Abstract
The relationship between encounter frequency (average number of provider-patient encounters over a period of time) and blood pressure for hypertensive patients is unknown. We tested the hypothesis that shorter encounter intervals are associated with faster blood pressure normalization.
We performed a retrospective cohort study of 5,042 hypertensive patients with diabetes treated at primary care practices affiliated with two academic hospitals between 2000 and 2005. Distinct periods of continuously elevated blood pressure (≥ 130/85) were studied. We evaluated the association of the average encounter interval with a) time to blood pressure normalization and b) rate of blood pressure decrease.
Blood pressure of the patients with the average interval between encounters ≤ one month normalized after a median of 1.5 months at the rate of 28.7 mm Hg/month compared to 12.2 months at 2.6 mm Hg/month for the encounter interval greater than one month (p < 0.0001 for all). Median time to blood pressure normalization was 0.7 vs. 1.9 months for the average encounter interval ≤ 2 weeks vs. between 2 weeks and 1 month, respectively (p < 0.0001). In proportional hazards analysis adjusted for patient demographics, initial blood pressure and treatment intensification rate, a one month increase in the average encounter interval was associated with a hazard ratio of 0.764 for blood pressure normalization (p < 0.0001).
Shorter encounter intervals are associated with faster decrease in blood pressure and earlier blood pressure normalization. Greatest benefits were observed at encounter intervals (≤ two weeks) shorter than what is currently recommended.
Keywords: hypertension, encounter frequency, visit frequency, outcomes
INTRODUCTION
Elevated blood pressure is one of the major risk factors for macro- and microvascular complications in diabetic patients1–7. Treatment of hypertension decreases these risks8–12 and is highly cost-effective13, 14. Despite abundant evidence of the benefits of lowering blood pressure, most patients with diabetes do not reach evidence-based treatment goals15–17. The reasons for this are not well understood.
Current guidelines recommend that patients be followed up within a month when an elevated blood pressure is noted18. However, the intervals between provider-patient encounters are substantially longer19–23. It is possible that this discrepancy between the guidelines and the practice of medicine contributes to the suboptimal outcomes in patients with hypertension. The currently available evidence on the relationship between encounter intervals and blood pressure is conflicting. Whereas a study of four hundred patients by Guthmann et al found a correlation between return visit interval and percent change in blood pressure, a smaller study of one hundred patients by Parchman et al. failed to detect a statistically significant relationship23, 24. Furthermore, there are no data to provide guidance with respect to the optimal encounter interval for blood pressure control and the current (JNC-VII) guidelines are based largely on expert opinion18.
We performed a retrospective study of over 5,000 patients with diabetes and hypertension followed by primary care physicians to test the hypothesis that shorter encounter intervals are associated with faster blood pressure normalization and to establish the encounter interval associated with optimal blood pressure control.
METHODS
Design
We conducted a retrospective cohort study to investigate whether shorter time between physician-patient encounters is associated with better blood pressure control in patients with diabetes. We evaluated the relationship between a) the average post-hypertensive encounter interval (predictor variable) and b) time to blood pressure normalization (primary outcome variable). We also conducted a secondary analysis to determine the relationship between a) the average post-hypertensive encounter interval and b) rates of decrease of systolic and diastolic blood pressure. Finally, we studied the associations between patient and encounter characteristics at a given physician-patient encounter with an elevated blood pressure and the interval to the next encounter.
Study Cohort
Hypertensive patients with diabetes followed by primary care physicians affiliated with Massachusetts General Hospital (MGH) and Brigham and Women’s Hospital (BWH) for at least two years between 01/01/2000 and 08/31/2005 were studied. Patients were included in the analysis if they were at least 18 years old, had a documented diagnosis of diabetes mellitus, and had at least one encounter with a physician in a primary care specialty during the study period where a blood pressure above the recommended treatment target was recorded. In order to capture both face-to-face and remote interactions between patients and providers, we defined an encounter as any note in the electronic medical record. Only encounters with documented blood pressures were used in the analysis.
We used 129 and 84 mm Hg as the recommended treatment goals of systolic and diastolic blood pressure, in accordance with the guidelines published prior to the beginning of the study period25. Diagnosis of diabetes was ascertained by analyzing the text of physician notes in the electronic medical record as previously described26. Patients who had at least one encounter with an endocrinologist during the study period that addressed diabetes (as ascertained using billing data and computerized analysis of the text of the notes) were excluded in order to focus the analysis on the care in primary care setting, where most patients with hypertension are treated.
The institutional review board at Partners HealthCare System approved the study, and the requirement for written informed consent was waived.
Study Measurements
A single hypertensive period served as the unit of analysis for the evaluation of primary and secondary outcomes, as previously described27. The beginning of a hypertensive period was defined as the date of the first encounter when a blood pressure above the treatment target was recorded. If the first encounter during the study period had documented blood pressure above the treatment target, this encounter was considered to be the beginning of a hypertensive period. The date of the first subsequent encounter with a blood pressure below the treatment target served as the end of the hypertensive period. If the last encounter during the study period had blood pressure above the treatment target, the date of that encounter was considered the end of the hypertensive period. If more than one blood pressure was documented for any of the study encounters, blood pressure with the lowest mean arterial pressure was used for the analysis. Transient elevations of blood pressure defined as a single encounter with an elevated blood pressure and no treatment intensification, followed by normalization of the blood pressure at the next encounter, were excluded from the analysis.
Time to blood pressure normalization for any hypertensive period was defined as the length of that hypertensive period. Average encounter interval for the hypertensive period was calculated as the length of the period divided by the number of physician-patient encounters during the period. Treatment intensification rate was defined as the ratio of the number of encounters during the hypertensive period where a new anti-hypertensive medication was initiated or the dose of an existing one was increased to the total number of encounters during the period as previously described28. Average rate of blood pressure change was calculated as the difference between the blood pressure at the first and the last encounter during the hypertensive period divided by the length of the period. It was calculated separately for systolic and diastolic blood pressures. The number of acute conditions addressed at an encounter was defined as the number of International Classification of Diseases, 9th edition, clinical modification (ICD-9-CM) billing codes associated with the encounter that represented an acute complaint (most commonly acute pain or infection), as previously described28. We identified a physician as the patient’s primary care provider if he or she had the largest number of encounters with the patient over the study period.
Data Sources
Demographic information, laboratory and billing data, and the text of physician notes were obtained from the Research Partners Data Registry (RPDR). RPDR is a data warehouse that serves as a central clinical data repository for participating hospitals and clinics within the Partners HealthCare System – an integrated healthcare delivery network in eastern Massachusetts that includes MGH and BWH. Blood pressure values and anti-hypertensive treatment intensification were computationally extracted from the text of computerized physician notes in the electronic medical record as previously described29. The sensitivity and specificity of this method are 91% and 96%, respectively, for identification of blood pressure values, and 84% and 95% for identification of anti-hypertensive treatment intensification. Physician specialty was identified using a combination of the information available from the Massachusetts Board of Registration in Medicine and the specialty of the clinic where the physician practiced.
Statistical Analysis
Summary statistics were constructed by using frequencies and proportions for categorical data and by using means, standard deviations, medians and ranges for continuous variables. The univariate associations between continuous variables were assessed using two-sided t-test.
The log-rank test was used to compare Kaplan-Meier survival curves for time to blood pressure normalization between different lengths of encounter interval. Sensitivity analysis limited to the first hypertensive period for each patient was conducted to assess possible effect of correlation between observations for individual patients. A marginal Cox proportional-hazards model for clustered data30 was used to adjust for covariates and to estimate the hazard ratio for blood pressure normalization while accounting for clustering within individual patients. The covariates used in the Cox model included patient age, gender, ethnicity, primary language, health insurance, as well as treatment intensification rate and initial systolic and diastolic blood pressure for the hypertensive period.
To determine the relationship between the encounter interval and the rate of blood pressure change, we constructed a hierarchical (multilevel) multivariable mixed linear regression model with random effects to account for clustering within individual patients and physicians. Random cluster effects were used to generate correlation structure for intra-cluster observations as well as account for individual patient and physician effect levels31. The model also included patient age, gender, ethnicity, primary language, and health insurance and the treatment intensification rate during the hypertensive period. P-values were obtained using type III test.
All analyses were performed with SAS statistical software, version 9.1 (SAS Institute, Inc., Cary, NC).
RESULTS
We identified 22,675 adult patients with diabetes mellitus who had at least one outpatient encounter at a practice affiliated with either of the two hospitals between January 1, 2000 and August 31, 2005. We excluded 763 patients who were treated by an endocrinologist or a diabetologist and 8,425 patients who did not have any encounters with primary care providers (i.e. their primary care physicians were likely outside of the Massachusetts General Hospital and Brigham and Women’s Hospital practice networks). We further excluded 7,190 patients who had been followed for less than two years and 604 patients who never had a blood pressure reading above the treatment target (129/84 mm Hg). Only transient blood pressure elevations (resolved at the next encounter without treatment intensification) were recorded for 651 patients. The remaining 5,042 patients were included in the study.
The median age of study patients was 65; the majority were women (Table 1). On average, the patients were followed for four years during the study period. Their blood pressure was above the recommended target for over 60% of that time. Anti-hypertensive treatment was intensified in 1 out of 5 encounters with elevated blood pressure. On average, patients had two to three distinct periods of continuously elevated blood pressure during the study period. These periods had a median length of 9.0 months, with some lasting up to 68 months. On average, there were 3.8 documented physician-patient encounters during each period of continuously elevated blood pressure (Table 2). Distinct hypertensive periods for the same patient were on average 10.5 months apart (median 8 months), separated by a mean of 3.2 encounters (median 2 encounters) with documented blood pressure below the treatment target.
Table 1.
Patient Characteristics
| Variable | Value |
|---|---|
| Study patients, n | 5,042 |
| Age*, years, mean (± SD) | 64.6 (± 13.3) |
| Women, n (%) | 2,939 (58.3) |
| Ethnicity, n (%) | |
| White | 2,921 (57.9) |
| Black | 914 (18.1) |
| Hispanic | 793 (15.7) |
| Other (includes unknown) | 414 (8.2) |
| English is the primary language, n (%) | 4,146 (82.2) |
| Health insurance*, n (%) | |
| Insured | 3,200 (63.5) |
| Underinsured† | 1,684 (33.4) |
| No prescription coverage‡ | 158 (3.1) |
| Blood pressure§, mm Hg, mean (± SD) | |
| Systolic | 133.5 (± 10.4) |
| Diastolic | 76.1 (± 7.2) |
| Length of follow-up, months, mean (± SD) | 48.2 (± 12.9) |
| Total time with elevated blood pressure, months, mean (± SD) | 29.1 (± 16.6) |
| Frequency of Treatment Intensification, %, mean (± SD) | 20.7 (± 21.4) |
At the end of the study period
Includes Medicaid and FreeCare – a program that provides fully or partially (depending on the income) subsidized health care in Massachusetts
Includes Medicare without supplemental insurance and patients with no reported insurance
Patient-weighted mean metric was calculated by taking the average of the mean metric calculated individually for all study patients
Table 2.
Hypertensive Periods
| Variable | Value |
|---|---|
| Total periods, n | 10,447 |
| Length, months, mean (± SD) | 14.1 (± 14.0) |
| Initial blood pressure, mm Hg, mean (± SD) | |
| Systolic | 141.4 (± 13.6) |
| Diastolic | 79.3 (± 10.7) |
| Maximum blood pressure, mm Hg, mean (± SD) | |
| Systolic | 148.7 (± 17.2) |
| Diastolic | 84.1 (± 10.8) |
| Periods ending in normal blood pressure, n (%) | 8,423 (80.6%) |
| Encounter interval, months, mean (± SD) | 3.7 (± 4.1) |
Encounter Interval and Time to Blood Pressure Normalization
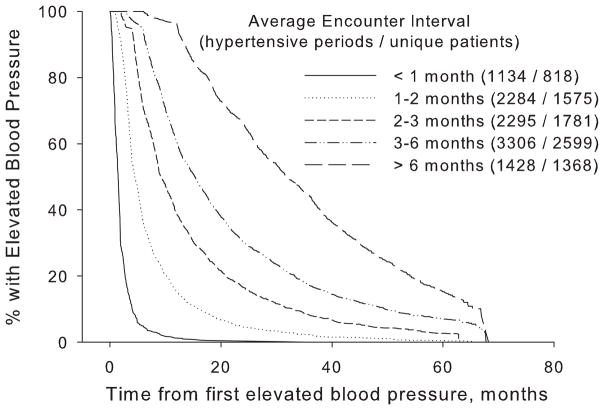
In univariate analysis, for a given hypertensive period the average time from the first documented encounter (for the specific hypertensive period being analyzed) with elevated blood pressure to blood pressure normalization rose progressively from 1.8 months when the average interval between encounters was less than one month to 29.4 months when the average interval was greater than six months (Figure 1). Blood pressure of the patients whose average encounter interval was ≤ 1 month (in accordance with the current guidelines18) normalized after a median of 1.5 months vs. 12.2 months for the patients whose average encounter interval was greater than one month (p < 0.0001). Sensitivity analysis limited to the first hypertensive period for each patient had similar results (data not shown).
Figure 1. Encounter Interval and Time to Blood Pressure Normalization.
Kaplan-Meier curves for time to normalization of blood pressure during a period of continuously elevated blood pressure were plotted for different average encounter intervals. Distinct periods of elevated blood pressure (from the first elevated to the first normal blood pressure) for the same patient were analyzed separately.
The difference in time to blood pressure normalization persisted at encounter intervals shorter than the currently recommended. In a subgroup analysis of 1,158 hypertensive periods of 832 unique patients with an average encounter interval ≤ 1 month, blood pressure of the patients with the average encounter interval ≤ two weeks normalized after a median of 0.7 months vs. 1.9 months for the average encounter interval between two weeks and one month (p < 0.0001). The median encounter interval in this subgroup was 20 days, while 10th and 90th percentiles were 7.5 and 28 days, respectively.
In multivariable analysis adjusted for the patients’ demographic characteristics, initial blood pressure, frequency of treatment intensification and for clustering within individual patients, an increase of one month in the average interval between encounters was associated with a hazard ratio of 0.764 (95% CI 0.755 to 0.774) for blood pressure normalization (p < 0.0001). Increase in the patient’s age and initial blood pressure were also associated with a longer time to blood pressure normalization (p < 0.0001 for each). The association between the average encounter interval and time to blood pressure normalization retained its significance at encounter intervals ≤ 1 month (hazard ratio 0.017; 95% CI 0.012 to 0.023; p < 0.0001). Analysis that was limited to the encounters that had associated billing codes for hypertension showed similar findings (data not shown). Analysis of the relationship between encounter intervals and blood pressure at a pre-specified time horizon showed that shorter encounter intervals were associated with increased probability of normalization of blood pressure at two years after the first elevated blood pressure was detected (data not shown).
Encounter Interval and Rate of Blood Pressure Change
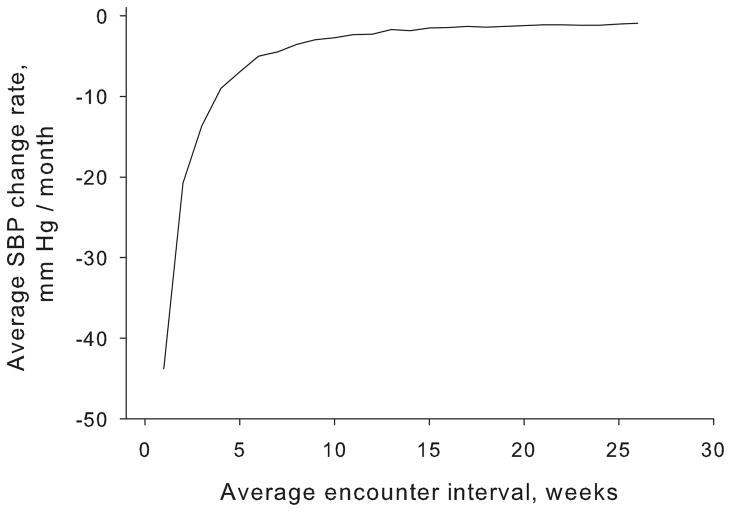
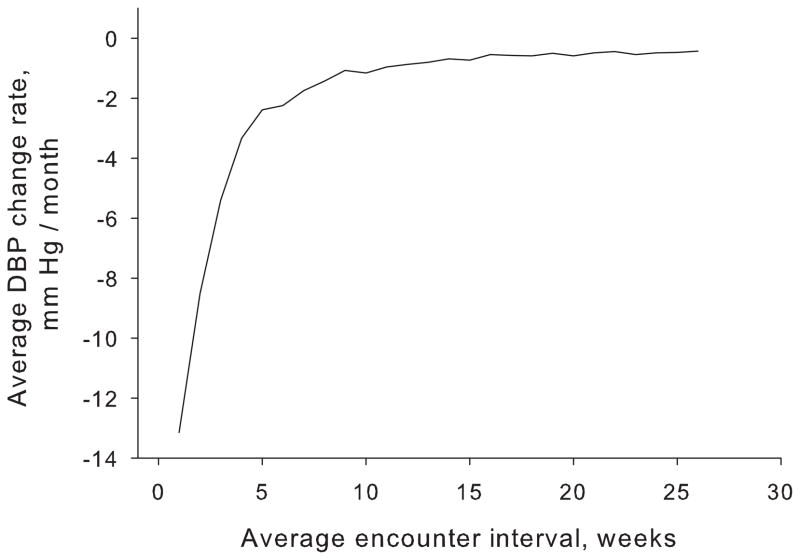
The rate of decrease in systolic blood pressure was over ten-fold higher (28.7 vs. 2.6 mm Hg/month) for patients with the average encounter interval ≤ 1 month compared to the patients with encounter interval greater than one month (p < 0.0001). The rate of decrease in diastolic blood pressure was similarly ten-fold higher (11.3 vs. 1.0 mm Hg/month) for patients with the average encounter interval less than or equal vs. greater than one month (p < 0.0001). When plotted against the average encounter interval, the rates of change in systolic and diastolic blood pressure decreased progressively with longer encounter intervals. For an encounter interval of 1–2 weeks, the rates of decrease for systolic and diastolic blood pressure were 43.8 and 13.1 mm Hg/month, respectively, whereas encounter intervals of 6 months had rates of 0.9 (systolic) and 0.4 mm Hg/month (diastolic) (Figure 2).
Figure 2.
Figure 2A. Encounter Interval and Rate of Change of Systolic Blood Pressure
The average monthly change in systolic (A) and diastolic (B) blood pressure, respectively, was plotted against the average encounter interval. Distinct periods of elevated blood pressure (from the first elevated to the first normal blood pressure) for the same patient were analyzed separately. Dotted lines indicate 95% confidence interval.
Figure 2B. Encounter Interval and Rate of Change of Diastolic Blood Pressure
In multivariable analysis adjusted for the patients’ demographic characteristics, initial blood pressure of the hypertensive period, treatment intensification rate and for clustering within individual patients, systolic blood pressure increased by 0.7 mm Hg/month for each additional month between encounters, while diastolic blood pressure increased by 0.3 mm Hg/month (p < 0.0001 for both). Both systolic and diastolic blood pressure decreased faster for patients who had higher treatment intensification rates (p < 0.0001).
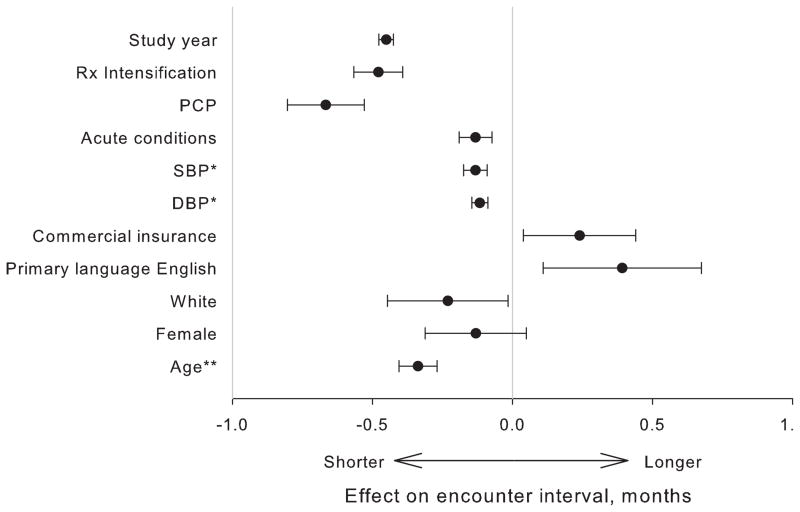
Predictors of Encounter Interval Length
We studied 47,831 patient encounters with documented elevated blood pressure to establish patient and encounter characteristics that were associated with changes in the interval to the follow-up encounter (Figure 3). In a multivariable analysis that included patients’ demographics and adjusted for clustering within individual patients and providers, we found that patients whose anti-hypertensive treatment was intensified during the encounter also had a shorter (by 14.4 days) follow-up interval (p < 0.0001). Length of the interval to the next encounter also decreased by 3.6 and 3.9 days for each 10 mm increase in systolic and diastolic blood pressure during the encounter, respectively, (p < 0.0001 for both). On the other hand, the interval to the next encounter increased by 20 days if the physician seeing the patient was not their regular primary care provider (p < 0.0001).
Figure 3. Effect of Patient and Encounter Characteristics on Encounter Interval.
Circles indicate effect estimates from a multivariable model that included all variables displayed in the figure. Whiskers indicate 95% confidence intervals. “PCP” variable indicates that the encounter was with the patient’s primary care provider (as opposed to a covering physician). “Acute conditions” variable indicates the number of billing codes linked to the encounter that represented an acute complaint (most commonly acute pain or infection). “Commercial insurance” variable indicates that the patient’s health insurance was provided by a private company, as opposed to Medicare and/or Medicaid. “Rx Intensification” indicates whether anti-hypertensive treatment was intensified (a new medication started or the dose of an existing medication increased) during the encounter.
*For every 10 mm Hg
**for every 10 years
DISCUSSION
In this large retrospective study of treatment of hypertension in patients with diabetes we have demonstrated that blood pressure decreases faster and blood pressure control is achieved sooner in patients who have shorter encounter intervals. We have confirmed previous reports that the current guidelines on the encounter interval for patients with elevated blood pressure are seldom followed20, 21, 32. Importantly, our results show that encounter intervals shorter than currently recommended are associated with even greater rates of decrease in blood pressure levels and faster blood pressure normalization.
The relationship between encounter intervals and patient outcomes remains largely unexplored33. A study of patients with rheumatoid arthritis showed that shorter encounter intervals were associated with small decreases in the pain scores and disability index34. However, two smaller studies of encounter intervals for hypertensive patients did not reach consistent conclusions23, 24, possibly due to insufficient sample size. To our knowledge, our report is the largest longitudinal study of the relationship of encounter intervals and outcomes to date –unequivocally showing that shorter encounter intervals are strongly associated with faster achievement of blood pressure control. This finding is particularly important in light of the recent evidence that even short-term elevations in blood pressure are associated with adverse events35.
There is a paucity of evidence to guide providers on the optimal encounter intervals. The report on patients with rheumatoid arthritis found a U-shaped relationship between encounter intervals and outcomes34 with the best outcomes achieved at encounter intervals between 1–2 months. However, this finding may have been biased by the fact that visits by patients with rheumatoid arthritis can be symptom-driven and therefore patients with more frequent visits may have more severe symptoms. This bias is likely to be less pronounced in patients with hypertension which is commonly asymptomatic, particularly at the lower blood pressure levels prevalent in our study population. Our analysis did not reveal a U-shaped relationship. On the contrary, the magnitude of the rate of blood pressure decrease rose progressively with shorter encounter intervals, all the way down to weekly encounters. While some recent studies reported an increased rate of cardiovascular events with aggressive lowering of blood pressure36, our analysis did not find a significant relationship between the rate of blood pressure decrease and mortality (data not shown).
There could be several explanations for our findings. Higher frequency of encounters provides more opportunities for medication intensification, and a number of studies have shown a strong relationship between the rate of treatment intensification and blood pressure control19, 20, 27. Additionally, increased encounter frequency has been linked to improved treatment adherence37, 38. It is possible that regression to the mean may have been a contributing factor as well. However, this phenomenon would have most likely manifested itself as spontaneous return of elevated blood pressure to normal without any intervention. We have therefore excluded patients whose blood pressure normalized after a single encounter with elevated blood pressure without any pharmacologic intervention to reduce its effect.
Some of the blood pressure normalizations could have been due to random variations in blood pressure. More frequent encounters could have led to a higher probability of such random variations being captured in documented blood pressure measurements. This would result in an apparent association between more frequent encounters and faster blood pressure normalization. However, our analysis showed that distinct hypertensive periods for the same patient were on average spaced 10.5 months apart, separated by a mean of 3.2 encounters with documented blood pressure below the treatment target. These findings are more consistent with a sustained decrease in blood pressure achieved by therapeutic intervention than with a random variation.
Similarly to the previously reported smaller observational studies and clinician surveys39, 40, we have found that higher blood pressure and treatment intensification were associated with a shorter interval before the next encounter. Other measures of clinical instability, such as the number of acute conditions addressed during the encounter, were also linked with shorter follow-up intervals. On the other hand, encounter intervals were longer if the patient was seen by the physician who was not their regular caregiver. Combined with our previous findings of lower treatment intensification rate by covering providers28, this result points to the importance of continuity of care in providing optimal treatment.
Shorter encounter intervals may be difficult to implement in practice. Most hypertensive patients are treated by their primary care physicians, and the nationwide shortage of these providers is likely to only grow in the future41, 42. Primary care physicians may therefore have little room to increase the frequency of patient visits, particularly as the demands on their time are already excessive43. Furthermore, patients may prefer longer visit intervals44, possibly because even a 15-minute appointment with a physician imposes a much more extensive temporal cost on the patient, including the time spent on travel and waiting to be seen.
It is evident, therefore, that if shorter encounter intervals are to be achieved, more creative approaches to patient care are needed45. Not all encounters need to be face-to-face visits by individual patients – some could be group visits or telephone or email communications46. Mid-level providers could take over algorithm-based medication titration to relieve the time pressure on the physicians – an approach shown to be effective in a number of studies47–49, even while the intervals between physician visits increased50.
Our study had a number of strengths. First, it included a large number of ethnically diverse patients treated at two hospitals that serve individuals from all socioeconomic strata. Our findings support the current recommendations for frequent follow-up for patients with uncontrolled blood pressure. Finally, our study focused on the treatment of high blood pressure in primary care practices because this is the setting where the majority of patients with hypertension receive their care.
Our study had several limitations. It was conducted in clinics affiliated with two academic medical centers in Eastern Massachusetts and this could limit its generalizability to other geographic and practice settings. The study focused on patients with diabetes and therefore the findings may not apply to other patients with hypertension. We do not have information on the blood pressure measurement techniques which may not have been consistent both between and within individual patients. We also did not have information on the anti-hypertensive medications the patients were taking at the study entry or their adherence to medications throughout the study period, limiting our ability to analyze potential etiological relationships. Hypertensive periods were censored at the beginning of the study. However, unless encounter intervals were systematically uneven over the duration of the period, this should not have biased our results. Our study focused on treatment delivered by physicians because physicians comprised the majority of healthcare providers in the primary care clinics studied51. Therefore our findings may not apply to mid-level providers. Our study utilized electronic medical records data recorded in the course of routine clinical care and it is therefore possible that some of the data could be missing. If the missing data were not missing at random with respect to the outcome variable, this could potentially confound our results. For example, it was not possible to ascertain exactly when the patients’ blood pressure normalized. Consequently shorter encounter intervals could lead to an appearance of accelerated normalization of blood pressure, introducing a bias in our findings. However, a separate analysis showed that shorter encounter intervals were associated with increased probability of normalization of blood pressure at two years after the first elevated blood pressure was detected. This finding supports our interpretation in a manner not subject to bias by the missing blood pressure data. Our analysis included all provider-patient encounters, independent of whether hypertension was addressed during the encounter. However, a separate analysis that was limited to the encounters that had associated billing codes for hypertension showed similar findings. Finally, retrospective nature of the study does not allow us to infer causality in the associations that we have found.
PERSPECTIVES
In summary, we have shown that shorter encounter intervals for diabetic patients with elevated blood pressure are associated with shorter time to blood pressure control and faster decrease in blood pressure. Based on our findings, optimal encounter intervals may be shorter than what is currently recommended. Interventional studies are now needed to confirm the direction of causality in these findings and provide evidence-based guidance for choosing encounter intervals to the thousands of primary care physicians who care for these patients.
Acknowledgments
SOURCES OF FUNDING
This study was supported in part by grants from Agency for Healthcare Research and Quality (5R18HS017030) and Diabetes Action Research and Education Foundation.
Footnotes
CONFLICT OF INTEREST DISCLOSURES
None
References
- 1.Stratton IM, Kohner EM, Aldington SJ, Turner RC, Holman RR, Manley SE, Matthews DR. UKPDS 50: risk factors for incidence and progression of retinopathy in Type II diabetes over 6 years from diagnosis. Diabetologia. 2001;44(2):156–163. doi: 10.1007/s001250051594. [DOI] [PubMed] [Google Scholar]
- 2.Turner RC, Millns H, Neil HA, Stratton IM, Manley SE, Matthews DR, Holman RR. Risk factors for coronary artery disease in non-insulin dependent diabetes mellitus: United Kingdom Prospective Diabetes Study (UKPDS: 23) Bmj. 1998;316(7134):823–828. doi: 10.1136/bmj.316.7134.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stamler J, Vaccaro O, Neaton JD, Wentworth D. Diabetes, other risk factors, and 12-yr cardiovascular mortality for men screened in the Multiple Risk Factor Intervention Trial. Diabetes Care. 1993;16(2):434–444. doi: 10.2337/diacare.16.2.434. [DOI] [PubMed] [Google Scholar]
- 4.Hovind P, Tarnow L, Rossing P, Jensen BR, Graae M, Torp I, Binder C, Parving HH. Predictors for the development of microalbuminuria and macroalbuminuria in patients with type 1 diabetes: inception cohort study. Bmj. 2004;328(7448):1105. doi: 10.1136/bmj.38070.450891.FE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Adler AI, Stratton IM, Neil HA, Yudkin JS, Matthews DR, Cull CA, Wright AD, Turner RC, Holman RR. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. Bmj. 2000;321(7258):412–419. doi: 10.1136/bmj.321.7258.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hypertension in Diabetes Study (HDS): II. Increased risk of cardiovascular complications in hypertensive type 2 diabetic patients. J Hypertens. 1993;11(3):319–325. doi: 10.1097/00004872-199303000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Patel A. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus (the ADVANCE trial): a randomised controlled trial. The Lancet. 2007;370(9590):829–840. doi: 10.1016/S0140-6736(07)61303-8. [DOI] [PubMed] [Google Scholar]
- 8.Hansson L, Zanchetti A, Carruthers SG, Dahlof B, Elmfeldt D, Julius S, Menard J, Rahn KH, Wedel H, Westerling S. Effects of intensive blood-pressure lowering and low-dose aspirin in patients with hypertension: principal results of the Hypertension Optimal Treatment (HOT) randomised trial. HOT Study Group. Lancet. 1998;351(9118):1755–1762. doi: 10.1016/s0140-6736(98)04311-6. [DOI] [PubMed] [Google Scholar]
- 9.Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. UK Prospective Diabetes Study Group. Bmj. 1998;317(7160):703–713. [PMC free article] [PubMed] [Google Scholar]
- 10.Matthews DR, Stratton IM, Aldington SJ, Holman RR, Kohner EM. Risks of progression of retinopathy and vision loss related to tight blood pressure control in type 2 diabetes mellitus: UKPDS 69. Arch Ophthalmol. 2004;122(11):1631–1640. doi: 10.1001/archopht.122.11.1631. [DOI] [PubMed] [Google Scholar]
- 11.Schrier RW, Estacio RO, Esler A, Mehler P. Effects of aggressive blood pressure control in normotensive type 2 diabetic patients on albuminuria, retinopathy and strokes. Kidney Int. 2002;61(3):1086–1097. doi: 10.1046/j.1523-1755.2002.00213.x. [DOI] [PubMed] [Google Scholar]
- 12.Curb JD, Pressel SL, Cutler JA, Savage PJ, Applegate WB, Black H, Camel G, Davis BR, Frost PH, Gonzalez N, Guthrie G, Oberman A, Rutan GH, Stamler J. Effect of diuretic-based antihypertensive treatment on cardiovascular disease risk in older diabetic patients with isolated systolic hypertension. Systolic Hypertension in the Elderly Program Cooperative Research Group. Jama. 1996;276(23):1886–1892. [PubMed] [Google Scholar]
- 13.Cost effectiveness analysis of improved blood pressure control in hypertensive patients with type 2 diabetes: UKPDS 40. UK Prospective Diabetes Study Group. Bmj. 1998;317(7160):720–726. [PMC free article] [PubMed] [Google Scholar]
- 14.Cost-effectiveness of intensive glycemic control, intensified hypertension control, and serum cholesterol level reduction for type 2 diabetes. Jama. 2002;287(19):2542–2551. doi: 10.1001/jama.287.19.2542. [DOI] [PubMed] [Google Scholar]
- 15.Resnick HE, Foster GL, Bardsley J, Ratner RE. Achievement of American Diabetes Association clinical practice recommendations among U.S. adults with diabetes, 1999–2002: the National Health and Nutrition Examination Survey. Diabetes Care. 2006;29(3):531–537. doi: 10.2337/diacare.29.03.06.dc05-1254. [DOI] [PubMed] [Google Scholar]
- 16.Saaddine JB, Engelgau MM, Beckles GL, Gregg EW, Thompson TJ, Narayan KM. A diabetes report card for the United States: quality of care in the 1990s. Ann Intern Med. 2002;136(8):565–574. doi: 10.7326/0003-4819-136-8-200204160-00005. [DOI] [PubMed] [Google Scholar]
- 17.Grant RW, Buse JB, Meigs JB. Quality of diabetes care in U.S. academic medical centers: low rates of medical regimen change. Diabetes Care. 2005;28(2):337–442. doi: 10.2337/diacare.28.2.337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jones DW, Hall JE. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure and evidence from new hypertension trials. Hypertension. 2004;43(1):1–3. doi: 10.1161/01.HYP.0000110061.06674.ca. [DOI] [PubMed] [Google Scholar]
- 19.Berlowitz DR, Ash AS, Hickey EC, Friedman RH, Glickman M, Kader B, Moskowitz MA. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339(27):1957–1963. doi: 10.1056/NEJM199812313392701. [DOI] [PubMed] [Google Scholar]
- 20.Okonofua EC, Simpson KN, Jesri A, Rehman SU, Durkalski VL, Egan BM. Therapeutic inertia is an impediment to achieving the Healthy People 2010 blood pressure control goals. Hypertension. 2006;47(3):345–351. doi: 10.1161/01.HYP.0000200702.76436.4b. [DOI] [PubMed] [Google Scholar]
- 21.Lichtenstein MJ, Sweetnam PM, Elwood PC. Visit frequency for controlled essential hypertension: general practitioners’ opinions. J Fam Pract. 1986;23(4):331–336. [PubMed] [Google Scholar]
- 22.Lichtenstein MJ, Steele MA, Hoehn TP, Bulpitt CJ, Coles EC. Visit frequency for essential hypertension: observed associations. J Fam Pract. 1989;28(6):667–672. [PubMed] [Google Scholar]
- 23.Guthmann R, Davis N, Brown M, Elizondo J. Visit frequency and hypertension. J Clin Hypertens (Greenwich) 2005;7(6):327–332. doi: 10.1111/j.1524-6175.2005.04371.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parchman ML, Bisonni RS, Lawler FH. Hypertension management: relationship between visit interval and control. Fam Pract Res J. 1993;13(3):225–231. [PubMed] [Google Scholar]
- 25.The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1997;157(21):2413–2446. doi: 10.1001/archinte.157.21.2413. [DOI] [PubMed] [Google Scholar]
- 26.Turchin A, Kohane IS, Pendergrass ML. Identification of patients with diabetes from the text of physician notes in the electronic medical record. Diabetes Care. 2005;28(7):1794–1795. doi: 10.2337/diacare.28.7.1794. [DOI] [PubMed] [Google Scholar]
- 27.Turchin A, Shubina M, Breydo E, Pendergrass ML, Einbinder JS. Comparison of information content of structured and narrative text data sources on the example of medication intensification. J Am Med Inform Assoc. 2009;16(3):362–370. doi: 10.1197/jamia.M2777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Turchin A, Shubina M, Chodos AH, Einbinder JS, Pendergrass ML. Effect of board certification on antihypertensive treatment intensification in patients with diabetes mellitus. Circulation. 2008;117(5):623–628. doi: 10.1161/CIRCULATIONAHA.107.733949. [DOI] [PubMed] [Google Scholar]
- 29.Turchin A, Kolatkar NS, Grant RW, Makhni EC, Pendergrass ML, Einbinder JS. Using regular expressions to abstract blood pressure and treatment intensification information from the text of physician notes. J Am Med Inform Assoc. 2006;13(6):691–695. doi: 10.1197/jamia.M2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lin DY. Cox regression analysis of multivariate failure time data: the marginal approach. Stat Med. 1994;13(21):2233–2247. doi: 10.1002/sim.4780132105. [DOI] [PubMed] [Google Scholar]
- 31.Greenland S. Principles of multilevel modelling. Int J Epidemiol. 2000;29(1):158–167. doi: 10.1093/ije/29.1.158. [DOI] [PubMed] [Google Scholar]
- 32.Berlowitz DR, Ash AS, Hickey EC, Glickman M, Friedman R, Kader B. Hypertension management in patients with diabetes: the need for more aggressive therapy. Diabetes Care. 2003;26(2):355–359. doi: 10.2337/diacare.26.2.355. [DOI] [PubMed] [Google Scholar]
- 33.Chapko MK, Fisher ES, Welch HG. When should this patient be seen again? Eff Clin Pract. 1999;2(1):37–43. [PubMed] [Google Scholar]
- 34.Ward MM. Rheumatology visit frequency and changes in functional disability and pain in patients with rheumatoid arthritis. J Rheumatol. 1997;24(1):35–42. [PubMed] [Google Scholar]
- 35.Julius S, Kjeldsen SE, Weber M, Brunner HR, Ekman S, Hansson L, Hua T, Laragh J, McInnes GT, Mitchell L. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. The Lancet. 2004;363(9426):2022–2031. doi: 10.1016/S0140-6736(04)16451-9. [DOI] [PubMed] [Google Scholar]
- 36.Sleight P, Redon J, Verdecchia P, Mancia G, Gao P, Fagard R, Schumacher H, Weber M, Bohm M, Williams B, Pogue J, Koon T, Yusuf S. Prognostic value of blood pressure in patients with high vascular risk in the Ongoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial study. J Hypertens. 2009;27(7):1360–1369. doi: 10.1097/HJH.0b013e32832d7370. [DOI] [PubMed] [Google Scholar]
- 37.Patel NC, Crismon ML, Miller AL, Johnsrud MT. Drug adherence: effects of decreased visit frequency on adherence to clozapine therapy. Pharmacotherapy. 2005;25(9):1242–1247. doi: 10.1592/phco.2005.25.9.1242. [DOI] [PubMed] [Google Scholar]
- 38.Plantinga LC, Fink NE, Sadler JH, Levey AS, Levin NW, Rubin HR, Coresh J, Klag MJ, Powe NR. Frequency of patient-physician contact and patient outcomes in hemodialysis care. J Am Soc Nephrol. 2004;15(1):210–218. doi: 10.1097/01.asn.0000106101.48237.9d. [DOI] [PubMed] [Google Scholar]
- 39.Schwartz LM, Woloshin S, Wasson JH, Renfrew RA, Welch HG. Setting the revisit interval in primary care. J Gen Intern Med. 1999;14(4):230–235. doi: 10.1046/j.1525-1497.1999.00322.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.DeSalvo KB, Bowdish BE, Alper AS, Grossman DM, Merrill WW. Physician practice variation in assignment of return interval. Arch Intern Med. 2000;160(2):205–208. doi: 10.1001/archinte.160.2.205. [DOI] [PubMed] [Google Scholar]
- 41.Hauer KE, Durning SJ, Kernan WN, Fagan MJ, Mintz M, O’Sullivan PS, Battistone M, DeFer T, Elnicki M, Harrell H, Reddy S, Boscardin CK, Schwartz MD. Factors associated with medical students’ career choices regarding internal medicine. Jama. 2008;300(10):1154–1164. doi: 10.1001/jama.300.10.1154. [DOI] [PubMed] [Google Scholar]
- 42.Bodenheimer T. Primary care--will it survive? N Engl J Med. 2006;355(9):861–864. doi: 10.1056/NEJMp068155. [DOI] [PubMed] [Google Scholar]
- 43.Ostbye T, Yarnall KS, Krause KM, Pollak KI, Gradison M, Michener JL. Is there time for management of patients with chronic diseases in primary care? Ann Fam Med. 2005;3(3):209–214. doi: 10.1370/afm.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wick A, Koller MT. Views of patients and physicians on follow-up visits. Swiss Medical Weekly. 2005;135:139–144. doi: 10.4414/smw.2005.10871. [DOI] [PubMed] [Google Scholar]
- 45.Okie S. Innovation in primary care--staying one step ahead of burnout. N Engl J Med. 2008;359(22):2305–2309. doi: 10.1056/NEJMp0805759. [DOI] [PubMed] [Google Scholar]
- 46.Lee TH, Bodenheimer T, Goroll AH, Starfield B, Treadway K. Perspective roundtable: redesigning primary care. N Engl J Med. 2008;359(20):e24. doi: 10.1056/NEJMp0809050. [DOI] [PubMed] [Google Scholar]
- 47.New JP, Mason JM, Freemantle N, Teasdale S, Wong LM, Bruce NJ, Burns JA, Gibson JM. Specialist nurse-led intervention to treat and control hypertension and hyperlipidemia in diabetes (SPLINT): a randomized controlled trial. Diabetes Care. 2003;26(8):2250–2255. doi: 10.2337/diacare.26.8.2250. [DOI] [PubMed] [Google Scholar]
- 48.Taylor CB, Miller NH, Reilly KR, Greenwald G, Cunning D, Deeter A, Abascal L. Evaluation of a nurse-care management system to improve outcomes in patients with complicated diabetes. Diabetes Care. 2003;26(4):1058–1063. doi: 10.2337/diacare.26.4.1058. [DOI] [PubMed] [Google Scholar]
- 49.Denver EA, Barnard M, Woolfson RG, Earle KA. Management of uncontrolled hypertension in a nurse-led clinic compared with conventional care for patients with type 2 diabetes. Diabetes Care. 2003;26(8):2256–2260. doi: 10.2337/diacare.26.8.2256. [DOI] [PubMed] [Google Scholar]
- 50.Schectman G, Barnas G, Laud P, Cantwell L, Horton M, Zarling EJ. Prolonging the return visit interval in primary care. Am J Med. 2005;118(4):393–399. doi: 10.1016/j.amjmed.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 51.Linder JA, Rigotti NA, Schneider LI, Kelley JH, Brawarsky P, Haas JS. An electronic health record-based intervention to improve tobacco treatment in primary care: a cluster-randomized controlled trial. Arch Intern Med. 2009;169(8):781–787. doi: 10.1001/archinternmed.2009.53. [DOI] [PMC free article] [PubMed] [Google Scholar]