Abstract
Purpose
Extensive attention has been focused on improving the dietary intake of Americans. Such focus is warranted due to increasing rates of overweight, obesity, and other dietary-related disease. To address suboptimal dietary intake requires an improved, contextualized understanding of the multiple and intersecting influences on healthy eating, particularly among those populations at greatest risk of and from poor diet, including rural residents.
Methods
During 8 focus groups (N=99) and 6 group key informant interviews (N=20), diverse Appalachian rural residents were queried about their perceptions of healthy eating, determinants of healthy food intake, and recommendations for improving the dietary intake of people in their communities. Participants included church members and other laypeople, public health officials, social service providers, health care professionals, and others.
Findings
Participants offered insights on healthy eating consistent with the categories of individual, interpersonal, community, physical, environmental and society-level influences described in the socioecological model. Although many participants identified gaps in dietary knowledge as a persistent problem, informants also identified extra-individual factors, including the influence of family, fellow church members, and schools, policy, advertising and media, and general societal trends, as challenges to healthy dietary intake. We highlight Appalachian residents’ recommendations for promoting healthier diets, including support groups, educational workshops, cooking classes, and community gardening.
Conclusions
We discuss the implications of these findings for programmatic development in the Appalachian context.
Keywords: dietary intake, health disparities, qualitative research, rural
Most Americans consume far below the recommended daily intake (RDI) for fruits and vegetables and far above the RDI for suboptimal foods.1–3 Such dietary patterns have been linked to overweight and obesity, metabolic syndrome, and other chronic conditions.4 Rural residents are more likely than their urban counterparts to experience these conditions, oftentimes leading to premature mortality.5 Social determinants, including lower socioeconomic status, lower likelihood of health insurance coverage, and more limited access to safety net and preventive medical services, place rural residents at elevated risk of and from these chronic conditions.6
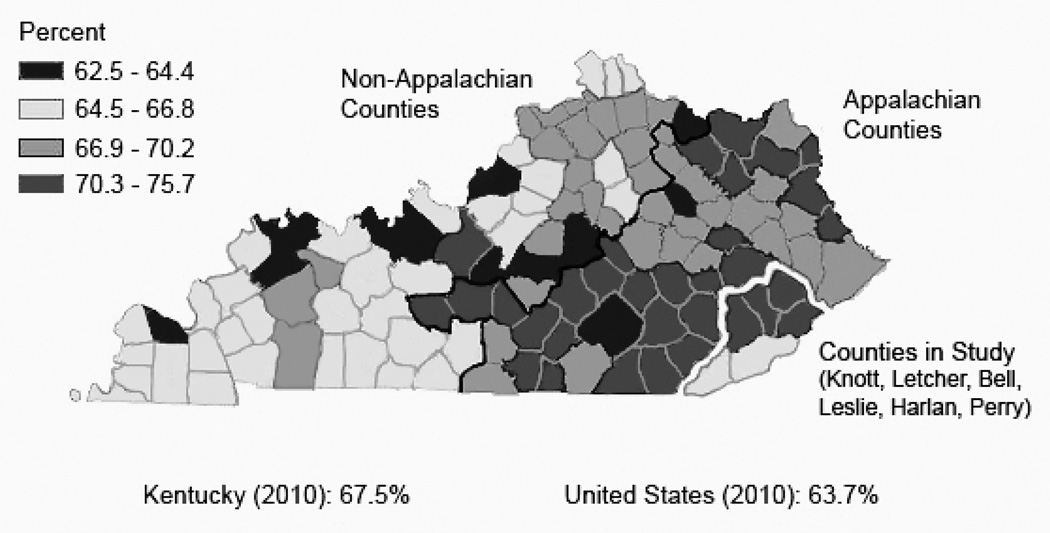
Kentucky residents, particularly those living in the rural, Appalachian portion of the state, suffer even higher rates of overweight, obesity, and associated chronic conditions than other rural residents.7 In 2005, 62.5% of adults in Kentucky were overweight or obese, as compared to 58.5% for the United States.8 Residents of the eastern Appalachian portion of Kentucky have among the highest rates of obesity and overweight in the United States, estimated between 62.5% and 76.2% (See Figure 1, which also highlights study counties. Data obtained from the CDC’s Behavioral Risk Factor Surveillance System).8–10 Rates of diabetes and cardiovascular disease in Appalachian counties in Kentucky also are among the highest in the state and the United States.10–12
Figure 1.
Overweight and Obesity Among Adults in Kentucky 2008–2010
Likely associated with these negative health outcomes, Kentucky ranks third nationally for those least likely to consume the RDI of fruits and vegetables; only 21.1% of Kentuckians and 19% of Appalachian residents meet this RDI, compared with 23.4% of Americans nationwide.13 In part, these consumption patterns stem from regional food ways, which tend to emphasize meats, biscuits, and fried foods over vegetables; these food preferences have become important components of rural Appalachian identities.15 Common uses of locally acquired ingredients and methods of preparation shared among rural Appalachians serve as an expression of belonging that not only reaffirms cultural ties to place, but also to family and community.14 The preference for these unhealthy foods among rural Appalachians, including the expectation that these culturally appropriate foods should be present at home and community events, has been identified as a potential barrier for individuals in the region to making healthy dietary choices.15
Dietary patterns in rural Appalachia also are shaped by a broad range of interacting social, cultural, geographical, and economic processes. For instance, some research has suggested that the economic transition in the region from farming and mining to employment in the service industry has contributed to a rising dependence on fast foods.16 Coupled with issues of food affordability,15 limited access to high-quality grocery stores,17 and increased demands on the use of time, the spiking number of fast food establishments in rural Appalachian communities has been met with a corresponding dependence on these foods in regional diets. This dependence sometimes supplants former food practices which are viewed as more time intensive to prepare.12
Given that Appalachian residents experience disproportionate risk of overweight, obesity, and associated negative health outcomes, new approaches to improve dietary intake are needed. These approaches will be most successful if they are grounded in local perspectives and address the interactions between regional food ways and shifting social, cultural, and economic contexts. Thus, the purpose of this article is to explore how rural, Appalachian residents think about healthy eating and their ideas for improving dietary intake.
METHODS
We used focus groups and group key informant interviews to understand how local residents think about food and gain insights into program development. Human subjects and research protocols, measures, and analytic procedures were similar between the focus groups and the group key informant interviews, with a few variations in sampling approach (focus group members were primarily recruited through churches while key informants were recruited through a purposive snowball approach), discussion guides (there was one additional question for the key informants about their professional perspectives of previous community programming to increase healthy diet), honoraria ($25 for focus group participants, a meal for key informants), and meeting location (focus groups convened at churches or community centers and key informant interviews convened at the public health department or library). Focus groups also differed from key informant interviews in the perspectives sought; focus groups provided general, lay insights and key informant interviews gathered insights from people with specialized knowledge of the community.18 All participants signed informed consent forms prior to participating in this study. Protocols were approved by the University of Kentucky Institutional Review Board.
Study Setting
Appalachia is a geographically and culturally diverse region of 410 counties in 13 states that contains nearly 22 million people, or 8.3% of the total United States population.19 Appalachian Kentucky counties have socioeconomic status indicators among the lowest in the United States. In 2006, the Appalachian poverty rate was nearly twice that of the nation as a whole and the per capita income slightly more than half the United States’ average. Forty-one of the 54 Appalachian counties in Kentucky, including all of those where this project took place, are considered “distressed” counties by the Appalachian Regional Commission and persistent poverty counties by the United States Department of Agriculture.20 Pertaining to rural designation, 5 of the 6 counties in this study are classified as 9 (out of a possible 9, indicating “completely rural not adjacent to a metropolitan area”) on the Rural-Urban Continuum Codes (Beale Codes), and one county t is considered a 7 (“urban population of 2,500 to 19,999, not adjacent to a metro area”).21
Sample
We primarily recruited focus group participants through our existing partnerships with community churches enhanced by a snowball sampling approach. Churches were selected as a community partner, as they tend to be diverse and well-attended.22, 23 Although faith-based recruitment strategies may bias samples toward those who are members of churches, most Eastern Kentucky residents are affiliated with a local church. Furthermore, the minority of residents not associated with a church tend to be closely associated with someone who attends a church. Moreover, our previous work has shown that primarily recruiting through churches provides a diverse array of participants (socioeconomic status, race/ethnicity, sex, etc.).16, 24, 25
Our community-based research staff first approached the minister of a church to describe the research opportunity and gauge interest. If interested, the minister was given a written description of the study to read during a church event (Sunday services, Bible study, etc.) and our staff was present to record the names of those interested in participating. One week prior to convening the focus group, potential participants were called and told that they should feel welcome to bring anyone else they wished to bring as long as he or she met the inclusion criteria (18 years of age or older, residents of Appalachia, and willing and able to participate in a focus group). This snowball approach allowed us to recruit non-church members, approximately 20% of each focus group.
Theoretical saturation principles guided our sample size,26 and a total of 8 focus groups, composed of 99 participants (See Table 1 for focus group participant characteristics), were conducted before reaching saturation. Focus groups were held in local churches and community centers. Groups ranged in size from 8 to 14 participants, with most focus groups averaging 12 participants.
Table 1.
Combined Focus Group Sample Characteristics (N = 99)
| Variable | Frequency | Percent | |
|---|---|---|---|
| Sex | |||
| Male | 28 | 28 | |
| Female | 71 | 72 | |
| Age | |||
| 18–30 | 12 | 12 | |
| 31–40 | 10 | 10 | |
| 41–50 | 22 | 22 | |
| 51–60 | 21 | 21 | |
| 61–70 | 24 | 24 | |
| 71+ | 10 | 10 | |
| Race | |||
| White | 88 | 88 | |
| African-American | 9 | 9 | |
| Other | 2 | 2 | |
| Education | |||
| Ninth grade or less | 7 | 7 | |
| Some High school | 12 | 12 | |
| High school graduate | 40 | 40 | |
| More than High school | 40 | 40 | |
| Marital Status | |||
| Married | 64 | 64 | |
| Separated/Divorced/Never married | 22 | 22 | |
| Widowed | 13 | 13 | |
| Perceived Income Adequacy | |||
| Struggle to get by | 24 | 24 | |
| Enough to get by | 47 | 47 | |
| More than I need | 24 | 24 | |
| Unable/unwilling to say | 4 | 4 | |
| Actual income | |||
| Under $10,000 | 20 | 20 | |
| $10,0001 – 20,000 | 12 | 12 | |
| $20,001–30,000 | 21 | 21 | |
| $30,001–40,000 | 9 | 9 | |
| Over $40,001 | 26 | 26 | |
| Unable/unwilling to say | 11 | 11 | |
| Perceived Health Status | |||
| Excellent | 5 | 5 | |
| Very good | 28 | 28 | |
| Good | 43 | 43 | |
| Fair | 19 | 19 | |
| Poor | 4 | 4 | |
Six group key informant interviews were conducted with 20 stakeholders from diverse locations, including churches (minister(s) or designees), social service, and health care agencies. (See Table 2 for key informant description). Key informants were selected through snowball sampling, with theoretical saturation guiding our sample size. Our community staff identified several key community stakeholders and requested their participation in a discussion group; the initial key informants were then asked to recommend other relevant individuals who might have important contributions to the discussion. In addition to age criteria (18 and older) and willingness to participate, key informant inclusion criteria also included specialized knowledge of healthy eating, historical perspectives on Appalachian diets, and familiarity with the community. Key informant group interviews ranged in size from 2 to 6 participants. Prior to initiating the focus group or group key informant interview, trained staff administered informed consent protocols.
Table 2.
Combined Group Key Informant Sample Characteristics (N = 20)
| Variable | Frequency | Percent | |
|---|---|---|---|
| Sex | |||
| Male | 2 | 10 | |
| Female | 18 | 90 | |
| Age | |||
| 18–30 | 7 | 35 | |
| 31–50 | 6 | 30 | |
| 51+ | 7 | 35 | |
| Race | |||
| White | 18 | 90 | |
| African-American | 2 | 10 | |
| Education | |||
| High school or less | 5 | 25 | |
| Some college | 4 | 20 | |
| College graduate | 5 | 25 | |
| Graduate school | 6 | 30 | |
| Marital Status | |||
| Married | 13 | 65 | |
| Separated/Divorced/Never married | 6 | 30 | |
| Widowed | 1 | 5 | |
| Perceived Income Adequacy | |||
| Struggle to get by | 4 | 20 | |
| Enough to get by | 9 | 45 | |
| More than I need | 7 | 35 | |
| Actual income | |||
| Under $20,000 | 6 | 30 | |
| $20,001–35,000 | 7 | 35 | |
| $35,001–50,000 | 4 | 20 | |
| Over $50,001 | 3 | 15 | |
| Perceived Health Status | |||
| Excellent | 3 | 15 | |
| Very good | 6 | 30 | |
| Good | 7 | 35 | |
| Fair | 3 | 15 | |
| Poor | 1 | 5 | |
Discussion Guide
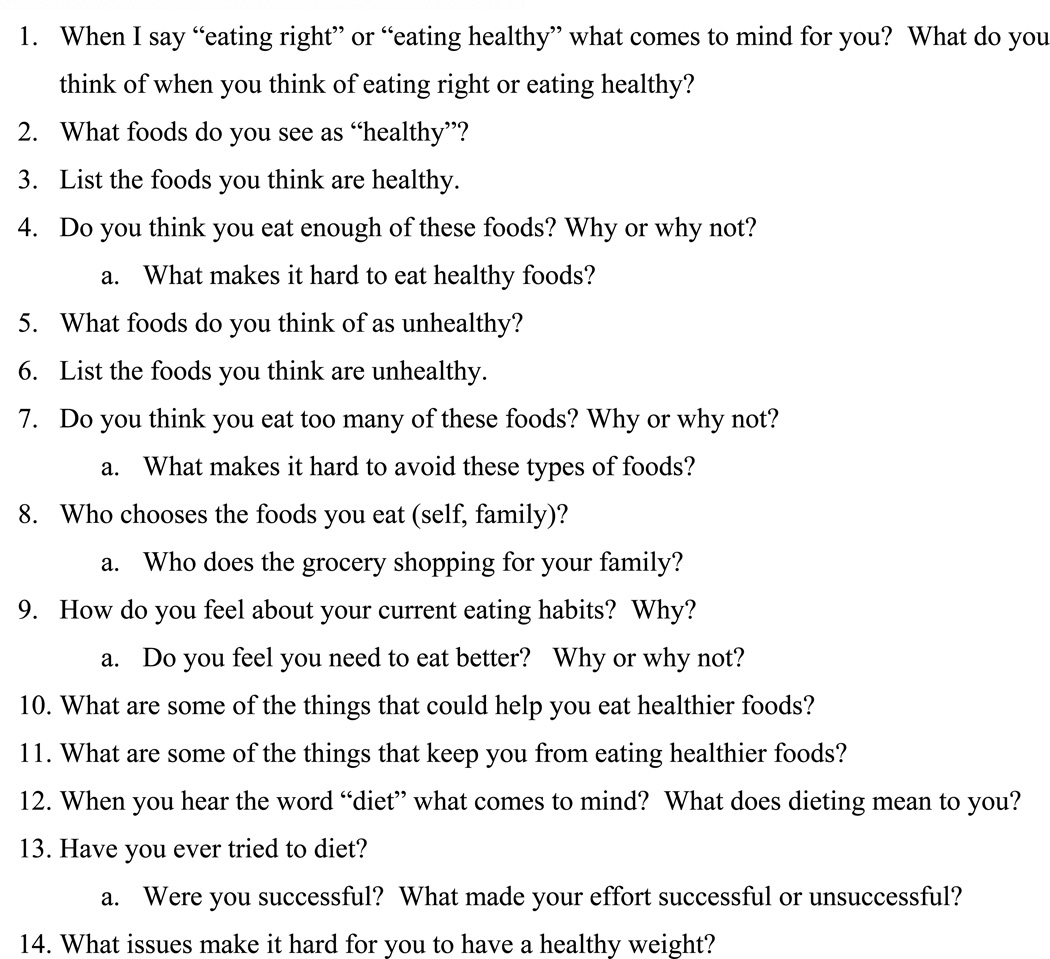
Our focus group guide (See Figure 2) was developed by academic researchers and community members, and it was pilot tested with additional community members. The guide focused on 3 main domains: perceptions of healthy versus unhealthy food, determinants of dietary intake, and perceptions of programs designed to improve the quality of dietary intake.
Figure 2.
Focus Group Guide
Procedures
Community staff trained and experienced in undertaking group interviews conducted the 8 focus groups and 6 group key informant interview sessions over 5 months. The moderator opened with a description of the purpose of the focus group or group key informant interviews, handed out sociodemographic forms and then posed the open-ended questions described in Figure 2. Most sessions lasted 90–120 minutes. Staff assisted participants with limited literacy in completing the forms.
Analysis
After the tape-recorded sessions were transcribed, staff reviewed them for accuracy. The transcripts were then imported into NVivo v. 8 (QSR International Inc., Burlington, Massachusetts) for coding, organization, and analysis. Coding began with one researcher engaging in line-by-line coding of the transcripts, affixing codes to each text segment, and eventually developing a preliminary codebook.27, 28 To ensure rigor, we co-coded a subsample of the transcripts, eventually obtaining inter-rater reliability of 82%,29 and we employed member checking.30 Member checking involved taking our major themes back to new groups of community members for their input and discussion.
RESULTS
Perspectives and Influences on Healthy Eating
Many participants equated healthy eating with dieting and weight loss. Dieting was often described as involving sacrifice and inconvenience, with participants using terms such as “starving” or “doing without.” Alternatively, some emphasized that healthy eating was related to increasing fruit and vegetable intake and reducing consumption of unhealthy foods such as soda, white bread, “greasy foods,” and most desserts. Participants also recognized that certain preparations of food were more healthful than others, such as baking and steaming instead of frying, with one key informant describing her family’s strategies, “We cook it, bake it, or broil it. People are really misled. It doesn’t have to be fried to be good.” Participants also recognized the unhealthy aspects of processed foods, stating “the more natural, the better it is for you” and one focus group participant (female) indicated “I think if you can’t read the words on the box you shouldn’t eat it because you’re putting junk in your body.”
Others acknowledged making unhealthy food choices in certain situations, including emotional experiences and when under time pressure. “Emotionally when I work really hard, I think I deserve a good [food] treat. When I’m sad, I think I deserve a good treat. And when I’m mad…” stated one female focus group participant. Busy schedules and personal preferences negatively influenced healthy eating. Participants often stated that their lives were too hectic to prepare and eat healthy foods. For example, one male focus group participant noted, “We live in a fast world, that’s why the fast food industry is doing good. We want things now.”
Other individual influences on healthy eating included managing existing health conditions. Several participants described the challenges of balancing healthy eating with chronic illness management. One woman (focus group) noted,
I have high blood pressure and diabetes so a lot of times I make something for my diabetes and it has too much sodium. But then I cut back on the sodium and it gets the diabetes, and there isn’t taste by then. It’s hard to come up with recipes that taste good that fit both diets.
Many participants emphasized the social influences on eating habits, including dietary negotiations among family members. One woman suggested during a focus group, “You have to take each day and realize what’s bad for you and try to get it out of your house because it’s not only affecting you but your family.” One woman identified these influences as having a negative impact on healthy eating, noting in her focus group that “family members don’t always want to eat healthy” while another stated, “my husband won’t eat whole wheat bread so there is no point in buying a whole loaf just for me, so I just eat what he likes.” However, as the traditional food purveyors and providers (“us women are the boss”), wives and mothers often described having a positive effect on the rest of the family. One male focus group participant indicated, “My wife does most of the shopping and she gets the wheat bread and the wheat buns” and a female focus group participant said, “I put my husband on a diet because of his health and he was successful at losing weight.” Participants also recognized the influence parents have on their children’s eating habits. As a female focus group participant explained, “I think it all goes back to what you learned as a child and changing and starting your children off the right way.” Another female focus group participant said, “As a parent, I think you choose how your children’s health is going to be. If you start letting them be health conscious then that will continue.”
Many participants explained how community-level influences (eg, norms and attitudes) often worked against healthy eating. One key informant described how different she felt from most community members, an uncomfortable feeling,
I have been told that I am a picky eater just because I only eat whole wheat and whole grains, skim milk, and other healthy foods. It is very difficult… People will always say to me, ‘just this once, it won’t hurt if we serve this junk food.’ Well if you say that once you will say it an average of 7 times during the week.
Participants underscored that changing community norms to make healthy eating more acceptable will not happen overnight. Another female key informant advised,
Trying to get people around here to eat tofu is a real stretch but if you can get them to know about the different items, they just might try them. In my mind, it has got to get them out of their comfort zone and then you can start to move forward once they realize that it is just as yummy and a whole lot better for you.
Another community influence on diet involved food served at social or public events including church gatherings, a venue frequently implicated in unhealthy eating practices. One key informant male participant noted, “The churches bring all the fat foods when they get together, it may start there” while another focus group participant (male) stated, “Social dinners at church make it nearly impossible to be healthy.”
Appalachia’s physical environment, ranging from the mountainous terrain to the stores and restaurants available to area residents, was cited as a strong influence on diet. Recognizing that not all rural residents have regular access to large supermarkets, one female key informant said, “A lot of what you can [eat] is obviously influenced by what you can get at the local grocery store. If the convenience store on the corner does not have a lot of healthy options, then that is a large influence in what you will eat.”
The poverty endemic to Appalachian Kentucky counties also emerged as an important factor in shaping diets. Many participants described an inability to access and afford high-quality foods due to low socioeconomic status, insufficient transportation, and geographic isolation. One woman (focus group) explained, “The economy has a lot to do with it. A lot of the healthy foods are more expensive, so you do the macaroni and cheese and that type of thing.” A male key informant connected optimal food choices with income, “Wherever the money is, is where you find the variety.” Another woman described the financial allure of less healthy eating in her focus group, noting that “Fast food places have the dollar menus, so it’s cheaper to go and buy a dollar burger than buy food and fix it yourself.”
Participants described that gardening, a traditional backbone of the Appalachian diet, influenced their eating patterns to varying extents. Despite the mountainous terrain in Appalachia which challenges residents to find a suitable growing area, many participants reported gardening in the summer as a source of healthy food. However, since the region has become dotted with small cities, many urban residents have little available land. As one man (focus group) described, “… if you live in the city, you don’t have the yard for a garden so you have to buy what’s on the shelf.”
Appalachian residents’ perceptions of the benefits of healthy eating frequently revolved around societal influences such as advertising and the media. As this formerly isolated region has become more integrated with the rest of the nation through highway systems, commerce, communications, and popular culture, these broader social influences have become more central to Appalachian life. One female key informant reported that, “McDonald’s was not in Harlan County when we moved here. When McDonald’s opened, their opening day here surpassed any other opening in the United States.” Speaking of residents in her community, another key informant said, “They know that a Big Mac is not healthy, but most will tune that out and go for the convenience or the marketing of the item that pushes them to make that choice.”
Suggestions for Healthy Eating Programs
In response to an open-ended question about ways to promote healthy eating, participants offered numerous program suggestions. At the individual level, participants described the need to increase knowledge to develop healthier eating habits, emphasizing nutrition and cooking classes. As one focus group participant noted, “Just get in line at Wal-Mart and look at some of the things people put in their carts. We need to teach people what to eat and how much to eat.” Another woman (focus group) agreed, “I think in order for an eating program to be successful people need to learn what is healthy and not just what they like.” Educational workshops were supported by several community members who expressed a desire to know more about “the food pyramid.” Another woman also suggested in her group key informant interview that, “Cooking classes could really make a big difference…. I think they would work well. We also need to focus on specialty groups like diabetics and family meals. We also might want to do cooking for singles and different methods of canning.”
Cooking classes held appeal because, as one key informant noted, “some people have fixed ingredients in their recipes and they won’t change them,” but a “cooking class is an excellent way to introduce new foods. You just have to be sure that it is something that tastes good.”
Recognizing the important role played by interpersonal factors in supporting behavioral change, participants strongly expressed preference for a healthy eating program that incorporated social support, agreeing with one focus group participant who explained, “Group programs work best for me. The motivation is a booster.” Another woman (key informant) stated that a good program makes sure community members are
…being supported by their peers…. A personal contact with a person [is the most important part of a healthy eating program]. If you just put it on paper, nothing is going to happen. They need that contact with people that they know and trust. Whether it is friends or pastors – just anyone.
Some participants advocated for using well-respected community members as nutrition coaches. Others expressed concern about this suggestion; one key informant cautioned that people might have difficulties with nutrition coaches if “they feel like they are being talked down to.”
Community gardening emerged as another suggestion to increase healthy eating, reinforcing messages from the cooking classes and from nutrition coaches. One woman (key informant) suggested that, “Community gardening would be nice, like at the housing projects or even in the schools…. You could incorporate the food you raise into the cooking classes.” A female key informant expressed that, “a lot of people just don’t know [how] to plant so they may want to learn or they may be embarrassed to try,” suggesting that community gardening could help them learn about growing food, and could potentially also help establish new healthier social norms.
While the topography of the region may continue to be a challenge, several suggestions for changing the food environment were offered. Participants suggested that enhancing healthy eating could be accomplished by simply offering healthier options through institutional kitchens at schools and other locations. One female cafeteria worker (key informant) noted, “The kids will really start eating whatever it is that we cook” and “If that is what you fix, then they will eventually eat it.” A focus group participant (female) suggested, “Instead of selling popcorn and pizza at ball games and stuff, sell healthier things.”
DISCUSSION
This study sought to understand how rural, Appalachian residents think about healthy eating and their ideas for improving dietary intake. One of the most striking and novel findings of this study is how closely the participants’ understandings of the challenges faced in maintaining healthy diets mirrored the socioecological model of health behavior. This was especially notable since the interview guide used in this research was intentionally phrased broadly, rather than focusing on any particular theories or constructs. Nonetheless, while participants did not use the language of behavioral theory, their responses were reflective of the key elements of the socioecological model, with emphasis on the multiple levels of influence on health behavior.31, 32 This contrasts with other research on Appalachian diet which emphasizes individual and interpersonal influences on diet.15, 33
On the individual level, while most participants felt that their own nutritional knowledge was adequate and that other forces led them to follow diets they knew were unhealthy, many suggested that other community members, such as those they see in store checkout lines, needed nutrition education. Many participants noted that promoting stand-alone nutrition education programs would be unlikely to achieve traction among people who felt they already had adequate nutritional knowledge.
The strong support expressed for cooking classes as a potential strategy for improving diets within Appalachian communities may reflect participants’ perceptions of the importance of intersecting individual, interpersonal, and community levels of influence on dietary intake. Such intersections have been previously described in ethnographic descriptions and survey analyses of Appalachian perspectives toward health.34, 35 Participants noted that cooking classes can be used to disseminate accurate knowledge and food preparation strategies at the individual level, which can ultimately affect the diets of others in their families and communities. Bringing together these levels of influence may address several new challenges to healthy eating in rural America. First, Appalachian families are increasingly experiencing time constraints associated with extracurricular activities, the need to commute significant distances for jobs,36 and women working outside the home.16 Such constraints, in conjunction with the proliferation of fast food outlets and advertisements promoting less healthy food options, are shifting community norms and personal and familial practices away from homemade meals. Compounding these challenges, rural residents oftentimes experience all of the stresses and strains of modern life without the accompanying benefits of convenient healthy lifestyle items (salad bars, fruit stands, local gyms for physical activity).16
Increasing attention has been paid to the role that families play in affecting dietary habits, resulting in recommendations to improve dietary quality through intergenerational approaches.37, 38 Shaping the decisions of key members of households, particularly those with primary responsibilities for shopping and cooking, could influence the diets of entire families. Since participants noted that community members and local organizations promoted unhealthy eating habits, targeting family units within social and group settings may help to improve community-level attitudes toward healthy foods and eating practices. As Goins and colleagues have recently described, many Appalachian residents view social integration and familial influences on health as a key determinant of a good and healthy lifestyle.39 As expressed by our participants, encouraging important community institutions, such as churches and schools, to offer healthy eating options (eg, through church suppers) may also be a promising direction for community-level interventions.
Although recent reports from noteworthy sources such as the Institute of Medicine and the Robert Wood Johnson Foundation emphasize the role of the food environment in shaping dietary patterns, our data are among the first to document this perspective among Appalachian residents themselves.40 Increasingly, rural researchers are focusing on the environmental challenges to high-quality diets, including the prevalence of fast food outlets, convenience stores, and needed income derived from the sale of unhealthy food at concessions or vending machines. Ahern and colleagues found that among non-metropolitan residents lower mortality rates were associated with greater access to full-service food venues (as opposed to fast food restaurants or convenience stores). Lower rates of diabetes and obesity were associated with fewer fast food restaurants and convenience stores, and lower obesity rates were associated with more per capita full-service restaurants.41 Emphasizing the diversity of rural communities, Hosler and colleagues noted even within 2 rural counties, lower socioeconomic status parts of town were far more likely than higher socioeconomic status areas to offer inexpensive, high-calorie but nutritionally limited foods (and cigarettes). Higher income community stores in rural communities, however, maintained a greater offering of fresh produce and nutritionally dense foods.42 Amarasinghe and colleagues’ work in Appalachian West Virginia highlighted the interacting effects of individual socioeconomic status and the surrounding economic environment.43 Such findings corroborate our informants’ perspectives that the environment and society matter regarding access to healthy food.
Limitations
Although this study is among the first to document local residents’ description of multifaceted and interlinking levels of influence on healthy eating, we acknowledge several limitations. First, this research focused in one region, Appalachian Kentucky; thus, we are not necessarily able to generalize our results throughout rural America or even to the 8.3% of the United States population that comprises Appalachia. However, we suspect the challenges that exist in Appalachian Kentucky (low socioeconomic status, geographic isolation, high unemployment, scarce health care resources, etc.) may simply represent a more dramatic version than many rural communities. Additionally, generalizability is limited by the more exploratory, descriptive nature of the project. Despite being relatively large for a qualitative project (8 focus groups and 6 group key informant interviews), we acknowledge the potential for selection bias.
CONCLUSION
There is increasing recognition of the importance of listening to the local community to better understand their health decision-making context and involve them in health promotion efforts.44 Consistent with the socioecological model, rural Appalachian residents described challenges and suggested approaches to address the multiple and intersecting layers of healthy eating; sustained improvements in dietary intake will require addressing all of these layers. Researchers and policy makers have begun to recognize the limitations of solely focusing on individual and interpersonal factors to enhance dietary intake, and have begun to develop broader and more innovative plans to address these intersecting layers. Contrary to images of the bucolic rural lifestyle where people labor in the garden all day, and satisfy their well-earned hunger on homegrown produce, our participants articulate a different reality, one involving a hurried lifestyle where meals are picked up at drive-through windows or at high school concession stands. With most participants bemoaning this reality and the accompanying health problems, many hope for constructive, innovative, feasible, and sustainable solutions. The next step involves constructive collaboration and engagement to develop, implement, and evaluate such culturally sensitive solutions, including those mentioned by these participants and important existing literature.45
Acknowledgments
Support for this research was provided by the National Institutes of Health/ National Center on Minority Health and Health Disparities/ National Institute on Diabetes and Digestive and Kidney Disease (R01 DK081324: Schoenberg).
Footnotes
We appreciate the contributions of Kaye Dollarhide, Sherry Wright, and the dozens of participants.
REFERENCES
- 1.Krebs-Smith S, Guenther P, Subar A, Kirkpatrick S, Dodd K. Americans do not meet federal dietary recommendations. The Journal of Nutrition. 2010;140(10):1832–1838. doi: 10.3945/jn.110.124826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bachman J, Reedy J, Subar A, Krebs-Smith S. Sources of food group intakes among the US population, 2001–2002. Journal of the American Dietetic Association. 2008;108(5):804–814. doi: 10.1016/j.jada.2008.02.026. [DOI] [PubMed] [Google Scholar]
- 3.Cohen D, Sturm R, Scott M, Farley T, Bluthenthal R. Not enough fruit and vegetables or too many cookies, candies, salty snacks, and soft drinks? Public Health Rep. 2010;125(1):88–95. doi: 10.1177/003335491012500112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mendoza JA, Drewnowski A, Christakis DA. Dietary energy density is associated with obesity and the metabolic syndrome in U.S. adults. Diabetes Care. 2007 Apr;30(4):974–979. doi: 10.2337/dc06-2188. 2007. [DOI] [PubMed] [Google Scholar]
- 5.Krishna S, Gillespie K, McBride T. Diabetes burden and access to preventive care in the rural United States. J Rural Health. 2010;26(1):3–11. doi: 10.1111/j.1748-0361.2009.00259.x. [DOI] [PubMed] [Google Scholar]
- 6.Jackson JE, Doescher MP, Jerant AF, Hart LG. A national study of obesity prevalence and trends by type of rural county. The Journal of Rural Health. 2005;21(2):140–148. doi: 10.1111/j.1748-0361.2005.tb00074.x. [DOI] [PubMed] [Google Scholar]
- 7.Della LJ. Exploring diabetes beliefs in at-risk Appalachia. J Rural Health. 2011;27(1):3–12. doi: 10.1111/j.1748-0361.2010.00311.x. [DOI] [PubMed] [Google Scholar]
- 8.Kentucky Department for Public Health. The Kentucky obesity epidemic. 2005 Retrieved on December 12, 2011. Available from http://www.fitky.org.
- 9.Centers for Disease Control and Prevention. Overweight and obesity. 2010 Retrieved on November 1, 2012. Available from http://www.cdc.gov/obesity/index.html.
- 10.Centers for Disease Control and Prevention. Diabetes data and trends. 2009 Retrieved on August 2, 2011. Available from http://apps.nccd.cdc.gov/DDTSTRS/default.aspx.
- 11.Rugg SS, Bailey AL, Browning SR. Preventing cardiovascular disease in Kentucky: epidemiology, trends, and strategies for the future. Journal of the Kentucky Medical Association. 2008;106:149–161. [PubMed] [Google Scholar]
- 12.Webber KH, Quintiliani L. Development of a weight loss program for Appalachian Kentucky adults: A formative research survey. Family and Consumer Sciences Research Journal. 2011;40:74–84. [Google Scholar]
- 13.Centers for Disease Control and Prevention. Behavioral risk factor surveillance system survey data. Atlanta, Georgia: U.S. Department of Health and Human Services; 2009. [Google Scholar]
- 14.Shortridge B. Apple stack cake for dessert: Appalachian regional foods. Journal of Geography. 2005;104(2):65–73. [Google Scholar]
- 15.Brown JL, Wenrich TR. Intra-family role expectations and reluctance to change identified as key barriers to expanding vegetable consumption patterns during interactive family-based program for Appalachian low-income food preparers. Journal of the Academy of Nutrition and Dietetics. 2012;112(8):1188–1200. doi: 10.1016/j.jand.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 16.Schoenberg N, Hatcher J, Dignan MB. Appalachian women's perceptions of their community's health threats. Journal of Rural Health. 2008;24(1):75–83. doi: 10.1111/j.1748-0361.2008.00140.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bovell-Benjamin AC, Hathorn CS, Ibrahim S, Gichuhi PN, EM. B. Healthy food choices and physical activity opportunities in two contrasting Alabama cities. Health Place. 2009;15(2):429–438. doi: 10.1016/j.healthplace.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 18.Sobo E, De Munck V. The forest of methods. In: De Munck V, Sobo E, editors. Using Methods in the Field. Walnut Creek, CA: AltaMira Press; 1998. [Google Scholar]
- 19.Appalachian Regional Commission. Demographic and health information. 2006 Retrieved on October 20, 2008. Available from www.arc.gov.
- 20.Appalachian Regional Commission. County Economic Status, Fiscal Year 2012: Appalachian Kentucky. Retrieved on January 4, 2012. Available from http://www.arc.gov/reports/region_report.asp?FIPS=21999&REPORT_ID=37.
- 21.US Department of Agriculture. Rural/urban continuum codes. 2003 Retrieved on October 11, 2008. Available from www.ers.usda.gov/Data/RuralUrbanContinuumCodes/.
- 22.Kosmin B, Mayer E, Keyser A. American religious identification survey. 2008 Retrieved on March 29, 2009. Available from http://commons.trincoll.edu/aris/.
- 23.Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based health promotion interventions: evidence and lessons learned. Annual Review of Public Health. 2007;28(1):213–234. doi: 10.1146/annurev.publhealth.28.021406.144016. [DOI] [PubMed] [Google Scholar]
- 24.Studts CR, Tarasenko YN, Schoenberg NE, Shelton BJ, Hatcher-Keller J, Dignan MB. A community-based randomized trial of a faith-placed intervention to reduce cervical cancer burden in Appalachia. Preventive Medicine. 2012;54(6):408–414. doi: 10.1016/j.ypmed.2012.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schoenberg NE, Hatcher J, Dignan MB, Shelton B, Wright S, Dollarhide KF. Faith Moves Mountains: an Appalachian cervical cancer prevention program. American Journal of Health Behavior. 2009;33:627–633. doi: 10.5993/ajhb.33.6.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Luborsky M, Rubenstein R. Sampling in qualitative research. Research on Aging. 1995;17(91):89–113. doi: 10.1177/0164027595171005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.MacQueen KM, McLellan E, Milstein KK, Milstein B. Codebook development for team-based qualitative analysis. Cultural Anthropology Methods. 1998;10(2):6. [Google Scholar]
- 28.Weston C, Gandell T, Beauchamp J, McAlpine L, Wiseman C, Beauchamp C. Analyzing interview data: The development and evolution of a coding system. Qualitative Sociology. 2001;24(3):15. [Google Scholar]
- 29.Boyatzis RE. Transforming qualitative information: thematic analysis and code development. Thousand Oaks: Sage; 1998. [Google Scholar]
- 30.Morse JM, Swanson JM, Kuzel AJ, editors. The nature of qualitative evidence. Thousand Oaks: Sage; 2001. [Google Scholar]
- 31.Green LW, Richard L, Potvin L. Ecological foundations of health promotion. American Journal of Health Promotion. 1996 Mar-Apr;10(4):270–281. doi: 10.4278/0890-1171-10.4.270. [DOI] [PubMed] [Google Scholar]
- 32.Sallis JF, Owen N, Fisher E. Ecological models of health behavior. In: Glanz K, Rimer B, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco: Jossey-Bass; 2008. [Google Scholar]
- 33.Wu TJ, Snider JB, Floyd MR, Florence JE, Stoots JM, Makamey MI. Intention for healthy eating among Southern Appalachian teens. American Journal of Health Behavior. 2009;33(2):115–124. doi: 10.5993/ajhb.33.2.1. [DOI] [PubMed] [Google Scholar]
- 34.Keefe S. Southern Appalachia: analytic models, social services, and native support systems. American Journal of Community Psychology. 1986:479–498. doi: 10.1007/BF00935354. [DOI] [PubMed] [Google Scholar]
- 35.Beaver PD. Rural community in the Appalachian south. Lexington: University Press of Kentucky; 1986. [Google Scholar]
- 36.Mather M. Demographic and socioeconomic change in Appalachia: housing and commuting patterns in Appalachia. Report of the Appalachian Regional Commission. 2004 Retrieved on September 17, 2012. Available from http://www.prb.org/pdf04/housingcommutingappalachia.pdf.
- 37.Swanson M, Studts CR, Bardach SH, Bersamin A, Schoenberg NE. Intergenerational energy balance interventions: A systematic literature review. Health Education Behavior. 2011;38(2):171–197. doi: 10.1177/1090198110378973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stolley MR, Fitzgibbon ML. Effects of an obesity prevention program on the eating behavior of African American mothers and daughters. Health Education and Behavior. 1997 Apr 1;24(2):152–164. doi: 10.1177/109019819702400204. [DOI] [PubMed] [Google Scholar]
- 39.Goins RT, Spencer SM, Williams K. Lay meanings of health among rural older adults in Appalachia. The Journal of Rural Health. 2011;27(1):13–20. doi: 10.1111/j.1748-0361.2010.00315.x. [DOI] [PubMed] [Google Scholar]
- 40.Committee on Accelerating Progress in Obesity Prevention. Accelerating progress in obesity prevention: solving the weight of the nation report. 2012 Retrieved on August 25, 2012. Available from http://www.iom.edu/Reports/2012/Accelerating-Progress-in-Obesity-Prevention.aspx. [PubMed]
- 41.Ahern M, Brown C, Dukas S. A national study of the association between food environments and county-level health outcomes. The Journal of Rural Health. 2011;27(4):367–379. doi: 10.1111/j.1748-0361.2011.00378.x. [DOI] [PubMed] [Google Scholar]
- 42.Hosler AS. Retail food availability, obesity, and cigarette smoking in rural communities. The Journal of Rural Health. 2009;25(2):203–210. doi: 10.1111/j.1748-0361.2009.00219.x. [DOI] [PubMed] [Google Scholar]
- 43.Amarasinghe A, D’Souza G, C B, Oh H, Borisova T. The Influence of socioeconomic and environmental determinants on health and obesity: A West Virginia case study. International Journal of Environmental Research and Public Health. 2009;6(8):2271–2287. doi: 10.3390/ijerph6082271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Potvin L, Cargo M, McComber AM, Delormier T, Macaulay AC. Implementing participatory intervention and research in communities: lessons from the Kahnawake Schools Diabetes Prevention Project in Canada. Social Science and Medicine. 2003 Mar;56(6):1295–1305. doi: 10.1016/s0277-9536(02)00129-6. [DOI] [PubMed] [Google Scholar]
- 45.Tessaro I, Rye S, Parker L, et al. Cookin' Up Health: developing a nutrition intervention for a rural Appalachian population. Health Promotion and Practice. 2006;7(2):252–257. doi: 10.1177/1524839905278887. [DOI] [PubMed] [Google Scholar]