Abstract
Lobomycosis is a chronic subcutaneous mycosis for which no standard treatment is available to date. We describe a patient in Peru with lobomycosis on the left earlobe that was successfully treated with posaconazole for 27 months. No evidence of recurrence was observed after five years of follow-up.
Lobomycosis (lacaziosis) is a chronic subcutaneous disease caused by the fungus Lacazia loboi, which is reported mainly in Central and South America, mostly from Brazil and Colombia.1,2 Peru has reported only two cases to date.3,4 Lobomycosis is characterized by subcutaneous nodules with keloid-like, ulcerated, or verrucomatous surfaces. Lacazia loboi has never been isolated in culture from humans. Therefore, the diagnosis is based on identifying yeast-like cells by direct examination of exudates or skin scrapings, or by histopathologic analysis. There is no standard treatment for this disease. A wide surgical excision for small and well-demarcated early lesions may be effective, but relapses are common. We report a third case of lobomycosis in a patient from Peru and the first patient treated with posaconazole.
Case Description
A 29 year-old man (forest ranger) who was a native of the Peruvian jungle noticed a painless but pruriginous papular lesion on his left earlobe at the age of 12 years. He did not recall previous trauma. At the age of 23, he was given a misdiagnosis of cutaneous leishmaniasis on the basis of clinical findings and was treated with meglumine antimoniate (Glucantime™) for five days with no improvement.
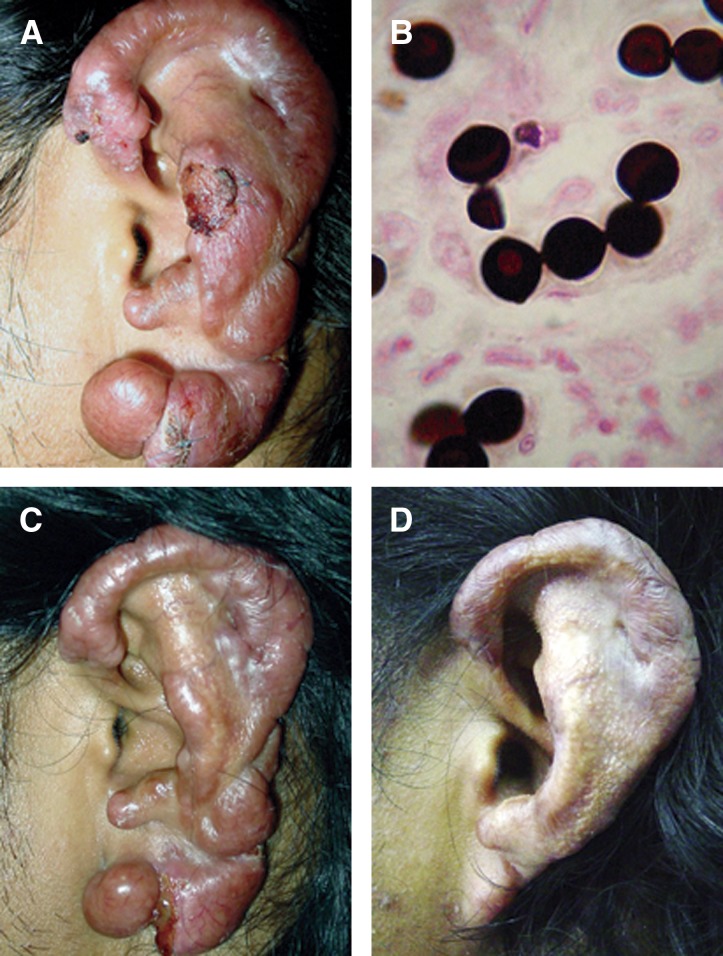
In September 2004, after 17 years of slow disease progression, the patient came to our hospital for clinical evaluation. At physical examination, the entire left earlobe was involved, presenting diffuse infiltration, as well as multiple nodules and ulcers (Figure 1A). At that time, direct examination and pathologic findings of a skin biopsy specimen showed multiple, round yeast-like cells in chains of 3–4 elements, typical of L. loboi (Figure 1B). The patient was enrolled in an open-label, limited access protocol of oral posaconazole for treatment of invasive fungal infections and received 400 mg, 2 times/day for 27 months. Significant clinical improvement was observed at four months compared with baseline (Figure 1C). A partial resection of a nodular lesion on the inferior border of the earlobe was performed at the eleventh month of treatment for cosmetic reasons.
Figure 1.
A, Multiple, ulcerated nodules on the left earlobe of the patient at baseline. B, Skin biopsy specimen showing characteristic yeast-like cells of Lacazia loboi (Grocott stain, original magnification ×1000). C, Significant improvement of the lesions after four months of treatment. D, Postinflamatory hyperpigmentation of the skin at the end of treatment.
The patient was considered clinically cured after 24 months (Figure 1D). At this time, all ulcers resolved and the inflammatory signs (edema and erythema) had disappeared, leaving only post-inflammatory hyperpigmentation. The medical treatment was continued for three months. A new examination from a surgical biopsy specimen of the earlobe taken at this time showed persistence of L. loboi cells. The patient was followed-up for five years and showed no further evidence of clinical recurrence. Tolerance to treatment was excellent. There were no treatment interruptions because of adverse events. He only reported a mild headache during the first three days of therapy, which might have been related to the drug. Hepatic enzyme levels remained within normal ranges throughout.
Discussion
Lobomycosis is a neglected, chronic, and sometimes disfiguring fungal disease, usually diagnosed several years after initial clinical manifestations. Although spontaneous remissions of macular lesions have been reported in three patients, relapses near the scar or in different body areas occurred in two of these patients. The third patient was followed-up for 2 years and showed no evidence of recurrence.5
The response to treatment for this disease is disappointing. Amphotericin B, 5-fluorocytosine, ketoconazole, itraconazole, and clofazamine have been used with limited or no success.1,6,7 Although a few patients have benefited from a combination of clofazimine and itraconazole therapy, no systematic evaluation supports this recommendation.8 Favorable results after surgical excision or cryosurgery have been obtained in early and small well-circumscribed lesions, but relapses at the margin of the excision may still occur.9,10
Posaconazole is a new triazole that has demonstrated efficacy in the treatment of subcutaneous diseases caused by Madurella grisea, Madurella mycetomatis, Scedosporium apiospermium, and Fonsecaea pedrosoi refractory to standard therapy.11 This antifungal agent appears to be safe and well tolerated when prescribed for prolonged periods (> 6 months) for treatment of subacute or chronic fungal infections.12
In our patient, the location of the lesion precluded any radical surgical excision. His favorable clinical response to posaconazole therapy was first observed after fourth months of treatment and continued throughout the follow-up period. Although there was a good clinical response, persistent L. loboi cells could be demonstrated in the biopsy specimen obtained after 27 months of therapy. The meaning of this finding in relation to the subsequent long period of disease-free status (five years) needs to be determined to better define the duration of treatment. A novel technique has been developed to determine the viability of L loboi to evaluate success of therapy. This method uses vital staining with fluorescein diacetate–ethidium bromide and has showed consistent sensitivity and specificity for detecting viability in a murine experimental model of lobomycosis.13 If the good results observed in this animal model are further corroborated in humans, this test could be useful for determining objectively the duration of treatment.
Posaconazole was clinically effective in the treatment of lobomycosis in this patient, and its prolonged administration was well tolerated. The precise follow-up period for detecting recurrence is not known. Posaconazole, either alone or combined with partial surgical excision, could be an alternative for patients with extensive disease, or for patients whose disease would require disfiguring surgery, as in this case. One of the most important limitations for its use is the high cost of the drug. Thus, there is an urgent need to find effective and affordable antifungal drugs for the treatment of lobomycosis.
ACKNOWLEDGMENTS
A preliminary report (P-0199) of this case was presented at the 16th Congress of the International Society for Human and Animal Mycology, Paris, France, June 25–29, 2006.
Footnotes
Financial support: Beatriz Bustamante participated as study investigator in a clinical trial sponsored by Schering Plough for which the patient was enrolled. Carlos Seas was supported by an Investigator Initiated Research grant from Pfizer.
Authors' addresses: Beatriz Bustamante and Carlos Seas, Departamento de Enfermedades Infecciosas, Tropicales y Dermatológicas, Hospital Nacional Cayetano Heredia, Lima, Peru, and Instituto de Medicina Tropical Alexander von Humboldt, Universidad Peruana Cayetano Heredia, Lima, Peru, E-mails: ana.bustamante@upch.pe and carlos.seas@upch.pe. Martín Salomon, Departamento de Enfermedades Infecciosas, Tropicales y Dermatológicas, Hospital Nacional Cayetano Heredia, Lima, Peru, E-mail: martin.salomon.n@upch.pe. Francisco Bravo, Instituto de Medicina Tropical Alexander von Humboldt, Universidad Peruana Cayetano Heredia, Lima, Peru, E-mail: fbravopuccio@gmail.com.
References
- 1.Woods WJ, Belone Ade F, Carneiro LB, Rosa PS. Ten years experience with Jorge Lobo's disease in the state of Acre, Amazon region, Brazil. Rev Inst Med Trop Sao Paulo. 2010;52:273–278. doi: 10.1590/s0036-46652010000500010. [DOI] [PubMed] [Google Scholar]
- 2.Rodríguez-Toro G, Tellez N. Lobomycosis in Colombian Amerindian patients. Mycopathologia. 1992;120:5–9. doi: 10.1007/BF00578495. [DOI] [PubMed] [Google Scholar]
- 3.Romero RO. Jorge Lobo's disease (keloyd blastomycosis). Diagnosis of the first Peruvian case. Arch Per Pat Clin. 1972;26:63–86. [Google Scholar]
- 4.Talhari S, Caparo AB, Ganter B. Jorge Lobo's disease. Second Peruvian case. Med Cut ILA. 1985;13:201–204. [PubMed] [Google Scholar]
- 5.Machado P de A. Spontaneous regression of macular lesions in Jorge Lobo's blastomycosis. Acta Amaz (Manaus) 1972;2:47–50. [Google Scholar]
- 6.Lawrence D, Ajello L. Lobomycosis in western Brazil: report of a clinical trial with ketoconazole. Am J Trop Med Hyg. 1986;35:162–166. doi: 10.4269/ajtmh.1986.35.162. [DOI] [PubMed] [Google Scholar]
- 7.Carneiro FP, Maia LB, Moraes MA, de Magalhães AV, Vianna LM, Zancanaro PC, Reis CM. Lobomycosis: diagnosis and management of relapsed and multifocal lesions. Diagn Microbiol Infect Dis. 2009;65:62–64. doi: 10.1016/j.diagmicrobio.2009.04.013. [DOI] [PubMed] [Google Scholar]
- 8.Fischer M, Chrusciak Talhari A, Reinel D, Talhari S. Sucessful treatment with clofazimine and itraconazole in a 46-year-old patient after 32 years duration of disease. Hautarzt. 2002;53:677–681. doi: 10.1007/s00105-002-0351-y. [DOI] [PubMed] [Google Scholar]
- 9.Miranda MF, Unger DA, Brito AC, Carneiro FA. Jorge Lobo's disease with restricted labial presentation. An Bras Dermatol. 2011;86:373–374. doi: 10.1590/s0365-05962011000200028. [DOI] [PubMed] [Google Scholar]
- 10.Baruzzi RG, Marcopito LF, Michalany NS, Livianu J, Pinto NR. Early diagnosis and prompt treatment by surgery in Jorge Lobo's disease (keloidal lastomycosis) Mycopathologia. 1981;74:51–54. doi: 10.1007/BF00441441. [DOI] [PubMed] [Google Scholar]
- 11.Negroni R, Tobon A, Bustamante B, Shikanai-Yasuda MA, Patino H, Restrepo A. Posaconazole treatment of refractory eumycetoma and chromoblastomycosis. Rev Inst Med Trop Sao Paulo. 2005;47:339–346. doi: 10.1590/s0036-46652005000600006. [DOI] [PubMed] [Google Scholar]
- 12.Raad II, Graybill JR, Bustamante AB, Cornely OA, Gaona-Flores V, Afif C, Graham DR, Greenberg RN, Hadley S, Langston A, Negroni R, Perfect JR, Pitisuttithum P, Restrepo A, Schiller G, Pedicone L, Ullmann AJ. Safety of long-term oral posaconazole use in the treatment of refractory invasive fungal infections. Clin Infect Dis. 2006;42:1726–1734. doi: 10.1086/504328. [DOI] [PubMed] [Google Scholar]
- 13.Vilani-Moreno FR, Belone Ade F, Rosa PS, Madeira S, Opromolla DV. Evaluation of the vital staining method for Lacazia loboi through the experimental inoculation of BALB/c mice. Med Mycol. 2003;41:211–216. doi: 10.1080/13693780310001597359. [DOI] [PubMed] [Google Scholar]