Abstract
Context
If family history is associated with clinical features that are thought to index seriousness of disorder, this could inform clinicians predicting patients’ prognosis and researchers selecting cases for genetic studies. Although tests of associations between family history and clinical features are numerous for depression, such tests are relatively lacking for other disorders.
Objective
To test the hypothesis that family history is associated with 4 clinical indexes of disorder (recurrence, impairment, service use, and age at onset) in relation to 4 psychiatric disorders (major depressive episode, anxiety disorder, alcohol dependence, and drug dependence).
Design
Prospective longitudinal cohort study.
Setting
New Zealand.
Participants
A total of 981 members of the 1972 to 1973 Dunedin Study birth cohort (96% retention).
Main Outcome Measures
For each disorder, family history scores were calculated as the proportion of affected family members from data on 3 generations of the participants’ families. Data collected prospectively at the study’s repeated assessments (ages 11–32 years) were used to assess recurrence, impairment, and age at onset; data collected by means of a life history calendar at age 32 years were used to assess service use.
Results
Family history was associated with the presence of all 4 disorder types. In addition, family history was associated with a more recurrent course for all 4 disorders (but not significantly for women with depression), worse impairment, and greater service use. Family history was not associated with younger age at onset for any disorder.
Conclusions
Associations between family history of a disorder and clinical features of that disorder in probands showed consistent direction of effects across depression, anxiety disorder, alcohol dependence, and drug dependence. For these disorder types, family history is useful for determining patients’ clinical prognosis and for selecting cases for genetic studies.
Family history of psychiatric disorder generally predicts the simple presence vs absence of that disorder among probands.1–8 However, there is a need to go further and test whether family history is also associated with clinical features of the disorder thought to represent a continuum of seriousness among individuals who meet criteria for diagnosis.
This article reports a test of the hypothesis that family history is associated with clinical indicators of a disorder’s developmental course (younger age at onset, more frequent recurrence) and health burden (worse impairment, more service use). Evidence that family history is associated with such seriousness indicators could inform both clinical practice and research design. First, if family history is associated with clinical features that are thought to index seriousness of disorder, then family history could be used prognostically to determine which patients will have the poorest outcome, and scarce treatment resources could be directed to patients with a positive family history of their disorder. Second, if family history is associated with certain clinical features, then those features might be inferred to indicate a form of disorder that is under greater genetic influence, and researchers might benefit from selecting individuals with those features for genetic studies.8
There are 3 notable research gaps. First, although a number of clinical features have been investigated in relation to family history of depression,3,9–13 other psychiatric disorders have been less well studied. There is a need for systematic investigation of the association between clinical indexes and family history across a broader range of disorder types. For example, for anxiety disorder, alcohol dependence, and drug dependence, there have been, to our knowledge, no family history studies reporting on recurrence of disorder and only a handful of studies reporting on impairment or use of mental health services.14–17
Second, there is a need to compare the association between clinical features and family history across multiple different disorders, but within the same cohort of families. Although a handful of studies have assessed familial aggregation across different disorders within the same sample,1,18 to our knowledge no study has sought to compare associations with clinical features across different disorders. Methodologic differences in sampling, design, measurement, and statistical approach among single-disorder studies have made it difficult to discern whether different disorders show the same or distinctive patterns of family history effects. A systematic investigation using one cohort of families would allow us to compare the direction of effects and effect sizes for family history’s effects on different disorders, while holding constant aspects of the study methods.
Third, there is a need to assess clinical features beyond age at onset. Age at onset is probably the only clinical feature that has been well studied in relation to family history across different disorders. Most studies have reported significant associations between early onset of disorder and family history of depression,10,13,19–42 anxiety disorders,43–48 alcohol dependence,15,16,49–59 and drug dependence.60,61 However, some researchers have failed to find an association (eg, for depression,9,11,62–70 anxiety disorders,71 alcohol dependence,72,73 and drug dependence17). Moreover, far less is known about associations between family history and other clinical features such as recurrence, impairment, and service use that may also indicate seriousness of disorder. We are aware that these 4 indicators are influenced by factors apart from seriousness; for example, measures of service use are influenced, in part, by access to health care. Nevertheless, we focus on these 4 clinical features because earlier onset of disorder leads to impaired social functioning,74 frequent recurrence of disorder disrupts long-term adult adjustment,75 self-reported impairment indicates that the disorder has subjectively interfered with personal goals, and service use indicates greater burden on health care systems.
In the present study, we tested hypotheses that family history would be associated with 4 clinical indexes of a disorder (recurrence, impairment, service use, and age at onset) in relation to 4 psychiatric disorders (major depressive episode, anxiety disorder, alcohol dependence, and drug dependence) in a birth cohort of 32-year-olds.
METHODS
PARTICIPANTS
Participants were members of the Dunedin Study, a 1-year birth cohort constituted at 3 years of age when investigators enrolled 91% of consecutive eligible births between April 1972 and March 1973 in Dunedin, New Zealand.76 Follow-up assessments were conducted at ages 5, 7, 9, 11, 13, 15, 18, 21, 26, and 32 years. Herein we report data from 981 participants (96.7% of the living sample of 1015; 50.9% male) who had available family history data. Cohort families represent the full range of socioeconomic status in New Zealand’s South Island and are primarily white. All participants gave informed consent before participating. Study protocols were approved by the ethics committees of all universities involved.
FAMILY HISTORY OF DISORDER
The Dunedin Study family history assessment has been described in detail elsewhere.7 Briefly, family history data were collected about each participant’s biological parents, grandparents, and siblings older than 10 years. Family histories were collected in 2003 to 2005 when the participants were 30 to 33 years of age. To minimize underreporting, 3 informants were sought to provide reports on each family member (eg, the participant and both of his or her parents; 80.5% of participants had 3 reporters, 15.7% had 2, and 3.8% had 1). Combining data from the 3 informants resulted in data for 7856 family members from the families of 981 participants (average of 8 members per family; range, 3–16). These included 3764 first-degree relatives (981 biological mothers, 974 biological fathers, and 1809 full siblings) and 4092 second-degree relatives (1845 biological grandmothers, 1817 biological grandfathers, and 430 half-siblings).
Family history was assessed by means of the Family History Screen (FHS), a valid and reliable measure of psychiatric family history that has been shown to have acceptable sensitivity and specificity across a range of disorders.77,78 The κ values for the protocol’s test-retest reliability across a 15-month period were 0.56 for depression, 0.52 for anxiety, 0.61 for alcohol abuse, and 0.66 for drug abuse.77 To minimize potential underreporting, the FHS uses pairs of questions to ascertain each symptom. First, a broadly sensitive “introductory screen” question is asked to stimulate memory and give the respondent time to reflect (eg, “Has anyone on the list of family members ever had a sudden spell or attack in which they felt panicked?”). If any family members are named in response to the introductory question, it is followed by a second, narrower “symptom definition” question (eg, “Did this person have several attacks of extreme fear or panic, even though there was nothing to be afraid of?”). For data analysis purposes, only the second questions are used.
To broaden the FHS’s coverage, we added items drawn from the Short Michigan Alcoholism Screening Test,79 the Drug Abuse Screening Test,80 and the Diagnostic Interview Schedule for DSM-IV.81 We also added a checklist of psychiatric conditions commonly understood by the public (eg, “alcoholism,” “depression”). In total, there were symptom definition items pertaining to major depressive episode (4 items), anxiety (13 items on generalized anxiety, panic, agoraphobia, phobia, and obsessive-compulsive disorder), alcohol dependence (3 items), and drug dependence (3 items).
The measures of family history were created as continuously distributed scores representing the proportion of a proband’s family members who had disorder. Following the recommendations of Vandeleur et al,82 a family member was considered to have a history of disorder if 1 or more of the disorder’s items were endorsed by at least 50% of the informants (ie, 2 of 3 informants, 1 of 2 informants, or 1 of 1 informant). Each participant’s family history of disorder was calculated as the proportion of members in the family with a positive history of disorder. To take account of genetic relatedness, second-degree relatives are considered to be “half” a family member for the purposes of calculating this proportion. For example, if a family comprises 4 grandparents, 2 parents, 1 full sibling, and 1 half-sibling, of whom 1 grandparent, 1 parent, and 1 full sibling were reported to have alcohol abuse, the proportion of family members with alcohol abuse would be 0.45 (ie, 2.5 [2 first-degree relatives plus 1 second-degree relative] divided by 5.5 [3 first-degree relatives plus 5 second-degree relatives]). Other scoring schemes can be used to define family history. However, we have demonstrated previously that proportion scores measure family history of disorder as well as—and, for some disorders, better than—alternative scoring schemes.7
To allow comparison across disorders, family liability scores for each disorder were z-standardized (mean, 0; SD, 1).
ASSESSMENT OF DISORDER IN PROBANDS
We assessed 4 disorders: major depressive episode (MDE), anxiety disorder (generalized anxiety, panic, agoraphobia, specific and social phobia, obsessive-compulsive disorder, and posttraumatic stress disorder), alcohol dependence, and drug dependence. Major depressive episode and anxiety were assessed at each of 7 ages: 11, 13, 15, 18, 21, 26, and 32 years. Alcohol dependence and drug dependence were assessed at each of 4 ages: 18, 21, 26, and 32 years. Disorders were assessed by means of the Diagnostic Interview Schedule for Children83 at younger ages (11–15 years) and the Diagnostic Interview Schedule for DSM-IV81,84 at older ages (18–32 years), with a past-year reporting period at each age. At ages 11, 13, and 15 years, diagnoses were made by means of the then-current Diagnostic and Statistical Manual of Mental Disorders (Third Edition) (DSM-III),85 at ages 18 and 21 years according to the then-current DSM-III-R,86 and at ages 26 and 32 years according to DSM-IV.87
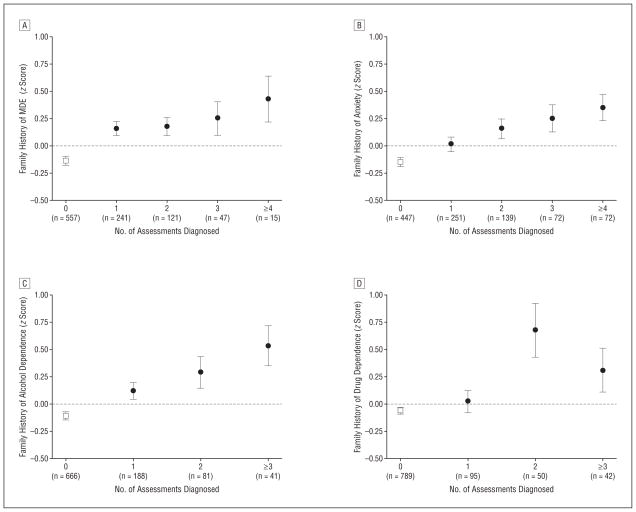
Recurrence was defined in this study as the number of assessment ages at which a disorder was diagnosed. The number of ages at which participants were diagnosed as having MDE was 0 (n=557), 1 (n=241), 2 (n=121), 3 (n=47), and 4 or more (n=15); for anxiety it was 0 (n=447), 1 (n=251), 2 (n=139), 3 (n=72), and 4 or more (n=72); for alcohol dependence it was 0 (n=666), 1 (n=188), 2 (n=81), and 3 or more (n=41); and for drug dependence it was 0 (n=789), 1 (n=95), 2 (n=50), and 3 or more (n=42). Data were unavailable for 5 participants for both alcohol dependence and drug dependence.
Impairment of function was determined at each of the assessments at ages 18, 21, 26, and 32 years among participants who reported diagnostic criteria for disorder. Participants were asked to rate on a 5-point scale (1, very little; 5, very much), “How much have these problems [associated with the disorder] interfered with your life, family, friends, work, or everyday activities?” The 4 repeated measures were used to calculate the maximum impairment due to each disorder experienced across ages 18 to 32 years.
Adult mental health service use was assessed at age 32 years by means of a life history calendar. This visual method (columns represent time units; rows represent events) has been shown to enhance recall reliability of health-related information.88,89 Participants first reported on the calendar easily recalled events involving their work lives (eg, jobs, spells of unemployment, educational enrollment) and family lives (eg, where they lived and with whom, when they moved, births of children, marriages, separations) as well as stressful life events (eg, deaths in the family, accidents, crime victimization). Using these data as anchors, respondents then reported on the calendar the years from ages 20 to 32 years in which they (1) received mental health treatment from a general physician, psychologist, psychiatrist, or emergency department; (2) took medication for a mental health problem; and (3) were treated as an inpatient in a psychiatric hospital, mental health rehabilitation center, or substance abuse facility. These 3 events were reported on a separate line of the calendar for each type of disorder (ie, depression, anxiety disorders, alcohol dependence, and drug dependence). One-month test-retest reliability of the resulting measures showed greater than 90% agreement.90 The calendar data were used to create 2 measures, whether from age 20 to 32 years cohort members had ever experienced (1) mental health treatment and (2) medication use/hospitalization.
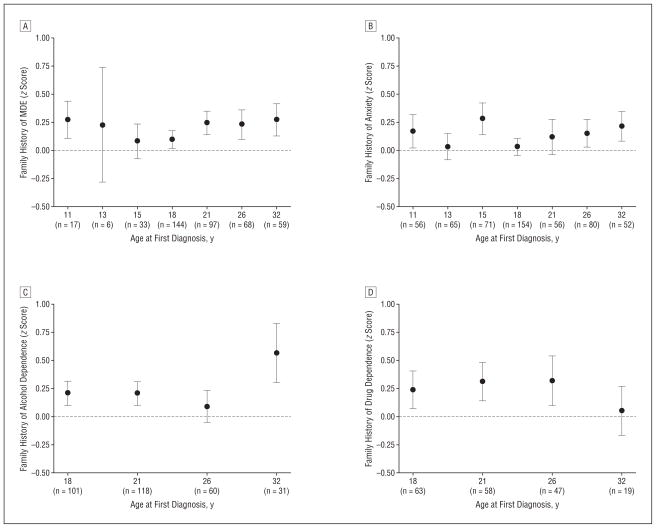
Age at onset was defined in this study as the earliest assessment age at which a disorder was diagnosed by the study. Age at onset of MDE was 11 years (n=17), 13 years (n=6), 15 years (n=33), 18 years (n=144), 21 years (n=97), 26 years (n=68), and 32 years (n=59); for anxiety it was 11 years (n=56), 13 years (n=65), 15 years (n=71), 18 years (n=154), 21 years (n=56), 26 years (n=80), and 32 years (n=52); for alcohol dependence it was 18 years (n=101), 21 years (n=118), 26 years (n=60), and 32 years (n=31); and for drug dependence it was 18 years (n=63), 21 years (n=58), 26 years (n=47), and 32 years (n=19). Because it was possible that a cohort member’s disorder could have onset during the intervening years not covered by our 12-month diagnostic assessments, we also created an additional indicator of age at onset by using each cohort member’s known age at first mental health service use. We were able to “fill in the gaps” for the period from age 20 to 32 years (the period for which mental health service use was recorded). We recoded the age-at-onset variable to the first age at which mental health services were used if that was younger than the first age at diagnosis by the study (recoding to a younger age occurred for 21 cases of MDE, 8 cases of anxiety disorder, 3 cases of alcohol dependence, and 4 cases of drug dependence).
STATISTICAL METHODS
We conducted the following series of analyses separately for each disorder in turn. First, we tested for evidence of familiality by comparing ever- vs never-disordered probands’ family history in a linear regression model. Next, we conducted tests of association between clinical features of disorder and family history by conducting 5 separate linear regression analyses, each with family history of disorder as the outcome and each separate analysis with 1 of the following 5 clinical features as the predictor: (1) the number of assessment ages at which a disorder was diagnosed (ie, recurrence); (2) the maximum rating of impairment of function; (3) whether the proband had received treatment for a disorder; (4) whether the proband had been hospitalized or had used medication for a disorder; and (5) the age at which a disorder was first diagnosed (ie, age at onset). All tests of association between clinical features of a disorder and family history were restricted to participants who had ever been diagnosed as having a disorder. The effects of sex were controlled in each analysis. Interactions between sex and the predictor were tested by entering a sex interaction term. All analyses were conducted with the use of Stata 9.1.91
RESULTS
FAMILIALITY
Figure 1 shows evidence of familiality for all 4 disorders (all P<.001). For each disorder, participants who had ever been diagnosed as having a disorder (circles in Figure 1) had family history scores that were approximately one-third standard deviation greater than those of participants who had never been diagnosed as having a disorder (squares in Figure 1). Effect sizes were as follows: MDE, 0.33; anxiety disorders, 0.29; alcohol dependence, 0.33; and drug dependence, 0.36. There was no evidence of any sex interactions between diagnosis of disorder and family history (all P>.1).
Figure 1.
Association between recurrence of disorder and family history of disorder. Data are shown for cohort members ever diagnosed (circles) as having major depressive episode (MDE) (A), anxiety (B), alcohol dependence (C), or drug dependence (D). For comparison purposes, family history scores for cohort members never diagnosed as having the disorders (squares) are also shown. Data points indicate the mean; error bars, standard error of the mean.
RECURRENCE
Among participants who ever received a diagnosis, there was a significant, graded association between recurrence and family history of disorder for anxiety (P=.005; Figure 1B) and alcohol dependence (P=.02; Figure 1C); as the number of assessments at which cohort members were diagnosed increased, so did the proportion of family members affected with a disorder. This positive linear association also applied to recurrence of drug dependence, but it did not reach conventional significance (P=.08; Figure 1D). However, post hoc analysis showed that cohort members who were drug dependent at 2 or more assessment ages had a significantly stronger family history of drug dependence than did those who were drug dependent at 1 assessment age only (P=.01). There was no evidence of sex interactions between recurrence and family history for anxiety, alcohol dependence, or drug dependence (all P>.30).
The association between recurrence of MDE and family history was not significant for the cohort as a whole (P=.33; Figure 1A). However, there was evidence of a sex interaction (P=.04), suggesting that data should be analyzed separately for the sexes. For men, there was a significant and positive association between recurrence and family history (n=161; P=.03). This association was not found for women (n=263; P=.73). In post hoc analyses we restricted analyses to women who were treated for MDE or who were more severely impaired by MDE and we repeated the test of the association between family depression history and recurrence. However, no association was found even in the subset of women who had received treatment for depression (n=119; P=.95); women who had been receiving medication or who had been hospitalized for depression (n=80; P =.58); or women in whom maximum impairment was rated as 3 or more (n=242; P=.89), 4 or more (n=169; P=.86), or 5 (n=101; P=.75).
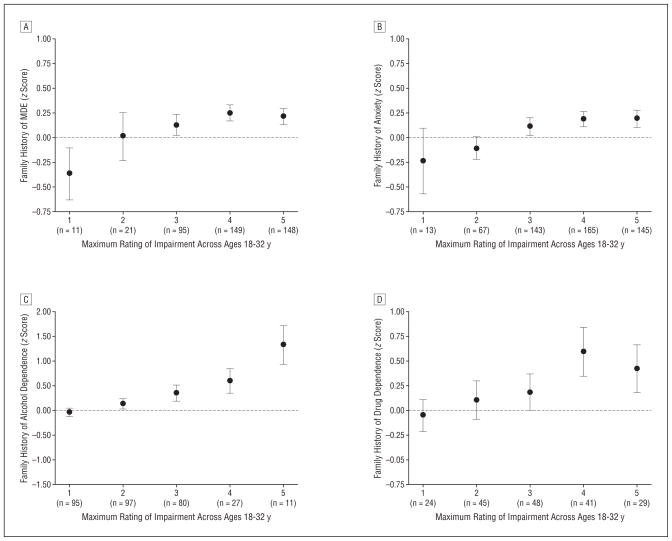
IMPAIRMENT OF FUNCTION
The association between self-rated impairment of function due to disorder and family history of disorder is shown in Figure 2. There were significant associations between self-rated impairment and family history for anxiety (Figure 2B; P=.03) and alcohol dependence (Figure 2C; P<.001). There were also trends for depression (Figure 2A; P=.10) and drug dependence (Figure 2D; P=.07). No significant sex interactions were detected (all P>.30).
Figure 2.
Association between impairment of function due to disorder (maximum rating across ages 18–32 years) and family history of disorder. Data are shown for cohort members ever diagnosed (circles) as having major depressive episode (MDE) (A), anxiety (B), alcohol dependence (C), or drug dependence (D). Data points indicate the mean; error bars, standard error of the mean.
MENTAL HEALTH SERVICE USE
The association with family history was significantly stronger for participants who experienced mental health treatment among those diagnosed as having MDE (Figure 3A; P=.04), alcohol dependence (Figure 3C; P=.01), and drug dependence (Figure 3D; P=.02), but this effect was not significant among those diagnosed as having anxiety (Figure 3B; P=.21). No significant sex interactions were detected (all P>.20).
Figure 3.
Association between receiving treatment for disorder and family history of disorder and between receiving medication or being hospitalized for disorder and family history of disorder. Data are shown for cohort members ever diagnosed as having major depressive episode (MDE) (A), anxiety (B), alcohol dependence (C), or drug dependence (D). Bar heights indicate the mean; error bars, standard error of the mean.
The association with family history was stronger for participants who experienced medication use or hospitalization among those diagnosed as having MDE (Figure 3A; P=.01) and alcohol dependence (Figure 3C; P=.007), and there was a nonsignificant trend for drug dependence (Figure 3D; P=.06). The association between family history and medication use or hospitalization was not significant for anxiety disorder (Figure 3B; P=.20). No significant sex interactions were detected (all P>.09).
AGE AT ONSET
No association was found between age at onset and family history for any disorder (all P>.20; Figure 4), nor were there any significant sex interactions (all P >.07). This lack of association may have been because the gaps between our past-year assessments led us to estimate the age at onset as being later than it actually was. We therefore conducted post hoc tests that used the alternate indicator of onset age that was recoded if age at first service use for a disorder was earlier than age at first diagnosis by the study. When we tested for associations between the recoded age-at-onset variables and family history of disorder, we still found no association for MDE (n = 474; P = .17), anxiety (n=552; P=.69), alcohol dependence (n=320; P=.64), or drug dependence (n=191; P=.66).
Figure 4.
Association between age at onset of disorder and family history of disorder. Data are shown for cohort members ever diagnosed (circles) as having major depressive episode (MDE) (A), anxiety (B), alcohol dependence (C), or drug dependence (D). Data points indicate the mean; error bars, standard error of the mean.
We undertook further post hoc analyses to test whether significant age-at-onset associations would be found among subsamples of participants who had been treated for or were more impaired by MDE. When we restricted affected cases to those who had ever experienced treatment for the disorder, no significant association was found for MDE (n = 167; P = .82), anxiety (n=86; P=.67), alcohol dependence (n=20; P=.95), or drug dependence (n = 33; P = .30). It was feasible to restrict affected cases to those who had taken medication or been hospitalized only for MDE and anxiety (numbers for alcohol and drug dependence were too small). However, when we did so, no significant associations were found (MDE: n=111, P=.33; anxiety: n=40, P=.86). When we restricted affected cases to those with a rating of 3 or greater for impairment, no significant associations were found (MDE: n=342, P=.91; anxiety: n=286, P=.41; alcohol dependence: n=96, P=.30; drug dependence: n = 87, P = .78). Similarly, when we restricted affected cases to those with a rating of 4 or greater for impairment, no significant associations were found (MDE: n=221, P=.78; anxiety: n=141, P=.55; alcohol dependence: n=31, P=.30; and drug dependence: n=48, P=.75). We could restrict affected cases to those with a rating of 5 for impairment only for MDE and anxiety (numbers were too small for alcohol and drug dependence), but still no significant associations between family history and age at onset were found (MDE: n=89, P=.59; anxiety: n=49, P=.34).
SENSITIVITY ANALYSES
Previous research has suggested that family history data can be biased by methodologic factors, including variation in the number of informants per family, the proportion of first-degree relatives per family pedigree, the sex of informants, whether informants are affected by the disorder, and the number of directly interviewed family members.77,78,92–102 We therefore undertook sensitivity analyses adjusting for each of these 5 factors to determine whether any of them had biased our results. All findings were unaltered in direction and remained significant after adjustment, except one: the association between family history of MDE and treatment for MDE became non-significant after adjustment for whether informants were affected by MDE (P=.13).
COMMENT
This study compared the associations between clinical indexes of disorder and family history among 4 psychiatric disorders: MDE, anxiety disorder, alcohol dependence, and drug dependence. In general, we found that associations showed a consistent direction of effect across all 4 disorders: (1) family history was associated with the presence vs absence of disorder for all 4 disorder types; (2) family history was associated with a recurrent course for all 4 disorders (but not significantly for women with depression); (3) family history was associated with worse impairment for all 4 disorders (but not significantly for depression and drug dependence); and (4) family history was associated with greater service use for all 4 disorders (but not significantly for anxiety disorder).
Family history was not associated with younger age at onset for any disorder. A number of explanations may be offered for this lack of association. First, our measures of age at onset may be flawed; one measure relied on repeated 1-year assessments with gaps between them, and the other measure relied on age at first mental health service use. Second, our sample may be too young—all were aged 32 years at the time of the most recent assessment—to detect associations between age at onset and family history (although there have been reports of associations with age at onset over the developmental period covered in the present study10,29,31,37,42). Third, it has been suggested that associations between age at onset and family history may be an artifact of clinic attendance, in that both early onset and having a strong family history might plausibly lead to treatment seeking.36 At least for depression, the literature is consistent with this view: the association between age at onset and family history appears to depend in part on whether a clinic sample was studied. For example, of the 26 studies we have identified that have found a significant association between age at onset and family history of depression,10,13,19–42 21 (81%) studied clinic samples.* In contrast, of 12 studies we identified that did not find a significant association between age at onset and family history of depression (the present study and 11 others9,11,62–70), only 5 (42%) studied clinic samples.62–64,66,67 It also remains possible that some methodologic feature that co-occurs with clinic sampling (eg, retrospective reporting) is responsible for the excess of significant associations reported by clinic studies.103 Further work may be needed to help determine why some studies find associations between family history and age at onset and some studies do not.
STRENGTHS
This study has a number of strengths. First, we presented results for several clinical indexes instead of just 1, enabling us to present a fuller clinical profile of individuals with a strong family history. Second, we presented results for 4 psychiatric disorders instead of focusing on just 1, enabling us to test the generality of family history associations. Elsewhere we have reported a strong relation between family history and childhood-onset persistent conduct disorder.104 Third, our family history measure was derived from reports from multiple informants, thus avoiding the underreporting associated with collecting reports from a single informant.77,78,92,93 Moreover, by collecting reports from multiple informants, we avoided biases associated with estimating family history solely from proband reports. That is, because informants with a disorder tend to over report that same disorder in family members,78,94–98 relying solely on probands as informants would result in artifactually inflated associations between family history and proband disorder outcomes. Fourth, our family history measure represented the proportion of family members with disorder as a continuous distribution. For some disorders, such measures have been shown to be more sensitive than measures that simply dichotomize participants as having or not having a family history.7
LIMITATIONS
Our findings should be interpreted in the context of the following limitations. First, our sample of probands consists primarily of white individuals born in New Zealand in 1972 and 1973, and replication in samples with different ethnicities and ages is necessary. Second, although we did our best to ensure the validity of family history reports (eg, by using a validated instrument and by obtaining reports from multiple informants), the validity of the family history screening method is known to be inferior to directly interviewing every relative.82,96,99–102 However, we used the family history screening method because it is an inexpensive way to collect psychiatric data on all relatives in a family. Collecting data on all family members is essential to avoid the undercounting bias associated with direct interviews, whereby relatives who can be interviewed have less psychopathology than those who cannot be interviewed because of death, estrangement, or unwillingness to take part.102 Third, we limited analyses to homotypic associations between family history and clinical indexes of disorder (eg, family history of depression with recurrence of depression). Heterotypic associations are of interest (eg, family history of depression with recurrence of anxiety), but are beyond the scope of the current paper. Fourth, our decision to analyze anxiety disorders as a group rather than separately precludes conclusions being drawn about specific anxiety disorders. We believe the strong cumulative comorbidity among anxiety disorders over the life course justifies studying anxiety disorders as 1 family.105 However, because panic disorder tends to begin later than other anxiety disorders, we reanalyzed our data excluding cases who had experienced panic disorder but no other anxiety disorder. Results were unaltered. Fifth, it is important to acknowledge that our data cannot resolve the direction of influence behind the reported associations between psychiatric family history and clinical feature of disorder. For example, although it is unlikely to completely account for the effect, the association between family history and mental health service use may in part arise because probands aware of their family history are quicker to seek treatment.106
IMPLICATIONS
There has been a recent revival of interest in the family history method both for public health screening and as a selection criterion for genetic research and imaging research, and in case-control studies to ensure that controls are free from familial disorder.107–110 Results from our study suggest 2 implications for this burgeoning area. First, from a public health perspective, family history may be useful for determining which patients will have the poorest prognosis. For example, among those with depression, anxiety disorder, alcohol dependence, and drug dependence, a family history screen may help determine whose illness will recur, whose illness will cause the greatest impairment, and who will be most likely to use treatment resources. Thus, family history may identify a subgroup in need of primary or early intervention, and for whom treatments appropriate for recurrent, highly disabling disorder may be needed.111 Second, selecting early-onset cases (ie, those whose onset is in their teens or 20s) may not necessarily result in the selection of homogeneous cases with a more familial or genetic form of disorder. Researchers may be better off selecting cases with recurrent disorder or those with high impairment of function or, better still, collecting family history information directly.
Acknowledgments
Funding/Support: This study was supported by grants MH45070, MH49414, and MH077874 from the National Institute of Mental Health, the Medical Research Council (G0100527), the William T. Grant Foundation, and the Health Research Council of New Zealand. Dr Caspi holds a Royal Society Wolfson Merit Award.
Footnotes
Author Contributions: Dr Milne takes responsibility for the integrity and accuracy of data reported herein. All authors had full access to the data.
Financial Disclosure: None reported.
Additional Contributions: We thank the Dunedin Study members and their families, unit research staff, Raewyn Crump, MPH, Wendy Slutske, PhD, Lucy Tully, DipClinPsy, and study founder Phil Silva, PhD.
References
- 1.Kendler KS, Davis KL, Kessler RC. The familial aggregation of common psychiatric and substance use disorders in the National Comorbidity Survey: a family history study. Br J Psychiatry. 1997;170:541–548. doi: 10.1192/bjp.170.6.541. [DOI] [PubMed] [Google Scholar]
- 2.Bierut LJ, Dinwiddie SH, Begleiter H, Crowe RR, Hesselbrock V, Nurnberger JI, Jr, Porjesz B, Schuckit MA, Reich T. Familial transmission of substance dependence: alcohol, marijuana, cocaine, and habitual smoking: a report from the Collaborative Study on the Genetics of Alcohol. Arch Gen Psychiatry. 1998;55 (11):982–988. doi: 10.1001/archpsyc.55.11.982. [DOI] [PubMed] [Google Scholar]
- 3.Sullivan PF, Neale MC, Kendler KS. Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry. 2000;157(10):1552–1562. doi: 10.1176/appi.ajp.157.10.1552. [DOI] [PubMed] [Google Scholar]
- 4.Hettema JM, Neale MC, Kendler KS. A review and meta-analysis of the genetic epidemiology of anxiety disorders. Am J Psychiatry. 2001;158(10):1568–1578. doi: 10.1176/appi.ajp.158.10.1568. [DOI] [PubMed] [Google Scholar]
- 5.Kendler KS, Diehl SR. The genetics of schizophrenia: a current, genetic-epidemiologic perspective. Schizophr Bull. 1993;19(2):261–285. doi: 10.1093/schbul/19.2.261. [DOI] [PubMed] [Google Scholar]
- 6.Brent DA, Mann JJ. Family genetic studies, suicide, and suicidal behavior. Am J Med Genet C Semin Med Genet. 2005;133C(1):13–24. doi: 10.1002/ajmg.c.30042. [DOI] [PubMed] [Google Scholar]
- 7.Milne BJ, Moffitt TE, Crump R, Poulton R, Rutter M, Sears MR, Taylor A, Caspi A. How should we construct psychiatric family history scores? a comparison of alternative approaches from the Dunedin Family Health History Study. Psychol Med. 2008;38(12):1793–1802. doi: 10.1017/S0033291708003115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Levinson DF. The genetics of depression: a review. Biol Psychiatry. 2006;60(2):84–92. doi: 10.1016/j.biopsych.2005.08.024. [DOI] [PubMed] [Google Scholar]
- 9.Klein DN, Lewinsohn PM, Rohde P, Seeley JR, Durbin CE. Clinical features of major depressive disorder in adolescents and their relatives: impact on familial aggregation, implications for phenotype definition, and specificity of transmission. J Abnorm Psychol. 2002;111(1):98–106. [PubMed] [Google Scholar]
- 10.Lieb R, Isensee B, Höfler M, Wittchen H-U. Parental depression and depression in offspring: evidence for familial characteristics and subtypes? J Psychiatr Res. 2002;36(4):237–246. doi: 10.1016/s0022-3956(02)00015-8. [DOI] [PubMed] [Google Scholar]
- 11.Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. Am J Psychiatry. 2006;163 (6):1001–1008. doi: 10.1176/ajp.2006.163.6.1001. [DOI] [PubMed] [Google Scholar]
- 12.Klein DN, Shankman SA, Rose S. Dysthymic disorder and double depression: prediction of 10-year course trajectories and outcomes. J Psychiatr Res. 2008;42(5):408–415. doi: 10.1016/j.jpsychires.2007.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tozzi F, Prokopenko I, Perry JD, Kennedy JL, McCarthy AD, Holsboer F, Berrettini W, Middleton LT, Chilcoat HD, Muglia P. Family history of depression is associated with younger age of onset in patients with recurrent depression. Psychol Med. 2008;38(5):641–649. doi: 10.1017/S0033291707002681. [DOI] [PubMed] [Google Scholar]
- 14.Manassis K, Hood J. Individual and familial predictors of impairment in childhood anxiety disorders. J Am Acad Child Adolesc Psychiatry. 1998;37(4):428–434. doi: 10.1097/00004583-199804000-00021. [DOI] [PubMed] [Google Scholar]
- 15.Penick EC, Powell BJ, Bingham SF, Liskow BI, Miller NS, Read MR. A comparative study of familial alcoholism. J Stud Alcohol. 1987;48(2):136–146. doi: 10.15288/jsa.1987.48.136. [DOI] [PubMed] [Google Scholar]
- 16.Araujo NP, Monteiro MG. Family history of alcoholism and psychiatric comorbidity in Brazilian male alcoholics and controls. Addiction. 1995;90(9):1205–1211. doi: 10.1046/j.1360-0443.1995.90912055.x. [DOI] [PubMed] [Google Scholar]
- 17.Caudill BD, Hoffman JA, Hubbard RL, Flynn PM, Luckey JW. Parental history of substance abuse as a risk factor in predicting crack smokers’ substance use, illegal activities, and psychiatric status. Am J Drug Alcohol Abuse. 1994;20(3):341–354. doi: 10.3109/00952999409106019. [DOI] [PubMed] [Google Scholar]
- 18.Weissman MM, Wickramaratne P, Adams PB, Lish JD, Horwath E, Charney D, Woods SW, Leeman E, Frosch E. The relationship between panic disorder and major depression: a new family study. Arch Gen Psychiatry. 1993;50(10):767–780. doi: 10.1001/archpsyc.1993.01820220017003. [DOI] [PubMed] [Google Scholar]
- 19.Kay D. Observationsonthenaturalhistoryandgeneticsofoldagepsychoses:aStockholm material, 1931–1937. Proc R Soc Med September. 1959;59:791–794. [Google Scholar]
- 20.Stendstedt A. Involutional melancholia. Acta Psychiatr Scand. 1959;33(suppl 127):5–71. [Google Scholar]
- 21.Winokur G, Cadoret RJ, Dorzab J, Baker M. Depressive disease: a genetic study. Arch Gen Psychiatry. 1971;24(2):135–144. doi: 10.1001/archpsyc.1971.01750080039006. [DOI] [PubMed] [Google Scholar]
- 22.Marten SA, Cadoret RJ, Winokur G, Ora E. Unipolar depression: a family history study. Biol Psychiatry. 1972;4(3):205–213. [PubMed] [Google Scholar]
- 23.Cadoret RJ, Woolson R, Winokur G. The relationship of age of onset in unipolar affective disorder to risk of alcoholism and depression in parents. J Psychiatr Res. 1977;13(3):137–142. doi: 10.1016/0022-3956(77)90002-4. [DOI] [PubMed] [Google Scholar]
- 24.Winokur G. Familial (genetic) subtypes of pure depressive disease. Am J Psychiatry. 1979;136(7):911–913. doi: 10.1176/ajp.136.7.911. [DOI] [PubMed] [Google Scholar]
- 25.Brown RP, Sweeney J, Loutsch E, Kocsis J, Frances A. Involutional melancholia revisited. Am J Psychiatry. 1984;141(1):24–28. doi: 10.1176/ajp.141.1.24. [DOI] [PubMed] [Google Scholar]
- 26.Weissman MM, Wickramaratne P, Merikangas KR, Leckman JF, Prusoff BA, Caruso KA, Kidd KK, Gammon GD. Onset of major depression in early adulthood: increased familial loading and specificity. Arch Gen Psychiatry. 1984;41(12):1136–1143. doi: 10.1001/archpsyc.1984.01790230022003. [DOI] [PubMed] [Google Scholar]
- 27.McGuffin P, Katz R, Bebbington P. Hazard, heredity and depression: a family study. J Psychiatr Res. 1987;21(4):365–375. doi: 10.1016/0022-3956(87)90083-5. [DOI] [PubMed] [Google Scholar]
- 28.Stancer HC, Persad E, Wagener DK, Jorna T. Evidence for homogeneity of major depression and bipolar affective disorder. J Psychiatr Res. 1987;21(1):37–53. doi: 10.1016/0022-3956(87)90007-0. [DOI] [PubMed] [Google Scholar]
- 29.Weissman MM, Gammon GD, John K, Merikangas KR, Warner V, Prusoff BA, Sholomskas D. Children of depressed parents: increased psychopathology and early onset of major depression. Arch Gen Psychiatry. 1987;44(10):847–853. doi: 10.1001/archpsyc.1987.01800220009002. [DOI] [PubMed] [Google Scholar]
- 30.Conwell Y, Nelson JC, Kim KM, Mazure CM. Depression in late life: age of onset as marker of a subtype. J Affect Disord. 1989;17(2):189–195. doi: 10.1016/0165-0327(89)90042-6. [DOI] [PubMed] [Google Scholar]
- 31.Kupfer DJ, Frank E, Carpenter LL, Neiswanger K. Family history in recurrent depression. J Affect Disord. 1989;17(2):113–119. doi: 10.1016/0165-0327(89)90033-5. [DOI] [PubMed] [Google Scholar]
- 32.Brodaty H, Peters K, Boyce P, Hickie I, Parker G, Mitchell P, Wilhelm K. Age and depression. J Affect Disord. 1991;23(3):137–149. doi: 10.1016/0165-0327(91)90026-o. [DOI] [PubMed] [Google Scholar]
- 33.Maier W, Lichtermann D, Minges J, Heun R, Hallmayer J, Klingler T. Unipolar depression in the aged: determinants of familial aggregation. J Affect Disord. 1991;23(2):53–61. doi: 10.1016/0165-0327(91)90092-7. [DOI] [PubMed] [Google Scholar]
- 34.Neuman RJ, Geller B, Rice JP, Todd RD. Increased prevalence and earlier onset of mood disorders among relatives of prepubertal versus adult probands. J Am Acad Child Adolesc Psychiatry. 1997;36(4):466–473. doi: 10.1097/00004583-199704000-00008. [DOI] [PubMed] [Google Scholar]
- 35.Wickramaratne PJ, Weissman MM. Onset of psychopathology in offspring by developmental phase and parental depression. J Am Acad Child Adolesc Psychiatry. 1998;37(9):933–942. doi: 10.1097/00004583-199809000-00013. [DOI] [PubMed] [Google Scholar]
- 36.Kendler KS, Gardner CO, Prescott CA. Clinical characteristic of major depression that predict risk of depression in relatives. Arch Gen Psychiatry. 1999;56(4):322–327. doi: 10.1001/archpsyc.56.4.322. [DOI] [PubMed] [Google Scholar]
- 37.Klein DN, Schatzberg AF, McCullough JP, Dowling F, Goodman D, Howland RH, Markowitz JC, Smith C, Thase ME, Rush AJ, LaVange L, Harrison WM, Keller MB. Age of onset in chronic major depression: relation to demographic and clinical variables, family history, and treatment response. J Affect Disord. 1999;55(2–3):149–157. doi: 10.1016/s0165-0327(99)00020-8. [DOI] [PubMed] [Google Scholar]
- 38.Parker G, Roy K, Hadzi-Pavlovic D, Mitchell P, Wilhelm K. Distinguishing early and late onset non-melancholic unipolar depression. J Affect Disord. 2003;74(2):131–138. doi: 10.1016/s0165-0327(02)00002-2. [DOI] [PubMed] [Google Scholar]
- 39.Benazzi F. Early onset vs late onset non-psychotic, non-melancholic unipolar depression. Int J Geriatr Psychiatry. 2004;19(7):701–703. doi: 10.1002/gps.1088. [DOI] [PubMed] [Google Scholar]
- 40.Kendler KS, Gatz M, Gardner CO, Pedersen NL. Age at onset and familial risk for major depression in a Swedish national twin sample. Psychol Med. 2005;35 (11):1573–1579. doi: 10.1017/S0033291705005714. [DOI] [PubMed] [Google Scholar]
- 41.Nierenberg AA, Trivedi MH, Fava M, Biggs MM, Shores-Wilson K, Wisniewski SR, Balasubramani GK, Rush AJ. Family history of mood disorder and characteristics of major depressive disorder: a STAR*D (Sequenced Treatment Alternatives to Relieve Depression) study. J Psychiatr Res. 2007;41(3–4):214–221. doi: 10.1016/j.jpsychires.2006.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zisook S, Rush AJ, Lesser I, Wisniewski SR, Trivedi M, Husain MM, Balasubramani GK, Alpert JE, Fava M. Preadult onset vs. adult onset of major depressive disorder: a replication study. Acta Psychiatr Scand. 2007;115(3):196–205. doi: 10.1111/j.1600-0447.2006.00868.x. [DOI] [PubMed] [Google Scholar]
- 43.Battaglia M, Bertella S, Politi E, Bernardeschi L, Perna G, Gabriele A, Bellodi L. Age at onsetofpanicdisorder:influenceoffamilialliabilitytothediseaseandofchild-hood separation anxiety disorder. Am J Psychiatry. 1995;152(9):1362–1364. doi: 10.1176/ajp.152.9.1362. [DOI] [PubMed] [Google Scholar]
- 44.Goldstein RB, Wickramaratne PJ, Horwath E, Weissman MM. Familial aggregation and phenomenology of “early”-onset (at or before age 20 years) panic disorder. Arch Gen Psychiatry. 1997;54(3):271–278. doi: 10.1001/archpsyc.1997.01830150097014. [DOI] [PubMed] [Google Scholar]
- 45.Pauls DL, Alsobrook JI, II, Goodman W, Rasmussen S, Leckman JF. A family study of obsessive compulsive disorder. Am J Psychiatry. 1995;152(1):76–84. doi: 10.1176/ajp.152.1.76. [DOI] [PubMed] [Google Scholar]
- 46.Seguí J, Márquez M, Garcia L, Canet J, Salvador-Carulla L, Ortiz M. Differential clinical features of early-onset panic disorder. J Affect Disord. 1999;54(1–2):109–117. doi: 10.1016/s0165-0327(98)00148-7. [DOI] [PubMed] [Google Scholar]
- 47.Nestadt G, Samuels J, Riddle M, Bienvenu OJ, III, Liang KY, LaBuda M, Walkup J, Grados M, Hoehn-Saric R. A family study of obsessive-compulsive disorder. Arch Gen Psychiatry. 2000;57(4):358–363. doi: 10.1001/archpsyc.57.4.358. [DOI] [PubMed] [Google Scholar]
- 48.Delorme R, Golmard JL, Chabane N, Millet B, Krebs MO, Mouren-Simeoni MC, Leboyer M. Admixture analysis of age at onset in obsessive-compulsive disorder. Psychol Med. 2005;35(2):237–243. doi: 10.1017/s0033291704003253. [DOI] [PubMed] [Google Scholar]
- 49.Volicer BJ, Volicer L, D’Angelo N. Variation in length of time to development of alcoholism by family history of problem drinking. Drug Alcohol Depend. 1983;12(1):69–83. doi: 10.1016/0376-8716(83)90055-8. [DOI] [PubMed] [Google Scholar]
- 50.Atkinson RM, Turner JA, Kofoed LL, Tolson RL. Early versus late onset alcoholism in older persons: preliminary findings. Alcohol Clin Exp Res. 1985;9(6):513–515. doi: 10.1111/j.1530-0277.1985.tb05594.x. [DOI] [PubMed] [Google Scholar]
- 51.Latcham RW. Familial alcoholism: evidence from 237 alcoholics. Br J Psychiatry. 1985;147:54–57. doi: 10.1192/bjp.147.1.54. [DOI] [PubMed] [Google Scholar]
- 52.Atkinson RM, Tolson RL, Turner JA. Late versus early onset problem drinking in older men. Alcohol Clin Exp Res. 1990;14(4):574–579. doi: 10.1111/j.1530-0277.1990.tb01203.x. [DOI] [PubMed] [Google Scholar]
- 53.Blankfield A. Female alcoholics, II: the expression of alcoholism in relation to gender and age. Acta Psychiatr Scand. 1990;81(5):448–452. doi: 10.1111/j.1600-0447.1990.tb05479.x. [DOI] [PubMed] [Google Scholar]
- 54.Worobec TG, Turner WM, O’Farrell TJ, Cutter HS, Bayog RD, Tsuang MT. Alcohol use by alcoholics with and without a history of parental alcoholism. Alcohol Clin Exp Res. 1990;14(6):887–892. doi: 10.1111/j.1530-0277.1990.tb01832.x. [DOI] [PubMed] [Google Scholar]
- 55.Svanum S, McAdoo WG. Parental alcoholism: an examination of male and female alcoholics in treatment. J Stud Alcohol. 1991;52(2):127–132. doi: 10.15288/jsa.1991.52.127. [DOI] [PubMed] [Google Scholar]
- 56.Turner WM, Cutter HSG, Worobec TG, O’Farrell TJ, Bayog RD, Tsuang MT. Family history models of alcoholism: age of onset, consequences and dependence. J Stud Alcohol. 1993;54(2):164–171. doi: 10.15288/jsa.1993.54.164. [DOI] [PubMed] [Google Scholar]
- 57.Dawson DA. The link between family history and early onset alcoholism: earlier initiation of drinking or more rapid development of dependence? J Stud Alcohol. 2000;61(5):637–646. doi: 10.15288/jsa.2000.61.637. [DOI] [PubMed] [Google Scholar]
- 58.Johnson BA, Cloninger CJ, Roache JD, Bordnick PS, Ruiz P. Age of onset as a discriminator between alcoholic subtypes in a treatment-seeking outpatient population. Am J Addict. 2000;9(1):17–27. doi: 10.1080/10550490050172191. [DOI] [PubMed] [Google Scholar]
- 59.Lieb R, Merikangas KR, Hofler M, Pfister H, Isensee B, Wittchen H-U. Parental alcohol use disorders and alcohol use and disorders in offspring: a community study. Psychol Med. 2002;32(1):63–78. doi: 10.1017/s0033291701004883. [DOI] [PubMed] [Google Scholar]
- 60.Chaudhry HR, Arria A, Tarter RE, Chaudhry S, Chaudhry N. Familial history of opium use and reported problems among opium addicts in Pakistan. Br J Addict. 1991;86(6):785–788. doi: 10.1111/j.1360-0443.1991.tb03105.x. [DOI] [PubMed] [Google Scholar]
- 61.Day NL, Goldschmidt L, Thomas CA. Prenatal marijuana exposure contributes to the prediction of marijuana use at age 14. Addiction. 2006;101(9):1313–1322. doi: 10.1111/j.1360-0443.2006.01523.x. [DOI] [PubMed] [Google Scholar]
- 62.Gershon ES, Mark A, Cohen N, Belizon N, Baron M, Knobe KE. Transmitted factors in the morbid risk of affective disorders: a controlled study. J Psychiatr Res. 1975;12(4):283–299. [Google Scholar]
- 63.Mendlewicz J, Baron M. Morbidity risks in subtypes of unipolar depressive illness: differences between early and late onset forms. Br J Psychiatry. 1981;139:463–466. doi: 10.1192/bjp.139.5.463. [DOI] [PubMed] [Google Scholar]
- 64.Greenwald BS, Kramer-Ginsberg E. Age at onset in geriatric depression: relationship to clinical variables. J Affect Disord. 1988;15(1):61–68. doi: 10.1016/0165-0327(88)90010-9. [DOI] [PubMed] [Google Scholar]
- 65.Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. The clinical characteristics of major depression as indices of the familial risk to illness. Br J Psychiatry. 1994;165(2):66–72. doi: 10.1192/bjp.165.1.66. [DOI] [PubMed] [Google Scholar]
- 66.Harrington R, Rutter M, Weissman MM, Fudge H, Groothues C, Bredenkamp D, Pickles A, Rende R, Wickramaratne P. Psychiatric disorders in the relatives of depressed probands, I: comparison of prepubertal, adolescent and early adult onset cases. J Affect Disord. 1997;42(1):9–22. doi: 10.1016/s0165-0327(96)00091-2. [DOI] [PubMed] [Google Scholar]
- 67.Johnson L, Andersson-Lundman G, Aberg-Wistedt A, Mathé AA. Age of onset in affective disorder: its correlation with hereditary and psychosocial factors. J Affect Disord. 2000;59(2):139–148. doi: 10.1016/s0165-0327(99)00146-9. [DOI] [PubMed] [Google Scholar]
- 68.Wickramaratne PJ, Greenwald S, Weissman MM. Psychiatric disorders in the relatives of probands with prepubertal-onset or adolescent-onset major depression. J Am Acad Child Adolesc Psychiatry. 2000;39(11):1396–1405. doi: 10.1097/00004583-200011000-00014. [DOI] [PubMed] [Google Scholar]
- 69.Birmaher B, Williamson DE, Dahl JP, Axelson DA, Kaufman J, Dorn LD, Ryan ND. Clinical presentation and course of depression in youth: does onset in childhood differ from onset in adolescence? J Am Acad Child Adolesc Psychiatry. 2004;43(1):63–70. doi: 10.1097/00004583-200401000-00015. [DOI] [PubMed] [Google Scholar]
- 70.Zimmermann P, Brückl T, Lieb R, Nocon A, Ising M, Beesdo K, Wittchen H-U. The interplay of familial depression liability and adverse events in predicting the first onset of depression during a 10-year follow-up. Biol Psychiatry. 2008;63(4):406–414. doi: 10.1016/j.biopsych.2007.05.020. [DOI] [PubMed] [Google Scholar]
- 71.Schreier A, Wittchen H-U, Höfler M, Lieb R. Anxiety disorders in mothers and their children: prospective longitudinal community study. Br J Psychiatry. 2008;192(4):308–309. doi: 10.1192/bjp.bp.106.033589. [DOI] [PubMed] [Google Scholar]
- 72.Stabenau JR. Implications of family history of alcoholism, antisocial personality, and sex differences in alcohol dependence. Am J Psychiatry. 1984;141(10):1178–1182. doi: 10.1176/ajp.141.10.1178. [DOI] [PubMed] [Google Scholar]
- 73.Cook BL, Winokur G. A family study of familial positive vs. familial negative alcoholics. J Nerv Ment Dis. 1985;173(3):175–178. doi: 10.1097/00005053-198503000-00007. [DOI] [PubMed] [Google Scholar]
- 74.Weissman MM, Wolk S, Goldstein RB, Moreau D, Adams P, Greenwald S, Klier CM, Ryan ND, Dahl RE, Wickramaratne P. Depressed adolescents grown up. JAMA. 1999;281(18):1707–1713. doi: 10.1001/jama.281.18.1707. [DOI] [PubMed] [Google Scholar]
- 75.Fergusson DM, Boden JM, Horwood LJ. Recurrence of major depression in adolescence and early adulthood, and later mental health, educational and economic outcomes. Br J Psychiatry. 2007;191:335–342. doi: 10.1192/bjp.bp.107.036079. [DOI] [PubMed] [Google Scholar]
- 76.Moffitt TE, Caspi A, Rutter M, Silva PA. Sex Differences in Antisocial Behaviour: Conduct Disorder, Delinquency, and Violence in the Dunedin Longitudinal Study. Cambridge, England: Cambridge University Press; 2001. [Google Scholar]
- 77.Weissman MM, Wickramaratne P, Adams P, Wolk S, Verdeli H, Olfson M. Brief screening for family psychiatric history: the family history screen. Arch Gen Psychiatry. 2000;57(7):675–682. doi: 10.1001/archpsyc.57.7.675. [DOI] [PubMed] [Google Scholar]
- 78.Milne BJ, Caspi A, Crump R, Poulton R, Rutter M, Sears MR, Moffitt TE. The validity of the family history screen for assessing family history of mental disorders. Am J Med Genet B Neuropsychiatr Genet. 2009;150B(1):41–49. doi: 10.1002/ajmg.b.30764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Selzer ML, Vinokur A, Van Rooijen L. A self-administered Short Michigan Alcoholism Screening Test (SMAST) J Stud Alcohol. 1975;36(1):117–126. doi: 10.15288/jsa.1975.36.117. [DOI] [PubMed] [Google Scholar]
- 80.Skinner HA. The drug abuse screening test. Addict Behav. 1982;7(4):363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- 81.Robins LN, Cottler L, Bucholz K, Compton W. Diagnostic Interview Schedule for DSM-IV. St Louis, MO: Washington University Press; 1995. [Google Scholar]
- 82.Vandeleur CL, Rothen S, Jeanpretre N, Lustenberger Y, Gamma F, Ayer E, Ferrero F, Fleischmann A, Besson J, Sisbane F, Preisig M. Inter-informant agreement and prevalence estimates for substance use disorders: direct interview versus family history method. Drug Alcohol Depend. 2008;92(1–3):9–19. doi: 10.1016/j.drugalcdep.2007.05.023. [DOI] [PubMed] [Google Scholar]
- 83.Costello A, Edelbrock C, Kalas R, Kessler M, Klaric S. Diagnostic Interview Schedule for Children (DISC) Rockville, MD: National Institute of Mental Health; 1982. [Google Scholar]
- 84.Robins LN, Helzer HE, Croughan J, Ratcliff KS. National Institute of Mental Health Diagnostic Interview Schedule: its history, characteristics, and validity. Arch Gen Psychiatry. 1981;38(4):381–389. doi: 10.1001/archpsyc.1981.01780290015001. [DOI] [PubMed] [Google Scholar]
- 85.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3. Washington, DC: American Psychiatric Association; 1980. [Google Scholar]
- 86.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3. Washington, DC: American Psychiatric Association; 1987. revised. [Google Scholar]
- 87.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 88.Caspi A, Moffitt TE, Thornton A, Freedman D, Amell JM, Harrington H, Smeijers J, Silva PA. The life history calendar: a research and clinical assessment method for collecting retrospective event-history data. Int J Methods Psychiatr Res. 1996;6(2):101–114. [Google Scholar]
- 89.Belli RF, Shay WL, Stafford FP. Event history calendars and question list surveys: a direct comparison of interviewing methods. Public Opin Q. 2001;65 (1):45–74. doi: 10.1086/320037. [DOI] [PubMed] [Google Scholar]
- 90.Moffitt TE, Harrington H, Caspi A, Kim-Cohen J, Goldberg D, Gregory AM, Poulton R. Depression and generalised anxiety disorder: cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Arch Gen Psychiatry. 2007;64(6):651–660. doi: 10.1001/archpsyc.64.6.651. [DOI] [PubMed] [Google Scholar]
- 91.Stata Statistical Software: Release 9.1. College Station, TX: StataCorp; 2005. [Google Scholar]
- 92.Kosten TA, Anton SF, Rounsaville BJ. Ascertaining psychiatric diagnoses with the family history method in a substance abuse population. J Psychiatr Res. 1992;26(2):135–147. doi: 10.1016/0022-3956(92)90005-9. [DOI] [PubMed] [Google Scholar]
- 93.Hardt J, Franke P. Validity, reliability and objectivity of the family history method in psychiatry: a meta analysis. Eur Psychiatry. 2007;22(1):49–58. doi: 10.1016/j.eurpsy.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 94.Kendler KS, Silberg JL, Neale MC, Kessler RC, Heath AC, Eaves LJ. The family history method: whose psychiatric history is measured? Am J Psychiatry. 1991;148(11):1501–1504. doi: 10.1176/ajp.148.11.1501. [DOI] [PubMed] [Google Scholar]
- 95.Chapman TF, Mannuzza S, Klein DF, Fyer AJ. Effects of informant mental disorder on psychiatric family history data. Am J Psychiatry. 1994;151(4):574–579. doi: 10.1176/ajp.151.4.574. [DOI] [PubMed] [Google Scholar]
- 96.Roy M-A, Walsh D, Kendler KS. Accuracies and inaccuracies of the family history method: a multivariate approach. Acta Psychiatr Scand. 1996;93(4):224–234. doi: 10.1111/j.1600-0447.1996.tb10639.x. [DOI] [PubMed] [Google Scholar]
- 97.Heun R, Maier W, Müller H. Subject and informant variables affecting family history diagnoses of depression and dementia. Psychiatry Res. 1997;71 (3):175–180. doi: 10.1016/s0165-1781(97)00058-9. [DOI] [PubMed] [Google Scholar]
- 98.Coelho HF, Cooper PJ, Murray L. Impact of psychiatric disturbance on identifying psychiatric disorder in relatives: study of mothers and daughters. Br J Psychiatry. 2006;188:288–289. doi: 10.1192/bjp.bp.105.010447. [DOI] [PubMed] [Google Scholar]
- 99.Orvaschel H, Thompson WD, Belanger A, Prusoff BA, Kidd KK. Comparison of the family history method to direct interview: factors affecting the diagnosis of depression. J Affect Disord. 1982;4(1):49–59. doi: 10.1016/0165-0327(82)90019-2. [DOI] [PubMed] [Google Scholar]
- 100.Andreasen NC, Rice J, Endicott J, Reich T, Coryell W. The family history approach to diagnosis: how useful is it? Arch Gen Psychiatry. 1986;43(5):421–429. doi: 10.1001/archpsyc.1986.01800050019002. [DOI] [PubMed] [Google Scholar]
- 101.Rice JP, Reich T, Bucholz K, Neuman RJ, Fishman R, Rochberg N, Hesselbrock VM, Nurnberger JJ, Jr, Schuckit MA, Begleiter H. Comparison of direct interview and family history diagnoses of alcohol dependence. Alcohol Clin Exp Res. 1995;19(4):1018–1023. doi: 10.1111/j.1530-0277.1995.tb00983.x. [DOI] [PubMed] [Google Scholar]
- 102.Davies NJ, Sham PC, Gilvarry C, Jones PB, Murray RM. Comparison of the family history with the family study method: report from the Camberwell Collaborative Psychosis Study. Am J Med Genet. 1997;74(1):12–17. doi: 10.1002/(sici)1096-8628(19970221)74:1<12::aid-ajmg3>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 103.Cohen P, Cohen J. The clinician’s illusion. Arch Gen Psychiatry. 1984;41(12):1178–1182. doi: 10.1001/archpsyc.1984.01790230064010. [DOI] [PubMed] [Google Scholar]
- 104.Odgers CL, Milne BJ, Caspi A, Crump R, Poulton R, Moffitt TE. Predicting prognosis for the conduct-problem boy: can family history help? J Am Acad Child Adolesc Psychiatry. 2007;46(10):1240–1249. doi: 10.1097/chi.0b013e31813c6c8d. [DOI] [PubMed] [Google Scholar]
- 105.Gregory AM, Caspi A, Moffitt TE, Koenen K, Eley TC, Poulton R. Juvenile mental health histories of adults with anxiety disorders. Am J Psychiatry. 2007;164(2):301–308. doi: 10.1176/ajp.2007.164.2.301. [DOI] [PubMed] [Google Scholar]
- 106.Kendler KS. Is seeking treatment for depression predicted by a history of depression in relatives? implications for family studies of affective disorders. Psychol Med. 1995;25(4):807–814. doi: 10.1017/s0033291700035054. [DOI] [PubMed] [Google Scholar]
- 107.Yoon PW, Scheuner MT, Peterson-Oehlke KL, Gwinn M, Faucett A, Khoury MJ. Can family history be used as a tool for public health and preventive medicine? Genet Med. 2002;4(4):304–310. doi: 10.1097/00125817-200207000-00009. [DOI] [PubMed] [Google Scholar]
- 108.Thompson D, Witte JS, Slattery M, Goldgar D. Increased power for case-control studies of single nucleotide polymorphisms through incorporation of family history and genetic constraints. Genet Epidemiol. 2004;27(3):215–224. doi: 10.1002/gepi.20018. [DOI] [PubMed] [Google Scholar]
- 109.Prescott CA, Sullivan PF, Myers JM, Patterson DG, Devitt M, Halberstadt LJ, Walsh D, Kendler KS. The Irish Affected Sib Pair Study of Alcohol Dependence: study methodology and validation of diagnosis by interview and family history. Alcohol Clin Exp Res. 2005;29(3):417–429. doi: 10.1097/01.alc.0000156085.50418.07. [DOI] [PubMed] [Google Scholar]
- 110.Chen X, Wang X, Hossain S, O’Neill FA, Walsh D, van den Oord E, Fanous A, Kendler KS. Interleukin 3 and schizophrenia: the impact of sex and family history. Mol Psychiatry. 2007;12(3):273–282. doi: 10.1038/sj.mp.4001932. [DOI] [PubMed] [Google Scholar]
- 111.Kornstein SG. Maintenance therapy to prevent recurrence of depression: summary and implications of the PREVENT study. Expert Rev Neurother. 2008;8(5):737–742. doi: 10.1586/14737175.8.5.737. [DOI] [PubMed] [Google Scholar]