each time point (0 h, 16 h, 24 h, 48 h) cells were washed with PBS and PrestoBlue™ reagent was added (10%(v)) to the medium. After 105 min 150 μl aliquots were placed in the BioTek Synergy™ 4 Hybrid Microplate Reader, excited at 560 nm and collected at 590 nm.
Cell survival assay
Propidium Iodide (PI) was added to a final concentration of 5 μM per well. The wells were incubated for 15 min at 37°C. Fluorescent imaging was performed using an inverted fully motorized Nikon TE2000E fluorescence microscope.
Passive therapeutic delivery
A mesh paper containing MTX-loaded PSi particles (in an equivalent dose to biolistic assay) was placed in direct contact with cell culture wells. Cell viability assays were performed using the PrestoBlue™ reagent test at the different time points.
Immunocytochemistry
The MDA-MB-231/GFP cells were fixed with 4% paraformaldehyde for 15 min at room temperature, washed with Phosphate-Buffered Saline (PBS) and permeabilized with 0.5% Triton X-100 in PBS (PBT) for 10 min. Next, cells were incubated in a blocking solution (containing 1% Bovine Serum Albumin (BSA) and 2% Normal Goat Serum (NGS) in 0.2% PBT) for 45 min. Cells were incubated for 45 min at room temperature with a goat polyclonal anti GFP (Abcam Inc., Cambridge, MA, USA). Following the incubation, cultures were rinsed with PBS and mounted in an aqueous mounting medium. Confocal imaging was performed using Leica TCS SP5 with Acousto-Optical Beam Splitter (AOBS) microscope.
Author Contributions
A.T.B. synthesized and characterized the porous Si particles, labeled the particles, and conducted drug loading and release experiments. N.Z. carried out the biolistic assays, immunocytochemistry and confocal microscopy studies. N.Z. and A.T.B. conducted cell viability experiments. O.S. and E.S. have conceived the research, designed the study, analyzed data and wrote the manuscript with input from all authors.
Supplementary Material
Chemical characterization and Cell viability assay
Acknowledgments
This work was partially supported by the NEVET Grant administered by the Russell Berrie Nanotechnology Institute (RBNI) and the Bar-Ilan Institute of Nanotechnology & Advanced Materials (BINA). O.S. acknowledges the EU-FP7 People IRG Grants 239482. E.S. acknowledges the support of the Lorry I. Lokey Interdisciplinary Center for Life Sciences and Engineering. N.Z. gratefully acknowledges the BINA Scholarship for Outstanding Graduate Students. A.T.B. gratefully acknowledges the RBNI Scholarship for Outstanding Graduate Students. The authors thank Prof. Alex Groisman from the University of California, San Diego, for his support in the setting of the biolistic setups.
References
- Klein T. M., Wolf E. D., Wu R. & Sanford J. C. High-velocity microprojectiles for delivering nucleic acids into living cells. Nature 327, 70–73 (1987). [PubMed] [Google Scholar]
- Gan W. B., Grutzendler J., Wong W. T., Wong R. O. & Lichtman J. W. Multicolor ‘DiOlistic' labeling of the nervous system using lipophilic dye combinations. Neuron 27, 219–225 (2000). [DOI] [PubMed] [Google Scholar]
- O'Brien J. A. & Lummis S. C. Nano-biolistics: a method of biolistic transfection of cells and tissues using a gene gun with novel nanometer-sized projectiles. Bmc Biotechnol. 11, 66 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wellmann H., Kaltschmidt B. & Kaltschmidt C. Optimized protocol for biolistic transfection of brain slices and dissociated cultured neurons with a hand-held gene gun. J. Neurosci. Methods 92, 55–64 (1999). [DOI] [PubMed] [Google Scholar]
- Rinberg D., Simonnet C. & Groisman A. Pneumatic capillary gun for ballistic delivery of microparticles. Appl. Phys. Lett. 87, 014103–014103–3 (2005). [Google Scholar]
- Shefi O. et al. Microtargeted gene silencing and ectopic expression in live embryos using biolistic delivery with a pneumatic capillary gun. J. Neurosci. 26, 6119–6123 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shefi O., Simonnet C., Groisman A. & Macagno E. R. Localized RNAi and ectopic gene expression in the medicinal leech. J. Vis. Exp. Jove (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal E. et al. Confinement of thermoresponsive hydrogels in nanostructured porous silicon dioxide templates. Adv. Funct. Mater. 17, 1153–1162 (2007). [Google Scholar]
- Ferrari M. Cancer nanotechnology: opportunities and challenges. Nat. Rev. Cancer 5, 161–171 (2005). [DOI] [PubMed] [Google Scholar]
- Santos H. A. & Hirvonen J. Nanostructured porous silicon materials: potential candidates for improving drug delivery. Nanomed. 7, 1281–1284 (2012). [DOI] [PubMed] [Google Scholar]
- Wu E. C., Andrew J. S., Buyanin A., Kinsella J. M. & Sailor M. J. Suitability of porous silicon microparticles for the long-term delivery of redox-active therapeutics. Chem. Commun. Camb. Engl. 47, 5699–5701 (2011). [DOI] [PubMed] [Google Scholar]
- Anglin E. J., Schwartz M. P., Ng V. P., Perelman L. A. & Sailor M. J. Engineering the chemistry and nanostructure of porous silicon fabry-pérot films for loading and release of a steroid. Langmuir 20, 11264–11269 (2004). [DOI] [PubMed] [Google Scholar]
- Slowing I. I., Vivero-Escoto J. L., Wu C. W. & Lin V. S. Y. Mesoporous silica nanoparticles as controlled release drug delivery and gene transfection carriers. Adv Drug. Deliv. Rev. 60, 1278–1288 (2008). [DOI] [PubMed] [Google Scholar]
- Tasciotti E. et al. Mesoporous silicon particles as a multistage delivery system for imaging and therapeutic applications. Nat. Nanotechnol. 3, 151–157 (2008). [DOI] [PubMed] [Google Scholar]
- Wu E. C. et al. Oxidation-triggered release of fluorescent molecules or drugs from mesoporous Si microparticles. Acs Nano 2, 2401–2409 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu L., Park J. H., Duong K. H., Ruoslahti E. & Sailor M. J. Magnetic luminescent porous silicon microparticles for localized delivery of molecular drug payloads. Small 6, 2546–2552 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godin B. et al. Discoidal porous Silicon particles: fabrication and biodistribution in breast cancer bearing mice. Adv. Funct. Mater. 22, 4225–4235 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin-Ortigosa S., Valenstein J. S., Lin V. S. Y., Trewyn B. G. & Wang K. Functionalized mesoporous silica nanoparticle mediated protein and DNA codelivery to plant cells via the biolistic method. Adv. Funct. Mater. 22, 3576–3582 (2012). [Google Scholar]
- Martin-Ortigosa S. et al. Parameters affecting the efficient delivery of mesoporous silica nanoparticle materials and gold nanorods into plant tissues by the biolistic method. Small 8, 413–422 (2012). [DOI] [PubMed] [Google Scholar]
- Torney F., Trewyn B. G., Lin V. S. Y. & Wang K. Mesoporous silica nanoparticles deliver DNA and chemicals into plants. Nat. Nanotechnol. 2, 295–300 (2007). [DOI] [PubMed] [Google Scholar]
- Durr F. E., Wallace R. E. & Citarella R. V. Molecular and biochemical pharmacology of mitoxantrone. Cancer Treat. Rev. 10, 3–11 (1983). [DOI] [PubMed] [Google Scholar]
- Labiano A. et al. Slow release kinetics of mitoxantrone from ordered mesoporous carbon films. Microporous Mesoporous Mater. 160, 143–150 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzur-Balter A., Gilert A., Massad-Ivanir N. & Segal E. Engineering porous silicon nanostructure as tunable caririers for Mitoxantrone dihydrochloride. Acta Biomater. 9, 6208–6217 (2012). [DOI] [PubMed] [Google Scholar]
- Anglin E. J. et al. Porous silicon in drug delivery devices and materials. Adv. Drug Deliv. Rev. 60, 1266–1277 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link J. R. & Sailor M. J. Smart dust: Self-assembling, self-orienting photonic crystals of porous Si. Proc. Natl. Acad. Sci. 100, 10607–10610 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tzur-Balter A., Rubinski A. & Segal E. Designing porous silicon-based microparticles as carriers for controlled delivery of mitoxantrone dihydrochloride. J. Mater. Res. 28, 231–239 (2012). [Google Scholar]
- Branski L. K. et al. A porcine model of full-thickness burn, excision and skin autografting. Burns 34, 1119–1127 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J. H. et al. Biodegradable luminescent porous silicon nanoparticles for in vivo applications. Nat. Mater. 8, 331–336 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salonen J. et al. Mesoporous silicon microparticles for oral drug delivery: loading and release of five model drugs. J. Control. Release 108, 362–374 (2005). [DOI] [PubMed] [Google Scholar]
- Park J. S. et al. Cisplatin-loaded porous Si microparticles capped by electroless deposition of platinum. Small 7, 2061–2069 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilpeläinen M. et al. In vivo delivery of a peptide, ghrelin antagonist, with mesoporous silicon microparticles. J. Control. Release 137, 166–170 (2009). [DOI] [PubMed] [Google Scholar]
- Shen H. et al. Enhancing chemotherapy response with sustained EphA2 silencing using multistage vector delivery. Clin. Cancer Res. 19, 1806–1815 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos H. A. Drug delivery with nanostructured porous silicon nanoparticles. SPIE (2013). [Google Scholar]
- Secret E. et al. Antibody-functionalized porous silicon nanoparticles for vectorization of hydrophobic drugs. Adv. Healthc. Mater. 2, 718–727 (2013). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Chemical characterization and Cell viability assay