Abstract
Depression is highly comorbid with HIV and may contribute to increased sexual transmission risk behavior (TRB) amongst HIV-infected MSM, the largest risk group for HIV in the U.S. However, examinations of this effect are inconsistent. The present longitudinal analyses of 746 HIV-infected MSM is from a multi-site “prevention for positives” study. A non-linear association between depression and TRB emerged. Moderate levels of depression (compared to either low or high levels) were associated with a more modest decline in the odds of sexual risk behavior over 12-month follow-up. Assessing depression in HIV primary care settings may help to identify those at risk and integrating the treatment of depression in to secondary prevention and treatment initiatives may decrease the likelihood of sexual risk and help to contain the epidemic among MSM.
Keywords: HIV prevention with positives, men who have sex with men, sexual risk, depression
INTRODUCTION
Gay, bisexual, and other men who have sex with men (MSM) are the group most heavily affected by HIV/AIDS in the United States [1]. The most recent surveillance data revealed that MSM accounted for 62% of all new HIV/AIDS diagnoses in the United States in 2011, and this group represents approximately half of all individuals living with HIV/AIDS in the United States despite representing approximately 4% of the population. In the absence of a vaccine or other bio-medical approach that durably prevents HIV acquisition, it continues to be important to identify risk factors that can be addressed through behavioral interventions. Although recent findings suggest that primary chemoprophylaxis [2] and treatment as prevention [3] can decrease HIV transmission, antiretroviral treatment is not a substitute for the promotion of safer sexual practices.
Depression is one of the most frequently occurring comorbidities in HIV-infected patients [4] and may potentiate sexual risk among MSM. Examinations of this effect, however, have produced inconsistent results with some studies reporting increased rates of risky sex in depressed MSM, and others reporting no differences in risk [5]. One potential explanation for equivocal findings for the association between depression and sexual risk behavior is that the association may be non-linear. In fact, a longitudinal analysis of 4295 HIV-negative MSM found that men with moderate levels of depression were more likely to acquire HIV during the course of the study compared to those with low or high depression, while controlling for a variety of other risk factors [6]. These authors hypothesized that MSM with moderate levels of depression may be less likely to seek treatment for their depressive symptoms than those with more severe depression, thus accounting for the increase in risk behavior.
Alternatively, the presence of depressive symptoms may reduce an individual’s motivation to engage in self-care and thus increase the likelihood of risk behavior [7]. However, individuals with more severe depressive symptomatology tend to experience the more debilitating neurovegetative symptoms of depression, including fatigue, social isolation, and loss of interest in sex. The presence of these neurovegetative symptoms at higher levels of depression may actually reduce the likelihood of engaging in risk behaviors. Accordingly, a non-linear relationship may better describe the association between depression and risk for HIV, as evidence suggests in HIV-uninfected MSM [6]. This effect, however, remains to be examined in a sample of HIV-infected MSM.
The purpose of the current study was to examine both potential linear and non-linear associations between depression and sexual risk in a large sample of HIV-infected MSM. Based on the existing literature, it was hypothesized that the linear relationship between depression and transmission risk behavior (TRB; unprotected anal or vaginal sex with negative or unknown status partners) over time would not be significant but that a significant non-linear relationship between depression and sexual risk behavior would emerge, such that depression would be more strongly linked to risky sexual behavior in HIV-infected MSM with moderate levels of depression than those with low or high levels of depression.
METHODS
Participants
Participants were HIV+ MSM from a “prevention for positives” trial of sexual risk reduction interventions for HIV+ men and women across 15different intervention sites in the United States (See Myers et al. [8] for more details). MSM were included in the current analyses from all sites that assessed for depression using continuous measures, resulting in 746 HIV+ MSM from six sites. Across these six sites, 56.6% were enrolled in an active treatment arm, and the mean age of the sample was 41.9 (SD = 8.5). The majority of this sub-sample was White (63.3%), followed by African American (23.4%), Hispanic/Latino (9.9%), and Other (3.4%), which was comparable to the racial/ethnic distribution of the MSM across all 15 sites [9].
Measures
Demographic Characteristics
Age, education level, and race/ethnicity were assessed via self-report. For full description of demographic characteristics of the sample, see Myers et al. [8].
Depression Measures
Different measures of depressive symptoms were used across the 6 study sites included in this analysis. The Center for Epidemiologic Studies Depression Scale (CES-D) was used at two sites and is a reliable measure for assessing depressive symptoms across racial, gender, and age categories [10, 11] with good internal consistency and construct validity [12]. One site used an abbreviated CES-D measure (three items assessing depression, sadness and loneliness on a 4-point scale). The possible scores ranged from 0–12. One site utilized the Depression subscale of the Profile of Mood States (POMS), which is a 65-item survey divided into six factor-derived subscales: vigor, tension, fatigue, confusion, anger, and depression (Cronbach's alpha = .91) [13]. One site used the Patient Health Questionnaire (PHQ) to assess depressive symptoms. The 9 –items of the PHQ were scored and totaled according to the standardized procedures [14]. One site used the Beck Depression Inventory (BDI), which is a 21-item measure of depressive symptoms using a four point likert scale (total score range is 0 to 63) [15].
Depression Variable
Those items that assessed the physical symptoms of depression (i.e., fatigue, appetite, sleep. loss of interest in sex) were removed to avoid overlap with symptoms of advancing HIV. The total affective/cognitive depression scores for each site were standardized separately using z-score transformation in order to be comparable across sites. Transformed variables were combined into a single aggregate measure of depression, and all subsequent analyses were conducted using this aggregate measure. This method for integrating measures from different distributions has been broadly recommended in behavioral research [16 17] and specifically for comparing across different measures and distributions [18]. The resulting variable had a mean of −.018 and a standard deviation of .98 indicating that the resulting variable closely approximated the standard deviation scores. To examine the linear effect of depression, on change in sexual risk over time this continuous measure was used. In order to examine the non-linear effect of depression on sexual risk behavior the continuous depression variable was categorized according to quartiles. Two dummy coded variables were created identifying low depression (lowest quartile), high depression (highest quartile) with moderate depression (the 2nd and 3rd quartiles) as the reference category. Categorization according to clinical severity cutoffs was not feasible as two of the study sites used measures of depression that do not have published clinical cutoffs. Further, clinical categorization is problematic because of the marked disparity across scales in the classification of depression severity [19]. Nevertheless, four of the sites utilized depression measures with published clinical cut off scores [10, 11, 14, 15] which allows for a general clinical description of the moderate depression category. Within the moderate depression category the range of BDI scores was 6 – 20 with 62.7% of the scores falling in the BDI “mild” range. For the two sites that used the CES-D the range of raw scores was 11–25 with 69.6% of scores less than16 (the CES-D cutoff for major depression). For the PHQ9 the range of scores was 2 – 17 with 90.5% of scores less than 15, the cutoff for major depression. These findings suggest that the moderate depression category performs well by including relatively few participants at or above the highest clinical cutoffs (e.g., serious depression, major depression7 severe), although, performs less well by including more participants at or below the lower clinical cutoffs (e.g., minimal depression).
Sexual Risk for HIV Transmission. This variable was assessed by self-report and assessed unprotected anal or vaginal intercourse in the three months prior to each assessment point with serodiscordant partners (HIV-uninfected or HIV status unknown). A dichotomous variable was created to indicate whether or not participants had engaged in unprotected anal or vaginal intercourse with serodiscordant partners in the previous three months (0 = no risk; 1 = HIV transmission risk).
Analyses
Analyses were conducted using Hierarchical Linear Modeling (HLM) [20]. HLM is well-suited for longitudinal analyses of slopes of change in an outcome variable (i.e., log odds of sexual risk behavior), and it allows for more reliable parameter estimates of the relationship between depression and change in log odds of sexual risk. Level 2 covariates included participant age, race/ethnicity, and treatment condition. The structure of the HLM models is provided by the following equations:
- Level 1 Model
ProbYti (Y = 1/b) = βti Log[βti/(1− β)] = β0i + βti*(Time)+ ℮ - Level-2 Model
β0i (intercept) = γ00 + μ0 βti (slope) = γ01 + γ11*(Depression) + γ12*(treatment condition) + γ13*(Age) + γ14*(race/ethnicity) + μ1.
Full maximum likelihood estimation was used to model frequency of unprotected sex as the dependent variable. A Bernoulli distribution was used in estimating the odds of unprotected sex as this technique helps to account for deviations from normality in dichotomous outcome variables and an over-preponderance of cases with values of zero. Estimates are from the population-average model using robust standard errors. All continuous variables in the model were centered around their mean and dichotomous variables were coded 0/1 to facilitate model interpretation. Time (months since baseline) provided the structure of the Level 1 model (0, 6, 12) with the presence or absence of sexual transmission risk as the outcome. This use of HLM is consistent with our previous work in HIV patient samples using Level 2 predictors to account for change in repeated measures, time structured, Level 1 data [21–23]. In order to facilitate the interpretation of the results, the log odds slope estimates were transformed back into predicted probabilities (i.e. the predicted proportion of the sample with sexual transmission risk)
RESULTS
Initially, an unconstrained model (without Level 2 predictors or covariates) was run to estimate the slope of the odds of sexual risk over time for the entire sample and to confirm the presence of individual variability in the slope.
There was a significant decrease in the odds of HIV sexual transmission risk for the sample as a whole (OR = .94; 95% CI: .93 – .95, df = 745, p< .001) per month between baseline and 12-month follow-up. There was also significant variability about the slope of sexual risk (χ2 = 2212.36, df = 745, p< .001), indicating the existence of unexplained variance in decreasing sexual risk over time that may be accounted for by predictors (i.e., depression) in the Level 2 model. Next, the Level 2 model was specified examining the linear effects of depression that included the continuous measure of depression and three covariates in order to control for potential differences in the change in predicted probability of sexual risk over time due to age, race/ethnicity, and receiving a sexual risk reduction intervention.
Depression did not significantly alter the change in odds of sexual risk over time (OR = 1.00; 95% CI: .98 – 1.01, df = 741, p = .66). Older age was associated with a significant reduction in the odds of sexual risk over time (OR = .99; 95% CI: .996 – .999, df = 741, p = .004). Neither race/ethnicity nor receiving treatment was associated with significant changes in the odds of sexual risk. For a comprehensive presentation of the treatment effects across all 15 study sites, including site-specific treatment effects, see Myers et al. [8].
The non-linear effects of depression were examined by replacing the continuous measure of depression with two dummy coded variables, as described above, in the Level 2 model. The decrease per month in the odds of sexual risk for those with moderate depression was significant (OR = .95: 95% CI: .93 – .98. df = 740, p < .001). The additional decrease in the odds of sexual risk associated with low depression (OR = .97: 95% CI: .94 – .99. df = 740, p< .05) was also significant (over and above the effects of the moderate depression reference category). Similarly, the additional decrease in the odds of sexual risk associated with high depression was also significant (OR = .97: 95% CI: .96 – .98. df = 740, p< .05). In the HLM equation change for the low (or high) depression group is estimated as an increment to the moderate depression. For this reason the odds ratios are not comparable but rather are additive. As these HLM models provide tests of the significances of the differences in the change in HIV sexual transmission risk over time for the low and high depression groups over and above the moderate depression group these are significance tests for the differences in slope of the odds of sexual risk. Therefore, over the course of 12 months of follow up HIV-infected MSM with moderate levels of depression experienced significantly less decline in the odds of HIV sexual transmission risk compared to those with either low depression or high depression.
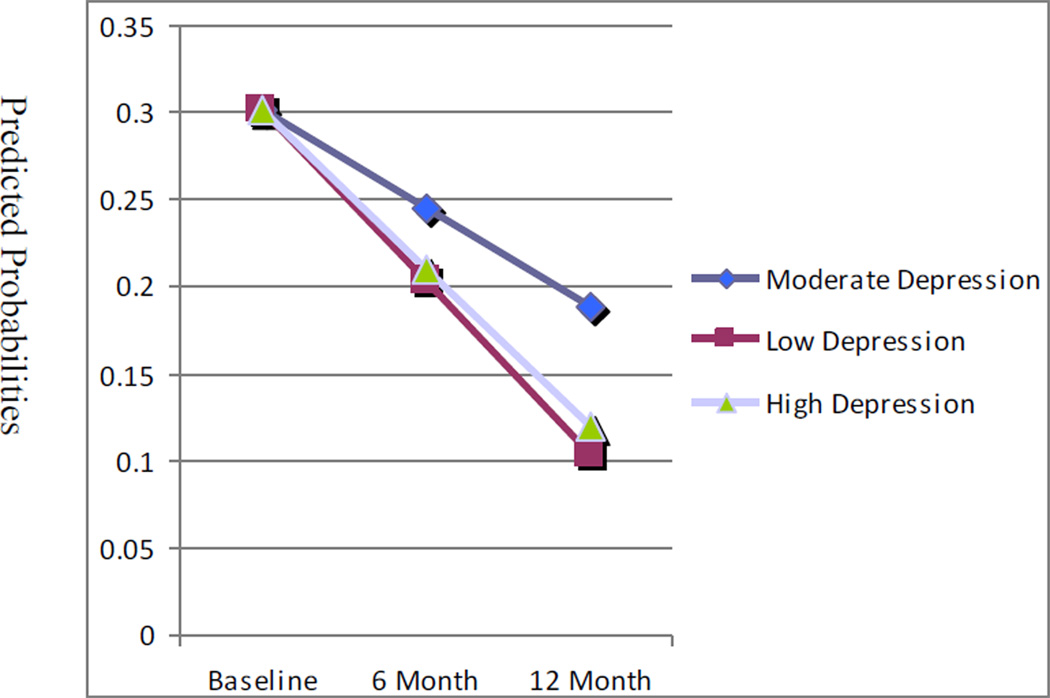
The odds for the low (and high) depression group reflect the additional change in slope over and above the change for the moderate depression group. The odds for the separate levels of depression were used with the HLM equations to calculate predicted probabilities of HIV sexual transmission risk behavior to illustrate the relative differences in slope estimates as the predicted probabilities are directly comparable across depression categories. For the moderate depression group decreasing 6 and 12 month predicted probabilities were 0.245 and 0.188 respectively. For those low in depression the predicted probability of sexual risk at 6 and 12 months was 0.203 and 0.104 respectively. Similarly for those with high depression the predicted probability of sexual risk at 6 and 12 months was 0.210 and 0.120 respectively. These are presented in Table 1 with their significance tests and are represented graphically in Figure 1.
Table 1.
Odds ratios, confidence intervals, significance tests, and predicted probabilities for sexual risk estimated separately for men with moderate, low, and high depression.
| Depression Level: |
Odds Ratio |
95% CI | t | Approx df |
p | 6 month predicted probability |
12 month predicted probability |
|---|---|---|---|---|---|---|---|
| Moderate | .95 | .93 – 98 | −3.49 | 740 | <.001 | 0.245 | 0.188 |
| Low | .97 | .94 – .99 | −2.27 | 740 | <.05 | 0.203 | 0.104 |
| High | .97 | .95 – .99 | −1.97 | 740 | <.05 | 0.210 | 0.120 |
Figure 1.
Change in the Predicted Probabilities of Sexual Risk Over Time for Groups Low, Moderate and High in Depression
NOTE: Depression groups were categorized by quartiles where by the middle two quartiles (moderate depression) are compared to the lowest quartile (low depression) and the highest quartile (high depression). The slopes reported are predicted probabilities controlling for other covariates in the model.
The relative differences in the odds of sexual risk over time between those with low depression and those with high depression was tested using alternate dummy codes and they did not differ significantly (OR = .996: 95% CI: .97 – 1.02. df = 740, p=76). The pattern or significances of these results did not change when an additional categorical covariate, coded to identify each of the 6 study sites, was added to the Level 2 model.
DISCUSSION
The current study reports on the relationship between depression and HIV sexual transmission risk from 6 of 15 sites that assessed continuous measures of depression in HIVinfected MSM enrolled in a multisite “prevention for positives” intervention across the United States [8]. Moderate levels of depression were associated with significantly less decrease in the odds of sexual transmission risk for HIV over 12 month follow up compared to those with either low depression scores or high depression scores. The linear effect of depression was not significantly related to the slope of change in odds of sexual risk. This is the first study to show this effect for moderate levels of depression on sexual risk in HIV-infected MSM. As MSM enrolled in this “prevention for positives” study reported significantly higher rates of sexual risk behavior compared to heterosexual participants [9] the identification of significant predictors of sexual risk amongst in this group is particularly relevant.
Our finding that moderate levels of depression are associated with less improvement over time in the odds of engaging in sexual risk in HIV-infected MSM is consistent with a previous finding in HIV-uninfected MSM [6]. It is plausible that MSM may be engaging in higher levels of sexual behavior to cope with moderate levels of depressive symptoms where as MSM with higher levels of depression may be suffering severe depression-related impairment (e.g., loss of interest in sex) that impact the frequency of both anal intercourse and unprotected anal intercourse. The association between moderate levels of depression and higher levels of risk over time helps to shed light on equivocal findings for the association between these two variables in the literature [5]. Future research should consider whether the processes by which depression leads to sexual risk function similarly in both HIV-infected and HIV-uninfected MSM. If this is the case, then similar intervention strategies to reduce depression and sexual risk may be efficacious in both populations.
Moreover, recent evidence identifies depression amongst MSM as only one of a number of overlapping (i.e., syndemic) risk factors that function synergistically to increase sexual risk and other health risk behaviors [24] As we now understand that these multiple symptomatology patterns and psychosocial stressors interact to confer increased risk, clinical interventions and future treatment development work with this population must consider multiple influences on health risk behavior. Mental health treatment priorities in this vulnerable patient population should begin to address depression and other mental health problems in the context of these myriad overlapping risk factors, including (but not limited to) trauma history, intimate partner violence, and alcohol and substance use.
These results are best interpreted within the context of methodological limitations to the design of the current study. Although the measures of depression used at each of the six sites included in this analysis are commonly reported in studies with HIV-infected individuals, the measures of depressive symptoms were not consistent across all sites. Although the individual measures were aggregated through z-score transformations in order to use all available data, these differing measures have varying psychometric properties and may represent variations of the same construct. It is not possible, within the context of the longitudinal design, to specify causality in the relationship between moderate levels of depression and sexual risk. The intervention sites differed in terms of the populations they served, and we were therefore unable to compare the effect of depression on sexual risk across sites. We acknowledge that there are limitations to using a dummy codes to examine the non-linear relationship between depression and HIV sexual transmission risk and that this method was selected over the use of quadratic transformation in the HLM models. Our hypotheses were based, in part, on previous research that distinguished moderate levels of depression from other levels of depression using categorical variables and our approach is broadly consistent with that approach [6]. In addition, the categorization of the standardized depression score was based upon quartiles, as clinical cutoffs were not available for all measures used. This categorization may have introduced some bias creating the possibility that, for some participants, categorization may not accurately capture the severity of their clinical depression.
Despite these limitations, the results of the current study, in conjunction with previous findings [6], indicate that the association between depression and sexual risk in MSM may be non-linear, and that MSM with moderate levels of depression may be particularly vulnerable to engaging in risky sexual behavior. These findings have important clinical implications and suggest that treating depressive symptoms with either medication or evidence-based interventions in this population may not only improve mental health functioning but may also lead to reductions in sexual transmission risk and help to offset new HIV infections. As evidence continues to emerge that multiple psychosocial stressors and mental health problems interact synergistically to increase risk for HIV acquisition and transmission and other negative health outcomes in this population, it may be particularly important to integrate mental health screening in to HIV primary care. This will facilitate the provision of quality care and help support secondary HIV prevention outcomes for those managing the dual challenges of depression and HIV.
ACKNOWLEDGMENTS
This project was supported by a grant awarded to Kenneth H. Mayer from the Health Resources and Services Administration Projects of National Significance Initiative (H97HA01293-01-00). During the preparation of this manuscript, Steven A. Safren was supported by a grant from the National Institute of Mental Health (K24MH094214). The content is solely the responsibility of the authors and does not necessarily represent the official views of the HRSA or the National Institute of Mental Health. The authors would also like to acknowledge the contributions of the Cross-Site Depression Prevention for Positives Team: Laura H. Bachman (University of Alabama), Ken Burton (El Rio Neighborhood Health Center), Nancy Glick (Mt. Sinai Hospital Chicago), Lourdes Illa (University of Miami), Steve Morin (University of California San Francisco), and E. Byrd Quinlivan (University of North Carolina), and the HRSA SPNS Project Officer, Faye Malitz.
Footnotes
The predicted probability estimates were calculated by applying the following formula φ= eηij/1 + eηij (where φ is the predicted probability, and ηij is the predicted log odds solving the for the equation γ00 + γ01 + γ11*(Depression Dummy Code 1) + γ12*(Depression Dummy Code 2) + γ13*(treatment condition)+ γ14*(Age) + γ15*(race/ethnicity) + μ1, with time (γ11) equal to 6 month and 12 months respectively and holding the other covariates constant.
REFERENCES
- 1.Center for Disease Control and Prevention (CDC) Fact Sheet: HIV among gay and bisexual men. Atlanta, GA, USA: Division of HIV/AIDS Prevention, CDC; 2012. May, http://www.cdc.gov/hiv/topics/msm/pdf/msm.pdf. [Google Scholar]
- 2.Grant RM, Lama JR, Anderson PL, McMahan V, Liu AY, Vargas L. Preexposure chemoprophylaxis for HIV prevention in men who have sex with men. New Engl J Med. 2010;363:2587–2599. doi: 10.1056/NEJMoa1011205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. New Engl J Med. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, et al. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Arch Gen Psychiatr. 2001;58:721–728. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- 5.Mustanski BS, Newcomb ME, Du Bois SN, Garcia SC, Grov C. HIV in young men who have sex with men: a review of epidemiology, risk and protective factors, and interventions. J Sex Res. 2011;48:218–253. doi: 10.1080/00224499.2011.558645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, et al. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;20:731–739. doi: 10.1097/01.aids.0000216374.61442.55. [DOI] [PubMed] [Google Scholar]
- 7.Allgower A, Wardle J, Steptoe A. Depressive symptoms, social support, and personal health behaviors in young men and women. Health Psychol. 2001;20:223–227. [PubMed] [Google Scholar]
- 8.Myers JJ, Shade SB, Rose CD, Koester K, Maiorana A, Malitz FE, et al. Interventions delivered in clinical settings are effective in reducing risk of HIV transmission among people living with HIV: results from the Health Resources and Services Administration (HRSA)'s Special Projects of National Significance initiative. AIDS Behav. 2010;14:483–492. doi: 10.1007/s10461-010-9679-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morin SF, Myers JJ, Shade SB, Koester K, Maiorana A, Rose CD. Predicting HIV transmission risk among HIV-infected patients seen in clinical settings. AIDS Behav. 2007;11:S6–S16. doi: 10.1007/s10461-007-9253-4. [DOI] [PubMed] [Google Scholar]
- 10.Knight RG, Williams S, McGee R, Olaman S. Psychometric properties of the Centre for Epidemiologic Studies Depression Scale (CES-D) in a sample of women in middle life. Behav Res and Ther. 1997;35:373–380. doi: 10.1016/s0005-7967(96)00107-6. [DOI] [PubMed] [Google Scholar]
- 11.Roberts RE, Vernon SW, Rhoades HM. Effects of language and ethnic status on reliability and validity of the Center for Epidemiologic Studies-Depression Scale with psychiatric patients. J Nerv Ment Dis. 1989;177:581–592. doi: 10.1097/00005053-198910000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 13.McNair DM, Lorr M, Droppleman LF, et al. Manual: Profile of Mood States. San Diego: Educational & Industrial Testing Service; 1971. [Google Scholar]
- 14.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 15.Beck AT. Depression: Causes and Treatment. Philadelphia: University of Pennsylvania Press; 2006. [Google Scholar]
- 16.Rosenthal R, Rosnow RL. Essential of behavioral research; methods and data analysis. 2nd ed. New York: McGraw Hill; 1991. [Google Scholar]
- 17.Cohen J. Statistical power analysis for the behavioral sciences. 2nd Ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- 18.Hedges LV, Olkin I. Statistical methods for meta-analysis. Orlando, FL: Academic Press; 1985. [Google Scholar]
- 19.Zimmerman M, Martinez JN, Friedman M, Boerescu DA, Attiullah N, Toba C. How can we use depression severity to guide treatment selection when measures of depression categorize patients differently? J Clin Psychiatry. 2012;73(10):1287–1291. doi: 10.4088/JCP.12m07775. [DOI] [PubMed] [Google Scholar]
- 20.Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd Ed. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 21.Ironson G, O'Cleirigh C, Fletcher MA, Laurenceau JP, Blabin E, Klimas N, et al. Psychosocial factors predict CD4 and viral load change in men and women with HIV in the era of HAART. Psychosom Med. 67:1013–1021. doi: 10.1097/01.psy.0000188569.58998.c8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ironson G, O'Cleirigh C, Leserman J, Stuetzle R, Fordiani J, Fletcher MA, et al. Gender specific effects of an augmented written emotional disclosure intervention on posttraumatic, depressive and HIV disease-related outcomes: a randomized, controlled trial. J Consult Clin Psych. doi: 10.1037/a0030814. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Safren SA, O'Cleirigh C, Bullis JR, Otto MW, Stein MA, Pollack MH. Cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected injection drug users: a randomized controlled trial. J Consult Clin Psych. 80:404–415. doi: 10.1037/a0028208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stall R, Mills TC, Williamson J, Hart T, Greenwood G, Paul J, et al. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. Am J Public Health. 2003;93:939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]