Abstract
Background:
Percutaneous coronary intervention (PCI) for chronic total occlusion (CTO) of the left anterior descending (LAD) specifically is associated with improved long-term 5 year survival as compared to PCI failure. The procedure is associated with usage of different types of dedicated guidewires by simple or complex techniques aiming to reopen the occluded artery.
Aim:
To describe types and outcome of guidewires used in LAD-CTO utilizing a first intentional single wiring simple strategy.
Methods:
A single center prospective registry for all consecutive patients with a PCI attempt to a native LAD CTO. The initial strategy for lesion crossing was Single wiring.
Results:
A total of 30 patients with LAD CTO lesions (100%), were recorded. Mean age was 71.6 + 15 years, 77% were Males, risk factors Hypertension in 63%, Diabetes 27%, Dyslipidemia 57%, smoking 40%, hereditary in 13% of patients. Isolated guidewire (GW) success rate was very high 93%. Single wiring was the prevailing technique used in 97% of successfull lesions (83% of total cases) while only 3% were by multiple wiring techniques. Successful single antegrade wiring represented 63% with a GW success rate of 92% of cases. Successful single retrograde wiring represented 13% with a GW success rate of 67%. Successful Crossing GW types in our patients were 44% Soft Tapered GWs; fielder XT (44%), 36% were Soft Non Tapered Pilot 50 (28%), whisper (8%), while 16% were Stiff Non tapered GWs; Miracle 12 (8%), Miracle 6 (4%), Miracle 3 (4%), and 4% were Stiff Tapered GWs; Progress 200 (4%).
Conclusions:
Single wiring as an initial strategy in PCI for LAD-CTO lesions has a high success rate and is associated with a 44% majority of Soft Tapered GWs, 36% Soft Non Tapered, 16% Stiff Non tapered GWs, and 4% Stiff Tapered GWs.
Keywords: Chronic total occlusion, first intention, guidewires, left anterior descending, single wiring
INTRODUCTION
The presence of chronic total occlusion (CTO) has been the most common reason for surgical referral[1] and the strongest predictor against the selection of percutaneous coronary intervention (PCI) as a treatment strategy.[2] CTO with multi-vessel disease is referred for coronary artery bypass graft (CABG) even if the other lesions are ideally suited for PCI.[3,4,2] Owing to the ongoing evolution in dedicated guidewires (GWs), materials, and techniques of PCI to CTOs, during the past decade, success rates jumped from 51% in the balloon angioplasty era to 70% in the Drug Eluting Stent (DES) era,[5] and now the presence of a CTO should no longer be a sufficient reason to switch from a percutaneous to a surgical approach in multi-vessel disease, in the absence of a significant left main disease, and when the other lesions are suitable for PCI.[6]
CTO is generally a stable lesion, in which a thrombus has progressed, commonly with the thrombus extending to a nearby side branch ostium.[7,8] The intimal plaque is located between the true lumen and subintima, and is more resistant than the subintimal tissue. The longer the duration the harder the intimal plaque, with denser calcium deposits. When a fresh thrombus is formed after vessel occlusion, it is gradually transformed into an organized thrombus with dense collagenous fibro-calcific tissues at the proximal and distal ends, referred to as proximal and distal fibrous ‘caps’. The proximal fibrous cap is more rigid and at a higher risk of subintimal guidewire (GW) migration than the distal fibrous cap, which is weaker and less rigid[8] (providing the rationale of being the entry point for retrograde approaches). Microchannels with lumen sizes approximately 200 um are present inside the CTO lesion, extending toward small side branches or vasa vasorum or continue longitudinally from the proximal to the distal lumen reaching up to 85% of the CTO length. They may become fewer as the CTO matures,[9] or continuously exist in loose tissue from the proximal to the distal fibrous caps, without relation to the CTO age,[7] offering an explanation for successful loose tissue tracking even in very old CTOs.[10] The subintimal space ‘media’ is located between the intima and the adventitia, near the external elastic lamina. It consists of weak connective tissue that may show an intramural hematoma, with a dissection that can easily expand widely in both longitudinal and transverse directions.
Percutaneous coronary intervention for CTO of the left anterior descending (LAD) specifically, is associated with an improved, long-term, 5 year survival, as compared to PCI failure.[11] The procedure is associated with usage of many different types of dedicated guidewires in the process, aiming to recanalize the occluded vessel. Crossing the occlusive lesion till it reaches the true lumen may be achieved by GW tracking, through the lesion's intima or subintima. According to the GW type, a ‘Soft Approach’ is crossing with a soft hydrophilic GW, for example, a tapered fielder XT, while a ‘Stiff approach’ is crossing with a stiff non-hydrophilic GW, for example, Miracle. The ‘Combo technique’ is penetrating the resistant cap with a stiff GW and crossing the less resistant portion with a soft GW.
AIM OF THE STUDY
To describe the different types and outcome of soft and stiff, tapered and non-tapered guidewires used in crossing CTO of the native LAD artery, utilizing a first intentional single wiring strategy.
MATERIALS AND METHODS
The study was a single center prospective registry. All consecutive patients with a PCI attempt to a native LAD-CTO from January to December, 2010 were registered. All patients showed evidence of myocardial viability in the LAD territory. All other coexisting non-LAD coronary lesions indicated for interventional therapy were treated before attempting the CTO procedure (30% of the cases within the same session). All cases were first attempts, with no previous attempt failure recorded of the specific CTO-LAD vessel. All patients had been pretreated and maintained on optimal medical treatment, including dual antiplatelet therapy, and were able to continue on an antiplatelet agent regimen consisting of aspirin indefinitely and clopidogrel or prasugrel daily, for at least six months after the procedure.
Procedure technique
The operator's initial strategy was to start with a radial access as the first choice whenever feasible, if not, a femoral access was chosen. Bilateral access was carried out whenever it was possible to better visualize the distal true lumen through the collaterals. Six French size sheathes and catheters were preferred whenever feasible. The decision to perform an antegrade or a retrograde approach was left to the operator's discretion and was dependent on each individual patient's condition.
The initial strategy for lesion crossing in either the antegrade or retrograde approach was Single wiring by lesion crossing, using only one guidewire (GW) as a simple technique. Multiple wiring by lesion crossing using multiple GWs, as a complex technique, was chosen when single wiring was not feasible. Lesion success was defined as a final percentage of diameter stenosis <50% with a TIMI 3 flow, guidewire (GW) crossing success was defined as the ability of the GW to cross the occlusion and reach the distal true lumen. Guidewires were classified according to the tip into, soft, stiff, tapered, or non-tapered GWs.
Statistical methods
Continuous variables were presented as mean ± SD or median and range if appropriate. Discrete variables were expressed as counts and percentages. All statistical analyses were performed with JMP version 8.0 (SAS Institute, Cary, North Carolina). The authors had full access to and took full responsibility for the integrity of the data.
RESULTS
Patient characteristics
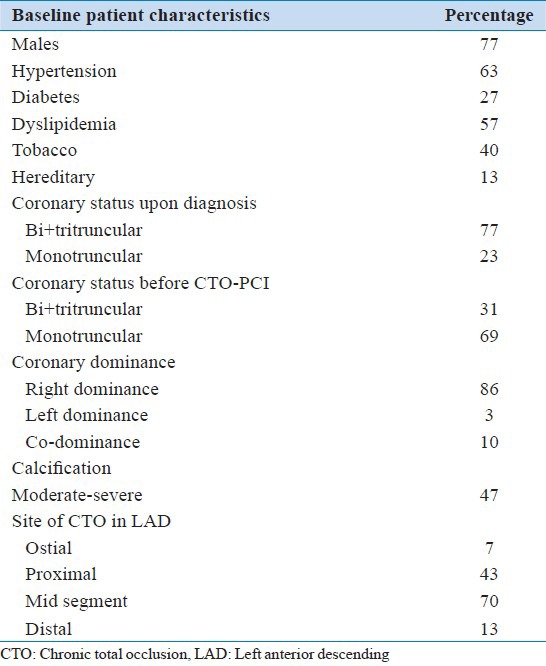
Between January 2010 and December 2010, a total of 30 patients with 30 LAD-CTO lesions (100%), were recorded. Mean age was 71.6 ± 15 years (37% were >80 years old), 77% were males, and 23% females. Cardiovascular risk factors: HTA 63%, Diabetes 27% (Insulin dependent 14%), Dyslipidemia 57%, smoking 40%, hereditary 13%.
Underlying coronary lesions
Upon initial diagnosis of the LAD-CTO the majority of patients, 77%, had Multivessel coronary disease, while only 23% had Single vessel disease (CTO-LAD). Coronary artery Dominance was Right in 86%, Left 3%, and Co-dominance in 10% of the patients. The Length of the occlusive lesion was <30 mm in 53% and >30 mm in 47% of the patients. Visible collaterals were evident. They were antegrade in 58%, retrograde in 62%, both anterograde and retrograde in 31%, and absent or nonvisible in 7% of the patients. Calcification was moderate in 30% and severe in 17% of the patients. Origin was de novo in 97% and in-stent in 3% of the patients. Site of lesion was ostial in 7%, proximal in 43%, middle in 70%, and distal in 13% of the patients. Reference Artery Diameter mean was 2.99 ± 0.33 mm, median 3, range 2.5 to 3.5 mm. Bifurcation lesion CTO-diagonal (>1.5 mm) was present in 20% of the patients [Table 1].
Table 1.
Baseline characteristics
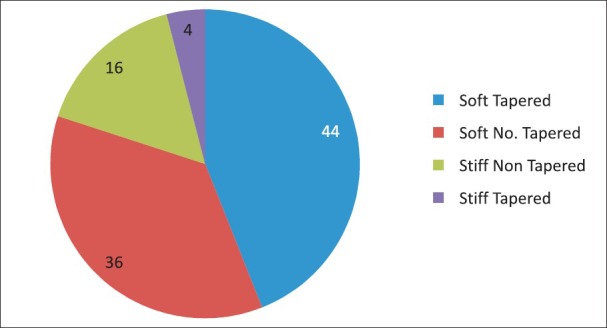
An Initial Antegrade approach was attempted in 80% of the cases while an Initial Retrograde approach was attempted in 20% of the cases. Conversion to an antegrade technique after a failed retrograde attempt occurred in 7% of the cases, bringing the total antegrade approach attempts to 87%, while no conversion was done to the retrograde approaches after any failed antegrade attempt (0%) [Figure 1].
Figure 1.
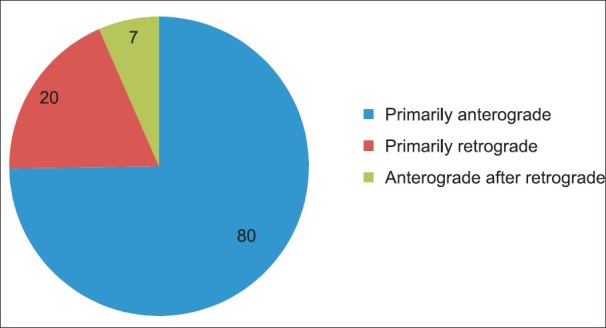
Procedural approach
In the antegrade approaches, 97% of the lesions were attempted with single wiring and 3% with multiple wiring techniques. The retrograde approaches were all carried out using the retrograde single wire crossing technique (100%), through visible septal collaterals (100%), without attempts through epicardial collaterals (0%).
The successful cases were finalized with antegrade stenting (83%). Kissing with provisional T stenting was done in 67% for bifurcational diagonal side branch CTOs, while in 33% of the cases there was stenting without kissing. Anchoring in a side branch septal or diagonal to facilitate stent delivery was done in 6% of the patients. Rotablateur 3%, IVUS 3%, and Tornus 3% were used to facilitate the procedure with success; all were with anterograde approaches.
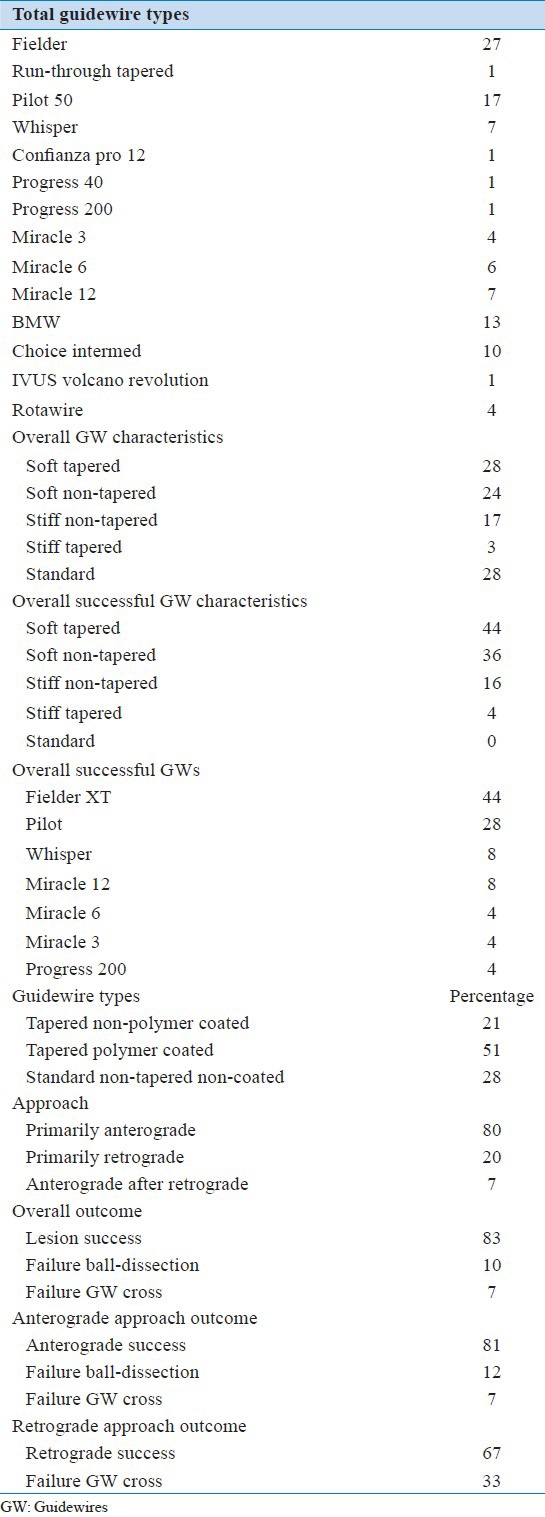
Guidewires (GWs): [Figure 2]
Figure 2.
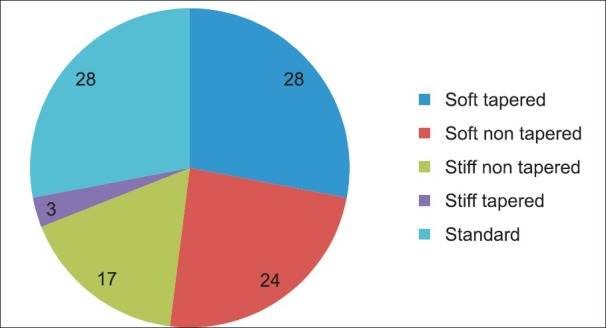
Overall characteristics of guidewires used
The Number of GWs used in the Total number of patients were 86 (100%), mean 3.2 ± 2.4, median 2, and range 1 to 9 GW/patient. In Antegrade cases, they were 49 (57%), mean 2.3 ± 1.6, median 2, and range 1 to 7 GW/patient. In Retrograde cases they were 37 (43%), mean 6.1 ± 2.4, median 6, and range 2 to 9 GW/patient were used. Fourteen different types of GWs were recorded in the study.
Soft hydrophilic tapered GWs in the Total patients were 28%; fielder XT (27%), and Run-through tapered (1%). In the Antegrade cases they were 26%; fielder XT (24%), and Run-through tapered (2%). In the Retrograde cases they were 30%; fielder XT (30%). Soft hydrophilic non-tapered GWs in the Total patients were 24%; Pilot 50 (17%), and whisper (7%). In the Antegrade cases they were 30%; Pilot 50 (22%), and whisper (8%). In the Retrograde cases they were 15%; Pilot 50 (9%), and whisper (6%).
Stiff non-tapered tip GWs in the Total patients were 17%; Miracle 6 (7%), Miracle 12 (6%), and Miracle 3 (4%). In the Antegrade cases they were 12% Miracle 6 (8%) and Miracle 12 (4%). In the Retrograde cases they were 24%; Miracle 6 (6%), Miracle 12 (9%), and Miracle 3 (9%). Stiff-tapered tip GWs in the Total patients were 3%, Confianza pro12 (1%), Progress 40 (1%), and Progress 200 (1%). In the Antegrade cases they were 6%, Confianza pro12 (2%), Progress 40 (2%), and Progress 200 (2%). In the Retrograde cases they were not recorded (0%).
Standard GWs used to complete the PCI procedure after successful wire crossing in the Total patients were 28%, BMW (13%), Choice intermediate (10%), Rotawire (4%), and Revolution Volcano (1%). In the Antegrade cases they were 26%; BMW (14%), Choice intermediate (8%), Rotawire (2%), and Revolution Volcano (2%). In the Retrograde cases they were 30%; BMW (12%), Choice intermediate (12%), and Rotawire (6%).
Successful Guidewire Crossings According to its Types: [Figures 3 and 4]
Figure 3.
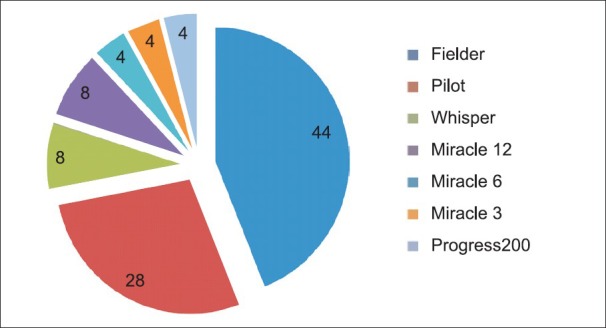
Overall successful guidewire types
Figure 4.
Successful guidewire characteristics
In the Total patients: Successful GW crossing occurred in 93% of the cases, 44% were Soft Tapered GWs; fielder XT (44%), 36% were Soft Non-tapered Pilot 50 (28%), and whisper (8%), while 16% were Stiff Non-tapered GWs, Miracle 12 (8%), Miracle 6 (4%), Miracle 3 (4%), and 4% were Stiff-tapered GWs, and Progress 200 (4%).
In the Antegrade approach successful GW crossing occurred in 92% of the cases; 38% of the successful crossing was by Soft-tapered GWs; fielder XT (38%), 42% were Soft Non-tapered GWs; Pilot 50 (32%), and whisper (10%), while 15% were Stiff Non-tapered GWs, Miracle 12 (10%), Miracle 6 (5%), 5% were Stiff-tapered GWs, and Progress 200 (5%).
In the Retrograde Approach successful GW crossing occurred in 67% of the cases; 75% of the successful crossing was by Soft-tapered GWs namely the fielder XT (75%), while 25% were Stiff Non-tapered GWs namely Miracle 6 (25%).
Overall success and failure
Overall Lesion Success (final diameter stenosis <50% with TIMI3 flow) occurred in 83% of the Total cases (79% in primary intention Antegrade and 67% in primary intention Retrograde approaches, respectively). A switching conversion to an Antegrade technique after a failed Retrograde attempt occurred in 7% of the cases adding to the success of the overall Antegrade approaches, which became 81%, while no Retrograde approach conversion was done after failed Antegrade attempts, leaving the overall Retrograde approaches at 67%. Successful Antegrade single wiring represented 63% of the total patients.
The cause of Lesion Failure in total patients was Balloon crossing failure or dissection (10%) followed by wire crossing failure (7%). In the Antegrade cases, Balloon crossing failure or dissection (12%) and wire crossing failure (7%) occurred. The only cause of failure in the Retrograde approach was collateral wire crossing failure (33%). [Table 2]
Table 2.
Guidewires and outcomes
DISCUSSION
The underlying coronary lesion was Monotruncular in 23% of our patients, while in other reports 28.9[12] and 28.8%[13] were monotruncular, and the rest of the patients had multivessel disease. Our study involved LAD-CTO lesions in all patients (100%), while in other registries it was 36[14] and 31%.[13] In our study 97% were de novo lesions of native LAD, which was comparable to the other registries with 93.8[13] and 93.7%.[14] Bifurcation lesion CTO-diagonal (>1.5 mm) was present in 20% of our patients versus 16% in other reports.[12] Proximal reference artery diameter in our patients mean was 2.99 ± 0.33 mm versus 2.9 ± 0.7 mm in the J-CTO Registry.[14]
Primary Anterograde approaches represented 80% of our patients versus 85.4% in the J-CTO Registry,[14] while Primary Retrograde approaches represented 20% of our total patients versus 14.6% in the J-CTO Registry.[14] Switching in-between approaches during the same session from an unsuccessful retrograde approach to an anterograde approach occurred in 7% of our cases with 100% success versus 14.6% with 79.6% success rate in the J-CTO Registry.[14] On the other hand, there was no switching (0%) from an unsuccessful anterograde to a retrograde approach, versus 11% with a success rate of around 70%, in the J-CTO Registry.[14]
Overall lesion success rate in our study was 83% of the lesions. This was comparable to the 86.2% success rate of the CONQUEST registry[15] and the 86.6% success rate of the J-CTO registry.[14] The lesion success rate of the Primary Anterograde procedures was 79% in our study versus 74% in the J-CTO Registry.[14] On the other hand, the lesion success rate of the Primary Retrograde procedures was 67% in our study versus the relatively high 79.2% in the J-CTO Registry.[14] Switching in-between approaches during the same session from an unsuccessful retrograde approach to an anterograde approach, occurred in 7% of our cases with 100% success, adding to the success of the Overall Antegrade approach, to become 81%, while no retrograde approach conversion was done after the failed antegrade attempts, leaving the Overall Retrograde approaches at 67%. Lesion failure due to wire crossing failure occurred in 7%, while lesion failure due to Balloon crossing failure and/or dissection occurred in 10% of the cases. In the Antegrade approach, there was Balloon crossing failure or dissection (12%) and wire crossing failure (7%). In the Retrograde approach, collateral wire crossing failure was the only cause of lesion failure (33%). GW crossing failure was the most common cause of CTO lesion failure according to the Euro-CTO Club Consensus.[6]
The median number of GWs used during our procedures was two (range 1 to 5) versus 4.0 (range 1 to 10) in the J-CTO Registry[14] and a median of three (range 1 to 11) specifically in the LAD.[13] Isolated GW success rates in our study were very high, 93% in total cases, compared to 87.7% in the J-CTO Registry.[14]
Single wiring was the prevailing technique in our study being used in 97% of the successful lesions (83% of total cases) versus 50% single wiring in the J-CTO Registry,[14] while only 3% were done using multiple wiring techniques. Successful single antegrade wiring represented 63% of our total study cases with a GW success rate of 92% of the cases versus 55.5% with a GW success rate of 91.8% in the J-CTO Registry.[14] Successful single retrograde wiring represented 13% of our total study cases with a GW success rate of 67% versus 12.4% of the cases with a GW success rate of 84.5% in the J-CTO Registry.[14]
Successful Crossing GW types in our patients were 44% Soft-tapered GWs; fielder XT (44%), 36% were Soft Non-tapered, Pilot 50 (28%), and whisper (8%), while 16% was the Stiff Non-tapered GW. Miracle 12 (8%), Miracle 6 (4%), Miracle 3 (4%), and 4% were Stiff-tapered GWs, and Progress 200 (4%). In other reports 33% were soft PT Graphics intermediate and 25.5% Crossaire NT, while non-hydrophilic Miracle 3 was used in 27%.[13]
The introduction of tapered GWs has been one of the major breakthroughs in the treatment of CTO lesions,[13] as it was unlikely that standard floppy guide wires could cross the CTO, but the support microcatheter (or OTW balloon) might force the wire through the lesion subintima, unless it was a very straight occlusion segment with a central tapered stump.[6] Microcatheters or OTW balloons allowed exchange of GWs and facilitated transmission of torque to the tip and improved feedback. Microcatheters could provide better tip flexibility than OTW balloons and were useful for CTOs immediately distal to a bend. Their larger inner lumen reduced friction during wire manipulation and also advantageous to have a radiopaque marker at the very tip of the catheter.[6]
Often, the general sequence of choice of GWs is to start initially with a polymer-coated floppy wire, to negotiate the segment proximal to the occlusion, and advance a microcatheter (or OTW balloon) up to the proximal stump and then exchange to a stiffer dedicated wire,[7,16] as they are more aggressive and may cause damage to the tortuous proximal segments before reaching the occlusion. On account of the poor feedback (wire-feel) with polymer-coated wires and the lack of resistance offered to advancement, checking by contralateral injection for any distal intraluminal wire passage is recommended, to avoid the creation of long subintimal tracks.[6]
Limitations
The number of cases is small and from a single center. The results of this study may be influenced by the selection criteria, operator skills, judgment, and individual experience in varying techniques. There is a lack of follow-up beyond the in-hospital phase. Finally, the techniques are still in continuous evolution and newer devices and techniques have been introduced during the course of the study. The documentation of materials of three patient's data, used in the Catheter Laboratory, was not retrievable.
CONCLUSIONS
Single wiring as an initial strategy in PCI for LAD-CTO lesions is associated with a high procedural success rate, by utilizing a wide variety of dedicated guidewires.
Successful GW crossing included a 44% majority of Soft Tapered GWs, 36% Soft Non-tapered, 16% Stiff Non-tapered GWs, and 4% Stiff-tapered GWs.
Case selection remains the key factor to maintain a balance among lesion complexity, procedural risk, and operator experience.
Footnotes
Source of Support: Toulouse Ranguil University Hospital
Conflict of Interest: None declared.
REFERENCES
- 1.Stone GW, Kandzari DE, Mehran R, Colombo A, Schwartz RS, Bailey S, et al. Percutaneous recanalization of chronically occluded coronary arteries: A consensus document: Part I. Circulation. 2005;112:2364–72. doi: 10.1161/CIRCULATIONAHA.104.481283. [DOI] [PubMed] [Google Scholar]
- 2.Christofferson RD, Lehmann KG, Martin GV, Every N, Caldwell JH, Christofferson RD, et al. Effect of chronic total occlusion on treatment strategy. Am J Cardiol. 2005;95:1088–91. doi: 10.1016/j.amjcard.2004.12.065. [DOI] [PubMed] [Google Scholar]
- 3.Delacretaz E, Meier B. Therapeutic strategy with total coronary artery occlusions. Am J Cardiol. 1997;79:185–7. doi: 10.1016/s0002-9149(96)00710-2. [DOI] [PubMed] [Google Scholar]
- 4.Bourassa MG, Roubin GS, Detre KM, Sopko G, Krone RJ, Attabuto MJ, et al. Bypass angioplasty revascularization investigation: Patient screening, selection, and recruitment. Am J Cardiol. 1995;75:3C–8C. [PubMed] [Google Scholar]
- 5.Prasad A, Rihal CS, Lennon RJ, Wiste HJ, Singh M, Holmes DR., Jr Trends in outcomes after percutaneous coronary intervention of chronic total occlusions: A 25 year experience from Mayo clinic. J Am Coll Cardiol. 2007;49:1611–8. doi: 10.1016/j.jacc.2006.12.040. [DOI] [PubMed] [Google Scholar]
- 6.Di Mario C, Werner GS, Sianos G, Galassi AR, Büttner J, Dudek D, et al. European perspective in the recanalisation of chronic total occlusions (CTO): Consensus document from the Euro CTO Club. Euro Intervention. 2007;3:30–43. [PubMed] [Google Scholar]
- 7.Srivatsa SS, Edwards WD, Boos CM, Grill DE, Sangiorgi GM, Garratt KN, et al. Histologic correlates of angiographic chronic total occlusion artery occlusion: Influence of occlusion duration on neovascular channel patterns and intimal plaque composition. J Am Coll Cardiol. 1997;29:955–63. doi: 10.1016/s0735-1097(97)00035-1. [DOI] [PubMed] [Google Scholar]
- 8.Godino C, Carlino M, Al-Lamee R, Colombo A. Coronary chronic total occlusion. Minerva Cardioangiol. 2010;58:41–60. [PubMed] [Google Scholar]
- 9.Munce NR, Straus BH, Qi X, Weisbrod MJ, Anderson KJ, Leung G, et al. Intravascular and extravascular microvessel formation in chronic total occlusions a micro-CT imaging study. JACC Cardiovasc Imaging. 2010;3:797–805. doi: 10.1016/j.jcmg.2010.03.013. [DOI] [PubMed] [Google Scholar]
- 10.Sumitsuji S, Inoue K, Ochiai M, Tsuchikane E, Ikeno F. Fundamental wire technique and current standard strategy of percutaneous intervention for chronic total occlusion With Histopathological Insights. JACC Cardiovasc Interv. 2011;4:941–51. doi: 10.1016/j.jcin.2011.06.011. [DOI] [PubMed] [Google Scholar]
- 11.Safley DM, House JA, Marso SP, Grantham JA, Rutherford BD. Improvement in survival following successful percutaneous coronary intervention of coronary chronic total occlusions: Variability by target vessel. JACC Cardiovasc Interv. 2008;1:295–302. doi: 10.1016/j.jcin.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 12.Rathore S, Katoh O, Matsuo H, Terashima M, Tanaka N, Kinoshita Y, et al. Retrograde percutaneous recanalization of chronic total occlusion of the coronary arteries: Procedural outcomes and predictors of success in contemporary practice. Circ Cardiovasc Interv. 2009;2:124–32. doi: 10.1161/CIRCINTERVENTIONS.108.838862. [DOI] [PubMed] [Google Scholar]
- 13.García-García HM, Kukreja N, Daemen J, Tanimoto S, van Mieghem C, Gonzalo N. Contemporary treatment of patients with chronic total occlusion: Critical appraisal of different state-of-the-art techniques and devices. EuroIntervention. 2007;3:188–96. doi: 10.4244/eijv3i2a34. [DOI] [PubMed] [Google Scholar]
- 14.Morino Y, Kimura T, Hayashi Y, Muramatsu T, Ochiai M, Noguchi Y, et al. J-CTO Registry Investigators. In-hospital outcomes of contemporary percutaneous coronary intervention in patients with chronic total occlusion insights from the J-CTO Registry (Multicenter CTO Registry in Japan) JACC Cardiovasc Interv. 2010;3:143–51. doi: 10.1016/j.jcin.2009.10.029. [DOI] [PubMed] [Google Scholar]
- 15.Mitsudo K, Yamashita T, Asakura Y, Muramatsu T, Doi O, Shibata Y, et al. Recanalization strategy for chronic total occlusions with tapered and stiff-tip guidewire. The results of CTO New techniQUE for STandard procedure (CONQUEST) trial. J Invasive Cardiol. 2008;20:571–7. [PubMed] [Google Scholar]
- 16.Katsuragawa M, Fujiwara H, Miyamae M, Sasayama S. Histologic studies in percutaneous transluminal coronary angioplasty for chronic total occlusion: Comparison of tapering and abrupt types of occlusion and short and long occluded segments. J Am Coll Cardiol. 1993;21:604–11. doi: 10.1016/0735-1097(93)90091-e. [DOI] [PubMed] [Google Scholar]


