Abstract
The objectives were to prospectively assess determinants of apolipoproteins B (ApoB), A1 (ApoA1), and the ApoB/ApoA1 ratio in 797 healthy black and white schoolgirls from mean ages 10 to 19. There was prospective 9-year follow-up, with measures of ApoB at mean ages 10, 12, 14,16 and 19, ApoA1at mean ages 12, 14, 16, and 19, and assessment of annual reports of delayed menstrual cyclicity (≥42 days) from ages 14 to 19. Studies of 402 black and 395 white healthy schoolgirls were done in public and private schools, in urban and suburban Cincinnati. Black girls had lower ApoB, higher ApoA1, and lower ApoB/ApoA1. SHBG at age 14 in white and black girls was inversely correlated with the ApoB/ApoA1. At age 19, ≥3 annual reports of menstrual delay ≥42 days and metabolic syndrome were associated with higher ApoB and a higher ApoB/ApoA1 ratio. From ages 14 to 19, BMI and TG were independently positively associated with ApoB. Menstrual cyclicity ≥42 days, metabolic syndrome, BMI, and TG were independently positively associated with ApoB/ApoA1 ratios, while black race was negatively associated. The atherogenic ApoB/ApoA1 ratio from ages 14 to 19 is lower in black girls, and positively associated with hyperandrogenism, menstrual cyclicity ≥42 days, BMI, TG, and the metabolic syndrome, facilitating an adolescent approach to primary prevention of cardiovascular disease.
1. Introduction
Secular trends in childhood and adolescence of increasing obesity [1], insulin resistance, and the associated metabolic syndrome should overall increase the atherogenic ApoB/ ApoA1 ratio, an independent prospective predictor of myocardial infarction in men [2,3]. Apolipoprotein B (ApoB), the primary protein moiety associated with VLDL and LDL cholesterol (VLDC, LDLC), may be an optimal index for assessing risk for cardiovascular disease, particularly in patients with type 2 diabetes mellitus or metabolic syndrome where LDLC may not be high, but there are increased numbers of small dense LDL particles, rich in ApoB [4]. Each molecule of very low-, intermediate-, and low-density lipoprotein cholesterol has one ApoB100 molecule. ApoB48, produced in the gut, is associated with chylomicrons, which transfer post-prandial triglyceride (TG) from the intestine to blood stream, but in fasting subjects with normal TG levels (<200 mg/dL), the total ApoB level represents the aggregate of atherogenic lipoproteins [5]. There is a common genetic origin of ApoB100 and ApoB48 [6]. ApoAI, the primary protein moiety associated with HDL cholesterol (HDLC) [7], is a major index of anti-atherogenic risk. The ApoB/ApoA1 ratio is related in adults to the metabolic syndrome, and to measures of insulin resistance (euglycemic insulin clamp glucose disposal rate) [2]; these factors, as well as plasma insulin [8] have been shown to be independent, prospective predictors of myocardial infarction in a community-based sample of middle-aged men [2]. In addition, the ApoB/ApoA1 ratio is associated with the metabolic syndrome in obese children [9].
In the Bogalusa Heart Study, low apoA1, a low ApoA1/ ApoB ratio, and a low LDLC/ApoB ratio in children were strongly related to parental incidence of myocardial infarction [10]. White children had lower ApoA1 and ratios of LDL cholesterol to ApoB than black children [10]. Hereditary influences on LDL cholesterol and ApoB were more important in white than in black children especially for ApoB [11]. The best predictor of the atherogenic ratio of LDL cholesterol to ApoB (higher ratio is less atherogenic) was HDL cholesterol or the more dense fraction of HDL (HDL-2 cholesterol) in all 4 sex–race groups [12].
In the current report, using data on 797 healthy schoolgirls in the Cincinnati Clinic of the National Growth and Health Study (NGHS), prospectively studied from mean ages 10 to 19, our specific aim was to examine determinants of Apo A1, Apo B, and the ApoB/ApoA1 ratio.
2. Materials and methods
2.1. The study population
In 1987, the National Heart, Lung, and Blood Institute (NHLBI) initiated a 10-year longitudinal multicenter study (the NHLBI Growth and Health Study [NGHS] [13–15]) to assess the development of obesity in black and white girls during adolescence and its environmental, psychosocial, and cardiovascular risk factor (CVD) correlates [14–16]. Participant eligibility was limited to black and white girls who were within 2 weeks of ages 9–10 years and lived in racially concordant households. Race was self-declared by both girls and parents and guardians. Annual visits were carried out from 9–10 years of age through 18–19 years of age.
2.2. IRB approval
In the NGHS [14] and the ancillary studies [17], procedures followed were in accordance with the ethical standards of the Institutional Review Board of the Cincinnati Children's Hospital, which approved the study. Signed informed consent was obtained from the girls' parents or guardians and assent from the girls in NGHS. After age 18, the girls signed informed consent for themselves.
2.3. Clinical data collection
As previously described, centrally trained staff used standard protocols [14] for annual measures of systolic and diastolic blood pressure and anthropometric data, including body mass index (kg/m2) to assess overweight and waist (beginning in Year 2) to assess fat patterning [15].
A single, trained registered nurse practitioner assessed sexual maturation annually during a brief physical examination and ascertained onset of menarche annually by interview. Most girls are menarchal [18] by age 14, up to 98% of whites, 97% of blacks [15,19]. In post-menarchal girls, the nurse practitioner recorded the number of days since the previous menstrual cycle and whether the participant was pregnant [13,14,17,20]. As previously described [20–22], in post-menarchal girls, we used previously reported cutpoints for menstrual delay(≥42 days since the last menses cycle [18,23,24]), assessing 6 annual reports from ages 14 to 19 years. We based our cutpoint for delayed menstrual cyclicity on the reports of Van Hooff et al [23,24] and Chiazze et al [18]. In a population study by Chiazze et al, in 15–19 year old girls, average menstrual cycle length was >40 days in 2.5% of girls [18]. Defining oligomenorrhea in 15-year old white Dutch girls by menses ≥42 days, Van Hooff et al [23,24] reported that oligomenorrheic girls were more likely than girls with either irregular or normal menses to be hyperandrogenic and to have polycystic ovaries.
Fasting blood was drawn for measures of lipid profiles, ApoB, and ApoA1 at mean ages 10, 12, 14, 16, and 19 [14]. Registered dietitians retrieved 3-day dietary records that included two week days and a weekend day at mean ages 10, 11, 12, 13, 14, 16, 17 and 19 [14]. Records were coded for calculation of total calories and calories from protein, fat, and carbohydrate using the most recent version of the Nutrition Data System for Research Software [14,25] developed by the Nutrition Coordinating Center, U Minnesota, Minneapolis, MN.
NGHS protocols for the collection of data on elective behaviors, including physical activity, and TV viewing time have been described previously [14,25]. A pedometer (Caltrac ) [26] was used over one 24-h period including a school day, to record activity. A longitudinally validated habitual physical activity questionnaire (HAQ) [26–28] was used to measure leisure-time physical activity including a school day, and separately for a summer day, once per year from ages 10 to 17. A general physical activity questionnaire was filled out at age 19 [26–28].
In addition, in ancillary projects, the Cincinnati Clinic measured total and free testosterone [29,30], DHEAS, and sex hormone binding globulin (SHBG) [31] at age 14, insulin at mean ages 10, 16, and 19, and glucose at ages 10 and 19.
2.4. Laboratory measurements and clinical definitions
Methods for measurement of all metabolites have been previously described [14]. Since different reagents were used for ApoAI in the measurements at each follow up visit, a sample (n = 168) of sera aliquots from Years 3, 5, 7, and 10 stored at −80 °C was re-tested at the Cleveland Clinic Lipid Laboratory using a single common reagent [32]. Since different reagents were used for ApoB only in the measurements at Year 10, ApoB was re-measured (n = 65) by the Cleveland Clinic Lipid Laboratory on the Year 7 and 10 samples using a single common reagent [32].
Pediatric metabolic syndrome was defined at mean age 14 by ≥3 of the following 5 risk factors as previously described [33]: TG ≥110 mg/dL, BMI≥the race–age specific 90th percentile, systolic or diastolic blood pressure≥the age- height-specific 90th percentile, HDLC≤50 mg/dL, and glucose ≥100 mg/dL. Metabolic syndrome (MetS) was also determined at each year by adult MetS criteria [34], ≥3 of the following 5 conditions: TG≥150 mg/dL, waist circumference >88 cm, systolic or diastolic blood pressure ≥130/85 mmHg, HDLC<50 mg/dL, and glucose ≥100 mg/dL. MetS category was defined as: 0=had neither pediatric nor adult MetS, 1=had either pediatric or adult MetS, 2=had both.
2.5. Statistical analysis
2.5.1. Statistical analyses were done using SAS version 9.1.3
Based on the ApoB and ApoA1 measurements using specific reagents which were used in NGHS and re-tested using a standard reagent (available in subsets, n = 168, n = 65), linear regression formulae were constructed to convert all ApoB, ApoA1 measures corresponding to the common reagent. Only the standardized ApoB, ApoA1 measures were exhibited in current report.
2.6. Cross sectional analyses
Demographic data were summarized separately by race and study year, and black–white differences at each year were assessed by Student's t tests.
Mean and 95% CI of ApoB, ApoA1, ApoB/ApoA1 at age 19 were calculated for categories of variables: metabolic syndrome [yes, no], insulin and glucose [highest vs other quintiles], and menses delay category (total number of annual reports of menstrual cyclicity ≥42 days during age 14–19, [0, 1, 2, ≥3]), comparisons of ApoB, ApoA1, ApoB/ ApoA1 among categories used analysis of variance after adjusting for race.
Spearman correlations were calculated between sex hormones and SHBG at age 14, and ApoB, ApoA1, and ApoB/ ApoA1 at ages 14, and the participants' last ApoB and ApoA1 measures during age 17–19, by race.
2.7. Longitudinal analyses
To view the profile of unadjusted ApoB, ApoA1, and the ApoB/ ApoA1 ratio over time in each race, repeated measures of ApoB, ApoA1 and ApoB/ApoA1 were fit by ordinary linear regression models of age, age2 and interaction with race for girls who had at least 3 measures. The predicted mean values and their 95% CI were plotted.
To assess independent determinants of the outcome variables of interest over time, mixed models for repeated measures analyses were used to assess ApoA1, ApoB, and the ApoB/ApoA1 ratio during ages 14 to 19. First, an ordinary linear regression with stepwise selection was carried out with the independent variables: race, age, BMI, waist circumference, TG, annual report of menstrual cycles ≥42 days, total calorie intake, % calorie from protein, % calories from fat, physical activity during a school day, physical activity during a summertime day (all during the same year); pediatric MetS, and MetS category. And multiple imputation for the explanatory variables was carried out (10 imputations) to maximize the number of observations which could be used in the model. Then, for each imputation the mixed model was constructed including only the significant explanatory variables from the stepwise selection above (as fixed effects), and subjects (girls' ID) as the blocking variable (random effect) with an AR (1) covariance structure. Finally, SAS MI analyze procedure was used to combine all 10 models to estimate the parameters.
3. Results
Girls with type 1 diabetes mellitus (n = 7) were excluded from the analysis sample for this report, as described previously [35], and 7 observations were excluded due to pregnancy. Four hundred and ninety-three girls had measures of sex hormones at age 14. Data on onset of menarche were obtained in 737 girls. Measures of ApoB were done in 797 girls, of whom 765 had data on length of menstrual cycles.
In the total cohort of 737 girls having data on onset of menarche, 1.5% had onset at age 10, 9.5% by age 11, 35% by age 12, 66% by age 13, 90% by age 14, 97% by age 15, 99% by age 16, and 100% by age 17. There was no association between age at menarche and the total number of annual reports of menstrual cycles ≥42 days from ages 14 to 19, Mantel– Haenszel X2 = 0.0026, p = .96.
Of 765 girls who had annual reports of menstrual cycle length, at age 14, 7% had cycles ≥42 days; at age 15, 6%; at age 16, 5%; at age 17, 9%; at age 18, 9%; at age 19, 10%; and for all 6 years from age 14 to 19, 8%.
Of the 765 girls with annual reports of menstrual cycle length, from ages 14 to 19, 564 (74%) had no menstrual cycles ≥42 days, 152 (20%) had 1 annual report ≥42 days, 35 (5%) had 2 reports ≥42 days, and 14 (1.8%) had ≥3 reports ≥42 days . Of the 14 girls who reported ≥3 annual reports of menstrual cycles ≥42 days, in 8 girls, cycles ≥42 days were sequential, 2 girls first reported delayed menses at age 14, 3 at age 15, and 3 at age 17. In 6 girls reporting ≥3 cycles ≥42 days, menstrual delays were intermittent, with 3 girls starting at age 14 and 3 starting at age 16.
ApoA1 and ApoB measurements were done in 797 girls, 395 white and 402 black during ages 10–19. Measurements for ApoB were obtained at ≥3 visits in 481 girls (60%). Comparing the 316 girls with <3 ApoB measures vs the 481 girls with ≥3 measurements, there were no differences in race, BMI, TG, LDLC, ApoA1, ApoB/ApoA1, LDLC/ApoB (all p > 0.2), however, the group with <3 ApoB measures was younger (13.7 ± 3.3 vs 14.0 ± 3.1 years, p = .01), and, pooling all ApoB measurements, had higher ApoB (73.4 ± 17.7 vs 71.7 ± 16.6 mg/dL, p = .05).
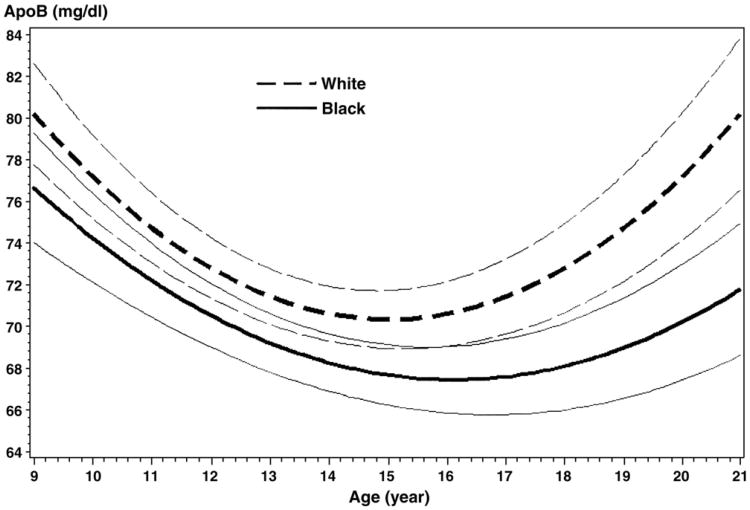
Of 2288 total measurements of ApoB, 1811 measures (79%) were obtained in 481 girls (243 W, 238 B) who had ≥3 measurements. Over 9 years of follow-up, ApoB levels in both white and black girls could be modeled as quadratic curves of age, main difference was a vertical shift (p = .005), with lower ApoB levels in blacks, Fig. 1:
White: ApoB = 131.9 − 8.2*age + 0.27*age2 (a concave parabola)
Black: ApoB = 114.6 − 5.8*age + 0.18*age2 (a concave parabola).
Fig. 1.
ApoB (mg/dL) in black and white girls from ages 10–19, mean and 95% confidence intervals.
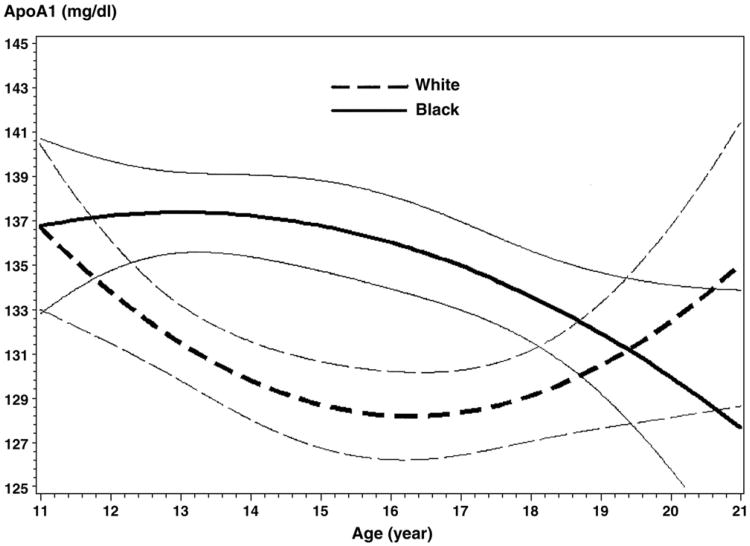
At mean ages 12, 14, 16, and 19, measurements for ApoA1 were obtained at ≥3 visits for 336 girls (177 white, 159 black). Of 1741 total measurements of ApoAI, 1130 measures (65%) were obtained in girls who had ≥3 measurements. Over the 7 years of follow-up, ApoA1 levels could be modeled as quadratic curves for white and black groups, but different in intercept (p = .009), in coefficient of age term (p = .004), and in coefficient of age2 term (p = .004), Fig. 2:
White: ApoA1 = 209.3 − 9.9*age + 0.31*age2 (a concave parabola)
Black: ApoA1 = 111.3 + 4.0*age − 0.16*age2 (a convex parabola).
Fig. 2.
ApoA1 (mg/dL) in black and white girls from ages 12–19, mean and 95% confidence intervals.
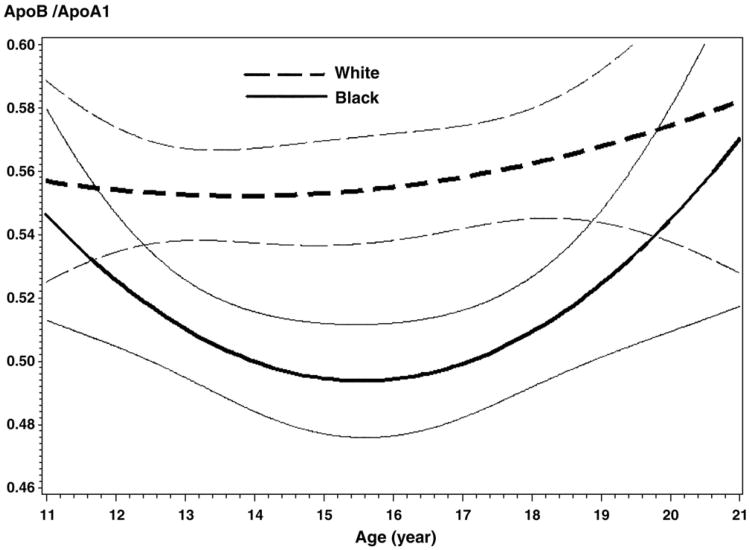
Over the 7 years of follow-up, the ApoB/ApoA1 ratios (n = 1130) could be modeled as an almost level straight line for whites and quadratic curve for black (all the 3 coefficients differ, p ≤ .01), as in Fig. 3:
White: ApoB/ApoA1 = 0.53 + 0.0018*age (a straight line)
Black: ApoB/ApoA1 = 1.11 − 0.079*age +0.0026*age2 (a concave parabola).
Fig. 3.
ApoB/ApoA1 ratio in black and white girls from ages 12–19, mean and 95% confidence intervals.
ApoB was lower in black than in white girls, significantly lower at ages 10 (74 ± 17 vs 78 ± 17 mg/dL), 14 (68 ± 15 vs 72 ± 15 mg/dL), and 19 (71 ± 17 vs 75 ± 21 mg/dL), Table 1. ApoA1 was higher in black than white girls, significantly higher at ages 12 (138 ± 14 vs 134 ± 13 mg/dL), 14 (138 ± 21 vs 131 ± 19 mg/dL), and 16 (136 ± 19 vs 131 ± 17 mg/dL), Table 1.
Table 1.
ApoA1, ApoB, and ApoB/ApoA1 in white and black girls, ages 10–19, in the NGHS study.
| Mean Age | White | Black | White vs Black | ||
|---|---|---|---|---|---|
|
|
|
|
|||
| n | Mean [95% CI of mean] | n | Mean [95% CI of mean] | Diff [95%CI] | |
| ApoB (mg/dL) | |||||
| 10 | 298 | 77.6 [75.6, 79.6] | 246 | 73.7 [71.6, 75.8] | 3.9 [1.0, 6.8]† |
| 12 | 233 | 73.1 [71.3, 74.9] | 242 | 72.1 [70.1, 74.0] | 1.0 [−1.6, 3.7] |
| 14 | 212 | 72.4 [70.4, 74.5] | 195 | 67.8 [65.6, 69.9] | 4.6 [1.7, 7.6]† |
| 16 | 232 | 69.2 [66.9, 71.6] | 231 | 66.5 [64.5, 68.5] | 2.8 [−0.3, 5.9] |
| 19 | 183 | 74.9 [71.9, 77.9] | 216 | 71.0 [68.7, 73.3] | 3.9 [0.2, 7.5]* |
| ApoA1 (mg/dL) | |||||
| 10 | 0 | 0 | |||
| 12 | 233 | 134.4 [132.8, 136.1] | 241 | 137.6 [135.9, 139.3] | −3.2 [−5.5, −0.8]† |
| 14 | 212 | 130.7 [128.2, 133.3] | 195 | 138.2 [135.3, 141.2] | −7.5 [−11.4, −3.7]§ |
| 16 | 232 | 130.8 [128.7, 133.0] | 229 | 135.6 [133.1, 138.0] | −4.7 [−8.0, −1.4]† |
| 19 | 183 | 130.0 [127.8, 132.2] | 216 | 129.3 [127.6, 131.0] | 0.7 [−2.0, 3.4] |
| ApoB/ApoA1 | |||||
| 10 | 0 | 0 | |||
| 12 | 233 | 0.55 [0.53, 0.56] | 241 | 0.53 [0.51, 0.54] | 0.02 [0.0002, 0.04]* |
| 14 | 212 | 0.57 [0.55, 0.59] | 195 | 0.50 [0.48, 0.52] | 0.07 [0.04, 0.09]§ |
| 16 | 232 | 0.54 [0.52, 0.56] | 229 | 0.50 [0.48, 0.52] | 0.04 [0.01, 0.06]† |
| 19 | 183 | 0.58 [0.56, 0.61] | 216 | 0.55 [0.53, 0.57] | 0.03 [−0.002, 0.06] |
p < .05.
p < .01.
p < .0001.
TG levels were lower in black than in white girls at age 10 (74 ± 30 vs 82 ± 33 mg/dL), at age 12 (77 ± 35 vs 94 ± 37 mg/dL), at age 14 (70 ± 30 vs 91 ± 47 mg/dL), at age 16 (71 ± 30 vs 93 ± 53 mg/ dL), at age 19 (76 ± 35 vs 98 ± 51 mg/dL); LDLC and the LDLC/ ApoB ratio did not differ significantly by race, Table 2.
Table 2.
Triglyceride, LDL cholesterol, and the ratio of LDL cholesterol to ApoB in white and black girls in the NGHS study.
| Mean Age | White | Black | White vs Black | ||
|---|---|---|---|---|---|
|
|
|
|
|||
| n | Mean [95% CI of mean] | n | Mean [95% CI of mean] | Diff [95%CI] | |
| TG (mg/dL) | |||||
| 10 | 298 | 82 [78, 86] | 246 | 74 [70, 78] | 8 [2, 13]† |
| 12 | 233 | 94 [89, 99] | 242 | 77 [73, 82] | 17 [11, 24]§ |
| 14 | 212 | 91 [84, 97] | 195 | 70 [66, 74] | 21 [13, 28]§ |
| 16 | 232 | 93 [87, 100] | 231 | 71 [68, 75] | 22 [14, 30]§ |
| 19 | 183 | 98 [91, 106] | 216 | 76 [71, 81] | 22 [14, 31]§ |
| LDL cholesterol (mg/dL) | |||||
| 10 | 295 | 108 [104, 111] | 246 | 103 [100, 107] | 4 [−0.5, 9.3] |
| 12 | 233 | 98 [95, 101] | 242 | 99 [95, 102] | −0.6 [−5, 4] |
| 14 | 212 | 93 [90, 97] | 195 | 88 [85, 92] | 5 [−0.3, 10] |
| 16 | 231 | 95 [91, 98] | 229 | 93 [89, 96] | 2 [−3, 7] |
| 19 | 182 | 101 [96, 106] | 216 | 97 [94, 101] | 3 [−2, 10] |
| LDL/ApoB | |||||
| 10 | 295 | 1.40 [1.37, 1.44] | 246 | 1.41 [1.38, 1.45] | −0.01 [−0.06, 0.04] |
| 12 | 233 | 1.33 [1.30, 1.35] | 242 | 1.35 [1.33, 1.38] | −0.03 [−0.06, 0.005] |
| 14 | 212 | 1.27 [1.25, 1.29] | 195 | 1.30 [1.27, 1.32] | −0.02 [−0.05, 0.01] |
| 16 | 231 | 1.37 [1.35, 1.39] | 229 | 1.40 [1.37, 1.42] | −0.03 [−0.06, 0.007] |
| 19 | 182 | 1.34 [1.31, 1.36] | 216 | 1.36 [1.34, 1.38] | −0.02 [−0.06, 0.01] |
p < .01.
p < .0001.
At age 19, girls with ≥3 reports of cycles ≥42 days had the highest ApoB compared to girls with 2, 1, and 0 menses delays, and they also had a higher ApoB/ApoA1 ratio than girls with 0 or 1 menses delay, Table 3. Girls with 2 menses cycles ≥42 days had lower ApoA1 than girls with no menses delay, Table 3. Girls with the metabolic syndrome had higher ApoB, lower ApoA1, and a higher ApoB/ApoA1 ratio than those without metabolic syndrome, Table 3. Top quintile insulin was associated with lower ApoA1 and with a higher ApoB/ApoAl ratio, Table 3. TG was positively correlated with the ApoB/ApoA1 ratio, Table 3.
Table 3.
Relationships of metabolic syndrome, menstrual cycles ≥42 days, insulin, glucose and triglyceride to ApoB, ApoA1 and ApoB/ApoA1 at age 19.
| ApoB (mg/dL) | n | Mean [95% CI of mean] |
|---|---|---|
| ALL | 399 | 72.8 [70.9, 74.6] |
| No menses delay during age 14–19 | 279 | 72.9 [70.7, 75.1] |
| 1 delay during age 14–19 | 85 | 71.5 [67.5, 75.5] |
| 2 delays during age 14–19 | 24 | 70.3 [62.8, 77.8] |
| ≥3 delays during age 14–19 | 11 | 84.6 [73.0, 96.2] * vs all other 3 categories |
| MetS at same year | 22 | 85.2 [75.0, 95.3] |
| Not | 375 | 72.0 [70.1, 73.8] ‡ |
| Insulin in top quintile | 77 | 74.8 [70.7, 78.9] |
| Not | 309 | 72.2 [70.1, 74.4] |
| Glucose in top quintile | 72 | 72.1 [67.7, 76.5] |
| Not | 295 | 72.5 [70.3, 74.6] |
| Correlation with Triglyceride | 399 | Spearman r=0.45§ |
| ApoA1 (mg/dL) | ||
| ALL | 399 | 129.6 [128.3, 131.0] |
| No menses delay during age 14–19 | 279 | 130.4 [128.8, 132.1] |
| 1 delay during age 14–19 | 85 | 128.5 [125.6, 131.4] |
| 2 delays during age 14–19 | 24 | 124.4 [118.9, 129.9]* vs no delay |
| ≥3 delays during age 14–19 | 11 | 127.9 [119.4, 136.4] |
| MetS at same year | 22 | 122.7 [117.4, 128.1] |
| Not | 375 | 130.1 [128.7, 131.5]* |
| Insulin in top quintile | 77 | 124.5 [121.7, 127.4] |
| Not | 309 | 130.6 [129.1, 132.1]‡ |
| Glucose in top quintile | 72 | 127.4 [124.3, 130.4] |
| Not | 295 | 130.0 [128.5, 131.6] |
| Correlation with Triglyceride | 399 | Spearman r = 0.12* |
| ApoB/ApoA1 | ||
| ALL | 399 | 0.57 [0.55, 0.58] |
| No menses delay during age 14–19 | 279 | 0.56 [0.55, 0.58] |
| 1 delay during age 14–19 | 85 | 0.56 [0.53, 0.59] |
| 2 delays during age 14–19 | 24 | 0.57 [0.51, 0.63] |
| ≥3 delays during age 14–19 | 11 | 0.66 [0.57, 0.76]* vs no delay, vs 1 delay |
| MetS at same year | 22 | 0.70 [0.61, 0.79] |
| Not | 375 | 0.56 [0.54, 0.57]§ |
| Insulin in top quintile | 77 | 0.61 [0.57, 0.64] |
| Not | 309 | 0.56 [0.54, 0.57]† |
| Glucose in top quintile | 72 | 0.57 [0.53, 0.61] |
| Not | 295 | 0.56 [0.54, 0.58] |
| Correlation with Triglyceride | 399 | Spearman r = 0.38§ |
Adjusted for race, differ between categories:
<.05;
p < .01;
p < .001;
p < .0001.
At age 14, in both white and black girls, the ApoB/ApoA1 ratio was inversely correlated with SHBG, Table 4. In black girls, at ages 17–19, ApoB and ApoB/ApoAl ratio were inversely correlated with age 14 SHBG, and ApoA1 was positively correlated with age 14 SHBG, Table 4.
Table 4.
Spearman correlations between age 14 free testosterone, DHEAS, sex hormone binding globulin (SHBG) and ApoB, ApoA1, ApoB/ApoA1 at mean ages 14, and 17–19 in NGHS girls.
| White (n=237), free testosterone, DHEAS and SHBG measured at age 14 yrs (13.9 ±0.4, median 13.9) | |||
|---|---|---|---|
|
| |||
| Free Testosterone 1.24±0.63, median 1.16 (pg/mL) | DHEAS 179±106, median 157 (mcg/dL) | SHBG 19.1 ±10.9, median 17.0 (nmol/L) | |
| ApoB at age 14 | r=−0.028, n=201 | r=−0.034, n=201 | r=−0.089, n=201 |
| ApoB at age 17–19 | r=−0.032, n=190 | r=−0.061, n=190 | r=−0.062, n=190 |
| ApoA1 at age 14 | r=−0.082, n=201 | r=−0.0088, n=201 | r=0.084, n = 201 |
| ApoA1 at age 17–19 | r=−0.10, n=190 | r=−0.080, n=190 | r=0.14, n = 190 |
| ApoB/ApoA1 at age 14 | r=0.020, n=201 | r=−0.0092, n=201 | r=−0.15*, n = 201 |
| ApoB/ApoA1 at age 17–19 | r=0.013, n=190 | r=−0.0052, n=190 | r=−0.12, n=190 |
| Black (n = 253), free testosterone, DHEAS and SHBG measured at age 14 yrs (14.0±0.5, median 14.0 ) | |||
|
| |||
| Free Testosterone 1.18±0.75, median 1.06 | DHEAS 179±91, median 161 | SHBG 18.5±9.9, median 17.0 | |
|
| |||
| ApoB at age 14 | r=0.0070, n=185 | r=−0.043, n=185 | r=−0.14, n=185 |
| ApoB at age 17–19 | r=0.083, n=195 | r=−0.067, n=195 | r=−0.23†, n = 195 |
| ApoA1 at age 14 | r=−0.049, n=185 | r=0.023, n=185 | r=0.21†, n=185 |
| ApoA1 at age 17–19 | r=−0.084, n=195 | r=− 0.0085, n = 195 | r=0.18,* n=198 |
| ApoB/ApoA1 at age 14 | r=0.028, n=185 | r=−0.064, n=185 | r=−0.24†, n = 185 |
| ApoB/ApoA1 at age 17–19 | r=0.11, n=195 | r=−0.054, n=195 | r=−0.30§, n=195 |
No significant differences between races in free testosterone, DHEAS or SHBG.
p < .05.
p < .01.
p < .0001.
Using Mixed Model analyses for repeated measures from age 14 to 19, BMI and TG were significant independent positive predictors of ApoB, Table 5. Black race, TG, and % calories from protein were positive predictors of ApoA1, while metabolic syndrome category and waist circumference were negative predictors, Table 5. For the ratio of ApoB to ApoA1, BMI, TG, pediatric metabolic syndrome, and menstrual delay ≥42 days were positive predictors, while black race was a negative predictor, Table 5.
Table 5.
Mixed model for repeated measures analysis of ApoB, ApoA1 and ApoB/ApoA1 in 670 girls during ages 14 to 19.
| Dependent Variable | Significant explanatory variable | Parameter estimate, 95% CI | p |
|---|---|---|---|
| ApoB | intercept | 50.56 [46.43, 54.70] | <.0001 |
| BMI (kg/m2) | 0.40 [0.24, 0.57] | <.0001 | |
| TG (mg/dL) | 0.13 [0.11, 0.15] | <.0001 | |
| ApoA1 | intercept | 143.86 [135.82, 151.90] | <.0001 |
| Black race | 5.66 [3.32, 8.00] | <.0001 | |
| Met S category (0, 1,2) | −9.03 [−12.81, −5.24] | <.0001 | |
| Waist circumference (cm) | −0.29 [−0.39, −0.19] | <.0001 | |
| TG (mg/dL) | 0.037 [0.013, 0.061] | .003 | |
| % calorie from protein | 0.40 [0.10, 0.70] | .008 | |
| ApoB/ApoA1 | intercept | 0.35 [ 0.32, 0.39] | <.0001 |
| Black race | −0.043 [ −0.063, −0.023] | <.0001 | |
| BMI (kg/m2) | 0.0057 [0.0041, 0.0072] | <.0001 | |
| TG (mg/dL) | 0.00080 [0.00063, 0.00098] | <.0001 | |
| Pediatric Met S (Yes as 1, no as 0) | 0.097 [0.049, 0.148] | <.0001 | |
| menstrual cycles ≥42 days (Yes as 1, no as 0) | 0.041 [0.013, 0.015] | .002 |
Stepwise regression was used to select significant explanatory variables from race, age, BMI, waist circumference, TG, annual report of menstrual cycles ≥42 days, total calorie intake, % calorie from protein, from fat, physical activity during school day, physical activity during a summer day (all at the same years), pediatric Met S, Met S category (neither pediatric MetS nor adult MetS as 0, either one as 1, both as 2), and total number of annual reports of menses delay (1–6). Multiple (n = 10) imputations for 1269 observations which had ApoB. Then for each imputation, mixed model for repeated measures analysis was constructed including only significant explanatory variables as fixed effect, and subjects as random effect, with AR(1) variance structure within subjects. Finally, Procedure MIanalyze combined all 10 models from 10 imputations and estimated parameters.
4. Discussion
Focusing on pediatric–adolescent determinants of ApoA1, ApoB, and the ApoB/ApoA1 ratio should facilitate primary approaches to prevention of coronary heart disease (CHD), given the strong, independent association of the ApoB/ApoA1 ratio to CHD [2–5,7,9]. In the current study, there were a number of novel findings relative to ApoB/ApoA1 in childhood and adolescence, which could be relevant to adult cardiovascular risk.
The first novel finding in our study was that menstrual cyclicity ≥42 days, associated with hyperandrogenism [36], ascertained yearly in post-menarchal girls from ages 14 through 19, was independently associated with increasing ApoB/ApoA1 ratios. In our study, 90% of girls were post-menarchal by age 14, the same as reported in the third NHANES study [37] where 90% of US girls were menstruating by 13.75 years. Other studies have shown that almost all girls are post-menarchal at age 14 [15, 18, 19], including 98% of whites and 97% of blacks [19]. In the current study, to provide the most inclusive assessment of annual reports of delayed menstrual cyclicity, we assessed 6 annual reports from ages 14 to 19. There was no association (p = 0.96) between age at menarche and the number of annual reports of menstrual cycles ≥42 days from ages 14 to 19. In our current and recent [21, 22] studies of the relationships of delayed cyclicity to CVD risk, metabolic syndrome, obesity, and polycystic ovary syndrome (PCOS), annual reports of menstrual cycles ≥42 days from ages 14 to 19 were used to identify girls with unequivocal menstrual delay. The ≥42 day cutpoint for menstrual delay was based on the reports of Van Hooff et al [23,24] and Chiazze et al [18], and, in the current analysis sample, was found in 8% of reports of menstrual cycle length from age 14 to 19. Van Hooff et al [23], whose ≥42-day indicator of oligomenorrhea we used in the current study, reported oligomenorrhea in 24% of 15 year old white Dutch schoolgirls. Van Hooff et al [23, 24] reported that “…our oligomenorrheic group will be a mixture of girls in whom this menstrual cycle pattern is a stage in their maturation to a regular menstrual cycle pattern and girls who have or will develop PCOS, characterized by oligo- or anovulation with high LH or androgen concentrations.”
In our current study, in girls with ≥3 menstrual cycles ≥42 days, the first of serial menstrual cycle delays started at ages 14, 15, and 16, a finding which should alert physicians to assess causes of oligomenorrhea early during adolescence. Previous longitudinal studies on adolescent oligomenorrhea or hyperandrogenemia have shown that adolescents maintain menstrual length characteristics in adulthood [38, 39]. Two thirds of adolescents whose oligomenorrhea persisted for 2 or more years still have oligomenorrhea 10 years later [39, 40]. Avvad et al [41] reported that menstrual irregularity within the first postmenarchal years can be an early clinical sign of PCOS.
A limitation of the current study is that the annual report of delayed menses does not fully disclose what is going on during the rest of the year (i.e., oligomenorrhea, amenorrhea, a single episode, etc). However, by obtaining annual reports from age 14 through 19, a pattern of menses delays over a 6 year period should provide a more reliable estimate of menses delay.
The second novel observation of the current study was the positive correlation of SHBG in black girls at age 14 to ApoA1 and its negative correlation with ApoB and the ApoB/ApoA1 ratio. In adult women, there is an inverse association of SHBG with coronary [42] and abdominal aortic calcification [43].
Low SHBG is associated with hyperandrogenism and is a characteristic finding in PCOS [13]. We speculate that age 14 low SHBG (hyperandrogenism) predicts later higher ApoB/ ApoA1 ratios in young adulthood, since adolescent hyperandrogenism may persist into adulthood [23,24]. Moreover, at age 19, the ApoB/ApoA1 ratio was higher in girls with top quintile insulin levels, congruent with higher ApoB/ApoA1 ratios in black girls with annual reports of menstrual cycles ≥42 days, since hyperinsulinemia, low SHBG, and oligomenorrhea commonly co-aggregate [13,36,44,45], particularly in PCOS [45].
Given the high prevalence of PCOS [46], our novel finding of reduced adolescent menstrual cyclicity, low SHBG, and hyperinsulinemia with an increase in the atherogenic ApoB/ ApoA1 ratio has implications for understanding the cardio-metabolic issues and increased cardiovascular disease in adulthood [42,43,47,48] in women with menstrual irregularity and PCOS. Our findings of a pro-atherogenic association of low SHBG and menstrual delay in adolescence with increasing ApoB/ApoA1 foretell outcomes in adult women, where women with a history of irregular cycles have increased risk of coronary heart disease (CHD) and type 2 diabetes mellitus compared to women with regular cycles (defined as 27 to 29 or 26 to 31days) [47–49]. Antecedent history of irregular menses and elevated androgens is associated with high risk for worsening cardiovascular event-free survival [47]. Age-adjusted risk for CHD mortality increases in adult women with irregular menstrual cycles [48].
Adolescent boys and girls with metabolic syndrome have lower SHBG levels than healthy controls [50]. Assessment of menstrual history and appropriate laboratory work-up may reveal the presence of PCOS in obese at-risk adolescent girls with a family history of the metabolic syndrome [51]. There are, however, no uniformly agreed upon standard cutpoints used in the diagnosis of pediatric–adolescent metabolic syndrome [52]. Ford et al [52] found that there were 40 different definitions of metabolic syndrome used, and the concept of a metabolic syndrome continues to be controversial whether used for adult or pediatric populations.
Our findings in black girls parallel those in male adolescents where obese boys with a high free androgen index had higher ApoB/ApoA1 ratios than those with a low free androgen index [53].
The third novel finding in our study was that from ages 12 to 19, by virtue of lower ApoB, higher ApoA1, lower ApoB/ApoA1, and lower TG, black girls had amore favorable apolipoprotein– TG risk factor profile, which, compared to white girls, should be less associated with adult atherosclerosis [10]. To the extent that higher ApoB/ApoA1 ratios are associated with increased risk for atherosclerosis by virtue of a relatively higher level of atherogenic apolipoprotein (ApoB) than anti-atherogenic apolipoprotein (ApoA1), stable higher ratios over time in white girls would be associated with higher risk for atherosclerosis. On the other hand, the ApoB/ApoA1 ratio in black girls was lower, and fell over time in a concave parabola (“U” shape).
Black children have lower LDL cholesterol and TG and higher HDL cholesterol [54,55], larger LDL particles, and favorable lipoprotein subclass concentrations [56,57], all associated with relatively lower CVD risk. Since black–white differences in the ApoB/ApoA1 ratio, ApoB, and ApoA1 track during childhood and from adolescence to young adulthood [58–60], they should protect against CVD in adult black women. Within this frame of reference, Lee et al have reported that the overall rate for fatal and nonfatal definite myocardial infarction was lower in blacks than in whites in the Community Cardiovascular Surveillance Program [61]. However, in the NHANES I epidemiologic follow-up study, age-adjusted risk for CHD was higher in African–American women ages 25 to 54 years than in white women, a difference which could be explained by higher BMI and higher blood pressure [62] in African–American women.
In mixed model analysis with repeated measures, black girls had higher ApoA1 during ages 14–19, congruent with findings in the Bogalusa study [10]. Black race, percent calories from protein, and TG were positively associated with ApoA1. Metabolic syndrome and waist circumference were inversely associated with ApoA1. Predictors of the ApoB/ApoA1 ratio were BMI, TG, metabolic syndrome, menstrual delay (all positive) and black race (negative). Hence black girls should be at lower CVD risk with respect to black–white differences in ApoB, ApoA1, and the ApoB/ApoA1 ratio. The metabolic syndrome has previously been associated with the ApoB/ ApoA1 ratio [9]. We have shown previously that metabolic syndrome in childhood predicts adult cardiovascular disease and type 2 diabetes mellitus 25 years later [63,64]. In the study by Lee et al [53], pediatric metabolic syndrome was significantly positively associated with the ApoB/ApoA1 ratio, congruent with our current finding. In obese Indian children, the ApoB/ApoA1 ratio was higher in children with the metabolic syndrome compared to those without metabolic syndrome [9]. In obese children, physical training reduced the ApoB/ApoA1 ratio by 43% (p < .01) [65]. The ApoB/ApoA1 ratio has been shown to be strongly associated with metabolic syndrome and its components in an urban Chinese population [66].
The importance of the atherogenic ApoB/ApoA1 ratio lies in its predictive capability for development of cardiovascular disease. In the Bogalusa study [10], Srinivasan reported that low values for ApoA1, the ApoA1 to ApoB ratio, and the LDL cholesterol/ApoB ratio in children were strongly related to parental incidence of myocardial infarction. The ApoB/ApoA1 ratio has been shown to be a significant independent predictor of insulin resistance in US non-diabetic adults [67]. In a 26.8-year follow-up of a community-based sample of 1825 men age 50 at baseline, the ApoB/ApoA1 ratio and the metabolic syndrome independently predicted risk for myocardial infarction [2]. In prospective studies of 7594 US adults, mean age 46 at entry from the NHANES III survey, ApoB and the ApoB/ ApoA1 ratio were significantly associated with CHD death after adjusting for other cardiovascular risk factors [68].
Although potential racial admixture of girls in the sampling frames was considered, assigning race by determination of polymorphic markers known to associate with white and black subgroups [69] was deemed too expensive to be used and also would result in probabilistic assignments. Consequently, the requirement of racial concordance between the girl and parents was used instead. We do not believe that the self-declared racial background systematically affected the results.
In the current study of adolescent girls, the atherogenic ApoB/ApoA1 ratio from ages 14 to 19 was inversely associated with black race, and positively associated with hyperandrogenism, menstrual cyclicity ≥42 days, BMI, TG, and the metabolic syndrome. Future studies are needed to determine how ApoB, ApoA1, or the ApoB/ApoA1 ratio could predict the development of the metabolic syndrome. Moreover, studies are needed to determine whether correction of ApoB levels or the ApoB/ApoA1 ratio offer more in terms of CHD risk reduction when compared to the classical LDLC or HDLC measurements.
Acknowledgments
Linda Levin PhD provided statistical consultation.
Funding: This research was supported in part by NIH HL55025, 48941, HL52911 and HL66430 (Drs Morrison and Daniels), and by the Lipoprotein Research Fund of the Jewish Hospital of Cincinnati (Dr Glueck).
Abbreviations
- ApoA1
Apolipoprotein A1
- ApoB
apolipoprotein B
- TG
triglyceride
- SHBG
sex hormone binding globulin
- MetS
metabolic syndrome
- CVD
cardiovascular disease
- CHD
coronary heart disease
- DHEAS
dehydroepiandrosterone sulfate
- VLDLC
very low density lipoprotein cholesterol
- LDLC
low density lipoprotein cholesterol
- HDLC
high density lipoprotein cholesterol
- MI
multiple imputation
- CI
confidence intervals
Footnotes
Author contributions: Author certification: Drs Morrison and Daniels were responsible for study design and collection of data. Drs Morrison, Daniels, Glueck, and Wang participated in writing the manuscript and in data analysis. Dr Horn participated in the data analysis, and revision of statistical methods.
Conflicts of interest: The authors have no conflicts of interest. There are no disclosures.
References
- 1.Glueck CJMJ, Umar M, Goldenberg N, Wang P. Long term metabolic complications of childhood obesity. In: Freemark MC, editor. Childhood obesity. 2010. pp. 253–65. Book Chapter. [Google Scholar]
- 2.Lind L, Vessby B, Sundstrom J. The apolipoprotein B/AI ratio and the metabolic syndrome independently predict risk for myocardial infarction in middle-aged men. Arterioscler Thromb Vasc Biol. 2006;26:406–10. doi: 10.1161/01.ATV.0000197827.12431.d0. [DOI] [PubMed] [Google Scholar]
- 3.McQueen MJ, Hawken S, Wang X, et al. Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): a case–control study. Lancet. 2008;372:224–33. doi: 10.1016/S0140-6736(08)61076-4. [DOI] [PubMed] [Google Scholar]
- 4.Davidson MH. Apolipoprotein measurements: is more widespread use clinically indicated? Clin Cardiol. 2009;32:482–6. doi: 10.1002/clc.20559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Andrikoula M, McDowell IF. The contribution of ApoB and ApoA1 measurements to cardiovascular risk assessment. Diabetes Obes Metab. 2008;10:271–8. doi: 10.1111/j.1463-1326.2007.00714.x. [DOI] [PubMed] [Google Scholar]
- 6.Innerarity TL, Young SG, Poksay KS, et al. Structural relationship of human apolipoprotein B48 to apolipoprotein B100. J Clin Invest. 1987;80:1794–8. doi: 10.1172/JCI113273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Straczek C, Tafflet M, Barberger-Gateau P, et al. Do lipids and apolipoproteins predict coronary heart disease under statin and fibrate therapy in the primary prevention setting in community-dwelling elderly subjects? The 3C Study Atherosclerosis. 2011;214:426–31. doi: 10.1016/j.atherosclerosis.2010.10.040. [DOI] [PubMed] [Google Scholar]
- 8.Lamarche B, Tchernof A, Mauriege P, et al. Fasting insulin and apolipoprotein B levels and low-density lipoprotein particle size as risk factors for ischemic heart disease. JAMA. 1998;279:1955–61. doi: 10.1001/jama.279.24.1955. [DOI] [PubMed] [Google Scholar]
- 9.Savas Erdeve S, Simsek E, Dallar Y, et al. Utility of ApoB/ApoA1 ratio for the prediction of cardiovascular risk in children with metabolic syndrome. Indian J Pediatr. 2010;77:1261–5. doi: 10.1007/s12098-010-0217-8. [DOI] [PubMed] [Google Scholar]
- 10.Srinivasan SR, Berenson GS. Serum apolipoproteins A-I and B as markers of coronary artery disease risk in early life: the Bogalusa Heart Study. Clin Chem. 1995;41:159–64. [PubMed] [Google Scholar]
- 11.Chen W, Srinivasan SR, Bao W, et al. Sibling aggregation of low- and high-density lipoprotein cholesterol and apolipoproteins B and A-I levels in black and white children: the Bogalusa Heart Study. Ethn Dis. 1997;7:241–9. [PubMed] [Google Scholar]
- 12.Srinivasan SR, Bao W, Berenson GS. The amount of cholesterol relative to apolipoprotein B in low-density lipoproteins relates primarily to high-density lipoprotein cholesterol in children: the Bogalusa Heart Study. Metabolism. 1994;43:1042–6. doi: 10.1016/0026-0495(94)90187-2. [DOI] [PubMed] [Google Scholar]
- 13.Glueck CJ, Morrison JA, Daniels S, et al. Sex hormone-binding globulin, oligomenorrhea, polycystic ovary syndrome, and childhood insulin at age 14 years predict metabolic syndrome and class III obesity at age 24 years. J Pediatr. 2011;159:306–13. doi: 10.1016/j.jpeds.2011.01.018. ePub 3/3/2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Obesity and cardiovascular disease risk factors in black and white girls: the NHLBI Growth and Health Study. Am J Public Health. 1992;82:1613–20. doi: 10.2105/ajph.82.12.1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kimm SY, Barton BA, Obarzanek E, et al. Racial divergence in adiposity during adolescence: the NHLBI Growth and Health Study. Pediatrics. 2001;107:E34. doi: 10.1542/peds.107.3.e34. [DOI] [PubMed] [Google Scholar]
- 16.Biro FM, McMahon RP, Striegel-Moore R, et al. Impact of timing of pubertal maturation on growth in black and white female adolescents: the National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr. 2001;138:636–43. doi: 10.1067/mpd.2001.114476. [DOI] [PubMed] [Google Scholar]
- 17.Morrison JA, Glueck CJ, Horn PS, et al. Pre-teen insulin resistance predicts weight gain, impaired fasting glucose, and type 2 diabetes at age 18–19 y: a 10-y prospective study of black and white girls. Am J Clin Nutr. 2008;88:778–88. doi: 10.1093/ajcn/88.3.778. [DOI] [PubMed] [Google Scholar]
- 18.Chiazze L, Jr, Brayer FT, Macisco JJ, Jr, et al. The length and variability of the human menstrual cycle. JAMA. 1968;203:377–80. [PubMed] [Google Scholar]
- 19.Anderson SE, Dallal GE, Must A. Relative weight and race influence average age at menarche: results from two nationally representative surveys of US girls studied 25 years apart. Pediatrics. 2003;111:844–50. doi: 10.1542/peds.111.4.844. [DOI] [PubMed] [Google Scholar]
- 20.Morrison JA, Glueck CJ, Daniels S, et al. Adolescent oligomenorrhea in a biracial schoolgirl cohort: a simple clinical parameter predicting impaired fasting glucose plus type 2 diabetes mellitus, insulin, glucose, insulin resistance, and centripetal obesity from age 19 to 25 years. Metabolism. 2011;60:1285–93. doi: 10.1016/j.metabol.2011.01.012. [DOI] [PubMed] [Google Scholar]
- 21.Glueck CJ, Morrison JA, Daniels S, et al. Sex hormone-binding globulin, oligomenorrhea, polycystic ovary syndrome, and childhood insulin at age 14 years predict metabolic syndrome and class III obesity at age 24 years. J Pediatr. 2011;159:308 e2–13 e2. doi: 10.1016/j.jpeds.2011.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morrison JA, Glueck CJ, Daniels S, et al. Ramifications of adolescent menstrual cycles >/=42 days in young adults. Fertil Steril. 2011;96:236 e1–40 e1. doi: 10.1016/j.fertnstert.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Hooff MH, Voorhorst FJ, Kaptein MB, et al. Insulin, androgen, and gonadotropin concentrations, body mass index, and waist to hip ratio in the first years after menarche in girls with regular menstrual cycles, irregular menstrual cycles, or oligomenorrhea. J Clin Endocrinol Metab. 2000;85:1394–400. doi: 10.1210/jcem.85.4.6543. [DOI] [PubMed] [Google Scholar]
- 24.van Hooff MH, Voorhorst FJ, Kaptein MB, et al. Polycystic ovaries in adolescents and the relationship with menstrual cycle patterns, luteinizing hormone, androgens, and insulin. Fertil Steril. 2000;74:49–58. doi: 10.1016/s0015-0282(00)00584-7. [DOI] [PubMed] [Google Scholar]
- 25.Morrison JA, James FW, Sprecher DL, et al. Sex and race differences in cardiovascular disease risk factor changes in schoolchildren, 1975–1990: the Princeton School Study. Am J Public Health. 1999;89:1708–14. doi: 10.2105/ajph.89.11.1708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kimm SY, Glynn NW, Kriska AM, et al. Longitudinal changes in physical activity in a biracial cohort during adolescence. Med Sci Sports Exerc. 2000;32:1445–54. doi: 10.1097/00005768-200008000-00013. [DOI] [PubMed] [Google Scholar]
- 27.Kimm SY, Glynn NW, Kriska AM, et al. Decline in physical activity in black girls and white girls during adolescence. N Engl J Med. 2002;347:709–15. doi: 10.1056/NEJMoa003277. [DOI] [PubMed] [Google Scholar]
- 28.Kimm SY, Glynn NW, Obarzanek E, et al. Relation between the changes in physical activity and body-mass index during adolescence: a multicentre longitudinal study. Lancet. 2005;366:301–7. doi: 10.1016/S0140-6736(05)66837-7. [DOI] [PubMed] [Google Scholar]
- 29.LabCorp. Testosterone, free, serum (equilibrium ultrafiltration) LabCorp Manual. 2011:1–3. [Google Scholar]
- 30.Vlahos I, MacMahon W, Sgoutas D, et al. An improved ultrafiltration method for determining free testosterone in serum. Clin Chem. 1982;28:2286–91. [PubMed] [Google Scholar]
- 31.Moll GW, Jr, Rosenfield RL. Testosterone binding and free plasma androgen concentrations under physiological conditions: characterization by flow dialysis technique. J Clin Endocrinol Metab. 1979;49:730–6. doi: 10.1210/jcem-49-5-730. [DOI] [PubMed] [Google Scholar]
- 32.Albers JJ, Marcovina SM, Kennedy H. International Federation of Clinical Chemistry standardization project for measurements of apolipoproteins A-I and B. II. Evaluation and selection of candidate reference materials. Clin Chem. 1992;38:658–62. [PubMed] [Google Scholar]
- 33.Morrison JA, Glueck CJ, Umar M, et al. Hyperinsulinemia and metabolic syndrome at mean age of 10 years in black and white schoolgirls and development of impaired fasting glucose and type 2 diabetes mellitus by mean age of 24 years. Metabolism. 2011;60:24–31. doi: 10.1016/j.metabol.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 34.Grundy SM, Brewer HB, Jr, Cleeman JI, et al. Definition of metabolic syndrome: report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433–8. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 35.Morrison JA, Glueck CJ, Horn PS, et al. Childhood predictors of adult type 2 diabetes at 9- and 26-year follow-ups. Arch Pediatr Adolesc Med. 164:53–60. doi: 10.1001/archpediatrics.2009.228. [DOI] [PubMed] [Google Scholar]
- 36.Morrison JA, Glueck CJ, Daniels S, Wang P, Stroop D. Ramifications of adolescent menstrual cycles >=42 days in young adults. Fertility and Sterility. 2011;96:236–40. doi: 10.1016/j.fertnstert.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chumlea WC, Schubert CM, Roche AF, et al. Age at menarche and racial comparisons in US girls. Pediatrics. 2003;111:110–3. doi: 10.1542/peds.111.1.110. [DOI] [PubMed] [Google Scholar]
- 38.Apter D, Vihko R. Endocrine determinants of fertility: serum androgen concentrations during follow-up of adolescents into the third decade of life. J Clin Endocrinol Metab. 1990;71:970–4. doi: 10.1210/jcem-71-4-970. [DOI] [PubMed] [Google Scholar]
- 39.Southam AL, Richart RM. The prognosis for adolescents with menstrual abnormalities. Am J Obstet Gynecol. 1966;94:637–45. doi: 10.1016/0002-9378(66)90398-x. [DOI] [PubMed] [Google Scholar]
- 40.World Health Organization multicenter study on menstrual and ovulatory patterns in adolescent girls. J Adolesc Health. 1986;7:236–44. [PubMed] [Google Scholar]
- 41.Avvad CK, Holeuwerger R, Silva VC, et al. Menstrual irregularity in the first postmenarchal years: an early clinical sign of polycystic ovary syndrome in adolescence. Gynecol Endocrinol. 2001;15:170–7. [PubMed] [Google Scholar]
- 42.Ouyang P, Vaidya D, Dobs A, et al. Sex hormone levels and subclinical atherosclerosis in postmenopausal women: the Multi-Ethnic Study of Atherosclerosis. Atherosclerosis. 2009;204:255–61. doi: 10.1016/j.atherosclerosis.2008.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Michos ED, Vaidya D, Gapstur SM, et al. Sex hormones, sex hormone binding globulin, and abdominal aortic calcification in women and men in the Multi-Ethnic Study of Atherosclerosis (MESA) Atherosclerosis. 2008;200:432–8. doi: 10.1016/j.atherosclerosis.2007.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Morrison JA, Glueck CJ, Umar M, et al. Hyperinsulinemia and metabolic syndrome at mean age of 10 years in black and white schoolgirls and development of impaired fasting glucose and type 2 diabetes mellitus by mean age of 24 years. Metabolism. 2011;60:24–31. doi: 10.1016/j.metabol.2009.12.013. [DOI] [PubMed] [Google Scholar]
- 45.Glueck CJ, Morrison JA, Friedman LA, et al. Obesity, free testosterone, and cardiovascular risk factors in adolescents with polycystic ovary syndrome and regularly cycling adolescents. Metabolism. 2006;55:508–14. doi: 10.1016/j.metabol.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 46.Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81:19–25. doi: 10.1016/j.fertnstert.2003.10.004. [DOI] [PubMed] [Google Scholar]
- 47.Gast GC, Grobbee DE, Smit HA, et al. Menstrual cycle characteristics and risk of coronary heart disease and type 2 diabetes. Fertil Steril. 2010;94:2379–81. doi: 10.1016/j.fertnstert.2010.03.044. [DOI] [PubMed] [Google Scholar]
- 48.Solomon CG, Hu FB, Dunaif A, et al. Menstrual cycle irregularity and risk for future cardiovascular disease. J Clin Endocrinol Metab. 2002;87:2013–7. doi: 10.1210/jcem.87.5.8471. [DOI] [PubMed] [Google Scholar]
- 49.Solomon CG, Hu FB, Dunaif A, et al. Long or highly irregular menstrual cycles as a marker for risk of type 2 diabetes mellitus. JAMA. 2001;286:2421–6. doi: 10.1001/jama.286.19.2421. [DOI] [PubMed] [Google Scholar]
- 50.Agirbasli M, Agaoglu NB, Orak N, et al. Sex hormones and metabolic syndromein children and adolescents. Metabolism. 2009;58:1256–62. doi: 10.1016/j.metabol.2009.03.024. [DOI] [PubMed] [Google Scholar]
- 51.Tfayli H, Arslanian S. Menstrual health and the metabolic syndrome in adolescents. Ann N Y Acad Sci. 2008;1135:85–94. doi: 10.1196/annals.1429.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ford ES, Li C. Defining the metabolic syndrome in children and adolescents: will the real definition please stand up? J Pediatr. 2008;152:160–4. doi: 10.1016/j.jpeds.2007.07.056. [DOI] [PubMed] [Google Scholar]
- 53.Lee YH, Choi SH, Lee KW, et al. Apolipoprotein B/A1 ratio is associated with free androgen index and visceral adiposity and may be an indicator of metabolic syndrome in male children and adolescents. Clin Endocrinol (Oxf) 2011;74:579–86. doi: 10.1111/j.1365-2265.2010.03953.x. [DOI] [PubMed] [Google Scholar]
- 54.Lee JM, Okumura MJ, Davis MM, et al. Prevalence and determinants of insulin resistance among U.S. adolescents: a population-based study. Diabetes Care. 2006;29:2427–32. doi: 10.2337/dc06-0709. [DOI] [PubMed] [Google Scholar]
- 55.Bacha F, Saad R, Gungor N, et al. Obesity, regional fat distribution, and syndrome X in obese black versus white adolescents: race differential in diabetogenic and atherogenic risk factors. J Clin Endocrinol Metab. 2003;88:2534–40. doi: 10.1210/jc.2002-021267. [DOI] [PubMed] [Google Scholar]
- 56.Freedman DS, Bowman BA, Otvos JD, et al. Levels and correlates of LDL and VLDL particle sizes among children: the Bogalusa heart study. Atherosclerosis. 2000;152:441–9. doi: 10.1016/s0021-9150(99)00495-5. [DOI] [PubMed] [Google Scholar]
- 57.Freedman DS, Bowman BA, Srinivasan SR, et al. Distribution and correlates of high-density lipoprotein subclasses among children and adolescents. Metabolism. 2001;50:370–6. doi: 10.1053/meta.2001.21027. [DOI] [PubMed] [Google Scholar]
- 58.Bao W, Srinivasan SR, Berenson GS. Tracking of serum apolipoproteins A-I and B in children and young adults: the Bogalusa Heart Study. J Clin Epidemiol. 1993;46:609–16. doi: 10.1016/0895-4356(93)90033-w. [DOI] [PubMed] [Google Scholar]
- 59.Matsuura T. An epidemiological study on the familial aggregation and the sequential changes of serum lipids and apolipoproteins in school children in a rural area of Awaji Island. Nihon Eiseigaku Zasshi. 1990;44:1083–96. doi: 10.1265/jjh.44.1083. [DOI] [PubMed] [Google Scholar]
- 60.Kurvinen E, Aasvee K, Zordania R, et al. Serum lipid and apolipoprotein profiles in newborns and six-year-old children: the Tallinn Young Family Study. Scand J Clin Lab Invest. 2005;65:541–50. doi: 10.1080/0365510500208324. [DOI] [PubMed] [Google Scholar]
- 61.Lee MH, Borhani NO, Kuller LH. Validation of reported myocardial infarction mortality in blacks and whites. A report from the Community Cardiovascular Surveillance Program. Ann Epidemiol. 1990;1:1–12. doi: 10.1016/1047-2797(90)90014-j. [DOI] [PubMed] [Google Scholar]
- 62.Gillum RF, Mussolino ME, Madans JH. Coronary heart disease incidence and survivalin African-American women and men. The NHANES I Epidemiologic Follow-up Study. Ann Intern Med. 1997;127:111–8. doi: 10.7326/0003-4819-127-2-199707150-00003. [DOI] [PubMed] [Google Scholar]
- 63.Morrison JA, Friedman LA, Gray-McGuire C. Metabolic syndrome in childhood predicts adult cardiovascular disease 25 years later: the Princeton Lipid Research Clinics Follow-up Study. Pediatrics. 2007;120:340–5. doi: 10.1542/peds.2006-1699. [DOI] [PubMed] [Google Scholar]
- 64.Morrison JA, Friedman LA, Wang P, et al. Metabolic syndrome in childhood predicts adult metabolic syndrome and type 2 diabetes mellitus 25 to 30 years later. J Pediatr. 2008;152:201–6. doi: 10.1016/j.jpeds.2007.09.010. [DOI] [PubMed] [Google Scholar]
- 65.Ben Ounis O, Elloumi M, Makni E, et al. Exercise improves the ApoB/ApoA-I ratio, a marker of the metabolic syndrome in obese children. Acta Paediatr. 2010;99:1679–85. doi: 10.1111/j.1651-2227.2010.01920.x. [DOI] [PubMed] [Google Scholar]
- 66.Zhong L, Li Q, Jiang Y, et al. The ApoB/ApoA1 ratio is associated with metabolic syndrome and its components in a Chinese population. Inflammation. 2010;33:353–8. doi: 10.1007/s10753-010-9193-4. [DOI] [PubMed] [Google Scholar]
- 67.Sierra-Johnson J, Romero-Corral A, Somers VK, et al. ApoB/apoA-I ratio: an independent predictor of insulin resistance in US non-diabetic subjects. Eur Heart J. 2007;28:2637–43. doi: 10.1093/eurheartj/ehm360. [DOI] [PubMed] [Google Scholar]
- 68.Sierra-Johnson J, Fisher RM, Romero-Corral A, et al. Concentration of apolipoprotein B is comparable with the apolipoprotein B/apolipoprotein A-I ratio and better than routine clinical lipid measurements in predicting coronary heart disease mortality: findings from a multi-ethnic US population. Eur Heart J. 2009;30:710–7. doi: 10.1093/eurheartj/ehn347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Morrison JA, Gruppo R, Glueck CJ, et al. Population-specific alleles: the polymorphism (K121Q) of the human glycoprotein PC-1 gene is strongly associated with race but not with insulin resistance in black and white children. Metabolism. 2004;53:465–8. doi: 10.1016/j.metabol.2003.10.029. [DOI] [PubMed] [Google Scholar]