Abstract
Purpose
Observation care is used to evaluate patients prior to admission or discharge. Often beneficial, such care also imposes greater financial liability on Medicare beneficiaries. While the use of observation care has increased recently, critical access hospitals (CAHs) face different policies than prospective payment (PPS) hospitals, which may influence their observation care use.
Methods
We used 100% Medicare inpatient and outpatient claims files and enrollment data for years 2007 to 2009, and the 2007 American Hospital Association data to compare trends in the likelihood, prevalence and duration of observation stays between CAHs and PPS hospitals in metro and non-metro areas among fee-for-service Medicare beneficiaries over age 65.
Findings
While PPS hospitals are more likely to provide any observation care, the 3-year increase in the proportion of CAHs providing any observation care is approximately 5 times as great as the increase among PPS hospitals. Among hospitals providing any observation care in 2007, the prevalence at CAHs was 35.7% higher than at non-metro PPS hospitals and 72.8% higher than at metro PPS hospitals. By 2009, these respective figures had increased to 63.1% and 111%. Average stay duration increased more slowly for CAHs than for PPS hospitals.
Conclusions
These data suggest that a growing proportion of CAHs are providing observation care and that CAHs provide relatively more observation care than PPS hospitals, but they have shorter average stays. This may have important financial implications for Medicare beneficiaries.
Keywords: Critical Access Hospital, elderly, Medicare, observation care, rural
Following initial presentation in the emergency department, observation care is designed to provide a temporary transition period prior to admission or discharge. While the appropriate use of observation care can reduce costs and improve quality, inappropriate use of observation care may reduce quality and impose greater financial liability on Medicare beneficiaries.1,2 For example, although they may spend 1 or more nights in the hospital, patients receiving observation care are classified as outpatients, and they are responsible for paying 20% coinsurance, which they would not pay as inpatients.
Reports that hospitals are increasingly substituting observation care for short stay admissions to avoid being penalized by the Medicare Recovery Audit Contractor (RAC) Program have led the Department of Health and Human Services to investigate observation care as part of its 2012 work plan.3 Indeed, both the prevalence and duration of observation care have increased nationally in recent years with substantial variation across states, hospital referral regions, and hospitals.4 This variation appears to be driven in part by critical access hospitals (CAHs), which, according to one cross-sectional study, are less likely than other hospitals to provide any observation care, but which have a higher prevalence and shorter average duration of observation stays than other hospitals if they do provide such care.5
While most hospitals shifted to the Medicare Prospective Payment System (PPS), the Balanced Budget Act of 1997 established the CAH program to support small, mostly rural hospitals via cost-based reimbursement. CAH designation criteria include being at least 35 miles from another hospital (or being certified by the state as a necessary provider), having no more than 25 inpatient beds, and providing 24-hour emergency care.6
CAHs are also subject to unique rules regarding observation stays. They may maintain “observation only” beds, which do not count towards their 25-bed maximum, and they must limit the duration of observation stays to 48 hours or less to prevent observation care from being substituted for inpatient admissions.7,8 Importantly, CAHs are reimbursed for every hour of observation care they provide, whereas PPS hospitals are only reimbursed separately for observation stays of at least 8 hours duration.9
CAHs are particularly sensitive to Medicare reimbursement policy because of their small size, and these payment and regulatory differences are likely to influence their use of observation care.10–12 However, the extent to which this occurs is unknown. Moreover, it is unclear whether the same trends of increasing prevalence and duration of observation stays observed nationally are occurring in the subset of CAHs. Therefore, this study examines the likelihood, prevalence and duration of observation care from 2007 to 2009 and compares trends among CAHs to trends among other short-term general PPS hospitals in both metro and non-metro areas.
METHODS
Data Sources and Sample
We used years 2007 through 2009 of the 100% Medicare Part A inpatient and Part B outpatient claims files (for institutional providers) and the Medicare enrollment file to identify the prevalence and duration of hospital observation stays among all fee-for-service Medicare beneficiaries over age 65. We identified all short-term general hospitals as CAHs or PPS hospitals using 2007 American Hospital Association data and further classified each hospital as being located in a metro or non-metro area on the basis of rural-urban continuum codes. We did this to ensure that any rural-urban differences in observation care within hospital type could be identified. We report results at the hospital level for approximately 4,300 hospitals annually as shown in Table 1. Excluded from our sample are 190 observations (117 CAH, 73 PPS) over the 3-year period for hospitals with fewer than 25 Medicare admissions annually, which produced outliers among our outcomes of interest. Because they are qualitatively different from the majority of CAHs, we also exclude from our analysis all CAHs located in metro areas, representing a total of 621 observations over the 3-year period.
Table 1.
Study Sample by Critical Access Hospital (CAH) Status, 2007 – 2009
| Year | CAH | Non-CAH | Total Hospitals | |
|---|---|---|---|---|
| Metro | Non-Metro | |||
| 2007 | 1020 (23.6%) | 2319 (53.7%) | 983 (22.7%) | 4,322 |
| 2008 | 1015 (23.7%) | 2300 (53.7%) | 971 (22.7%) | 4,286 |
| 2009 | 1010 (23.8%) | 2277 (53.6%) | 961 (22.6%) | 4,248 |
Measures
Using the Medicare claims data described above, we derived measures of observation care prevalence and duration. For each hospital, we defined observation care prevalence as the annual number of observation stays per 1,000 inpatient admissions, and observation stay duration as the average hours per stay.
Analysis
Using the Medicare Part B outpatient claims, we identified individual observation stays at the beneficiary level using both revenue center codes and Healthcare Common Procedure Coding System classifications. The hours of observation care, available in the “service units” field, were also counted. We then identified inpatient admissions at the beneficiary level using the Medicare Part A inpatient claims. We merged both the inpatient and outpatient files with the Medicare enrollment file, which contains demographic data on beneficiaries, and excluded all beneficiaries under age 65. We focused on this population because it is the most at risk of adverse consequences, including high out-of-pocket costs, arising from frequent and extended observation stays. By contrast, the under-65 disabled population has a higher likelihood of being dually eligible for Medicare and Medicaid, which would shield them from these costs.
Next, we aggregated these annual measures to the hospital level. Finally, we constructed our outcome measures by standardizing each hospital's total annual number of observation stays for every 1,000 inpatient admissions and calculating each hospital's average observation stay duration by summing total hours of observation care and dividing that figure by the total number of stays. Additionally, we constructed 2 binary variables to further distinguish prevalence and duration. These indicated whether or not a hospital provided any observation care during the calendar year, and whether or not a hospital's mean observation stay duration was greater than 24 hours. These data and the derivation of our outcomes of interest have been previously described in more detail.4
RESULTS
As shown in Table 1, our sample includes all short-term general hospitals with at least 25 annual inpatient admissions, stratified by critical access hospital status and metro/non-metro location for PPS hospitals. Nearly 1 out of every 4 hospitals in our nationally representative sample is a CAH. The total number of hospitals decreased by 1.7% over the study period due to consolidations and closures. However, both CAHs and PPS hospitals were affected equally, leading the composition of the sample by hospital type relatively unchanged.
As shown in Figure 1, the proportion of both CAHs and PPS hospitals providing at least some observation care increased every year during the study period. While the proportion of PPS hospitals providing any observation care in 2007 was nearly 3 times the proportion of CAHs providing any such care that same year, CAHs have quickly narrowed the gap. From 2007 to 2009, the proportion of CAHs providing any observation care increased by 19.1 percentage points, compared to just a 3.4 percentage point increase in the proportion among PPS hospitals in non-metro areas, and a 4.0 percentage point increase among PPS hospitals in metro areas.
Figure 1.
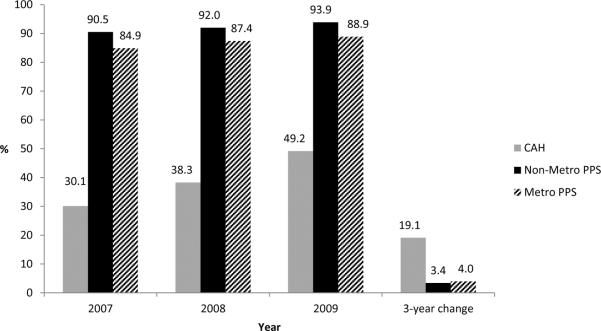
Proportion of Hospitals Providing Any Observation Care, by Critical Access Status, 2007 – 2009
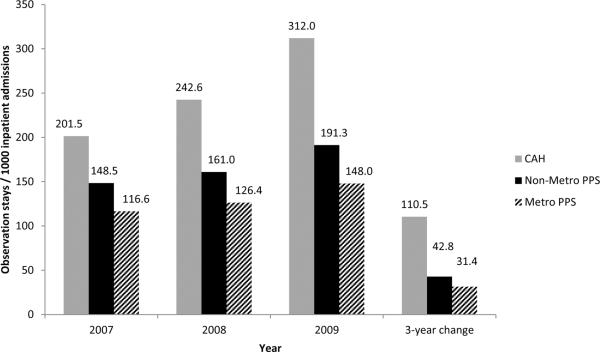
While CAHs are less likely than either metro or non-metro PPS hospitals to provide observation care, a different trend emerges regarding the prevalence of observation stays among hospitals providing any observation care. As shown in Figure 2, CAHs provide a significantly higher volume of observation care relative to inpatient admissions, and the gap has been growing over time. At CAHs, the prevalence of observation stays increased by nearly 55% in just 3 years, compared to a 28.8% increase in prevalence among non-metro PPS hospitals, and a 26.9% increase in prevalence among metro PPS hospitals. In 2007, the prevalence of observation care at CAHs was 35.7% higher than the prevalence at non-metro PPS hospitals and 72.8% higher than the prevalence at metro PPS hospitals. By 2009, these respective figures had increased to 63.1% and 110.8%. In short, while many more PPS hospitals provide observation care, the CAHs that do provide such care are providing it at 1.6 to 2.1 times the rate of their PPS hospital peers depending on metro and non-metro location.
Figure 2.
Hospital Prevalence of Observation Care Conditional on Providing Any, by Critical Access Status, 2007 – 2009
Multiplying the proportion of hospitals providing any observation care and the prevalence of observation care conditional on the hospital providing any observation care, yields the unconditional prevalence of observation stays for each hospital type. The unconditional prevalence among CAHs has risen from 60.7 per 1,000 admissions in 2007 to 153.5 per 1,000 admissions in 2009. By comparison, the unconditional prevalence among non-metro PPS hospitals has risen from 134.4 per 1,000 admissions in 2007 to 179.6 per 1,000 admissions in 2009, while for metro PPS hospitals the unconditional prevalence went from 98.9 to 131.6. In just 3 years, the unconditional prevalence of observation care at CAHs has surpassed the unconditional prevalence of observation care at metro PPS hospitals, and it is rapidly closing in on non-metro PPS hospitals.
Across the study period, the average duration of observation stays is approximately 5 hours shorter in CAHs compared to PPS hospitals. Both CAHs and PPS hospitals have seen an increase in observation stay duration. From 2007 to 2009, the average duration of observation stays at CAHs increased from 19.9 hours to 21.4 hours. By comparison, the average duration of observation stays at PPS hospitals increased from 24.5 hours to 26.7 hours over the same time period. Among PPS hospitals in non-metro areas, the average stay went from 23.4 hours to 25.5 hours, while for PPS hospitals in metro areas it went from 24.9 hours to 27.2 hours.
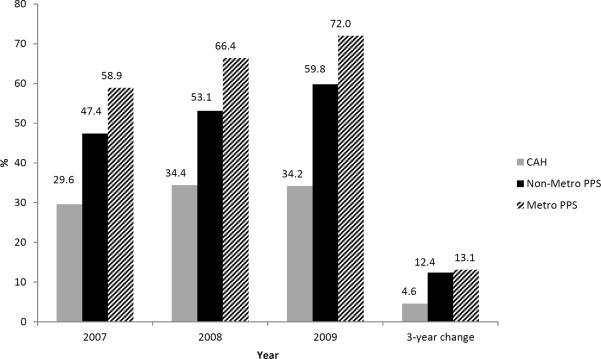
The data in Figure 3 examine stays in excess of 24 hours, which are particularly concerning as they are recognized as being inefficient for hospitals and burdensome for patients.1,2 In 3 years, the proportion of CAHs with an average observation stay length greater than 24 hours has grown by just 4.6 percentage points (29.6% to 34.2%), compared to 12.4 percentage points among non-metro PPS hospitals (47.4% to 59.8%) and 13.1 percentage points among metro PPS hospitals (58.9% to 72.0%). Moreover, while 6 or 7 of every 10 PPS hospitals have average observation stays in excess of 24 hours duration depending on metro location, the trend among CAHs actually declined slightly from 2008 to 2009.
Figure 3.
Proportion of Hospitals with Average Observation Stay Greater than 24 Hours, by Critical Access Status, 2007 – 2009
DISCUSSION
These trend data suggest that a growing proportion of CAHs are choosing to provide observation care and that CAHs provide relatively more observation care than other short-term general hospitals, although they have shorter stays on average. While this is consistent with prior findings that CAHs derive a greater share of their revenue from outpatient care,10–12 we believe that the reimbursement each hospital type receives and the length of stay policy for CAHs may also contribute to these trends.
CAHs receive cost-based reimbursement for every hour of observation care they provide, beginning with the first hour. In addition, they are reimbursed at 101% of costs regardless of whether patients placed under observation are subsequently admitted or discharged. Consequently, CAHs have an incentive to place patients under observation to generate additional revenue, given that the threshold which triggers reimbursement is not as high. Moreover, if they subsequently admit an observation patient, they are still able to bill everything separately on a cost basis. This may explain the higher prevalence of observation stays observed at CAHs. The lower mean duration of observation stays at CAHs could be the result of the strict 48-hour time limit they face. Indeed, it appears that this policy is having the intended effect of reducing particularly lengthy stays at CAHs (as measured by average stays in excess of 24 hours).
By contrast, PPS hospitals are only reimbursed under the PPS with a single payment for observation stays of 8 or more hours. In addition, if a patient held for observation care is subsequently admitted, the outpatient care may fall within the preadmission payment window, meaning that the hospital will receive a single DRG payment and will not receive separate reimbursement for the observation stay or any services provided during that time. Therefore, PPS hospitals will maximize their financial benefits if their observation patients are held for at least, but not more than, 8 hours, and discharged home rather than admitted.2 This may result in more selective utilization of observation care by PPS hospitals, and it may lead them to hold patients under observation longer than necessary to reach the 8 hours required for Medicare reimbursement. This may also explain why the mean duration of observation stays is longer at PPS hospitals than at CAHs. Given that observation stays are intended to be resolved within a day, it is striking that fully 72% of PPS hospitals in metro areas have average stays in excess of 24 hours.
While cost-based reimbursement has effectively sustained small, rural hospitals, there is also evidence that it has made them less efficient than hospitals reimbursed under the PPS.13 In this case, it appears that both hospital types may be operating inefficiently in their provision of observation care as the result of arbitrary cutoffs in Medicare reimbursement policy. Specifically, CAHs have very strong incentives to place patients under observation care, but hold them for a shorter period of time, while PPS hospitals may be more selective in placing patients under observation, but they have very strong incentives to hold them for at least 8 hours. Clinical decision-making should guide the use of observation care, but the trends we observe in these data suggest that payment policy may also play a significant role.
This study has some limitations. For instance, we do not control for patient acuity. Prior studies have shown that high acuity patients are more likely to bypass their local CAH in favor of a more distant, but larger hospital.14 This may mean that patients who are more likely to be admitted are not presenting at the CAH, and it could partially explain why CAHs are providing relatively more observation care (with a lower mean number of hours) than other hospitals. Moreover, our data source precludes us from determining whether the disposition of each observation case was appropriate. We have limited data on the relative use of RAC audits among a sample of CAHs and PPS hospitals. If the increase in the use of observation care was solely related to RAC audits, it would suggest that CAHs are a more likely target for such audits than PPS hospitals. This seems highly unlikely, given that 57.7% of CAHs participating in the American Hospital Association's RACTrac survey report audit activity, compared to 95.9% of participating PPS hospitals reporting audit activity.15
In conclusion, access to observation care appears to be limited at approximately half of CAHs, while being widely utilized at the remaining CAHs. This may have important financial implications for Medicare beneficiaries in these areas as they are responsible for a greater share of their total charges when they are placed under observation rather than admitted. More work is needed, however, to understand what factors lead CAHs to begin providing observation care, as well as to assess the appropriateness of observation care as currently utilized, and the effect of observation stays of extended duration on patients' finances and health outcomes.
Acknowledgments
This work was funded by the Retirement Research Foundation (Grant No. 2011-066), the National Institute on Aging (Grant No. P01AG027296) and the Agency for Healthcare Research and Quality (Grant No. 5T32H000011-27). The Medicare enrollment and claims data used in this analysis were made available through a data use agreement (DUA 21845) authorized by the Centers for Medicare and Medicaid Services.
Footnotes
None of the authors have any disclosures to report.
REFERENCES
- 1.Brillman J, Mathers-Dunbar L, Graff L, et al. Management of observation units. Ann Emerg Med. 1995;25(6):823–830. doi: 10.1016/s0196-0644(95)70215-6. [DOI] [PubMed] [Google Scholar]
- 2.Baugh CW, Venkatesh AK, Bohan JS. Emergency department observation units: a clinical and financial benefit for hospitals. Health Care Manage Rev. 2011;36(1):28–37. doi: 10.1097/HMR.0b013e3181f3c035. [DOI] [PubMed] [Google Scholar]
- 3.Carlson J. Caught in the middle: under tough scrutiny from the CMS over which patients should be admitted for care, hospitals are frustrated—and patients are fighting back. Mod Healthc. 2012;42(May 14):6. [PubMed] [Google Scholar]
- 4.Feng Z, Wright B, Mor V. Sharp rise in Medicare enrollees being held in hospitals for observation raises concerns about causes and consequences. Health Aff (Milwood) 2012;31(6):1251–1259. doi: 10.1377/hlthaff.2012.0129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wright B, Jung HY, Feng Z, Mor V. Hospital characteristics associated with the prevalence and duration of observation care. Under review at Med Care. doi: 10.1111/1475-6773.12166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reif SS, Ricketts TC. The Medicare critical access hospital program: the first year. J Rural Health. 1999;15(1):61–66. doi: 10.1111/j.1748-0361.1999.tb00599.x. [DOI] [PubMed] [Google Scholar]
- 7.Department of Health and Human Services. Centers for Medicare and Medicaid Services CMS Manual System. Pub. 100-07 State Operations. Provider Certification. Transmittal 34. [Accessed August 17, 2012];Revision to Appendix W, “Survey Protocol, Regulations and Interpretive Guidelines for Critical Access Hospitals (CAHs).”. 2008 Apr 4; Available at: http://www.cms.gov/Regulations-and-Guidance/Guidance/Transmittals/downloads/R34SOMA.pdf.
- 8.Hale DK. Observation status: a guide to compliant level of care determinations. Second edition. HCPro, Inc; 2008. [Accessed July 6, 2012]. Available at: http://www.hcmarketplace.com/supplemental/6325_browse.pdf. [Google Scholar]
- 9.Mackaman D. Critical access hospitals: setting the top 10 myths straight. HCPro, Inc; Jun, 2010. [Accessed July 6, 2012]. Available at: http://blogs.hcpro.com/revenuecycleinstitute/wp-content/uploads/2010/07/RCI_SR2510_06_10_web.pdf. [Google Scholar]
- 10.Dalton K, Slifkin RT, Howard HA. The role of critical access hospital status in mitigating the effects of new prospective payment systems under Medicare. J Rural Health. 2000;16(4):357–370. doi: 10.1111/j.1748-0361.2000.tb00486.x. [DOI] [PubMed] [Google Scholar]
- 11.Mohr PE, Franco SJ, Blanchfield BB, Cheng M, Evans WN. Vulnerability of rural hospitals to Medicare outpatient payment reform. Health Care Financ Rev. 1999;21(1):1–18. [PMC free article] [PubMed] [Google Scholar]
- 12.Moscovice I, Stensland J. Rural hospitals: trends, challenges, and a future research and policy analysis agenda. J Rural Health. 2002;18(5):197–210. doi: 10.1111/j.1748-0361.2002.tb00931.x. [DOI] [PubMed] [Google Scholar]
- 13.Rosko MD, Mutter RL. Inefficiency differences between critical access hospitals and prospectively paid rural hospitals. J Health Polit Policy Law. 2010;35(1):95–126. doi: 10.1215/03616878-2009-042. [DOI] [PubMed] [Google Scholar]
- 14.Liu JJ, Bellamy GR, McCormick M. Patient bypass behavior and critical access hospitals: implications for patient retention. J Rural Health. 2007;23(1):17–24. doi: 10.1111/j.1748-0361.2006.00063.x. [DOI] [PubMed] [Google Scholar]
- 15.American Hospital Association Exploring the impact of the RAC program on hospitals nationwide. [Accessed December 4, 2012];Results of AHA RACTrac survey, 3rd quarter 2012. 2012 Nov 30; Available at: http://www.aha.org/content/12/12Q3ractracresults.pdf.