Summary
Background
Research into social inequalities in health has tended to focus on low socioeconomic status in adulthood. We aimed to test the hypothesis that children’s experience of socioeconomic disadvantage is associated with a wide range of health risk factors and outcomes in adult life.
Methods
We studied an unselected cohort of 1000 children (born in New Zealand during 1972–73) who had been assessed at birth and ages 3, 5, 7, 9, 11, 13, and 15 years. At age 26 years, we assessed these individuals for health outcomes including body-mass index, waist:hip ratio, blood pressure, cardiorespiratory fitness, dental caries, plaque scores, gingival bleeding, periodontal disease, major depression, and tobacco and alcohol dependence, and tested for associations between these variables and childhood and adult socioeconomic status.
Findings
Compared with those from high socioeconomic status backgrounds, children who grew up in low socioeconomic status families had poorer cardiovascular health. Significant differences were also found on all dental health measures, with a threefold increase in adult periodontal disease (31·1% vs 11·9%) and caries level (32·2% vs 9·9%) in low versus high childhood socioeconomic status groups. Substance abuse resulting in clinical dependence was related in a similar way to childhood socioeconomic status (eg, 21·5% vs 12·1% for adult alcohol dependence). The longitudinal associations could not be attributed to life-course continuity of low socioeconomic status, and upward mobility did not mitigate or reverse the adverse effects of low childhood socioeconomic status on adult health.
Interpretation
Protecting children against the effects of socioeconomic adversity could reduce the burden of disease experienced by adults. These findings provide strong impetus for policy makers, practitioners, and researchers to direct energy and resources towards childhood as a way of improving population health.
Introduction
Research into social inequalities and health has tended to focus on low socioeconomic status in adulthood as the main causal variable, cardiovascular disease as the main outcome variable, adults’ stress experiences as the main mediating mechanism, and redistribution of income among adult workers as the solution.1,2 Previous research documenting significant but modest correlations between measures of low childhood socioeconomic status and adult health3–6 has been interpreted as suggesting that the experience of disadvantage during childhood could have small—albeit long-lasting and harmful—effects on adult health. However, several gaps in the evidence base challenge this interpretation.
First, because measurement of childhood socioeconomic status has not been ideal, previous research might have actually underestimated the long-term effect of childhood experiences. Most studies rely on adults’ retrospective reports about their childhood circumstances,7–9 but there is evidence that such reports are compromised by poor recall and measurement error.10 Additionally, most studies measure childhood circumstances by using retrospective reports about a single age (eg, when the child was 14 years old) or about short durations during childhood. Limited-duration information is an unreliable indicator of, and weak proxy for, more complete information spanning the entire childhood period.11 We aimed to use prospective, repeated measures of socioeconomic status to quantify the degree of socioeconomic disadvantage experienced throughout childhood to examine its relation to adult health.
Second, to ascertain whether children’s experience of disadvantage with respect to socioeconomic status is related to their adult health, the child’s initial infant health status should be controlled for. Children from families of low socioeconomic status are more likely to begin life in poor health because fetal and birth complications are more prevalent in the lower socioeconomic strata.12,13 Poor newborn health is known to have continuity to adult health.14 In this study, we aimed to control for perinatal health before assessing the association between childhood socioeconomic status and adult health.
Third, to ascertain whether the experience of disadvantage with respect to socioeconomic status during childhood is related to adult health, adult socioeconomic status also needs to be controlled for, since there is moderate continuity of socioeconomic status across the life course.15 A statistical association between childhood socioeconomic status and adult health could therefore be mistaken as evidence for a childhood effect, whereas it might simply represent concurrent effects of adult socioeconomic status on adult health.16,17 We planned to examine the influence of life-course continuity in socioeconomic status, before assessing the effects of childhood socioeconomic status on adult health.
Fourth, if there is an association between childhood socioeconomic status and adult health, it is important to test whether changes in socioeconomic circumstances after childhood can counteract the effects of childhood socioeconomic status. According to the upward mobility hypothesis, a rise in socioeconomic status from childhood to adulthood could have a protective effect and lead to better health. The downward mobility hypothesis predicts that a fall in the socioeconomic status hierarchy could have a risk effect and lead to worse health. By contrast, according to the social-origins hypothesis, growing up in conditions of low socioeconomic status has enduring adverse influences on adult health, irrespective of adult socioeconomic status. We aimed to test these three life-course hypotheses in this study.
Finally, it is important to establish whether the association between childhood socioeconomic status and adult health is pervasive across health domains or is domain specific. Knowledge about the pervasiveness versus specificity of these longitudinal associations can help to focus attention on plausible risk mechanisms. We intended to examine the association between low childhood socioeconomic status and a wide range of adult health outcomes—including physical health, dental health, and mental health and substance abuse—that are known to impair life functioning and that signal risk for future disease.
Methods
Sample
Participants were members of the Dunedin Multidisciplinary Health and Development Study—a longitudinal investigation of health and behaviour in a complete birth cohort.18 The study members were born in Dunedin, New Zealand, between April, 1972, and March, 1973. Of these individuals, 1037 (91% of eligible births; 52% male) participated in the first follow-up assessment at age 3 years, which constituted the base sample for the remainder of the study. Cohort families represented the full range of socioeconomic status in the general population of New Zealand’s South Island and were mainly white. Follow-ups were done at ages 5, 7, 9, 11, 13, 15, 18, 21, and most recently at age 26 years when we assessed 980 (96%) of the 1019 study members still alive.
Participants attended the research unit within 60 days of their birthday for a full day of individual data collection. The unit reimbursed study members’ costs to remove all barriers to their participation—eg, travel, lost wages, child care. The various assessments (eg, dental examination, psychiatric interview) were presented as standardised modules in counterbalanced order, each administered by a different examiner who was unaware of responses given in other assessments.
The Research Ethics Committee of the Otago Hospital Board granted ethics approval for each phase of this longitudinal study. Study members gave informed consent before participating.
Socioeconomic circumstances in childhood and adulthood
The socioeconomic status of the study members’ families was measured with a six-point scale which assessed parents’ self-reported occupational status.19 The scale places each occupation into one of six categories (6=unskilled labourer, 1=professional) on the basis of the educational levels and income associated with that occupation in data from the New Zealand census.
The variable used in our analyses, childhood socioeconomic status, is the average of the highest socioeconomic status level of either parent, assessed repeatedly at the study member’s birth and at ages 3, 5, 7, 9, 11, 13, and 15 years. Measurement of socioeconomic status at a single point early in the life-course does not capture cumulative exposure to low socioeconomic status, because there is some socioeconomic status change within childhood; for example, the correlation between socioeconomic status at birth and age 15 years was r=0·5. The variable of childhood socioeconomic status thus reflects the socioeconomic conditions experienced by the study members while they grew up. Study members were designated as growing up in families whose mean socioeconomic status was low (groups 6 and 5—eg, oyster canner, car painter), medium (groups 4 and 3—eg, butcher, secretary), or high (groups 2 and 1—eg, architect, dentist).
Adult socioeconomic status was the status of the study member’s current adult occupation (both men and women), assessed during the age-26 interview. Study members were similarly designated into having occupations with low, medium, or high socioeconomic status. Homemakers and students were excluded from analyses.
Infant health
The infant health index used in this study consisted of the sum of the following complications: maternal diabetes; glycosuria; epilepsy; hypertension; eclampsia; antepartum haemorrhage; accidental haemorrhage; placenta praevia; previous small baby; gestational age less than 37 weeks or more than 41 weeks; birthweight less than 2·5 kg or more than 4 kg; either small (<10th percentile) or large (>90th percentile) for gestational age; low Apgar score at birth; hypoxia at birth (idiopathic respiratory distress syndrome or apnoea); major or minor neurological signs; rhesus incompatibility; ABO incompatibility; and non-haemolytic hyperbilirubinaemia.
In this paper, all analyses that assess the association between low childhood socioeconomic status and adult health control for infant health, because Dunedin children who grew up in families of low socioeconomic status were significantly more likely to have had compromised health at birth (proportion that experienced one or more birth complications: low childhood socioeconomic status 52%, medium socioeconomic status 46%, and high socioeconomic status 37%; p=0·01).
Adult physical health
Examinations at age 26 years were done by health professionals with either a medical or nursing degree. Height was measured to the nearest mm with a portable Harpenden stadiometer. Weight was recorded to the nearest 0·1 kg with calibrated scales (Tanita, model number 1609N; Tokyo, Japan). Measurements were repeated and the average used to calculate body-mass index. Girths were measured using a steel tape, calibrated in centimetres with millimetre gradations. Waist girth was the perimeter at the level of the noticeable waist narrowing located between the costal border and the iliac crest. Hip girth was taken as the perimeter at the level of the greatest protuberance and at about the symphysion pubic level anteriorly. Measurements were repeated and the average used to calculate waist:hip ratio.
Blood pressure was assessed according to standard protocols with a Hawksley random-zero sphygmomanometer with a constant deflation valve. Cuffs were chosen on the basis of the circumference of an individual’s arm. Study members were seated in a quiet room with their right arm resting at heart level. A 5-min rest period preceded the first measurement, followed by two further measures 5 min apart. Systolic blood pressure values were averaged across the three measurement occasions. The assessment of cardiorespiratory fitness required study members to complete a submaximum exercise test on a friction-braked cycle ergometer (Monark, Sweden). Dependent on the extent to which heart rate increased during a 2-min 50 W warm-up, the workload was adjusted to elicit a steady heart-rate in the range 130–170 beats per minute. After a further 6-min constant power output stage, the maximum heart rate was recorded and used to calculate predicted maximum oxygen uptake (VO2max) according to standard protocols.
Study members who indicated that they were pregnant were excluded from analyses involving adult physical health outcomes.
Adult dental health
Examinations at age 26 years were done by calibrated dental examiners. Tooth cleanliness was assessed with the simplified oral hygiene index.20 Periodontal measurements were made in two quadrants by standard procedures.21 Gingival bleeding was assessed for each tooth (excluding third molars) by determination of the presence or absence of blood at any of the three probing sites 10 s after probing, and recorded as the number of sites that bled, expressed as a percentage of total sites. Loss of periodontal attachment for each site was calculated by summation of the measurements for gingival recession and probing depth. Periodontal disease was judged present if there was more than 4 mm loss of periodontal attachment for at least one site. Dental caries was measured with the decayed missing filled surfaces scale and its components. Because this measure was very skewed, study members were categorised into those who had fewer than four and those who had four or more surfaces affected (top 20% of the sample).
Adult mental health and substance use
These variables were assessed at age 26 years with the diagnostic interview schedule, administered by health professionals with either a medical or clinical masters degree. The reporting period was 12 months before interview. Here we report on study members who met criteria for a major depressive episode, alcohol dependence, and tobacco dependence according to the fourth edition of the diagnostic and statistical manual of mental disorders (DSM-IV).22 The essential feature of a major depressive episode is a period of at least 2 weeks during which there is either depressed mood or the loss of interest or pleasure in all activities. One must also experience four of the following additional symptoms: changes in weight, appetite, sleep, or psychomotor activity; decreased energy; feelings of worthlessness or guilt; difficulty thinking or concentrating; or recurrent thoughts of death or suicidal ideation. Lastly, the episode must be accompanied by clinically significant distress or impairment in social, occupational, or other important areas of functioning.
The essential feature of substance dependence (alcohol and tobacco) is a maladaptive pattern of substance use leading to clinically significant impairment or distress, accompanied by symptoms of psychological or physiological dependence. Symptoms of physiological dependence include increased tolerance for the substance or withdrawal symptoms after stopping substance use. Psychological symptoms of dependence include continued use despite harmful effects, difficulties in cutting down, and large amounts of time spent using the substance.
Statistical analysis
Regression analyses were used to test the hypothesis that low childhood socioeconomic status predicts poor adult health. For continuous adult health outcomes (eg, blood pressure), we used ordinary least squares; for dichotomous outcomes (eg, depression), logistic regressions. In each regression model, we estimated the effects of childhood socioeconomic status on adult health, controlling for sex, infant health, and the study member’s own adult socioeconomic status:
where logit (Yi) is the log odds of the dichotomous health outcome Y for individual i; Zj is a set of observed covariates (ie, sex, infant health); X1 and X2 represent the effects of low and medium adult socioeconomic status, respectively; and X3 and X4 represent the effects of growing up in low and in medium childhood socioeconomic status environments, respectively. The contrast group for both adult and childhood socioeconomic status is the high socioeconomic status group; B1 and B2 thus estimate the unique effects of adult socioeconomic status, controlling for childhood experiences, and B3 and B4 estimate the unique effects of childhood socioeconomic status, controlling for contemporaneous socioeconomic experiences in adulthood.
Social mobility was analysed in terms of movement between childhood (ie, their parents’) and adulthood (ie, their own) socioeconomic status. Four socioeconomic trajectories were created from the 3×3 mobility table: persistent low socioeconomic status, in which study members experienced low socioeconomic status childhoods and were also employed in low socioeconomic status adult occupations; upwardly mobile, in which study members experienced low socioeconomic status childhoods but were employed in medium or high socioeconomic status adult occupations; downwardly mobile, in which study members experienced high socioeconomic status childhoods but were employed in medium or low socioeconomic status adult occupations; and persistent high socioeconomic status, in which study members experienced high socioeconomic status childhoods and were also employed in high socioeconomic status adult occupations.
For purposes of the mobility analysis only, we excluded study members who grew up in medium socioeconomic status homes so that we could focus on the effects of social mobility (upward and downward) from the extremes of social-class origins. Predictions derived from each of the three life-course hypotheses (social-origins, upward-mobility, and downward-mobility hypotheses) were tested by use of sets of contrast codes in a multiple regression framework.23 The null hypothesis is that the contrast applied to the group means equals 0, which is tested for significance under the usual assumptions. All mobility analyses were done on means and proportions adjusted for sex and newborn health.
Role of the funding sources
The funding sources had no role in the design of this study; the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit this paper for publication.
Results
All physical health measures at age 26 years, except systolic blood pressure, showed a graded relation with childhood socioeconomic status (table). As socioeconomic status increased, body-mass index and waist:hip ratio decreased and cardiorespiratory fitness increased. The adverse associations with low childhood socioeconomic status remained significant after controlling for infant health, and after adding statistical controls for contemporaneous adult socioeconomic status.
All dental health measures at age 26 years also showed a graded relation with childhood socioeconomic status. As socioeconomic status increased, the amount of plaque and gingival bleeding, and the proportion of individuals with periodontal disease and decayed surfaces, decreased. The adverse influence of low childhood socioeconomic status was seen after controlling for infant health and contemporaneous adult socioeconomic status. Additionally, the results showed that low adult socioeconomic status had a significant effect on poor adult dental health after controlling for low childhood socioeconomic status.
The age-26 mental health and substance abuse measures showed different patterns of association with childhood socioeconomic status than did the physical and dental health measures. Depression at age 26 years was not linked to low childhood socioeconomic status but was significantly associated with contemporaneous adult socioeconomic status. Alcohol and tobacco dependence at age 26 years were weakly linked to low childhood socioeconomic status and were more strongly associated with contemporaneous adult socioeconomic status.
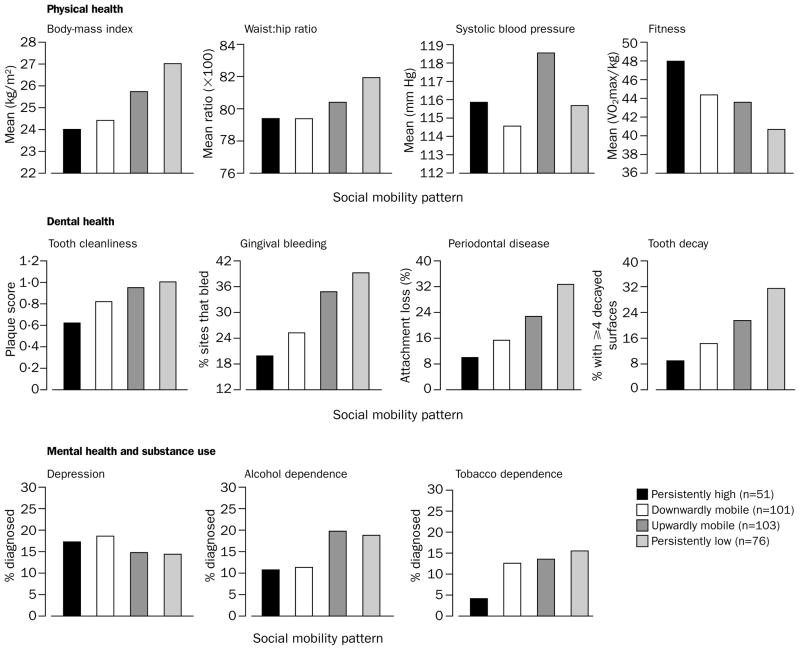
The figure shows variations in health at age 26 years as a function of four different socioeconomic trajectories from childhood to adulthood. If there is a protective effect of upward mobility, adults who rise in the socioeconomic status hierarchy (upwardly mobile) should be in better health than those who remain in low socioeconomic status conditions from childhood to adulthood (persistently low). This hypothesis was supported in relation to only one adult health outcome: upward mobility was associated with low waist:hip ratio (t=2·14, p=0·03). If there is a risk effect of downward mobility, adults who fall in the socioeconomic status hierarchy (downwardly mobile) should be in poorer health than those who remain in high socioeconomic status conditions from childhood to adulthood (persistently high). Significance testing provided some support for this hypothesis: downward mobility was associated with poor cardiorespiratory fitness (t=2·02, p=0·04) and tooth cleanliness (t=2·31, p=0·02). Finally, if the social-origins hypothesis is correct, children who grow up in low-socioeconomic status households should have poorer health in adulthood, relative to children who grow up in high-socioeconomic status homes, regardless of their respective adult socioeconomic status. This hypothesis was supported in relation to body-mass index (t=3·70, p=0·003), waist:hip ratio (t=3·26, p=0·001), systolic blood pressure (t=2·12, p=0·03), poor cardiorespiratory fitness (t=2·64, p=0·009), tooth cleanliness (t=3·42, p=0·0007), gingival bleeding (t=4·48, p<0·0001), periodontal disease (odds ratio 3·05, 95% CI 1·65–5·63), tooth decay (3·79, 1·99–7·22), and alcohol dependence (1·94, 1·05–3·60). It was not supported in relation to depression or tobacco dependence.
Figure. Variations in age-26 health outcomes as a function of four socioeconomic trajectories from childhood to adulthood.
Figure shows means and proportions adjusted for sex and newborn health.
Discussion
This life-course study, spanning the period from birth to age 26 years, shows that low childhood socioeconomic circumstances have long-lasting negative influences on adult health, irrespective of what health cache one begins life with, or where one ends up in the socioeconomic hierarchy as an adult. Specifically, the findings document that the social gradient in health—which has been amply documented among middle-aged and older adults—actually emerges in childhood. Whereas clinical and research interest in the social gradient has been generated mostly by studies of adults, the findings from this study suggest that the social gradient must be scrutinised in paediatric and adolescent populations as well. Further, whereas most studies of the social gradient have narrowed their attention to specific diseases, such as cardiovascular diseases, we document that the social gradient is far more ubiquitous and troubling. Low social class adversely affects many areas of people’s health, including their physical, dental and mental health.
These findings do not mean that adult social class is inconsequential for health. Four findings underscore the contribution of contemporaneous adult socioeconomic status. First, both low-childhood and low-adult status were related to poor cardiorespiratory fitness and poor dental health (table), suggesting that exposure to adverse environments in childhood and in adulthood contribute additively to some adult health risks.3,13,17 Second, upward mobility from childhood to adulthood was associated with lower waist:hip ratio (figure). Third, downward mobility from childhood to adulthood was associated with poorer fitness and poorer dental health (figure). Finally, depression and tobacco dependence were more strongly linked to adult socioeconomic status than to childhood socioeconomic status (table), suggesting that proximal experiences in adulthood better account for the association between low socioeconomic status and these mental health disorders.24
Several limitations are apparent. First, our measure of childhood socioeconomic origins was limited to parental occupational status and did not incorporate all potential indicators of social inequality.25 However, in so far as childhood social origins were measured contemporaneously, directly, and across the entire childhood period, this method represents improvement on previous attempts to identify childhood socioeconomic status via adult recall or through proxy measurements. Second, adult socioeconomic status at age 26 years might not reflect final socioeconomic destination, and adult achievements later in life might increasingly undo earlier childhood influences. However, most of the Dunedin Study members have completed their formal education, and rates of adult return to education in New Zealand are low. Because educational attainment is an excellent predictor of socioeconomic status at midlife (age 50 years),15 we repeated all analyses substituting a measure of the study members’ educational achievement for the measure of adult occupational status, categorised as no or little school qualification (School Certificate [roughly equivalent to the British General Certificate in Secondary Education] or less; n=304, 31%); 6th Form Certificate (equivalent to British A-levels or a US high school degree; n=461, 47%); and bachelors degree or higher (n=215, 22%). We obtained the same pattern of results, suggesting that the influence of childhood socioeconomic status is unlikely to vanish. Finally, the findings from this contemporary New Zealand cohort (born 1972–73) require replication in other parts of the world. Previous studies examined links between childhood socioeconomic status and adult mortality and morbidity in older cohorts (born 1906–58),6,13,17,26 but our study suggests that these links continue to hold today. Moreover, childhood socioeconomic status has pervasive effects on adult health despite the fact that members of this contemporary cohort grew up with access to universal subsidised health care.
The present study provides a strong test of the effect of childhood socioeconomic experiences on adult health, while ruling out potential alternative explanations. Research now needs to identify the key mechanisms that bring about this longitudinal association. Although lack of resources and structural impediments (eg, lack of community facilities for physical activities) might play a part, the breadth of adult-health variables affected (ranging across physical health, dental health, and substance abuse) suggests several other candidate mechanisms.26 First, class-biased health-care delivery during children’s formative years might create long-lasting health inequalities. Second, social-class related differences in health-promoting parenting practices might contribute to early-emerging and long-lasting health differences among children.27 Finally, social-class related stressors in childhood might alter biological systems and exert long-lasting influences on adult health.28 Developmental studies, in particular, should focus on health-related parenting practices and on the nature of stressors experienced by children in different social strata to provide insight into the origins of the enduring association between childhood socioeconomic status and adult health.29 If risk for later morbidity is influenced by early life circumstances, efforts to reduce health inequalities must begin as early as practicable to ensure the greatest impact on burden of disease.30
Table 1.
Table Health outcomes at age 26 years according to childhood socioeconomic position and adult socioeconomic position
| Socioeconomic group
|
Statistical test of effect of socioeconomic status*
|
||||||
|---|---|---|---|---|---|---|---|
| Low | Medium | High | Low vs high socioeconomic status | p | Medium vs high status socio- economic status | p | |
|
|
|
|
|
|
|
|
|
| Adult physical health† | |||||||
| Body-mass index (kg/m2) | |||||||
| Childhood socioeconomic status | 26·1 (5·3) | 24·9 (4·2) | 24·4 (3·9) | 1·95 (0·49) | <0·0001 | 0·55 (0·39) | 0·16 |
| Adult socioeconomic status | 25·3 (4·8) | 24·9 (4·0) | 24·8 (4·1) | 0·01 (0·43) | 0·98 | –0·12 (0·38) | 0·75 |
| Waist:hip ratio | |||||||
| Childhood socioeconomic status | 81·1 (7·0) | 79·9 (6·8) | 79·3 (6·9) | 1·57 (0·51) | 0·002 | 0·35 (0·41) | 0·39 |
| Adult socioeconomic status | 81·8 (6·7) | 79·5 (6·9) | 79·3 (6·8) | 0·55 (0·45) | 0·22 | –0·16 (0·39) | 0·69 |
| Systolic blood pressure (mm Hg) | |||||||
| Childhood socioeconomic status | 117·0 (11·6) | 117·4 (11·2) | 114·6 (9·9) | 2·58 (1·15) | 0·02 | 2·73 (0·91) | 0·003 |
| Adult socioeconomic status | 117·6 (11·2) | 117·2 (11·1) | 116·5 (11·0) | –0·98 (1·02) | 0·33 | 0·09 (·88) | 0·92 |
| Cardiorespiratory fitness (VO2max/kg) | |||||||
| Childhood socioeconomic status | 41·6 (11·5) | 44·7 (10·8) | 45·2 (10·6) | –2·61 (1·29) | 0·04 | –0·68 (1·00) | 0·50 |
| Adult socioeconomic status | 43·9 (11·0) | 44·2 (10·9) | 46·1 (10·6) | –2·54 (1·14) | 0·03 | –1·89 (0·98) | 0·05 |
|
|
|
|
|
|
|
|
|
| Adult dental health | |||||||
| Tooth cleanliness (plaque score)† | |||||||
| Childhood socioeconomic status | 0·98 (0·59) | 0·86 (0·53) | 0·77 (0·46) | 0·14 (0·06) | 0·02 | 0·06 (0·05) | 0·25 |
| Adult socioeconomic status | 1·03 (0·58) | 0·83 (0·51) | 0·71 (0·48) | 0·26 (0·05) | <0·0001 | 0·10 (0·05) | 0·02 |
| Proportion of teeth with gingival bleeding† | |||||||
| Childhood socioeconomic status | 37·7% (29·1) | 28·9% (24·4) | 23·7% (23·2) | 10·76 (2·90) | 0·0002 | 4·14 (2·30) | 0·07 |
| Adult socioeconomic status | 35·7% (27·1) | 27·9% (24·6) | 24·0% (22·0) | 9·39 (2·54) | 0·0002 | 2·74 (2·20) | 0·21 |
| Proportion with periodontal disease‡ | |||||||
| Childhood socioeconomic status | 31·1% | 16·6% | 11·9% | 2·88 (1·53–5·39) | 0·001 | 1·39 (0·80–2·44) | 0·25 |
| Adult socioeconomic status | 22·3% | 17·7% | 11·9% | 1·57 (0·88–2·78) | 0·13 | 1·41 (0·84–2·39) | 0·19 |
| Proportion with ≥4 surfaces affected by dental caries‡ | |||||||
| Childhood socioeconomic status | 32·2% | 19·4% | 9·9% | 3·18 (1·66–6·10) | 0·0005 | 1·84 (1·03–3·30) | 0·04 |
| Adult socioeconomic status | 26·9% | 18·9% | 10·2% | 2·46 (1·37–4·40) | 0·003 | 1·84 (1·06–3·18) | 0·03 |
|
|
|
|
|
|
|
|
|
| Adult mental health and substance abuse‡ | |||||||
| Proportion with depression | |||||||
| Childhood socioeconomic status | 16·5% | 16·8% | 17·8% | 0·63 (0·34–1·14) | 0·13 | 0·80 (0·50–1·29) | 0·36 |
| Adult socioeconomic status | 22·3% | 15·0% | 13·1% | 2·30 (1·34–3·96) | 0·003 | 1·25 (0·76–2·06) | 0·39 |
| Proportion with alcohol dependence | |||||||
| Childhood socioeconomic status | 21·5% | 17·3% | 12·1% | 1·80 (0·97–3·34) | 0·06 | 1·37 (0·80–2·35) | 0·25 |
| Adult socioeconomic status | 21·1% | 18·3% | 11·5% | 1·62 (0·92–2·85) | 0·10 | 1·61 (0·96–2·71) | 0·07 |
| Proportion with tobacco dependence | |||||||
| Childhood socioeconomic status | 16·2% | 13·7% | 9·6% | 1·12 (0·56–2·25) | 0·76 | 1·12 (0·62–2·04) | 0·70 |
| Adult socioeconomic status | 21·1% | 11·4% | 6·0% | 3·81 (1·89–7·65) | 0·0002 | 1·98 (1·01–3·89) | 0·05 |
Regression coefficients represent effects of unit changes in socioeconomic status on health outcomes, adjusting for other covariates in model. For example, relative to those from high socioeconomic status backgrounds, those from low socioeconomic status backgrounds have increased body-mass index of 1·95. Odds ratios are adjusted for other covariates in model. Childhood socioeconomic status is adjusted for sex, infant health, and adult socioeconomic status; adult socioeconomic status is adjusted for sex, infant health, and childhood socioeconomic status, n=931.
Unstandardised regression coefficients (SE) or odds ratios (95% CI).
Unadjusted means (SD).
Unadjusted percentages.
Acknowledgments
We thank the Dunedin Study members and their parents, Unit research staff, Air New Zealand, study founder Phil A Silva, Charlotte Paul, and Sandhya Ramrakha. The Dunedin Multidisciplinary Health and Development Research Unit is supported by the New Zealand Health Research Council. This research received support from the National Heart Foundation of New Zealand, the W T Grant Foundation, and US-NIMH grants MH45070 and MH49414.
Footnotes
Contributors
R Poulton and A Caspi devised the hypothesis, collected data, and drafted the paper. T E Moffitt collected data and drafted the paper. B J Milne and A Taylor did the statistical analyses. W M Thomson and M R Sears collected data and provided critical editorial comment.
Conflict of interest statement
None declared.
References
- 1.Marmot M, Wilkinson RG, editors. Social determinants of health. Oxford: Oxford University Press; 1999. [Google Scholar]
- 2.Leon D, Walt G, editors. Poverty inequality and health: an international perspective. Oxford: Oxford University Press; 1999. [Google Scholar]
- 3.Blane D, Hart CL, Davey Smith G, et al. Association of cardiovascular disease risk factors with socioeconomic position during childhood and during adulthood. BMJ. 1996;313:1434–38. doi: 10.1136/bmj.313.7070.1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brunner E, Davey Smith G, Marmot M, Canner R, Beksinska M, O’Brien J. Childhood social circumstances and psychosocial and behavioural factors as determinants of plasma fibrinogen. Lancet. 1996;347:1008–13. doi: 10.1016/s0140-6736(96)90147-6. [DOI] [PubMed] [Google Scholar]
- 5.Power C, Hertzman C. Social and biological pathways linking early life and adult disease. Br Med Bull. 1997;53:210–21. doi: 10.1093/oxfordjournals.bmb.a011601. [DOI] [PubMed] [Google Scholar]
- 6.Wannamethee SG, Whincup PH, Shaper G, Walker M. Influence of fathers’ social class on cardiovascular disease in middle aged men. Lancet. 1996;348:1259–63. doi: 10.1016/S0140-6736(96)02465-8. [DOI] [PubMed] [Google Scholar]
- 7.Elford J, Whincup P, Shaper AG. Early life experience and adult cardiovascular disease: longitudinal and case-control studies. Int J Epidemiol. 1991;20:833–44. doi: 10.1093/ije/20.4.833. [DOI] [PubMed] [Google Scholar]
- 8.Gliksman MD, Kawachi I, Hunter D, et al. Childhood socioeconomic status and risk of cardiovascular disease in middle aged US women: a prospective study. J Epidemiol Community Health. 1995;49:10–15. doi: 10.1136/jech.49.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marmot MG, Shipley M, Brunner E, Hemingway H. Relative contribution of early life and adult socioeconomic factors to adult morbidity in the Whitehall II study. J Epidemiol Community Health. 2001;55:301–07. doi: 10.1136/jech.55.5.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Looker ED. Accuracy of proxy reports of parental status characteristics. Sociol Educ. 1989;62:257–76. [Google Scholar]
- 11.Wolfe B, Haveman R, Ginther D, An CB. The “window problem” in studies of children’s attainments: a methodological exploration. J Am Stat Assoc. 1996;91:970–82. [Google Scholar]
- 12.Conley D, Bennett NG. Is biology destiny? Birth weight and life chances. Am Sociol Rev. 2000;65:558–567. [Google Scholar]
- 13.Power C, Matthews S, Manor O. Inequalities in self-rated health: explanations from different stages of life. Lancet. 1998;351:1009–14. doi: 10.1016/S0140-6736(97)11082-0. [DOI] [PubMed] [Google Scholar]
- 14.Barker DJP. Mothers, babies and health in later life. 2. Edinburgh: Churchill Livingstone; 1998. [Google Scholar]
- 15.Hauser RM, Warren JR, Haung MS, Carter WY. Social stratification across three generations. In: Arrow K, Bowles S, Durlauf S, editors. Meritocracy and inequality. Princeton, NJ: Princeton University Press; 2000. pp. 179–229. [Google Scholar]
- 16.Ben-Shlomo Y, Davey Smith G. Deprivation in infancy or in adult life: which is more important for mortality risk? Lancet. 1991;337:530–34. doi: 10.1016/0140-6736(91)91307-g. [DOI] [PubMed] [Google Scholar]
- 17.Davey Smith G, Hart C, Blane D, Hole D. Adverse socioeconomic conditions in childhood and cause specific adult mortality: prospective observational study. BMJ. 1998;316:1631–35. doi: 10.1136/bmj.316.7145.1631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Silva PA, Stanton WR, editors. From child to adult: the Dunedin Multidisciplinary Health and Development Study. Oxford: Oxford University Press; 1996. [Google Scholar]
- 19.Elley WB, Irving JC. Revised socio-economic index for New Zealand. N Z J Educ Stud. 1976;11:25–56. [Google Scholar]
- 20.Greene JC, Vermillion JR. The simplified oral hygiene index. J Am Dent Assoc. 1964;68:7–13. doi: 10.14219/jada.archive.1964.0034. [DOI] [PubMed] [Google Scholar]
- 21.Thomson WM, Hashim R, Pack ARC. The prevalence and intra-oral distribution of periodontal loss of attachment in a birth cohort of 26-year-olds. J Periodontol. 2000;71:1840–45. doi: 10.1902/jop.2000.71.12.1840. [DOI] [PubMed] [Google Scholar]
- 22.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 23.Rosenthal R, Rosnow R. Contrast analysis: focused comparison in the analysis of variance. New York: Cambridge University Press; 1985. [Google Scholar]
- 24.Miech RA, Caspi A, Moffitt TE, Wright BR, Silva PA. Low socioeconomic status and mental disorders: a longitudinal study of causation and selection. Am J Sociol. 1998;104:1096–1131. [Google Scholar]
- 25.Winkleby MA, Jatulis DE, Frank E, Fortmann SP. Socio-economic status and health: how education, income, and occupation contribute to risk factors for cardiovascular disease. Am J Public Health. 1992;82:816–20. doi: 10.2105/ajph.82.6.816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wadsworth MEJ. Health inequalities in the life course perspective. Soc Sci Med. 1997;44:859–69. doi: 10.1016/s0277-9536(96)00187-6. [DOI] [PubMed] [Google Scholar]
- 27.Taylor SE, Repetti RL. Health psychology: what is an unhealthy environment and how does it get under the skin? Annu Rev Psychol. 1997;48:411–47. doi: 10.1146/annurev.psych.48.1.411. [DOI] [PubMed] [Google Scholar]
- 28.Brunner E. Stress and the biology of inequality. BMJ. 1997;314:1472–76. doi: 10.1136/bmj.314.7092.1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kuh D, Power C, Blane D, Bartley M. Social pathways between childhood and adult health. In: Kuh D, Ben-Shlomo Y, editors. A life course approach to chronic disease epidemiology. Oxford: Oxford University Press; 1997. pp. 169–98. [Google Scholar]
- 30.Hertzman C, Wiens M. Child development and long-term outcomes: a population health perspective and summary of successful interventions. Soc Sci Med. 1996;43:1083–95. doi: 10.1016/0277-9536(96)00028-7. [DOI] [PubMed] [Google Scholar]