Abstract
OBJECTIVE:
There are several treatments for obstructive sleep apnea syndrome, such as weight loss, use of an oral appliance and continuous positive airway pressure, that can be used to reduce the signs and symptoms of obstructive sleep apnea syndrome. Few studies have evaluated the effectiveness of a physical training program compared with other treatments. The aim of this study was to assess the effects of physical exercise on subjective and objective sleep parameters, quality of life and mood in obstructive sleep apnea patients and to compare these effects with the effects of continuous positive airway pressure and oral appliance treatments.
METHODS:
Male patients with moderate to severe obstructive sleep apnea and body mass indices less than 30 kg/m2 were randomly assigned to three groups: continuous positive airway pressure (n = 9), oral appliance (n = 9) and physical exercise (n = 7). Polysomnographic recordings, blood samples and daytime sleepiness measurements were obtained prior to and after two months of physical exercise or treatment with continuous positive airway pressure or an oral appliance. Clinicaltrials.gov: NCT01289392
RESULTS:
After treatment with continuous positive airway pressure or an oral appliance, the patients presented with a significant reduction in the apnea-hypopnea index. We did not observe changes in the sleep parameters studied in the physical exercise group. However, this group presented reductions in the following parameters: T leukocytes, very-low-density lipoprotein and triglycerides. Two months of exercise training also had a positive impact on subjective daytime sleepiness.
CONCLUSIONS:
Our results suggest that isolated physical exercise training was able to modify only subjective daytime sleepiness and some blood measures. Continuous positive airway pressure and oral appliances modified the apnea-hypopnea index.
Keywords: Obstructive Sleep Apnea, CPAP, OA, Exercise Training, Subjective Daytime Sleepiness, Polysomnography
INTRODUCTION
Obstructive sleep apnea syndrome (OSAS) refers to a breathing sleep disorder characterized by recurrent, partial or complete episodes of upper airway obstruction (1).
The gold standard treatment most commonly used to treat OSAS is Continuous Positive Airway Pressure (CPAP). The main benefit of CPAP is a reduction of subjective excessive daytime sleepiness (2).
Oral appliances (OAs), another form of treatment, effectively reduce primary snoring and are recommended for mild to moderate OSAS patients and for those with severe OSAS who do not respond to or are unable to use CPAP (3,4).
Few studies have evaluated the effectiveness of a physical training program in reducing the symptoms of OSAS. In most patients, exercise is an adjunct to treatment through the loss of fat mass (5). Some studies have observed improvements in the apnea-hypopnea index, in the structure of sleep and in subjective measurements after a supervised exercise program (7-9). A recent study by our group demonstrated that aerobic exercise associated with CPAP had a positive impact on subjective daytime sleepiness, quality of life and mood but did not change the structure of sleep (10).
The literature is still controversial when assessing the inter-relationship between physical capacity and treatments for OSAS. The above data also highlight the need to assess the isolated effects of physical exercise, CPAP and OA use in OSAS patients.
MATERIALS AND METHODS
Sample
Patients with the clinical and polysomnographic criteria of OSAS were selected from the Sleep Disorders Ambulatory clinic (Disciplina de Medicina e Biologia do Sono - UNIFESP - EPM) (11). The patients were pre-selected according to the criteria described in Table 1.
Table 1.
Criteria for the pre-selection of patients.
| Inclusion Criteria | Exclusion Criteria |
| 25 to 55 years of age | Habits or occupations that lead to sleep deprivation or alterations in the sleep-wake cycle |
| Sedentary | History of regular sports activities |
| Body mass index≤30 kg/m2 | Inability to perform physical exercise |
| AHI>10/h | Other sleep disorders |
| Hemogram, cholesterol, HDL, triglycerides, fasting glucose, creatinine, TSH within the normal range | Anatomical obstructive upper airway: tonsils grade III and IV and septal deviation grade III (severe) that can affect the outcome of CPAP use |
| Lung function test (spirometry), chest X-rays (for smokers and former smokers), resting and stress electrocardiogram and otorhinolaryngologic examination without significant changes | Clinical disease decompensation (chronic obstructive pulmonary disease, asthma, interstitial lung diseases, neuromuscular diseases, heart failure, thyroid disease, rheumatologic and psychiatric diseases) |
| Use of sleeping pills | |
| Other treatments for OSAS | |
| Loss of dental support that subsequently compromises the retention of OA | |
| Periodontal disease | |
| Dental crown/tooth root relationship less than or equal to 1 | |
| Primary dental care (cavities, root canal treatment or retreatment or extensive dental prostheses) | |
| Anterior open bite | |
| Protrusive displacement less than 5 mm | |
| Limited mouth opening | |
| Alcoholism |
AHI: apnea-hypopnea index; HDL: high-density-lipoprotein; TSH: thyreoid stimulant hormone.
Patients were randomized into three groups: exercise (n = 7), CPAP (n = 9) and OA (n = 9). All patients completed two months of treatment with CPAP, OA or exercise training.
This study received appropriate ethical clearance (UNIFESP #0352/09) and was entered into the Clinical Trials database (NCT01289392).
Subjective assessment
Epworth Sleepiness Scale (ESS): This self-administered questionnaire was used to assess subjective daytime sleepiness in quotidian situations.
Fletcher & Lucket Questionnaire: This self-administered questionnaire was used to address 25 situations related to sleep habits and sleep complaints.
Short Form Health Survey (SF-36): This questionnaire was used to assess patient quality of life.
Profile of Mood States (POMS): This questionnaire was used to evaluate the mood states of the patients.
Polysomnography (PSG)
Full-night polysomnography was performed by previously trained professionals using a polysomnographic recorder (Somnologica, version 3.3.1; Reykjavík, Iceland). An electroencephalogram (EEG) (C3/A2, C4/A1, O1/A2, O2/A1), bilateral electrooculogram (EOG) and submentonian electromyogram (EMG) were used to assess the sleep stages. For respiration, the nasal flow was assessed using a nasal cannula with a pressure transducer, and a thermistor was used for oral and nasal respiration. Additionally, thoracic and abdominal movements were measured using non-calibrated inductance plethysmography, oxyhemoglobin saturation was measured using pulse oximetry, and snoring was measured with a tracheal microphone. Sleep position was determined using a position sensor. An electrocardiogram (ECG - V2 modified) was used to access heart rate variability. An anterior tibial electromyelogram (EMG) was also employed.
We obtained the following polysomnographic recordings of each patient: baseline and after treatment procedure (CPAP, OA or exercise training). Sleep stage scoring was performed using Rechtschaffen and Kales criteria (12). Respiratory events were analyzed according to the American Academy of Sleep Medicine (1), and arousals and periodic leg movements were scored as defined by the American Sleep Disorders Association (13,14).
Laboratory tests
We collected 30 ml of venous blood to determine the blood measurements.
CPAP treatment
The patients received a fixed mode device (REMstar® Plus; Respironics Inc., Murrysville, PA) that allowed for pressure variations between 4 and 20 cm H2O.
Dental appliance
A mandibular repositioning appliance (Brazilian Dental Appliance, São Paulo, SP, Brazil) was individually constructed and installed. The Brazilian Dental Appliance is an adjustable OA made of acrylic resin that allows progressive mandibular protrusion.
Exercise protocol
All patients in the exercise group were submitted to an aerobics/resistance training program. The exercises were conducted at the University wellness center.
The patients were supervised by an experienced professional over a 2-month period, three times per week, with a mean duration of 1 hour per session (5 p.m-6 p.m or 6 p.m-7 p.m).
Statistical analyses
The data were expressed as means±standard deviations. The analyses of the visually scored sleep variables, blood measurements and subjective scales in the two assessments were primarily performed using parametric testing and repeated-measures analysis of variance (ANOVA). The post-hoc Tukey's test was used to detect averages that were significantly different.
RESULTS
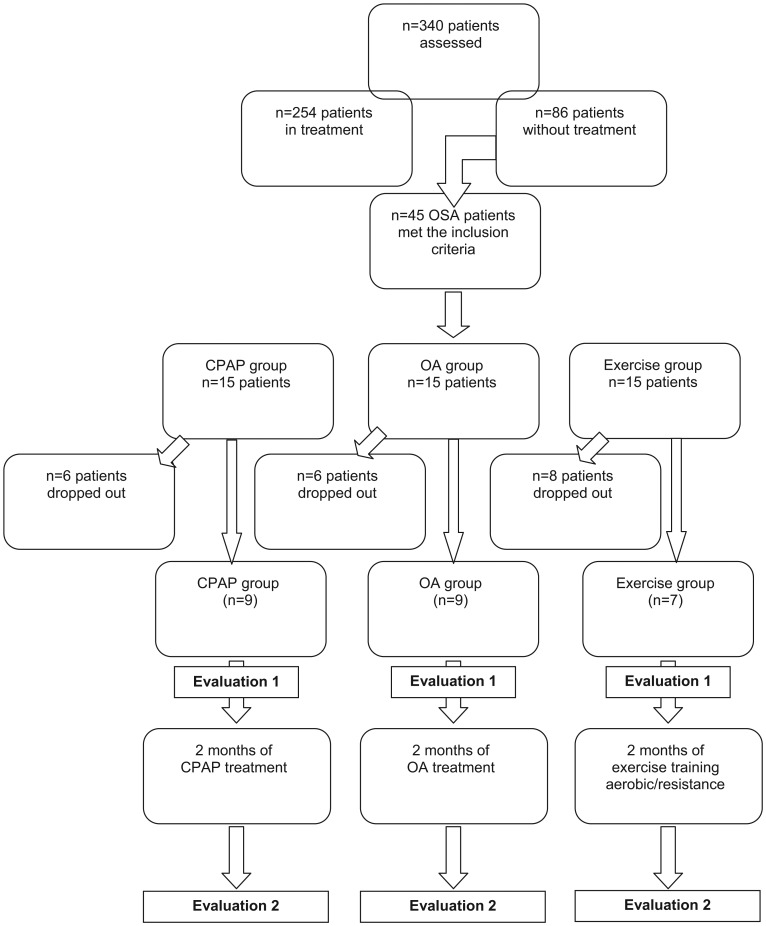
In total, 340 patients were assessed at the Sleep Disorders Ambulatory clinic; of these patients, 86 were not already undergoing treatment for sleep disorders. Forty-five patients were selected in accordance with the clinical and polysomnographic criteria of OSAS. Twenty-five male patients completed the study: nine in the CPAP group, nine in the OA group and seven in the exercise group (Figure 1. The main reasons for patient drop-out were professional problems (11 patients), inability to adapt to CPAP (six patients), health problems (two patients) and failure to comply with CPAP use (one patient). All patients in this study, including drop-out patients, had similar ages, body mass indices and neck circumferences, and these values were maintained throughout the observation period (Table 2.
Figure 1.
Experimental design.
Table 2.
Baseline and post-treatment patient characteristics.
| Drop-out Patients Baseline | CPAP Group Baseline | CPAP Group Post-treatment | OA Group Baseline | OA Group Post-treatment | Exercise Group Baseline | Exercise Group Post-treatment | p-value | |
| Age (years) | 40.45±8.32 | 38.62±8.15 | 38.62±8.15 | 42.33±6.20 | 42.33±6.20 | 42.28±8.28 | 42.28±8.28 | NS |
| BMI (kg/m2) | 27.13±1.91 | 25.90±5.31 | 27.23±4.91 | 29.26±1.73 | 29.86±2.61 | 28.14±1.63 | 29.02±2.34 | NS |
| Neck Circumference (cm) | 44.67±1.40 | 42.70±2.04 | 41.30±2.30 | 43.06±1.92 | 42.52±2.05 | 43.82±2.38 | 43.53±2.02 | NS |
The values are expressed as means±SD. NS – non-significant.
The apnea-hypopnea index decreased (F(2,20) = 6.41; p<0.01) in the CPAP and OA groups (p<0.001) after their respective treatments. No modifications were observed in the other polysomnography measurements evaluated (Table 3.
Table 3.
The effects of CPAP, the oral appliance and physical exercise on sleep parameters.
| CPAP Group | OA Group | Exercise Group Baseline Post-treatment | p value | ||||
| Baseline | Post-treatment | Baseline | Post-treatment | ||||
| Sleep Efficiency (%) | 78.5±16.5 | 89.5±5.8 | 78.5±8.5 | 84.2±8.8 | 79.9±9.0 | 83.7±11.0 | NS |
| Sleep Latency (min) | 18.7±27.8 | 8.7±7.9 | 21.7±20.5 | 14.6±20.6 | 12.7±10.5 | 11.4±17.5 | NS |
| REM Sleep Latency (min) | 111.9±67.2 | 112.1±78.7 | 139.1±75.3 | 127.9±90.8 | 116.8±93.2 | 110.5±57.1 | NS |
| Awake (min) | 63.8±61.6 | 37.1±24.4 | 82.1±37.2 | 55.0±22.2 | 68.7±22.6 | 55.1±46.0 | NS |
| Sleep Stage N1 (%) | 5.4±5.0 | 5.1±2.0 | 4.4±1.8 | 8.2±3.4 | 7.3±2.5 | 9.1±4.9 | NS |
| Sleep Stage N2 (%) | 54.3±11.6 | 50.0±6.6 | 66.6±13.6 | 56.7±8.7 | 52.3±8.3 | 56.9±7.3 | NS |
| Sleep Stage N3 (%) | 22.7±9.4 | 25.8±2.9 | 15.9±9.2 | 19.8±7.3 | 16.9±12.4 | 13.8±12.8 | NS |
| Sleep Stage NREM (%) | 17.3±6.9 | 17.9±4.3 | 13.2±6.2 | 15.3±5.4 | 17.7±5.4 | 16.0±3.9 | NS |
| Apnea-Hypopnea Index(AHI) | 25.1±10.5 | 1.9±1.2* | 30.8±19.0 | 9.6±10.3* | 22.8±12.8 | 18.7±10.5 | <0.01 |
| Arousal Index | 26.1±12.6 | 12.1±3.3 | 32.5±12.7 | 14.4±5.8 | 24.4±11.3 | 20.4±9.7 | NS |
Values are expressed as means±SD. *Significant difference from respective baseline records (p<0.001, ANOVA, Tukey's test).
In the blood analysis, we verified significant changes only in the physical exercise group. The ANOVA (F(2,20) = 4.63; p<0.05) revealed that the physical exercise patients had increased levels of glucose (p<0.05) and that this increase was maintained during the monitoring period (Table 4. Finally, in the exercise group, there were reductions in the following parameters: T leukocytes (p<0.05), very-low-density lipoprotein (VLDL) (p<0.05) and triglycerides (p<0.05; Table 4.
Table 4.
The effects of CPAP, the oral appliance and physical exercise on the blood sample parameters.
| CPAP Group | OA Group | Exercise Group | p-value | ||||
| Baseline | Post-treatment | Baseline | Post-treatment | Baseline | Post-treatment | ||
| Hemoglobin | 14.84±1.03 | 15.48±0.87 | 15.51±0.88 | 15.20±1.04 | 15.63±1.12 | 15.67±1.28 | NS |
| Hematocrit | 45.29±3.00 | 45.77±2.31 | 46.75±2.44 | 45.80±2.32 | 47.01±3.37 | 47.13±4.16 | NS |
| Platelets | 247.50±23.10 | 208.67±28.51 | 243.13±59.28 | 231.20±59.24 | 264.86±63.03 | 224.17±54.94 | NS |
| T Leukocytes | 7.11±3.03 | 6.65±2.24 | 6.13±2.28 | 6.12±1.16 | 7.55±1.60 | 5.34±0.64* | 0.05 |
| Glucose | 92.13±5.64 | 97.67±8.36 | 90.88±6.13 | 93.00±4.69 | 103.71±11.76#) | 100.83±13.26#) | 0.02 |
| Urea | 36.63±4.24 | 37.17±3.25 | 33.88±5.00 | 36.60±6.35 | 37.00±10.05 | 33.33±7.81 | NS |
| Creatinine | 0.95±0.11 | 1.01±0,15 | 1.10±0.13 | 1.11±0.19 | 1.07±0.07 | 1.01±0.10 | NS |
| Cholesterol | 192.75±31.13 | 184.33±11.08 | 203.00±22.32 | 198.60±24.18 | 205.71±49.03 | 199.67±39.16 | NS |
| HDL | 58.50±16.66 | 58.00±16.89 | 53.75±9.88 | 49.00±11.31 | 50.86±4.67 | 49.50±5.96 | NS |
| LDL | 109.13±24.20 | 106.67±16.82 | 125.00±18.69 | 118.80±27.49 | 123.61±39.01 | 125.00±30.12 | NS |
| VLDL | 25.13±7.14 | 19.67±5.89 | 24.25±12.28 | 29.80±16.75 | 31.14±12.94 | 25.17±10.82* | 0.01 |
| Triglycerides | 126.13±36.78 | 98.67±28.88 | 119.88±61.03 | 148.80±84.52 | 155.57±64.61 | 125.67±53.96* | 0.009 |
| Uric Acid | 5.66±1.28 | 6.45±1.96 | 5.79±0.92 | 6.16±1.08 | 6.37±0.95 | 6.52±1.09 | NS |
| Proteins | 7.10±0.47 | 6.80±0.09 | 7.19±0.29 | 6.86±0.29 | 7.39±0.43 | 6.88±0.28 | NS |
| Albumin | 4.81±0.14 | 4.68±0.29 | 4.69±0.15 | 4.64±0.23 | 4.83±0.24 | 4.53±0.23 | NS |
| Globulin | 2.29±0.40 | 2.12±0.26 | 2.50±0.26 | 2.22±0.29 | 2.56±0.49 | 2.35±0.30 | NS |
| Sodium | 140.88±0.99 | 141.67±1.97 | 141.00±2.07 | 140.80±1.64 | 140.14±1.68 | 142.17±1.47 | NS |
| Potassium | 4.19±0.39 | 4.35±0.35 | 4.15±0.26 | 3.82±0.11 | 4.19±0.34 | 4.43±0.25 | NS |
| TGO | 23.50±4.93 | 24.67±5.79 | 30.50±17.09 | 22.80±3.70 | 29.86±15.14 | 29.83±10.23 | NS |
| TGP | 27.75±10.69 | 30.17±9.95 | 37.50±27.01 | 31.60±7.70 | 34.43±18.54 | 35.67±12.77 | NS |
| Alkaline Phosphatase | 62.88±16.07 | 64.00±19.01 | 76.38±15.09 | 83.40±6.77 | 65.86±26.53 | 66.50±30.98 | NS |
| Ultra-sensitive PCR | 0.44±0.59 | 0.25±0.20 | 0.44±0.43 | 0.51±0.34 | 0.38±0.44 | 0.23±0.24 | NS |
Values are expressed as the mean±SD. *Significant difference from the respective baseline record (p<0.05).
Significant difference from the other baseline records (p<0.05, ANOVA, Tukey's test).
ANOVA (F(2,20) = 4.11; p<0.05) followed by Tukey's test indicated that a physical exercise program had a positive impact on subjective daytime sleepiness; the Epworth sleepiness scale was reduced from 14.14±5.64 to 9.57±4.24 (p<0.05) (Table 5.
Table 5.
The effects of CPAP, the oral appliance and physical exercise on subjective parameters.
| CPAP Group | OA Group | Exercise Group | p-value | ||||
| Baseline | Post-treatment | Baseline | Post-treatment | Baseline | Post- treatment | ||
| Epworth | 9.88±5.17 | 6.43±4.12 | 6.00±4.31 | 5.00±4.24 | 14.14±5.64# | 9.57±4.24* | 0.03 |
| POMS – Tension | 37.63±5.63 | 37.86±6.15 | 39.25±7.85 | 36.33±3.14 | 43.14±5.01 | 40.14±6.20 | NS |
| POMS – Depression | 44.63±8.14 | 46.43±11.50 | 45.38±8.31 | 44.50±6.77 | 46.43±4.28 | 45.43±7.32 | NS |
| POMS – Anger | 43.00±5.63 | 45.00±7.90 | 47.63±11.10 | 45.50±6.16 | 50.00±6.45 | 48.43±5.56 | NS |
| POMS – Fatigue | 44.38±5.26 | 45.00±8.16 | 44.63±7.13 | 52.83±5.71 | 43.86±7.13 | 42.71±7.54 | NS |
| POMS – Vigor | 45.38±5.32 | 45.29±5.65 | 45.13±7.16 | 46.50±8.12 | 48.29±6.37 | 46.43±5.91 | NS |
| POMS – Confusion | 34.75±3.49 | 34.14±5.05 | 34.00±5.15 | 34.00±5.69 | 34.86±5.11 | 34.43±3.55 | NS |
| SF36 – Physical functioning | 81.88±13.87 | 82.14±11.85 | 76.25±19.59 | 85.00±13.04 | 85.71±15.66 | 81.43±16.51 | NS |
| SF36 – Role limitations due to emotional health problems | 75.00±18.90 | 60.71±19.67 | 56.25±41.73 | 66.67±40.82 | 82.14±23.78 | 95.83±10.21 | NS |
| SF36 – Bodily pain | 66.50±17.85 | 69.71±13.89 | 64.50±20.23 | 83.83±17.89 | 66.43±25.81 | 70.29±27.20 | NS |
| SF36 – General health perceptions | 61.25±13.30 | 71.00±18.94 | 68.63±22.58 | 71.67±15.06 | 64.17±13.57 | 77.71±13.36 | NS |
| SF36 – Vitality | 54.38±15.91 | 59.29±26.37 | 45.00±29.15 | 53.33±22.06 | 47.86±23.43 | 55.00±21.60 | NS |
| SF36 – Social functioning | 70.31±23.09 | 64.29±22.16 | 71.88±24.78 | 72.92±16.61 | 78.57±20.04 | 73.21±20.95 | NS |
| SF36 – Role limitations due to emotional health problems | 66.67±35.63 | 52.38±32.53 | 58.33±34.50 | 72.22±44.31 | 95.24±12.60 | 72.22±32.77 | NS |
| SF36 – Mental health | 78.00±18.27 | 68.57±24.38 | 64.00±21.80 | 68.00±16.20 | 59.43±12.53 | 60.57±17.65 | NS |
Values are expressed as means±SD. *Significant difference from the respective baseline record (p<0.05).
Significant difference from the other baseline records (p<0.05, ANOVA, Tukey's test).
DISCUSSION
Our results suggest that physical exercise resulted in marked blood alterations and subjective daytime sleepiness modifications but yielded no changes in the sleep parameters. The patients treated with CPAP or OA experienced significant reductions in the apnea-hypopnea index.
CPAP is a highly effective and safe treatment for OSAS and is generally considered the current primary treatment for severe cases; the limiting factor is its acceptance and adherence (15). Alternative treatments that are safe, acceptable, effective and inexpensive are needed. There are several forms of treatment, such as OAs and physical exercise, that can be used to reduce the signs and symptoms of OSAS. Although CPAP is more efficacious in reducing sleep apnea, the OA has been demonstrated to be the preferred therapy when subjects used both treatments. OA therapy is considered a first-line choice of therapy for some patients with mild or moderate OSAS and an alternative form of treatment in those intolerant of CPAP use (16).
In this study, among the evaluated sleep parameters, only the apnea-hypopnea index exhibited significant changes. This index decreased to approximately 1.86 and 9.59 respiratory events after treatment with CPAP and OA, respectively. Therefore, these two methods of treatment reduced the obstructive events in OSAS; however, only CPAP was able to normalize the apnea-hypopnea index, in agreement with a previous study that concluded that both CPAP and the OA produced significantly greater improvements in sleep parameters than conservative measures, with CPAP being superior to the OA (16,17). A recent study comparing the use of CPAP and the OA in sleep apnea treatment indicated that the OA is similar to CPAP for patients with mild disease, whereas CPAP is superior for patients with moderate to severe disease (18).
Thus, the OA can be used as a treatment option for patients with moderate obstructive sleep apnea if the patients do not accept CPAP, corroborating previous findings (3),.
The patients that underwent the physical exercise protocol showed no changes in any of the evaluated sleep parameters, similar to results obtained in our previous study (10). Behavioral modifications as a treatment measure alone (17) or physical exercise may have clinical benefits in some individuals, but as a group, this treatment modality did not yield any significant changes in sleep-disordered breathing. One study revealed that physical exercise promoted a significant decrease in the respiratory disturbance index; however, the patients may have used CPAP in association with exercise (6). In other studies, the authors observed improvements in the apnea-hypopnea index, total sleep time, sleep efficiency and number of awakenings (7) or only in the respiratory disturbance index (8) after 6 months of a supervised exercise program associated with CPAP.
When we evaluated the blood samples obtained in the three groups studied, we noted significant changes only in the exercise group. The exercise group patients experienced reductions in the following parameters: T leukocytes, VLDL and triglycerides. During prolonged low-intensity exercise, there is an increased level of adrenaline in the blood, which increases the activity of lipase and promotes lipolysis. This increase in lipolysis enhances free fatty acids in the blood and muscle and promotes fat metabolism (22,23).
In the subjective parameters, only one significant change was observed in the exercise group: there was a reduction of excessive daytime sleepiness, which was verified by the Epworth sleepiness scale. Although we randomly distributed the patients into the three treatment arms, chance was responsible for the patients in the exercise group having higher ESS scores at baseline compared with the other groups. This difference may have created a bias in the interpretation because the variation in this group would be expected to be higher. We believe that with a larger number of patients, ESS scores could be higher at baseline in the CPAP and OA groups. Thus, reductions would have also occurred with these two treatments. Another study (8) showed that a supervised physical program improved the subjective daytime sleepiness in mild to moderate sleep apnea patients, although some of these patients appeared to use CPAP regularly. Some authors (24) did not observe reduced sleepiness after 3 months of breathing and aerobic exercise in OSAS subjects. In a recent study by our group (10), the authors concluded that CPAP and CPAP+exercise were effective in improving subjective sleepiness. CPAP has been shown to be effective in improving subjective sleepiness in subjects with severe sleep apnea (25) but not consistently in milder cases (26,27). Clinical trials have also demonstrated that OAs may improve excessive daytime somnolence (EDS), quality of life, cognition, mood (4) and systemic blood pressure (28).
Unfortunately, we could not recruit more patients, and reporting only a fraction of the predicted number of patients leads to inadequate power. This small sample size may explain the lack of statistical significance of some comparisons reported despite trends towards difference, which can promote a misleading interpretation of the results. The interim analysis of a randomized trial may lead to the necessity of increasing the total number of patients included.
In conclusion, isolated physical exercise training was able to modify only subjective daytime sleepiness and some blood measures. CPAP and the OA modified the apnea-hypopnea index.
Thus, the association of physical exercise with these two treatments should be evaluated because they may provide better subjective responses in patients and result in a higher quality of life than obstructive sleep apnea patients experience when treated with isolated therapies.
ACKNOWLEDGMENTS
This work was supported by AFIP, CEPE, CEMSA, CNPq and FAPESP (2009/01031-1 and CEPID #98/14303-3 to S.T.).
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. The Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22(5):667–89. [PubMed] [Google Scholar]
- 2.Kushida CA, Littner MR, Hirshkowitz M, Morgenthaler TI, Alessi CA, Bailey D, et al. Practice parameters for the use of continuous and bilevel positive airway pressure devices to treat adult patients with sleep-related breathing disorders. Sleep. 2006;29(3):375–80. doi: 10.1093/sleep/29.3.375. [DOI] [PubMed] [Google Scholar]
- 3.Kushida CA, Morgenthaler TI, Littner MR, Alessi CA, Bailey D, Coleman J, Jr, et al. Practice parameters for the treatment of snoring and obstructive sleep apnea with oral appliances: an update for 2005. Sleep. 2006;29(2):240–43. doi: 10.1093/sleep/29.2.240. [DOI] [PubMed] [Google Scholar]
- 4.Naismith SL, Winter VR, Hickie IB, Cistulli PA. Effect of oral appliance therapy on neurobehavioral functioning in obstructive sleep apnea: a randomized controlled trial. J Clin Sleep Med. 2005;1(4):374–80. [PubMed] [Google Scholar]
- 5.Shneerson J, Wright J. Lifestyle modification for obstructive sleep apnea.Cochrane Database Syst Rev. 2001;(1):CD002875. doi: 10.1002/14651858.CD002875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Netzer N, Lormes W, Giebelhaus V, Halle M, Keul J, Mattys H, et al. Physical training of patients with sleep apnea. Pneumologie. 1997;51 Suppl 3:779–82. [PubMed] [Google Scholar]
- 7.Giebelhaus V, Strohl KP, Lormes W, Lehmann M, Netzer N. Physical exercise as an adjunct therapy in sleep apnea – an open trial. Sleep Breath. 2000;4(4):173–6. doi: 10.1007/s11325-000-0173-z. [DOI] [PubMed] [Google Scholar]
- 8.Norman JF, Von Essen SG, Fuchs RH, McElligott M. Exercise training effect on obstructive sleep apnea syndrome. Sleep Res Online. 2000;3(3):121–9. [PubMed] [Google Scholar]
- 9.Sengul YS, Ozalevli S, Oztura I, Itil O, Baklan B.The effect of exercise on obstructive sleep apnea: a randomized, controlled trial. Sleep Breath. 2011;15(1):49–56. doi: 10.1007/s11325-009-0311-1. [DOI] [PubMed] [Google Scholar]
- 10.Ackel-D'Elia C, Silva AC, Santos-Silva R, Truksinas E, Sousa BS, Tufik S, et al. Effects of exercise training associated with continuous positive airway pressure treatment in patients with obstructive sleep apnea syndrome. Sleep Breath. 2012;16(3):723–35. doi: 10.1007/s11325-011-0567-0. [DOI] [PubMed] [Google Scholar]
- 11.American Academy of Sleep Medicine. 2005: Diagnostic and coding manual. Westchester, Illinois: American Academy of Sleep Medicine; ICSD-2- International Classification of sleep disorders, 2nd ed. [Google Scholar]
- 12.Rechtschaffen A, Kales A. Los Angeles: Brain Information/Brain Research Institute UCLA; 1968. A manual of standardized terminology, tecniques and scoring system of sleep stages of humans subjects. [Google Scholar]
- 13.EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep. 1992;15(2):174–84. [PubMed] [Google Scholar]
- 14.Recording and scoring leg movements. The Atlas Task Force. Sleep. 1993;16(8):748–59. [PubMed] [Google Scholar]
- 15.Weaver TE. Adherence to positive airway pressure therapy. Curr Opin Pulm Med. 2006;12(6):409–13. doi: 10.1097/01.mcp.0000245715.97256.32. [DOI] [PubMed] [Google Scholar]
- 16.Ferguson KA, Ono T, Lowe AA, Keenan SP, Fleethan JA. A randomized crossover study of an oral appliance vs nasal-continuous positive airway pressure in the treatment of mild-moderate obstructive sleep apnea. Chest. 1996;109(5):1269–75. doi: 10.1378/chest.109.5.1269. [DOI] [PubMed] [Google Scholar]
- 17.Lam B, Sam K, Mok WYW, Cheung MT, Fong DYT, Lam JCM, et al. Randomised study of three non-surgical treatments in mild to moderate obstructive sleep apnoea. Thorax. 2007;62(4):354–9. doi: 10.1136/thx.2006.063644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holley AB, Lettieri CJ, Shah AA. Efficacy of an adjustable oral appliance and comparison with continuous positive airway pressure for the treatment of obstructive sleep apnea syndrome. Chest. 2011;140(6):1511–6. doi: 10.1378/chest.10-2851. [DOI] [PubMed] [Google Scholar]
- 19.Ferguson KA, Cartwrigt R, Rogers R, Schimidt-Nowara W. Oral appliance for snoring and obstructive sleep apnea: A Review. Sleep. 2006;29(2):244–62. doi: 10.1093/sleep/29.2.244. [DOI] [PubMed] [Google Scholar]
- 20.Cistulli PA, Gotsopoulos H, Marklund M, Lowe AA. Treatment of snoring and obstructive sleep apnea with mandibular repositioning appliances. Sleep Med Rev. 2004;8(6):443–57. doi: 10.1016/j.smrv.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 21.Lim J, Lasserson YJ, Feetham J, Wrigth J. Oral Appliances for Obstructive Sleep Apnoea. Cochrane Database Syst Rev. 2006;(1):CD004435. doi: 10.1002/14651858.CD004435.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ball-Burnett M, Green H, Houston M. Energy metabolism in human slow and fast twich fibers during prolonged cycle exercise. J Physiol. 1991;437:257–67. doi: 10.1113/jphysiol.1991.sp018594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ladu M, Kapsas H, Palmer W. Regulation of lipoprotein lipase in muscle and adipose tissue during exercise. J Applied Physiol. 1991;71(2):404–09. doi: 10.1152/jappl.1991.71.2.404. [DOI] [PubMed] [Google Scholar]
- 24.Sengul YS, Ozalevli S, Oztura I, Itil O, Baklan B. The effect of exercise on obstructive sleep apnea: a randomized and controlled trial. Sleep Breath. 2009;15(1):49–56. doi: 10.1007/s11325-009-0311-1. [DOI] [PubMed] [Google Scholar]
- 25.Montserrat JM, Ferrer M, Hernandez L, Farré R, Vilaqut G, Navajas D, et al. Effectiveness of CPAP treatment in daytime function in sleep apnea syndrome: a randomized controlled study with an optimized placebo. Am J Resp Crit Care Med. 2001;164(4):608–13. doi: 10.1164/ajrccm.164.4.2006034. [DOI] [PubMed] [Google Scholar]
- 26.Barnes M, Houston D, Worsnop CJ, Neil AM, Mykytyn IJ, Kay A, et al. A randomized controlled trial of continuous positive airway pressure in mild obstructive sleep apnea. Am J Respir Crit Care Med. 2002;165(6):773–80. doi: 10.1164/ajrccm.165.6.2003166. [DOI] [PubMed] [Google Scholar]
- 27.Gotsopoulus H, Chen C, Quian J, Cistulli PA. Oral appliance therapy improves symptoms in obstructive sleep apnea: a randomized controlled trial. Am J Resp Crit Care Med. 2002;166(5):743–8. doi: 10.1164/rccm.200203-208OC. [DOI] [PubMed] [Google Scholar]
- 28.Barnes M, McEvoy RD, Banks S, Tarquinio N, Murray CG, Vowles N, et al. Efficacy of positive airway pressure and oral appliance in mild to moderate obstructive sleep apnea. Am J Respir Crit Care Med. 2004;170(6):656–64. doi: 10.1164/rccm.200311-1571OC. [DOI] [PubMed] [Google Scholar]