Abstract
Background
We sought to determine whether perceived patient-centered medical home (PCMH) characteristics are associated with staff morale, job satisfaction, and burnout in safety net clinics.
Methods
Self-administered survey among 391 providers and 382 clinical staff across 65 safety net clinics in 5 states in 2010. The following 5 subscales measured respondents’ perceptions of PCMH characteristics on a scale of 0 to 100 (0 indicates worst and 100 indicates best): access to care and communication with patients, communication with other providers, tracking data, care management, and quality improvement. The PCMH sub-scale scores were averaged to create a total PCMH score.
Results
Six hundred three persons (78.0%) responded. In multivariate generalized estimating equation models, a 10% increase in the quality improvement subscale score was associated with higher morale (provider odds ratio [OR], 2.64; 95% CI, 1.47–4.75; staff OR, 3.62; 95% CI, 1.84–7.09), greater job satisfaction (provider OR, 2.45; 95% CI, 1.42–4.23; staff OR, 2.55; 95% CI 1.42–4.57), and freedom from burnout (staff OR, 2.32; 95% CI, 1.31–4.12). The total PCMH score was associated with higher staff morale (OR, 2.63; 95% CI, 1.47–4.71) and with lower provider freedom from burnout (OR, 0.48; 95% CI, 0.30–0.77). A separate work environment covariate correlated highly with the quality improvement subscale score and the total PCMH score, and PCMH characteristics had attenuated associations with morale and job satisfaction when included in models.
Conclusions
Providers and staff who perceived more PCMH characteristics in their clinics were more likely to have higher morale, but the providers had less freedom from burnout. Among the PCMH subscales, the quality improvement subscale score particularly correlated with higher morale, greater job satisfaction, and freedom from burnout.
Policy makers, health care organizations, and patient advocates have tended to focus on whether the patient-centered medical home (PCMH) improves patient outcomes. However, a critical question is how the PCMH influences provider and clinical staff morale, satisfaction, and burnout (MSB). Core components of the PCMH include comprehensive primary care, quality improvement, care management, and enhanced access.1,2 For many practices, the model may increase workload and significantly change staff roles. Therefore, providers and staff may be strained by the transformation that occurs with implementation of the PCMH.3 On the other hand, providers and staff might benefit from a more efficient and satisfying work environment.
The effect of the PCMH on providers and staff in safety net clinics is especially important because personnel turnover has been high and the work environment can be difficult.4 Resources are frequently constrained, physician and nursing shortages cause understaffing, patients often have significant social and economic challenges, and access to specialists is limited.5 Within this context, the Centers for Medicare & Medicaid Services have recently undertaken the Federally Qualified Health Center Advanced Primary Care Practice Demonstration,6 a project evaluating the effectiveness, accessibility, quality, and cost of patient-centered care in up to 500 federally qualified health centers (HCs). The PCMH may be important for HCs to provide quality care in this complex evolving environment,1 but success and sustainability are dependent on provider and staff buy-in to the model.3
The literature describes general determinants of MSB among health care providers and staff. Work environment is crucial.7,8 Among physicians, correlates of MSB include control over one’s own work, positive workplace relationships, differences between experienced and expected workload, and satisfaction with income.9 Among nurses, correlates of MSB include autonomy, job stress, and nurse-physician collaboration.10 In HCs, sources of increased stress are insufficient resources, high workload, and time pressure. Stress increases the likelihood that staff leave an organization within 3 years.4
Specific domains of the PCMH may influence MSB. Physicians whose practices engaged in quality improvement efforts noted significantly less isolation, stress, and dissatisfaction with their work.11 In the quality improvement initiative of the Health Disparities Collaboratives12 program by the Health Resources and Services Administration, 40% of HCs reported improved staff morale as a result of the initiative, but 20% noted worsened staff morale. Participants stated that personal recognition, career promotion, and skill development opportunities would improve morale and lower burnout. Various care management and open access interventions improve job satisfaction,13–15 while difficulty in coordinating care with other providers negatively correlates with job satisfaction.16
We are aware of only one peer-reviewed study that has directly examined the effect of PCMH implementation on provider outcomes; none to date have examined staff outcomes. The PCMH intervention at a Group Health Cooperative of Puget Sound (Seattle, Washington) clinic reduced provider emotional exhaustion and depersonalization scores by half.17 However, this study has limited generalizability, especially to safety net clinics serving vulnerable populations. Therefore, we sought to determine whether PCMH characteristics were associated with staff morale, job satisfaction, and burnout across 65 safety net clinics.
METHODS
We conducted a mailed self-administered survey among providers and clinical staff practicing at 65 safety net clinics during the first year of the 5-year Safety Net Medical Home Initiative supported by The Commonwealth Fund. At the time of the study, Qualis Health and the MacColl Institute for Health-care Innovation18 were working with providers and staff in the clinics to implement the PCMH using a framework of 8 change concepts. Implementation of the first 2 change concepts began during the survey period; these included (1) empanelment of patients to providers and (2) continuous and team-based healing relationships linking patients to a provider and care team.
SURVEY
Surveys were mailed to 391 providers and 382 clinical staff across 65 participating safety net clinics. Providers were defined as physicians, physician assistants, and nurse practitioners. Clinical staff were defined as behavioral health specialists, educators, certified medical assistants, counselors, dieticians, medical assistants, nurses (licensed practical nurse or registered nurse), psychiatrists, psychologists, or social workers. The Safety Net Medical Home Initiative clustered clinics into 5 regional coordinating centers (RCCs) in Colorado, Idaho, Massachusetts, Oregon, and Pennsylvania (clustered around Pittsburgh). The RCCs helped coordinate the training of the HCs in that region. The 5 RCCs were chosen from 42 candidate RCCs based on selection criteria that included size, geographic setting, leadership support, prior PCMH efforts, prior quality improvement activities, adequate staffing, and support from state Medicaid agencies and other stakeholders.
In 2010, we mailed surveys to providers and staff. Based on power calculations assuming a 70% response rate, we set a target of 15 responses from each clinic, with a split of 9 providers and 6 staff. For clinics with more than 15 providers and staff, we randomly surveyed 9 providers and 6 staff at each clinic; for clinics with fewer than 15 providers and staff, all providers and staff were surveyed. If a clinic had fewer than 9 providers, we included more staff until we had surveyed 15 respondents at that clinic. A one-time incentive of $10 was included with each initial mailing. After the initial surveys were mailed, 2 more waves of the surveys were mailed to nonresponders.
PCMH CHARACTERISTICS
Based on the 2008 National Committee for Quality Assurance PCMH standards,19 we created the following 5 PCMH sub-scales: access to care and communication with patients, communication with other providers, tracking data, care management, and quality improvement. We created a total PCMH score, which was the mean of 4 of 5 PCMH subscale scores (the surveys and scoring algorithms are available http://www.commonwealthfund.org/Content/Innovations/Tools/2011/Staff-Morale-in-Safety-Net-Clinics.aspx). Questions in the communication with other providers subscale asked respondents how often they experienced difficulty in communicating with outside specialists, hospital-based providers, and emergency departments. We believed that these questions would not be relevant to staff, so they were excluded from the staff survey and the total PCMH score calculation. Some questions were taken or adapted from health care provider surveys7,20 and from PCMH evaluation surveys20,21 (M. W. Friedberg, MD, MPP, written communication, September 9, 2010), and some questions were created by us. Questions were selected for subscales based on content validity. Each question was rescaled from a 5-point Likert-type scale to a score range of 0 to 100 (0 indicates worst and 100 indicates best, with 1 on the Likert-type scale representing 0 points, 2 representing 25 points, 3 representing 50 points, 4 representing 75 points, and 5 representing 100 points). These rescaled scores were then averaged within their respective subscale. Finally, the total PCMH score was calculated as the mean of 4 of 5 PCMH subscale scores (excluding communication with other providers), yielding a total PCMH score with a potential range of 0 to 100. Cronbach α for the 5 subscales ranged from .48 (5-item access to care and communication with patients subscale) to .82 (7-item care management subscale), with an overall α=.87 for the 22-item total PCMH score.
COVARIATES
We constructed the following control variables based on factors known to be associated with MSB in prior literature: the presence of an electronic medical record (EMR),22 work environment,7–9 whether the clinic reported provider or nursing shortages,12 and years since the end of clinical training.9 We used a binary variable for the presence or absence of an EMR. The work environment covariate subscale consists of 5 questions that examine the culture, teamwork, and leadership of the practice. Similar to the PCMH subscales, each question was rescaled from a 5-point Likert-type scale to a score range of 0 to 100, and the overall work environment score was the mean of the scores on these 5 questions. We tested for correlation of the PCMH subscales with the work environment covariate sub-scale using Pearson product moment correlation coefficient to check for possible collinearity. The provider and nursing shortage questions came from a previous baseline organizational survey.23 The order of responses in some questions was reversed to create consistent scaling (worst to best). All covariates except years since the end of clinical training were used as clinic-level variables. That is, for each clinic we took the mean of each continuous covariate and took the majority response for the binary covariates (presence of an EMR), so that all respondents within each clinic had the same value for those covariates. However, years since the end of clinical training was used as an individual-level variable.
OUTCOME VARIABLES
Three survey questions on MSB served as the 3 outcome variables for the study. Respondents were asked to “Rate staff morale in your clinic” on a 5-point Likert-type scale that ranged from “poor” to “excellent.” Job satisfaction was measured by survey participants’ response to the statement “Overall, I am satisfied with my current job,” with responses on a 5-point Likert-type scale that ranged from “strongly disagree” to “strongly agree” (M. W. Friedberg, MD, MPP, written communication, September 9, 2010). Burnout was measured using a validated question in which respondents were prompted with the statement “Using your own definition of ‘burnout,’ please check one” and were given 5 options along an ordinal response scale that ranged from “I enjoy my work. I have no symptoms of burn-out,” to “I feel completely burned out and often wonder if I can go on.”24 We used pairwise correlation to examine the relationships among MSB. All 3 outcome variables were measured at the individual level and were converted to binary values for logistic regression analysis, with cut points based on face validity and the distribution of responses.
STATISTICAL ANALYSIS
We generated descriptive statistics for providers, staff, and clinic characteristics. To investigate the relationship between the binary outcome variables (MSB) and PCMH subscale scores, while allowing for a clustering effect, we fitted univariate and multivariate generalized estimating equation models. In particular, we ran general linear models with logistic link and exchangeable correlation structure to allow clustering effect within each clinic. For univariate analyses, the clinic-level mean (taking the mean of individual-level values for each clinic) for the 5 PCMH subscale scores and the total PCMH score were used as the independent variable in a univariate model for each individual’s MSB (18 univariate models in total). For multivariate analyses, the PCMH subscale scores for access to care and communication with patients, tracking data, care management, and quality improvement were included with the control variables representing the presence of an EMR, provider shortage, nursing shortage, and years since the end of clinical training. We also ran a second set of multivariate models that included only the total PCMH score with all of the covariates. For both univariate and multivariate models, we included interaction terms between the respondent’s position type (provider vs staff) and the PCMH subscale and total PCMH scores to allow differential influence of these covariates for different position types.25,26 Because work environment is conceptually important but highly correlated with several PCMH subscales and with the total PCMH score, we performed multivariate analyses with and without work environment in the models.
We reported the results of univariate and multivariate analyses using odds ratios (95% CIs) that reflected either a 10-point or 10% increase in variables coded on a scale of 0 to 100 or a change from 0 (not present) to 1 (present) for binary-coded variables. All analyses were performed using commercially available software (STATA version 11; StataCorp LP, College Station, Texas).
RESULTS
CHARACTERISTICS OF PROVIDERS, STAFF, AND CLINICS
We received 603 completed surveys (78.0%) from 773 sampled providers and staff, with a 79.8% response rate for providers and a 76.2% response rate for staff. Non-responders (n=170) differed significantly from responders by region and by location (P=.002 for both). For example, nonrespondents were disproportionately from Massachusetts (40.5% for nonresponders vs 25.5% for responders, P <.001) and from city-based clinic locations (61.3% for nonresponders vs 50.1% for responders, P=.01) as opposed to suburban or rural locations. We received a similar number of responses from providers (n=312) and from staff (n=291). Most respondents were female and of non-Hispanic white race/ethnicity, and approximately half of the clinics were located in a city (Table 1).
Table 1.
Characteristics of Providers, Staff, and Clinics
| Variable | Value |
|---|---|
| Respondents (n = 603) | |
| Female sex, % | 78.3 |
| Race/ethnicity, %a | |
| White | 71.8 |
| Hispanic or Latino | 15.1 |
| Black | 5.1 |
| Asian | 3.3 |
| Otherb | 4.0 |
| Not reported | 0.7 |
| Provider or staff type, % | |
| Physician | 33.5 |
| Nurse practitioner or physician assistant | 19.1 |
| Registered nurse | 13.3 |
| Licensed practical nurse or medical assistant | 22.7 |
| Otherc | 11.4 |
| Years since the end of clinical training, mean (SD) | 13.1 (11.0) |
| Years working at this clinic, mean (SD) | 6.1 (6.1) |
| Hours per week working at this clinic, mean (SD) | 34.2 (11.6) |
| Primary patient population, % | |
| Children <18 y | 6.0 |
| Adults ≥18 y | 23.6 |
| Children and adults | 70.4 |
| Presence of an EMR, % | 74.7 |
|
| |
| Clinics (n = 65) | |
| Location, % | |
| City | 50.8 |
| Suburban | 7.7 |
| Small town | 15.4 |
| Rural | 18.5 |
| Frontier | 7.7 |
| No. of providers, mean (SD) | 9.6 (20.1) |
| Provider shortage, % | 50.8 |
| Nursing shortage, % | 26.2 |
|
| |
| Clinic Patients, Mean (SD), % | |
| Insuranced | |
| Medicaid | 37.4 (19.3) |
| Medicare | 13.5 (10.8) |
| Private | 19.2 (13.8) |
| Uninsured | 28.6 (19.4) |
| Other public insurance | 1.5 (3.5) |
| Hispanic or Latino ethnicitye,f | 54.2 (18.9) |
| Racee | |
| White | 57.2 (25.4) |
| African American | 7.5 (10.8) |
| Otherg | 3.7 (4.0) |
| >1 Race | 4.4 (16.6) |
| Not reported or refused | 27.2 (19.0) |
| Limited English proficiencye | 32.0 (26.7) |
Abbreviation: EMR, electronic medical record.
Ethnicity and race questions from the provider and staff surveys were combined. Any individual self-identifying his or her race or ethnicity as Hispanic or Latino was included in that grouping. All other listed categories (eg, white, black, and Asian) are exclusively non-Hispanic.
Includes American Indian, Alaska Native, Native Hawaiian, and Pacific Islander.
Includes behavioral health specialists, educators, counselors, dieticians, psychiatrists, psychologists, and social workers.
Patient insurance data were obtained from Qualis Health and include 64 of 65 clinics (98.5%). For some clinics where site-level data were unavailable, patient insurance mix was imputed from data on the larger system or health center.
Ethnicity, race, and limited English proficiency characteristics were obtained from Uniform Data System reports. Federally qualified health centers are required to report their patients’ ethnic, racial and insurance demographics in the form of Uniform Data System reports to the Health Resources and Services Administration. We were able to obtain Uniform Data System information for 44 of 65 clinics (67.7%). The remaining clinics were not federally qualified health centers at the time of the survey.
Hispanic or Latino ethnicity is reported independent of race and overlaps with the race categories to an unknown extent owing to the aggregated totals provided by the Uniform Data System.
Includes American Indian, Hawaiian, Pacific Islander, and Asian.
MORALE, JOB SATISFACTION, AND BURNOUT
Morale showed a normal distribution, with the largest group of respondents (32.8%) rating morale in their clinics as good (Table 2). Job satisfaction and burnout were strongly skewed toward positive responses; the largest groupings of respondents were found in the second-highest categories, with 53.7% rating job satisfaction as very good and 49.5% noting that “Occasionally I am under stress at work, but I don’t feel burned out.” Morale, job satisfaction, and burnout moderately correlated with each other (r=0.48 for morale and job satisfaction, r=0.32 for morale and burnout, and r=0.44 for job satisfaction and burnout) (P<.001 for all).
Table 2.
Distribution of Provider and Staff Morale, Job Satisfaction, and Burnout
| Provider and Staff Rating | % of Respondents |
|---|---|
| Morale (n = 603) | |
| Poor | 9.1 |
| Fair | 23.4 |
| Good | 32.8 |
| Very good | 27.5 |
| Excellent | 7.1 |
| Job satisfaction (n = 598)a | |
| Strongly disagree | 1.8 |
| Disagree | 7.9 |
| Neither agree nor disagree | 13.2 |
| Agree | 53.7 |
| Strongly agree | 23.4 |
| Burnout (n = 600) | |
| I feel completely burned out and often wonder if I can go on. | 1.3 |
| The symptoms of burnout that I’m experiencing won’t go away. I think about frustrations at work a lot. | 7.8 |
| I have one or more symptoms of burnout, such as physical or emotional exhaustion. | 29.5 |
| Occasionally I am under stress at work, but I don’t feel burned out. | 49.5 |
| I enjoy my work. I have no symptoms of burnout. | 11.8 |
Response to “Overall, I am satisfied with my current job.”
DISTRIBUTIONS FOR PCMH AND WORK ENVIRONMENT
Table 3 gives the distribution of survey responses used to construct the PCMH subscale scores, the total PCMH score, and the work environment covariate. The mean (SD) total PCMH score was 64 (7) on a scale of 0 to 100. The mean (SD) PCMH subscale scores ranged from 61 (8) for access to care and communication with patients to 66 (10) for tracking data. The mean (SD) overall work environment score was 68 (10).
Table 3.
Distribution of Survey Responses Used to Construct the PCMH Subscale Scores, the Total PCMH Score, and the Work Environment Covariatea
| Variableb | % of Respondentsc | ||||
|---|---|---|---|---|---|
| Access to Care and Communication With Patients Subscale (mean [SD] score, 61 [8]; α = .48) | |||||
| Strongly Disagree | Disagree | Neither Agree nor Disagree | Agree | Strongly Agree | |
| Patients see me rather than some other provider when they come in ford | |||||
| A routine visit | 1.3 | 2.6 | 4.9 | 53.7 | 37.5 |
| An urgent care visit | 3.9 | 17.9 | 33.1 | 38.6 | 6.5 |
| Patients with an urgent problem can easily get a same-day appointment with me or another provider in our clinic | 2.2 | 9.7 | 15.8 | 44.6 | 27.8 |
| It is difficult to spend enough time with patients to meet their medical needs | 18.0 | 35.0 | 19.0 | 24.7 | 3.4 |
| I have adequate access to interpreters | 5.3 | 17.1 | 17.1 | 35.5 | 25.0 |
|
| |||||
| Communication With Other Providers Subscale (mean [SD] score, 62 [12]; α = .78) | |||||
| Rarely | Occasionally | Sometimes | Frequently | Almost Always | |
| How often is it difficult for you to communicate about your patients withd | |||||
| Outside specialists | 10.9 | 26.1 | 37.3 | 22.1 | 3.6 |
| Hospital-based providers | 21.7 | 29.1 | 27.1 | 19.4 | 2.7 |
| Emergency departments | 34.3 | 26.0 | 25.3 | 11.3 | 3.0 |
|
| |||||
| Tracking Data Subscale (mean [SD] score, 66 [10]; α = .56) | |||||
| Strongly Disagree | Disagree | Neither Agree nor Disagree | Agree | Strongly Agree | |
| My practice can easily identify patients with a particular disease | 2.4 | 12.0 | 21.0 | 48.4 | 16.2 |
| Our clinic has good systems to track test results and follow up with patients | 2.5 | 14.0 | 17.1 | 47.2 | 19.2 |
|
| |||||
| Care Management Subscale (mean [SD] score, 65 [8]; α = .82) | |||||
| Strongly Disagree | Disagree | Neither Agree nor Disagree | Agree | Strongly Agree | |
| Our clinic has a good system for identifying patients at high risk for poor outcomes | 4.2 | 20.5 | 27.8 | 39.2 | 8.3 |
| Our clinic intensifies services for patients at high risk for poor outcomese | 1.9 | 14.6 | 23.1 | 47.5 | 13.1 |
| Our clinic individualizes services to different patients with different needs | 1.2 | 5.8 | 16.1 | 55.4 | 21.5 |
| Our clinic is effective in helping patients self-manage their chronic illness | 1.4 | 12.7 | 28.9 | 48.2 | 8.8 |
| Care is coordinated well among physicians, nurses, and clinic staff within our clinic | 1.2 | 8.6 | 16.9 | 53.2 | 20.1 |
| Our practice utilizes community resources to meet patients’ care needs | 0.3 | 8.8 | 18.5 | 50.0 | 22.4 |
| Our EMR provides prompts at the time of the patient visit to remind me of key actions to take for the patientse | 10.3 | 21.5 | 19.8 | 35.5 | 13.0 |
|
| |||||
| Quality Improvement Subscale (mean [SD] score, 63 [7]; α = .80) | |||||
| Strongly Disagree | Disagree | Neither Agree nor Disagree | Agree | Strongly Agree | |
| The structure of our clinic promotes giving high-quality care to patients | 0.8 | 6.7 | 16.7 | 54.2 | 21.7 |
| We are actively doing things to improve patient safety | 0.2 | 3.0 | 10.3 | 58.3 | 28.2 |
| Our clinic studies patients’ complaints to identify patterns and prevent the same problems from recurring | 0.8 | 10.9 | 23.4 | 45.7 | 19.2 |
| When we experience a problem in the practice, we make a serious effort to figure out what’s really going on | 1.7 | 8.5 | 17.2 | 52.7 | 20.0 |
| My clinic sends me reports on the quality of care I provide to my patients | 7.5 | 26.9 | 26.7 | 28.4 | 10.5 |
| Most people in this practice are willing to change how they do things in response to feedback from others | 1.8 | 7.5 | 19.0 | 55.7 | 16.0 |
| Providers and staff in the clinic are provided with adequate release time from their regular job duties for quality improvement activities | 10.3 | 28.2 | 28.7 | 25.6 | 7.2 |
| I am rewarded for the work I do in quality improvement | 14.0 | 23.8 | 33.5 | 23.0 | 5.6 |
|
| |||||
| Work Environment Covariate (mean [SD] score, 68 [10]; α = .85) | |||||
| Strongly Disagree | Disagree | Neither Agree nor Disagree | Agree | Strongly Agree | |
| People in this clinic operate as a team | 1.7 | 9.8 | 17.0 | 53.7 | 17.8 |
| Leadership creates an environment where things can be accomplished | 4.0 | 14.3 | 21.8 | 45.9 | 14.0 |
| Leadership promotes an environment that is an enjoyable place to work | 4.2 | 11.0 | 27.2 | 41.9 | 15.7 |
| Candid and open communication exists between physicians and other staff | 3.3 | 10.2 | 18.2 | 50.3 | 18.0 |
| The work I do is appropriate for my role and training | 1.0 | 4.8 | 9.3 | 55.2 | 29.7 |
| I typically have adequate control over | |||||
| My clinic schedule | 5.2 | 15.5 | 18.6 | 47.7 | 13.0 |
| Work interruptions | 10.0 | 23.9 | 21.0 | 37.0 | 8.1 |
| Volume of my patient load | 9.7 | 20.3 | 25.9 | 36.2 | 7.9 |
Abbreviations: EMR, electronic medical record; PCMH, patient-centered medical home.
The survey questions were mapped to the domains of the 2008 National Committee for Quality Assurance PCMH standards and were then consolidated into 5 subscales based on content validity. Each question was scored from 0 to 100 (worst to best), and the subscale scores are the means of these rescaled questions. The mean (SD) total PCMH score was 64 (7) (α = .87), calculated as the mean of 4 of 5 subscale scores (excluding communication with other providers subscale).
The exact wording of some survey questions was changed slightly for brevity.
Due to rounding, data do not sum to 100%.
Included only responses from providers.
Included only responses for clinics that have EMRs.
CORRELATES OF MORALE, JOB SATISFACTION, AND BURNOUT
In the univariate models, the PCMH subscale scores for access to care and communication with patients and for quality improvement were significantly associated with better morale and with increased job satisfaction (Table 4). The PCMH subscale score for care management was associated with higher morale among clinical staff.
Table 4.
Univariate Correlates of Provider and Staff Morale, Job Satisfaction, and Burnouta
| Variable | Odds Ratio (95% CI)
|
|||||
|---|---|---|---|---|---|---|
| Provider
|
Staff
|
|||||
| Morale | Job Satisfaction | Burnout | Moraleb | Job Satisfaction | Burnout | |
| Access to care and communication with patients subscale | 1.77 (1.19–2.62)c | 1.59 (1.21–2.09)d | 1.05 (0.82–1.34) | 2.23 (1.50–3.31)d | 1.54 (1.18–2.01)c | 1.07 (0.84–1.37) |
| Tracking data subscale | 1.13 (0.83–1.54) | 0.90 (0.70–1.14) | 0.83 (0.69–1.01)e | 1.11 (0.83–1.48) | 0.87 (0.69–1.11) | 0.85 (0.70–1.03)e |
| Care management subscale | 1.43 (0.94–2.18)e | 1.10 (0.81–1.48) | 0.91 (0.71–1.17) | 1.74 (1.20–2.53)c | 1.07 (0.80–1.43) | 0.93 (0.73–1.19) |
| Quality improvement subscale | 2.51 (1.66–3.79)d | 1.80 (1.34–2.42)d | 1.12 (0.85–1.47) | 3.39 (2.19–5.24)d | 1.75 (1.30–2.35)d | 1.14 (0.87–1.51) |
| Work environment covariate | 2.14 (1.59–2.86)d | 1.75 (1.41–2.16)d | 1.19 (0.97–1.46)e | 2.94 (2.10–4.12)d | 1.70 (1.38–2.11)d | 1.21 (0.98–1.49)e |
| Total PCMH score | 2.03 (1.24–3.32)c | 1.32 (0.93–1.87) | 0.91 (0.68–1.23) | 2.37 (1.50–3.75)d | 1.28 (0.91–1.81) | 0.93 (0.69–1.25) |
Abbreviation: PCMH, patient-centered medical home.
Odds ratios (95% CIs) are reported from univariate generalized estimating equation logistic regression analyses. Odds ratios indicate how much a 10% increase in the PCMH subscale score, total PCMH score, or covariate score increases the odds that providers and staff rated their workplace morale highly, were satisfied with their job, or had less burnout.
Cut points for morale, job satisfaction, and burnout are as follows: For morale, “poor” and “fair” were combined vs “good,” “very good,” and “excellent.” For job satisfaction, “strongly disagree,” “disagree,” and “neither agree nor disagree” were combined vs “agree” and “strongly agree.” For burnout, “I feel completely burned out and often wonder if I can go on,” “The symptoms of burnout that I’m experiencing won’t go away. I think about frustrations at work a lot,” and “I have one or more symptoms of burnout, such as physical or emotional exhaustion” were combined vs “Occasionally I am under stress at work, but I don’t feel burned out” and “I enjoy my work. I have no symptoms of burnout.”
P < .01.
P < .001.
P >.05 and <.10.
In the multivariate models that included 4 control variables (the presence of an EMR, provider shortage, nursing shortage, and years since the end of clinical training), higher scores on the quality improvement PCMH subscale were significantly associated with higher provider and staff morale, greater provider and staff job satisfaction, and freedom from burnout among clinical staff (Table 5). The associations for the other PCMH sub-scales were attenuated in the adjusted models. To place the meaning of the odds ratios in Table 5 into context, we give the following example of the mean marginal effect of a variable.27 In the multivariate model without work environment, the mean marginal effects of the quality improvement subscale score on morale are 0.18 (95% CI, 0.08–0.28) for providers and 0.23 (95% CI, 0.13–0.33) for staff. In other words, a 10-point increase in the quality improvement subscale score implies mean increases of 0.18 and 0.23 in the probability of higher morale for providers and staff, respectively.
Table 5.
Multivariate Correlates of Provider and Staff Morale, Job Satisfaction, and Burnouta
| Variable | Odds Ratio (95% CI)
|
|||||
|---|---|---|---|---|---|---|
| Provider
|
Staff
|
|||||
| Morale | Job Satisfaction | Burnout | Moraleb | Job Satisfaction | Burnout | |
| Models Without Work Environment – PCMH Subscales | ||||||
| Access and communication with patients | 1.06 (0.63–1.81) | 0.86 (0.52–1.43) | 0.76 (0.47–1.23) | 2.07 (1.13–3.81)c | 1.54 (0.92–2.60) | 1.09 (0.64–1.84) |
| Tracking data | 0.98 (0.65–1.48) | 0.77 (0.51–1.17) | 0.92 (0.63–1.34) | 0.72 (0.45–1.17) | 0.92 (0.59–1.43) | 0.94 (0.61–1.45) |
| Care management | 0.69 (0.36–1.32) | 0.73 (0.38–1.42) | 0.69 (0.38–1.26) | 0.88 (0.46–1.68) | 0.66 (0.37–1.16) | 0.68 (0.38–1.20) |
| Quality improvement | 2.64 (1.47–4.75)d | 2.45 (1.42–4.23)d | 1.01 (0.61–1.67) | 3.62 (1.84–7.09)d | 2.55 (1.42–4.57)e | 2.32 (1.31–4.12)e |
|
| ||||||
| Models Without Work Environment – Total PCMH Score | ||||||
| Total PCMH score | 1.64 (0.95–2.81)f | 1.04 (0.62–1.76) | 0.48 (0.30–0.77)e | 2.63 (1.47–4.71)d | 1.63 (0.99–2.67)f | 1.26 (0.80–1.99) |
|
| ||||||
| Models With Work Environment – PCMH Subscales | ||||||
| Access and communication with patients | 0.99 (0.60–1.63) | 0.85 (0.52–1.41) | 0.74 (0.46–1.21) | 1.78 (1.00–3.17)c | 1.42 (0.84–2.38) | 1.13 (0.67–1.93) |
| Tracking data | 0.92 (0.62–1.37) | 0.73 (0.48–1.12) | 0.92 (0.62–1.35) | 0.64 (0.40–1.03)f | 0.87 (0.56–1.36) | 0.92 (0.60–1.42) |
| Care management | 0.67 (0.36–1.26) | 0.72 (0.37–1.40) | 0.64 (0.34–1.18) | 1.02 (0.56–1.88) | 0.74 (0.41–1.31) | 0.68 (0.38–1.21) |
| Quality improvement | 1.19 (0.55–2.54) | 1.69 (0.80–3.56) | 0.63 (0.30–1.30) | 1.66 (0.71–3.87) | 1.75 (0.80–3.81) | 2.50 (1.12–5.57)c |
| Work environment | 2.29 (1.31–3.97)e | 1.45 (0.85–2.47) | 1.59 (0.95–2.69)f | 2.43 (1.29–4.59)e | 1.50 (0.84–2.68) | 0.91 (0.52–1.62) |
|
| ||||||
| Models With Work Environment – Total PCMH Score | ||||||
| Total PCMH score | 0.66 (0.34–1.26) | 0.49 (0.24–0.99)c | 0.33 (0.18–0.62)d | 0.97 (0.52–1.82) | 0.87 (0.48–1.57) | 0.88 (0.50–1.54) |
| Work environment | 2.51 (1.62–3.90)d | 2.03 (1.30–3.17)e | 1.43 (0.97–2.12)f | 3.34 (2.02–5.54)d | 2.20 (1.39–3.48)d | 1.55 (1.01–2.36)c |
Abbreviation: PCMH, patient-centered medical home.
Odds ratios (95% CIs) are reported from multivariate generalized estimating equation logistic regression analyses. Odds ratios indicate how much a 10% increase in the PCMH subscale or covariate score increases the odds that providers and staff rated their workplace morale highly, were satisfied with their job, or had less burnout. In addition to the PCMH scores and work environment covariate (when listed), all multivariate models contained covariates on the presence of an electronic medical record, provider shortage, nursing shortage, and years since the end of clinical training. For each set of PCMH scores and covariates, we fit 3 multivariate models, one for each outcome of morale, job satisfaction, and burnout.
Cut points for morale, job satisfaction, and burnout are as follows: For morale, “poor” and “fair” were combined vs “good,” “very good,” and “excellent.” For job satisfaction, “strongly disagree,” “disagree,” and “neither agree nor disagree” were combined vs “agree” and “strongly agree.” For burnout, “I feel completely burned out and often wonder if I can go on,” “The symptoms of burnout that I’m experiencing won’t go away. I think about frustrations at work a lot,” and “I have one or more symptoms of burnout, such as physical or emotional exhaustion” were combined vs “Occasionally I am under stress at work, but I don’t feel burned out” and “I enjoy my work. I have no symptoms of burnout.”
P < .05.
P < .001.
P < .01.
P >.05 and <.10.
The work environment covariate correlated highly with several PCMH scores, especially with the quality improvement subscale score (r=0.78) and with the total PCMH score (r=0.59) (P<.001 for both) (Figure). In analyses that included work environment, the associations of PCMH subscale scores with MSB largely disappeared; however, the access to care and communication with patients subscale score correlated with higher staff morale and the quality improvement subscale score correlated with more staff freedom from burnout (Table 5).
Figure.
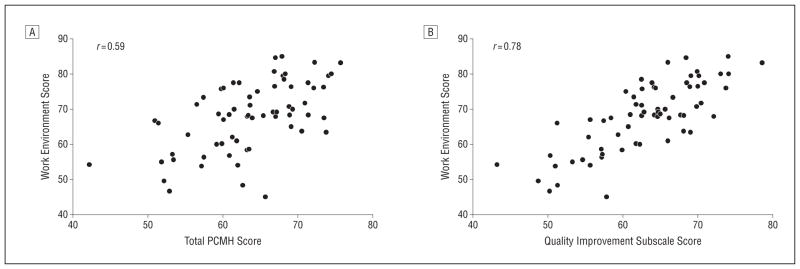
Correlation of work environment score with patient-centered medical home (PCMH) and quality improvement scores at 65 clinics. A, Work environment score vs total PCMH score (r = 0.59). B, Work environment score vs quality improvement subscale score (r = 0.78).
In the multivariate models using the total PCMH score and control variables that excluded work environment, higher total PCMH score correlated with higher staff morale but with less provider freedom from burnout. When work environment was added to the model, the total PCMH score no longer correlated with morale. For providers, a higher total PCMH score was associated with lower job satisfaction and with reduced freedom from burnout.
COMMENT
Our survey of providers and clinical staff at safety net clinics demonstrated that perceptions of PCMH capability were associated on univariate analysis with whether they had higher morale and greater job satisfaction. Specifically, access to care and communication with patients subscale scores and quality improvement subscale scores were associated with better morale and job satisfaction for both providers and staff, and care management subscale scores were associated with better morale for staff. On multivariate analysis of the PCMH subscale scores without the work environment covariate, the quality improvement subscale score was the most consistent independent correlate. The quality improvement subscale includes survey questions on commitment to quality and patient safety, collection of quality data, and willingness of providers and staff to change. These factors may support interventions and culture that improve MSB. In multivariate models without the work environment covariate, the total PCMH score was associated with higher staff morale and tended to correlate with higher provider morale and greater staff job satisfaction. However, the total PCMH score negatively correlated with provider freedom from burnout. Although the findings herein are positive overall, it is important to monitor for increased provider burnout that may result from the work and stress of PCMH implementation and maintenance.
When work environment was added to the models, the associations of PCMH subscale scores with morale and job satisfaction largely disappeared. However, we found that work environment highly correlated with PCMH characteristics, particularly the quality improvement subscale score and the total PCMH score. Work environment has been widely recognized as affecting MSB.7–9 Our measurement of work environment included survey questions on teamwork, supportive leadership, and autonomy. Our univariate and multivariate analyses without work environment showed that the presence of PCMH characteristics likely correlates with higher morale and job satisfaction. However, it may be that PCMH characteristics influence the work environment or that a good work environment greatly facilitates the development of strong PCMH characteristics.
Our study has several limitations. First, a baseline cross-sectional study can show correlations but cannot prove causation. Similarly, it is difficult to determine the exact relationships among PCMH characteristics, work environment, and MSB. Second, we cannot generalize our findings to all safety net clinics because the study clinics were not randomly sampled. Study clinics may have higher motivation and greater capacity for increasing PCMH capability. Third, the evaluation occurred during the early months of the intervention rather than at absolute baseline, but few effects were likely perceived yet by the front-line providers and staff. Fourth, although our response rate of 78.0% is high for provider and staff surveys,28 response bias is possible. Fifth, we created our survey in 2009 based on the 2008 National Committee for Quality Assurance PCMH standards, which do not reflect the 2011 standards.19,28 However, the standards are reasonably similar for the purposes of this evaluation of staff MSB. Sixth, we had limited information on EMR capability. Seventh, our findings represent the perceptions of providers and staff rather than objective criteria. However, perceptions of MSB are probably the most appropriate measures of these constructs. Similarly, provider and staff perceptions of their clinic’s PCMH characteristics are critically important for implementation and sustainability of the PCMH model.
Overall, our study shows that the PCMH model may be promising for improving provider and staff morale and job satisfaction but indicates that provider burnout must be monitored. The PCMH models may be helpful for improving provider and staff satisfaction, increasing the primary care workforce, and reducing turnover. Patient perceptions of the PCMH model are also important, and we are surveying patients about their impressions. However, provider and staff perceptions of the PCMH are critical in their own right. Longitudinal studies of interventions to improve PCMH capacity will enable us to determine whether implementation of the PCMH can truly improve these vital provider and staff outcomes.
Acknowledgments
Funding/Support: This study was supported by The Commonwealth Fund. Dr Birnberg was supported by Postdoctoral Fellowship in Health Services Research award T32-5T32 HS00084-12 from the Agency for Healthcare Research and Quality. Dr Chin is supported by Midcareer Investigator Award in Patient-Oriented Research K24 DK071933 from the National Institute of Diabetes and Digestive and Kidney Diseases and by grants P60 DK20595 and P30 DK092949 from the National Institute of Diabetes and Digestive and Kidney Diseases Diabetes Research and Training Center and Chicago Center for Diabetes Translation Research.
Footnotes
Financial Disclosure: None reported.
Disclaimer: The views presented herein are those of the authors and do not necessarily represent those of The Commonwealth Fund, its directors, officers, or staff.
Previous Presentations: This study was presented in part at the Safety Net Medical Home Initiative; March 8, 2011; Boston, Massachusetts; at the 34th Annual Meeting of the Society of General Internal Medicine; May 6, 2011; Phoenix, Arizona; at the 2011 Annual Research Meeting of AcademyHealth; June 13, 2011; Seattle, Washington; and at the Midwest region meeting of the Society of General Internal Medicine; September 16, 2011; Chicago, Illinois.
Author Contributions: Ms Lewis and Mr Nocon made equal contributions to the research. Study concept and design: Lewis, Nocon, Tang, Vable, Casalino, Quinn, Burnet, Summerfelt, Birnberg, and Chin. Acquisition of data: Lewis, Nocon, Vable, Burnet, and Summerfelt. Analysis and interpretation of data: Lewis, Nocon, Tang, Young Park, Vable, Casalino, Huang, Quinn, Burnet, Summerfelt, Birnberg, and Chin. Drafting of the manuscript: Lewis, Nocon, Tang, Young Park, Quinn, and Chin. Critical revision of the manuscript for important intellectual content: Lewis, Nocon, Tang, Young Park, Vable, Casalino, Huang, Quinn, Burnet, Summerfelt, Birnberg, and Chin. Statistical analysis: Lewis, Nocon, Tang, Young Park, and Quinn. Obtained funding: Chin. Administrative, technical, and material support: Lewis, Nocon, Vable, Quinn, Burnet, and Summerfelt. Study supervision: Lewis, Casalino, Huang, Birnberg, and Chin.
References
- 1.American Academy of Family Physicians, American Academy of Pediatrics, American College of Physicians, American Osteopathic Association. American College of Physicians Web site. [Accessed March 1, 2011];Joint principles of a patient-centered medical home released by organizations representing more than 300,000 physicians. 2007 Mar 5; http://www.acponline.org/pressroom/pcmh.htm.
- 2.National Committee for Quality Assurance. [Accessed August 1, 2011];Patient-centered medical home. http://www.ncqa.org/tabid/631/Default.aspx.
- 3.Nutting PA, Crabtree BF, Miller WL, Stewart EE, Stange KC, Jaén CR. Journey to the patient-centered medical home: a qualitative analysis of the experiences of practices in the National Demonstration Project [published correction appears in Ann Fam Med. 2010;8(4):369] Ann Fam Med. 2010;8(suppl 1):S45–S56. S92. doi: 10.1370/afm.1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hayashi AS, Selia E, McDonnell K. Stress and provider retention in underserved communities. J Health Care Poor Underserved. 2009;20(3):597–604. doi: 10.1353/hpu.0.0163. [DOI] [PubMed] [Google Scholar]
- 5.Rosenblatt RA, Andrilla CHA, Curtin T, Hart LG. Shortages of medical personnel at community health centers: implications for planned expansion. JAMA. 2006;295(9):1042–1049. doi: 10.1001/jama.295.9.1042. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Medicare & Medicaid Services. [Accessed March 1, 2011];Details for Federally Qualified Health Center Advanced Primary Care Practice Demonstration. 2010 Nov 10; http://www.cms.gov/demoprojectsevalrpts/md/itemdetail.asp?itemid=CMS1230557.
- 7.Linzer M, Manwell LB, Williams ES, et al. MEMO (Minimizing Error, Maximizing Outcome) Investigators. Working conditions in primary care: physician reactions and care quality. Ann Intern Med. 2009;151(1):28–36. W6–W9. doi: 10.7326/0003-4819-151-1-200907070-00006. [DOI] [PubMed] [Google Scholar]
- 8.Williams ES, Konrad TR, Linzer M, et al. SGIM Career Satisfaction Study Group. Physician, practice, and patient characteristics related to primary care physician physical and mental health: results from the Physician Worklife Study. Health Serv Res. 2002;37(1):121–143. [PubMed] [Google Scholar]
- 9.Scheurer D, McKean S, Miller J, Wetterneck T. U.S. physician satisfaction: a systematic review. J Hosp Med. 2009;4(9):560–568. doi: 10.1002/jhm.496. [DOI] [PubMed] [Google Scholar]
- 10.Zangaro GA, Soeken KL. A meta-analysis of studies of nurses’ job satisfaction. Res Nurs Health. 2007;30(4):445–458. doi: 10.1002/nur.20202. [DOI] [PubMed] [Google Scholar]
- 11.Quinn MA, Wilcox A, Orav EJ, Bates DW, Simon SR. The relationship between perceived practice quality and quality improvement activities and physician practice dissatisfaction, professional isolation, and work-life stress. Med Care. 2009;47(8):924–928. doi: 10.1097/MLR.0b013e3181a393e4. [DOI] [PubMed] [Google Scholar]
- 12.Graber JE, Huang ES, Drum ML, et al. Predicting changes in staff morale and burnout at community health centers participating in the Health Disparities Collaboratives. Health Serv Res. 2008;43(4):1403–1423. doi: 10.1111/j.1475-6773.2007.00828.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marsteller JA, Hsu YJ, Reider L, et al. Physician satisfaction with chronic care processes: a cluster-randomized trial of guided care. Ann Fam Med. 2010;8(4):308–315. doi: 10.1370/afm.1134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leibowitz R, Day S, Dunt D. A systematic review of the effect of different models of after-hours primary medical care services on clinical outcome, medical workload, and patient and GP satisfaction. Fam Pract. 2003;20(3):311–317. doi: 10.1093/fampra/cmg313. [DOI] [PubMed] [Google Scholar]
- 15.Belardi FG, Weir S, Craig FW. A controlled trial of an advanced access appointment system in a residency family medicine center. Fam Med. 2004;36(5):341–345. [PubMed] [Google Scholar]
- 16.Thind A, Freeman T, Thorpe C, Burt A, Stewart M. Family physicians’ satisfaction with current practice: what is the role of their interactions with specialists? Healthc Policy. 2009;4(3):e145–e158. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2653706/?tool=pubmed. Accessed October 9, 2011. [PMC free article] [PubMed] [Google Scholar]
- 17.Reid RJ, Coleman K, Johnson EA, et al. The Group Health medical home at year two: cost savings, higher patient satisfaction, and less burnout for providers. Health Aff (Millwood) 2010;29(5):835–843. doi: 10.1377/hlthaff.2010.0158. [DOI] [PubMed] [Google Scholar]
- 18.Qualis Health Web site. [Accessed March 1, 2011];Safety Net Medical Home Initiative: change concepts. 2010 Apr; http://www.qhmedicalhome.org/safety-net/upload/Change-Concepts-Sequenced-Final-4_12_10.pdf.
- 19.National Committee for Quality Assurance. [Accessed August 1, 2011];PCMH standards & guidelines. http://www.ncqa.org/tabid/1016/Default.aspx.
- 20.Nutting PA, Miller WL, Crabtree BF, Jaen CR, Stewart EE, Stange KC. Initial lessons from the first National Demonstration Project on practice transformation to a patient-centered medical home. Ann Fam Med. 2009;7(3):254–260. doi: 10.1370/afm.1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reid RJ, Fishman PA, Yu O, et al. Patient-centered medical home demonstration: a prospective, quasi-experimental, before and after evaluation. Am J Manag Care. 2009;15(9):e71–e87. http://www.ajmc.com/publications////AJMC_09sep_ReidWEbX_e71toe87/. Accessed October 12, 2011. [PubMed] [Google Scholar]
- 22.Menachemi N, Powers TL, Brooks RG. The role of information technology usage in physician practice satisfaction. Health Care Manage Rev. 2009;34(4):364–371. doi: 10.1097/HMR.0b013e3181a90d53. [DOI] [PubMed] [Google Scholar]
- 23.Birnberg JM, Drum ML, Huang ES, et al. Development of a Safety Net Medical Home Scale for health centers [published online ahead of print August 12, 2011] J Gen Intern Med. 2011 doi: 10.1007/s11606-011-1767-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rohland BM, Kruse GR, Rohrer JE. Validation of a single-item measure of burn-out against the Maslach Burnout Inventory among physicians. Stress Health. 2004;20(2):75–79. [Google Scholar]
- 25.Smith CS, Morris M, Hill W, et al. Testing the exportability of a tool for detecting operational problems in VA teaching clinics. J Gen Intern Med. 2006;21(2):152–157. doi: 10.1111/j.1525-1497.2006.00313.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O’Malley AJ, Landon BE, Guadagnoli E. Analyzing multiple informant data from an evaluation of the Health Disparities Collaboratives. Health Serv Res. 2007;42(1 pt 1):146–164. doi: 10.1111/j.1475-6773.2006.00597.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greene WH. Econometric Analysis. 3. Upper Saddle River, NJ: Prentice Hall; 1997. pp. 339–350. [Google Scholar]
- 28.Asch DA, Jedrziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50(10):1129–1136. doi: 10.1016/s0895-4356(97)00126-1. [DOI] [PubMed] [Google Scholar]


