Abstract
Major depressive disorder (MDD) co-occurs frequently with posttraumatic stress disorder (PTSD), and both disorders are linked to suicidal ideation. An emergent literature examines suicidal ideation in U.S. Afghanistan/Iraq-era veterans. Little research, however, has studied the role of PTSD and comorbid MDD on suicidal ideation across service eras. Therefore, this study aimed to examine the impact of depression on suicidal ideation in Afghanistan/Iraq-era and Vietnam-era veterans with PTSD. The sample included 164 Vietnam and 98 Afghanistan/Iraq veterans diagnosed with PTSD at a VA outpatient PTSD Clinic. Using structured interviews, 63% of the Vietnam sample and 45% of the Afghanistan/Iraq sample were diagnosed with comorbid current MDD. Measures included self-report assessments of PTSD and depressive symptoms and the Personality Assessment Inventory. Results of analyses suggested that in veterans of both eras, PTSD, MDD, and their interaction were significantly related to suicidal ideation (PTSD: η2 = .01; MDD: η2 = .10; PTSD × MDD: η2 = .02). For veterans reporting greater depressive symptoms, there was a stronger relationship between PTSD symptoms and suicidal ideation. These results suggest that veterans from both eras display a similar clinical presentation and highlight the need to consider depressive symptoms when assessing veterans with PTSD. Future research should examine suicidal ideation and behaviors as they change over time in these two cohorts.
Posttraumatic stress disorder (PTSD) is one the most frequently diagnosed psychiatric disorders in treatment-seeking veterans (Elhai, North, & Frueh, 2005). Of those veterans diagnosed with PTSD, many have comorbid psychiatric disorders, typically major depressive disorder (MDD), substance use disorders, and other anxiety disorders (Kulka et al., 1990). In fact, one study found that 69% of treatment-seeking individuals diagnosed with PTSD also met criteria for MDD (Brown, Campbell, Lehman, Grisham, & Mancill, 2001). Veterans with PTSD are also more likely to have social, occupational, and functional difficulties, including social isolation, frequent interpersonal altercations, and suicidal ideation (Panagioti, Gooding, & Tarrier, 2009). When the model contained age, major depression, and substance use, treatment-seeking veterans diagnosed with PTSD were four times more likely to endorse suicidal ideation than those without PTSD (Jakupcak et al., 2009).
PTSD and MDD occur together frequently, and both disorders have been separately linked to increased risk of suicidal ideation (Bryan & Corso, 2011; Guerra, Mid-Atlantic Mental Illness Research, Education and Clinical Center Workgroup, & Calhoun, 2011; Rudd, Goulding, & Bryan, 2011). It is unclear, however, whether the combination of comorbid MDD and PTSD confers an increased risk for suicidal ideation beyond the risk presented by either diagnosis alone (see Panagioti et al., 2009, for a review). Several studies of veteran samples have found that the combination of PTSD and MDD did not place individuals at greater risk for suicidal ideation than did a single diagnosis (Guerra et al., 2011; Jakupcak et al., 2009). Conversely, Oquendo and colleagues (2003) found that individuals with current MDD and comorbid PTSD were more likely to endorse suicidal ideation compared to those without a current PTSD diagnosis.
Previous research regarding the relationship between suicidal ideation and co-occurring MDD and PTSD has varied not only in its findings, but also in the measurement of these diagnostic variables. Some recent studies with veteran samples (Guerra et al., 2011; Jakupcak et al., 2009) analyzed MDD and PTSD dichotomously, whereas others (Bryan & Corso, 2011; Rudd et al., 2011) examined the data continuously. Bryan and Corso (2011) in particular emphasized the importance of continuous measurement to maximize external validity. Given the complex nature of the relationship among suicidal ideation, depression, and PTSD, the current study utilized continuous symptom measures of PTSD and MDD to allow a fuller representation of the presentation of veterans with PTSD, MDD, and suicidal ideation.
Although most studies have controlled for MDD in their analysis of PTSD and suicidal ideation, the goal of the current study was to examine the unique and interrelated effects of PTSD, depressive symptoms, and suicidal ideation among veterans presenting to a VA outpatient PTSD clinic for evaluation. PTSD and depressive symptoms were expected to interact such that those with the highest PTSD and depressive symptoms would endorse the most suicidal ideation.
The current study also involved an exploratory analysis of self-reported PTSD, MDD, and suicidal ideation in two different veteran service cohorts: Vietnam and Afghanistan/Iraq. Though the face of VA PTSD Clinics is changing with more Afghanistan/Iraq veterans returning home, there is limited research investigating differences in mental health outcomes (e.g., diagnostic status, Fontana & Rosenheck, 2008; quality of life, Schnurr, Lunney, Bovin, & Marx, 2009) based on service eras, yielding mixed results. Thus, both cohorts were included in the current study to inform this growing literature.
Method
Participants
Participants were drawn from 347 treatment-seeking veterans presenting to a VAMC outpatient PTSD Clinic for evaluation of PTSD between April 2003 and April 2008. Only veterans who met DSM-IV-TR criteria for PTSD (84%) were included. PTSD and MDD diagnoses were established through a structured clinical interview (Clinician Administered PTSD Scale [CAPS]; Blake et al., 1995) and the Major Depressive Disorder Module of the Structured Clinical Interview for DSM-IV [SCID]; First, Spitzer, Gibbon, & Williams, 1998). Only Vietnam-era and Afghanistan/Iraq-era veterans were included (19.51% excluded). Veterans with invalid profiles on the Personality Assessment Inventory (PAI; Morey, 1991), defined by Inconsistency scores above 73, Infrequency scores above 75, Negative Impression Management scores above 110, and Positive Impression Management scores above 68, were also excluded (11.78% excluded; guidelines proposed by Calhoun, Collie, Clancy, Braxton, & Beckham, 2010). This resulted in a final sample of 164 Vietnam-era veterans and 98 Afghanistan/Iraq-era veterans. Participants were mostly male (97%), almost half were Caucasian (46%), and over half were married (61%; no differences between eras). The mean age for Vietnam veterans was 56 years, and the mean age for Afghanistan/Iraq veterans was 32 years. A greater percentage of Afghanistan/Iraq veterans (68%) than Vietnam veterans (42%) were currently working, χ2(1, N = 261) = 17.41, p <.001), and the majority of those employed in both groups were fully employed (82% of Vietnam veterans and 84% of Afghanistan/Iraq veterans). Vietnam veterans were of slightly higher socioeconomic status (SES) than Afghanistan/Iraq veterans, t(258) = 3.88, p < .001 and were more likely to be diagnosed with MDD (63%) than Afghanistan/Iraq veterans (45%; χ2 (1, N = 258) = 8.20, p = .004). Participants reported being moderately impaired in occupational (M = 5.88, SD = 3.17), social (M = 6.89, SD = 2.64), and family (M = 6.54, SD = 2.86) domains (no differences between eras; Sheehan Disability Scale; Sheehan, 1983).
Measures
During a PTSD evaluation, veterans completed the following self-report measures in an initial visit and structured clinical interview (including the CAPS and MDD module of the SCID) in a second visit.
The PAI is a 344-item self-report measure of psychopathology. Items are rated on a 4-point Likert scale and combined to produce an overall profile consisting of four validity scales, 11 clinical scales, and five treatment scales. The current study utilized the Suicidal Ideation Scale (SUI) to measure thoughts about suicide. The scale consists of 12 items (e.g., “I’ve thought about death,” “I’ve made plans about how to kill myself”). The time frame for the PAI SUI is present-focused but open-ended, as it does not include specific participant instructions regarding time frame. Scores can be classified as follows: below 60T (no significant SI); 60T-69T (typical, transient SI); 70T-84T (recurrent but ambivalent SI); 85T-99T (more intense and frequent thoughts of suicide); and above 100T (preoccupation with thoughts of death, may have completed steps leading towards suicide). The scale demonstrates excellent reliability (α = .93 in the original clinical sample) and correlates with depression (i.e., Beck Depression Inventory), thus demonstrating good convergent validity (Morey, 1991). In the current sample, the PAI SUI was highly correlated with Item 9 on the BDI-II (r = .63, p < .001), a single-item measure sometimes used to predict severity of suicidal ideation when more comprehensive measures are not available (see Wenzel, Brown, & Beck, 2009).
In the current sample, 143 veterans (55%) scored below 60T, 45 (17%) scored 60T-69T, 47 (18%) scored 70T-84T, 14 (5%) scored 85T-99T, and 13 scored at or above 100T (5%). Distribution of scores did not differ by service era, χ2(4, N = 262) = 9.09, p = .059. Continuous PAI SUI scores were used as the dependent measure in all analyses.
The Davidson Trauma Scale (DTS; Davidson et al., 1997) is a 17-item self-report scale corresponding to DSM-IV criteria for PTSD. For each item, participants rate frequency and severity of reexperiencing (e.g., “Have you had distressing dreams of the event?”), avoidance (e.g.., “Have you had difficulty enjoying things?”), and hyperarousal (e.g., “Have you had difficulty concentrating?”) symptoms during the past week on a 5-point scale (maximum score = 136; sample α = .95).
The Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) contains 21 items rated on a 4-point scale. Scores represent depression symptom severity for the previous 2 weeks (maximum score = 63; sample α = .91).
Analyses
An ordinary least squares multiple regression analysis was conducted to investigate the relationship between service era, PTSD symptoms, depressive symptoms, and their interaction on suicidal ideation. Specifically, a multiple regression was conducted using DTS score (centered), BDI-II score (centered), service era, and all two-way and three-way interactions to account for PAI SUI scores. Due to the positive skew of the dependent variable, we considered log transformation or Poisson regression; however, these analytic strategies yielded a similar pattern of results. Therefore, for ease of interpretation, we utilized the raw data in the analyses, as least-squares estimation is robust to skew (Fox, 1984). To compensate for possible overlap in measurement of suicidal ideation and depressive symptoms, the analysis was repeated omitting Item 9 of the BDI-II from the total score. Again, the pattern of results did not substantially change; therefore, reported results include total BDI-II score to aid interpretability.
Results
Overall, participants reported high levels of PTSD (M = 95.12, SD = 25.66) and depressive symptoms (M = 31.53, SD = 11.41), and these scores were moderately correlated, r(260) = .61, p < .001. Scores for the two era samples were similar with the exception of BDI-II score, t(260) = 2.55, p = .011, such that Vietnam veterans reported higher levels of depressive symptoms (Vietnam: M = 32.90, SD = 11.67; Afghanistan/Iraq: M = 29.23, SD = 10.64).
The relationship between various demographic variables (i.e., age, gender, minority status, SES, education, work status, marital status, and alcohol use) and suicidal ideation was explored. Only education (B = −1.07, t = −2.34, p = .020) was significantly related to PAI SUI. Veterans with a higher educational level reported lower levels of suicidal ideation. Including significant demographics in the regression analysis did not change the pattern of results; therefore, to simplify reporting, the final model did not include demographics.
For the main multiple regression analysis, the overall model was significant, R2 = .33, F(7, 254) = 17.96, p < .001. DTS, BDI-II, and their interaction were significantly associated with PAI SUI, while service era and the remaining interactions were not significant (see Table 1). PTSD symptoms were positively associated with suicide at higher, but not lower levels of depression. That is, for veterans who reported lower levels of depression, PTSD symptoms were not significantly related to suicidal ideation; however, for those who reported higher depressive symptoms, experiencing more PTSD symptoms was associated with higher levels of suicidal ideation (see Figure 1).
Table 1.
Regression Analyses for Suicidal Ideation Using PTSD, Depression, and Service Era
| Variable | Estimate | B | SE | t | p | η2 |
|---|---|---|---|---|---|---|
| Intercept | 60.15 | 1.31 | 46.01 | <.001 | ||
| Service era | −0.38 | −0.01 | 2.12 | −0.18 | .86 | .00 |
| DTSa | 0.11 | 0.16 | 0.05 | 2.04 | .04 | .01 |
| BDI-IIa | 0.74 | 0.49 | 0.12 | 6.16 | <.001 | .10 |
| DTS × BDI-II | 0.01 | 0.16 | 0.00 | 2.50 | .01 | .02 |
| Service era × DTS | −0.04 | −0.03 | 0.11 | −0.37 | .71 | .00 |
| Service era × BDI-II | −0.03 | −0.01 | 0.21 | −0.14 | .89 | .00 |
| Service era × DTS × BDI-II | −0.00 | −0.01 | 0.01 | −0.12 | .90 | .00 |
Note. N = 262. PTSD = posttraumatic stress disorder; PAI SUI = Personality Assessment Inventory Suicidal Ideation Index; DTS = Davidson Trauma Scale; BDI = Beck Depression Inventory.
These variables were centered.
Figure 1.
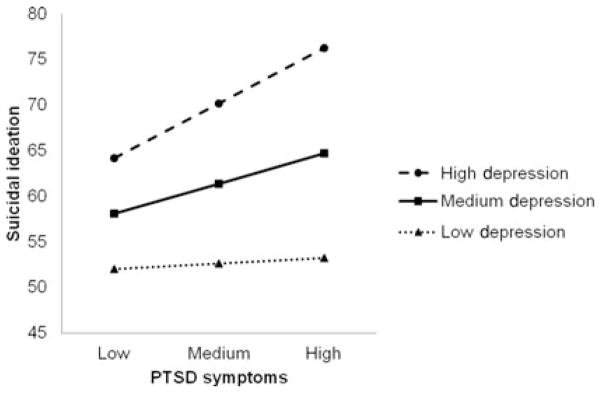
The relationship between posttraumatic stress disorder (PTSD) symptoms and suicidal ideation as a function of major depressive symptoms in treatment-seeking veterans with PTSD. For depression and PTSD, low is de-fined as one standard deviation below the sample mean; medium is the sample mean; high is one standard deviation above the sample mean.
Discussion
The current study analyzed comorbid PTSD and depressive symptoms and their relationship to suicidal ideation among Vietnam-era and Afghanistan/Iraq-era veterans seeking treatment for PTSD. This study extends previous research by examining symptom-level data in two service era groups. For both veteran cohorts, symptoms of PTSD and depression showed an interaction with suicidal ideation. There was also a main effect of both depression and PTSD on suicidal ideation.
The current findings help clarify previous research investigating the relationship between comorbidity and suicidal ideation (e.g., Guerra et al., 2011; Jakupcak et al., 2009). Comorbid PTSD and depressive symptoms were related to greater suicidal ideation in individuals seeking PTSD evaluation. Findings of some previous studies with veteran samples may differ because MDD and PTSD were analyzed categorically; the current study examined depression and PTSD continuously. Similar studies (i.e., Bryan & Corso, 2011) have emphasized the importance of continuous measurement of these variables to better approximate the clinical manifestation of the symptoms of PTSD and depression. This approach was also similar to that of Tarrier and Gregg (2004) who found that higher levels of self-reported depression were related to greater risk of suicidal ideation in a civilian sample of individuals with PTSD.
The current study has several limitations. The sample was predominantly treatment-seeking males at a VA PTSD outpatient clinic from two service eras, thus limiting generalizability. Also, the study employed self-report measures of PTSD and depressive symptoms and a nontraditional measure of suicidal ideation (the PAI SUI subscale); however, the PAI is increasingly used in VA outpatient clinics as a measure of psychopathology (Calhoun et al., 2010). Therefore, these results have additional applicability to clinicians routinely using these measures in assessments. Because the sample comprised only veterans diagnosed with PTSD, there was a restricted range of PTSD symptoms. Future studies should examine a more diverse sample of veterans and utilize clinician-rated symptom severity measures. Future research should also employ a measure of suicidal behavior in addition to suicidal ideation, as previous research has indicated an imperfect relationship between these two constructs. Finally, longitudinal analyses would allow research to investigate cohort effects and time effects simultaneously.
The current study extends our understanding of the complex relationship among symptoms of PTSD, depression, and suicidal ideation. Clinicians should take level of depressive symptoms into consideration when assessing veterans with PTSD, as results suggest that reporting high levels of both PTSD and depressive symptoms is associated with higher levels of suicidal ideation. The severity of both PTSD and depressive symptoms offers valuable information about suicidal ideation beyond that of each diagnostic category alone, and this information should be used to inform suicide prevention efforts as part of treatment planning. Improving our understanding of PTSD and depressive symptoms and their relationship to suicidal ideation will help guide not only early intervention efforts for newly returning veterans with PTSD, but also ongoing efforts to address chronic PTSD and depressive symptoms in Vietnam veterans.
Acknowledgments
We would like to thank Michelle Dennis for assisting with data management. We would also like to acknowledge Laura Hayward for her assistance with data analysis while this manuscript was being revised.
References
- Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corp; 1996. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of Abnormal Psychology. 2001;110:585–599. doi: 10.1037//0021-843X.110.4.585. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Corso KA. Depression, PTSD, and suicidal ideation among active duty veterans in an integrated primary care clinic. Psychological Services. 2011;8:94–103. doi: 10.1037/a0023451. [DOI] [Google Scholar]
- Calhoun PS, Collie CF, Clancy CP, Braxton LE, Beckham JC. Use of the PAI in assessment of posttraumatic stress disorder among help-seeking veterans. In: Blais MA, Baity MR, Hopwood CJ, editors. Clinical applications of the Personality Assessment Inventory. New York: Routledge Taylor & Francis Group; 2010. pp. 93–112. [Google Scholar]
- Davidson JRT, Book SW, Colket JT, Tupler LA, Roth S, David D, Feldman ME. Assessment of a new self-rating scale for post-traumatic stress disorder: The Davidson Trauma Scale. Psychological Medicine. 1997;27:153–160. doi: 10.1017/S0033291796004229. [DOI] [PubMed] [Google Scholar]
- Elhai JD, North TC, Frueh BC. Health service use predictors among trauma survivors: A critical review. Psychological Services. 2005;2:3–19. doi: 10.1037/1541-1559.2.1.3. [DOI] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM–IV Axis I Disorders. New York: Biometrics Research, New York State Psychiatric Institute; 1998. (Patient ed.) [Google Scholar]
- Fontana A, Rosenheck R. Treatment-seeking veterans of Iraq and Afghanistan: Comparison with veterans of previous wars. The Journal of Nervous and Mental Disease. 2008;196:513–521. doi: 10.1097/NMD.0b013e31817cf6e6. [DOI] [PubMed] [Google Scholar]
- Fox J. Linear statistical models and related methods: With applications to social research. New York: Wiley; 1984. [Google Scholar]
- Guerra VS, Calhoun PS Mid-Atlantic Mental Illness Research, Education Clinical Center Workgroup. Examining the relation between posttraumatic stress disorder and suicidal ideation in an OEF/OIF veteran sample. Journal of Anxiety Disorders. 2011;25:12–18. doi: 10.1016/j.janxdis.2010.06.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakupcak M, Cook J, Imel Z, Fontana A, Rosenheck R, McFall M. Posttraumatic stress disorder as a risk factor for suicidal ideation in Iraq and Afghanistan war veterans. Journal of Traumatic Stress. 2009;22:303–306. doi: 10.1002/jts.20423. [DOI] [PubMed] [Google Scholar]
- Kulka RA, Schlenger WE, Fairbank JA, Hough RL, Jordan BK, Marmar CR, Weiss DS. Trauma and the Vietnam war generation: Report of findings from the National Vietnam Veterans Readjustment Study. Philadelphia, PA: Brunner/Mazel; 1990. [Google Scholar]
- Morey LC. The Personality Assessment Inventory professional manual. Odessa, FL: Psychological Assessment Resources; 1991. [Google Scholar]
- Oquendo MA, Friend JM, Halberstam B, Brodsky BS, Burke AK, Grunebaum, Mann JJ. Association of comorbid posttraumatic stress disorder and major depression with greater risk for suicidal behavior. American Journal of Psychiatry. 2003;160:580–582. doi: 10.1176/appi.ajp.160.3.580. [DOI] [PubMed] [Google Scholar]
- Panagioti M, Gooding P, Tarrier N. Post-traumatic stress disorder and suicidal behavior: A narrative review. Clinical Psychology Review. 2009;29:471–482. doi: 10.1016/j.cpr.2009.05.001. [DOI] [PubMed] [Google Scholar]
- Rudd MD, Goulding J, Bryan CJ. Student veterans: A national survey exploring psychological symptoms and suicide risk. Professional Psychology: Research and Practice. 2011;42:354–360. doi: 10.1037/a0025164. [DOI] [Google Scholar]
- Schnurr PP, Lunney CA, Bovin MJ, Marx BP. Posttraumatic stress disorder and quality of life: Extension of findings to veterans in the wars in Iraq and Afghanistan. Clinical Psychology Review. 2009;29:727–735. doi: 10.1016/j.cpr.2009.08.006. [DOI] [PubMed] [Google Scholar]
- Sheehan DV. The anxiety disease. New York: Scribner; 1983. [Google Scholar]
- Tarrier N, Gregg L. Suicide risk in civilian PTSD patients: Predictors of suicidal ideation, planning, and attempts. Social Psychiatry and Psychiatric Epidemiology. 2004;39:655–661. doi: 10.1007/s00127-004-0799-4. [DOI] [PubMed] [Google Scholar]
- Wenzel A, Brown GK, Beck AT. Cognitive therapy for suicidal patients: Scientific and clinical applications. Washington, DC: American Psychological Association; 2009. [Google Scholar]


