Abstract
The recent decline in the number of new patients undergoing dialysis and transplantation in the United States may be linked to a reduction in the incidence of early-start dialysis, defined as the initiation of renal replacement therapy (RRT) at an estimated GFR ≥10 ml/min per 1.73 m2. We examined the most recent data from the U.S. Renal Data System to determine how this trend will affect the future incidence of ESRD in the United States. The percentage of early dialysis starts grew from 19% to 54% of all new starts between 1996 and 2009 but remained stable between 2009 and 2011. Similarly, the incident RRT population increased substantially in all age groups between 1996 and 2005, with the largest increase occurring in patients aged ≥75 years. Early dialysis starts accounted for most of the increase in the incident RRT population in all age groups during this time period, and between 2005 and 2010, the increase slowed dramatically. Although the future incident RRT population will be determined in part by population growth, these results suggest that later dialysis starts and greater use of conservative and palliative care, which may improve quality of life for elderly patients with advanced renal failure, will continue to attenuate the increase observed in previous years.
Since the beginning of the United States Medicare ESRD program in 1973, there has been a rising tide in the number of persons initiating renal replacement (dialysis or transplantation) therapy (RRT). Part of the recent increase was attributed to the trend to early start of dialysis, defined as RRT initiation at a reported Modification of Diet in Renal Disease–estimated GFR (eGFR) ≥10 ml/min per 1.73 m2. Rosansky et al. concluded that most of the growth in the United States dialysis population between 1996 and 2005 arose from this early-start cohort.1 This trend appears to have been based on conventional wisdom unsupported by peer-reviewed publications.2 Several articles, including the IDEAL (Initiation of Dialysis Early and Late) randomized controlled trial and observational studies based on national and international dialysis registries, failed to show a survival benefit for early dialysis initiation.2
Couchoud et al. reported that after adjustment for socioeconomic and medical risk factors, treatment incidence increases as a result of early start.3 We report on the most recent U.S. Renal Data System (USRDS) incident data that show a possible reversal of the early-start trend.4 We consider the secular trend toward palliative nondialytic care in the elderly5–7 and how this trend and a trend toward later dialysis start may affect future incidence of ESRD in the United States.
Reversal of the Early-Start Trend
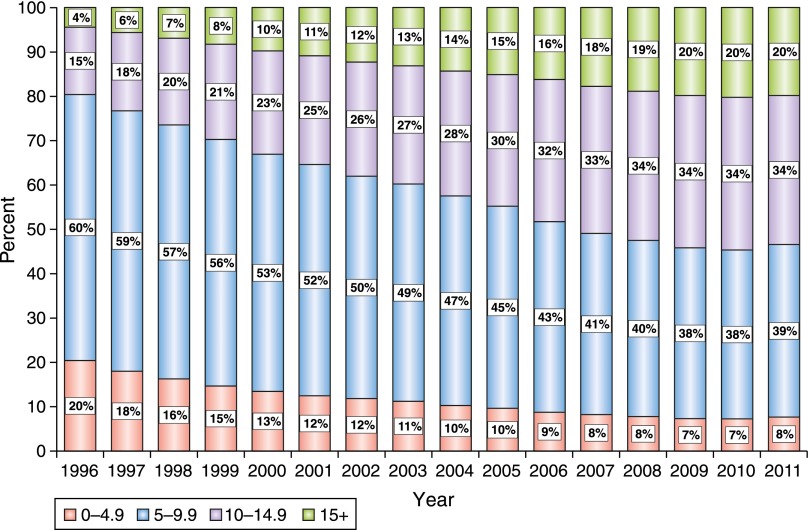
The percentage of the United States incident dialysis population that received an early start increased steadily from 1996 through 2008 (Figure 1). Starting in 2008, there appears to be no further increase in early starts as a percentage of new dialysis starts.
Figure 1.
Incident cases by eGFR category and percentage of total cases among all persons. New RRT starts by four groupings of eGFR (in ml/min per 1.73 m2), calculated using the Modification of Diet in Renal Disease four-variable equation. The groupings are 0–4.9, 5–9.9, 10–14.9, and >15. Early start, defined by a pretherapy eGFR >10 ml/min per 1.73 m2, increased from 19% to 54% of the new starts between 1996 and 2009 and remained stable between 2009 and 2011. Patients initiating therapy at an eGFR >15 ml/min per 1.73 m2 increased by approximately 1% per year from 1996 to 2009. ADR, annual data report; SAF, standard analysis files.
RRT incidence, based on the USRDS quarterly data (updated through September 2012), shows that the 2011 incident count (99% complete) is about 114,000, 2.4% lower than the nearly 117,000 new starts reported in 2010.4 Treatment incidence counts for persons age ≥65 years in 2012 were 4% lower than in 2011. Furthermore, the mean serum creatinine among incident cases from the first quarter of 2010 through the first quarter of 2012 gradually increased from 6.1 mg/dl to 6.3 mg/dl, suggesting a slight reversal of the early-start trend.
Latest Canadian Registry Treatment Incidence and Dialysis Withdrawal Data
The 2013 Canadian Organ Replacement Registry Report (CORR) shows a similar recent decline in treatment incidence. Incident rates per million population for 2009, 2010, and 2011 for patients age 65–74 years were 571, 553, and 517, respectively.8 For patients age >75, the rates for these years were 742, 725, and 668. From the 2001–2009 CORR data, Ellwood et al. found a doubling of the incident dialysis population that withdrew from dialysis, with a 20% withdrawal rate for 2009 new starts.9 Early start of dialysis was a factor associated with discontinuation of dialysis.
United States Age- and Population Growth–Adjusted RRT Incidence Rates and Early Start
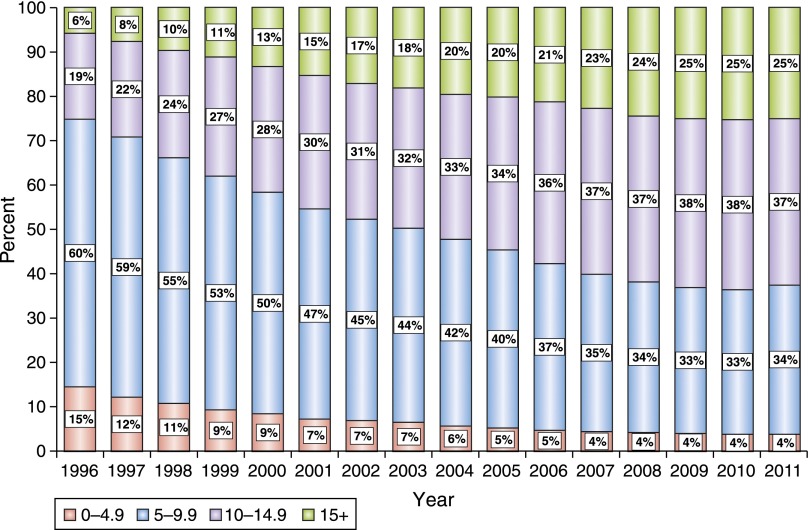
Figures 1 and 2 show that between 1996 and 2009, early starts increased from 19% to 54% for all patients and new starts increased from 25% to 63% for those age ≥75 years. By 2009, very early starts (predialysis eGFR >15 ml/min per 1.73 m2) accounted for 20% of the overall incident RRT population and 25% of new starts in patients age ≥75 years. Early starts did not increase in 2009, 2010, and 2011, either in total or for the ≥75 age group (Figures 1 and 2).
Figure 2.
Incident cases by eGFR category and percentage of total cases among patients age >75 years. This figure shows the same information as Figure 1 but for patients who initiated RRT at age >75 years. An even greater increase in early start of RRT is seen in this population: from 25% to 63% of new starts between 1996 and 2009. Patients initiating therapy at an eGFR >15 ml/min per 1.73 m2 increased from 6% to 25% of these new starts from 1996 to 2009. ADR, annual data report; SAF, standard analysis files.
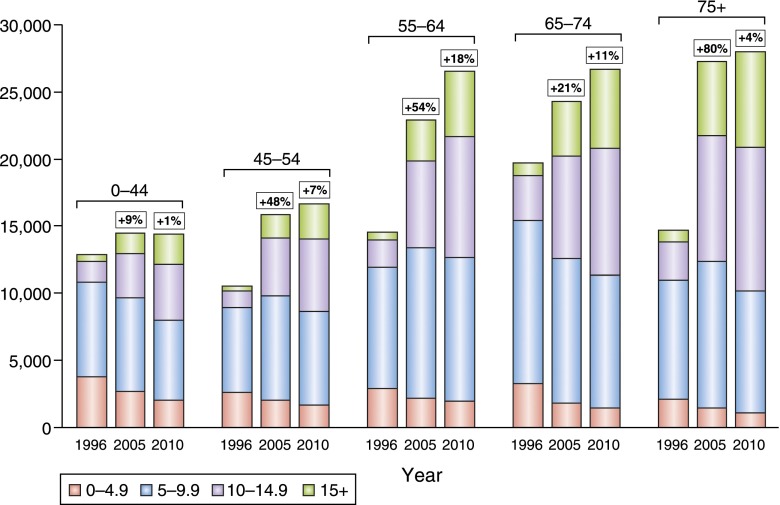
Growth of the incident RRT population by age group and estimated eGFR for 1996, 2005, and 2010 (Figure 3) shows a 9% increase for the population aged <45 years between 1996 and 2005 and a 1% increase from 2005 to 2010. Persons ≥75 years show an 80% increase from 1996 to 2005 but only a 4% increase from 2005 to 2010. These trends in treatment incidence were accompanied by a decrease in persons who initiated RRT at an eGFR <10 ml/min per 1.73 m2 (Figure 3). This same pattern of relatively large increases in incidence related to early start in 1996–2005 and much smaller increases in 2005–2010 was seen in all age groups.
Figure 3.
Incidence counts by eGFR in 1996, 2005, and 2010 by age at time of ESRD. The eGFR groupings are the same as those in Figures 1 and 2, and by age groupings are 0–44, 45–54, 55–64, 65–74, and >75 years. Most of the incident count growth occurred in the 1996–2005 interval, with a much smaller growth in 2005–2010. The largest relative growth occurred in patients >75 years of age, with an 80% increase in new treatment counts between 1996 and 2005. Most of the growth in incident counts is accounted for by the early-start (dialysis initiation at eGFR >10 ml/min per 1.73 m2) subgroups. Even after adjustment for population increase, which explains part of the incident count growth, the new starts among patients >75 years increased by 52% between 1996 and 2005.
Much of the increase in RRT incidence shown in Figure 3 is due to population growth. The United States population grew by 17% from 1996 to 2010 (265 million and 309 million, respectively). Nevertheless, even after adjustment for population growth (not shown), RRT incidence for the ≥75 age groups increased 52% because of early starts.
The implications for delaying dialysis until a lower eGFR is attained vary by age. For example, younger cohorts are much more likely to survive to an eGFR of <10 ml/min per 1.73 m2 than are patients age ≥75 years. The expectation is that, in contrast to younger cohorts, this older age group will probably show a decline in RRT incidence as a result of a trend toward later dialysis starts. Not only is the extent of competing mortality higher in patients age ≥75 years than in younger cohorts, but also these elderly patients may have a slower rate of renal function loss from an eGFR of 15 to <10 ml/min per 1.73 m2.7,10 In a prospective follow-up of a cohort with a mean age of 82 years and a mean eGFR of 14 ml/min per 1.73 m2, Moranne et al. found that 43% of these patients could postpone dialysis initiation because of stable renal function.11
Future New Starts for Patients Age ≥75 Years
Many factors will affect future new starts in elderly patients. The United States population >75 years is expected to double by 2030.12 In addition, increasing rates of diabetes may contribute to new patients starting RRT.13 Reducing early starts will attenuate, but probably not offset, these demographic and diagnostic trends.
A trend toward a later start coupled with population growth predictions and a trend toward palliative and conservative management will affect future dialysis patient numbers. This is foreshadowed by several events. First, nephrology publications on palliative care and geriatric dialysis have recently increased. Second, in December 2013, a Kidney Disease Improving Global Outcomes (KDIGO) conference on controversies in palliative care in nephrology will convene. This meeting may well produce palliative care guidelines over the next few years. A third factor to consider is the statement issued by the American Society of Nephrology that states, “Limited observational data suggest that survival may not differ substantially for older adults with a high burden of comorbidity who initiate chronic dialysis versus those managed conservatively.”14 Finally, the most recent KDIGO 2013 recommendations for RRT initiation suggest that dialysis be initiated when uremia-related symptoms occur in a GFR range of 5–10 ml/min per 1.73 m2.15 These factors may contribute to a further reversal of the early-start trend for all age groups and even more so for the incident RRT population age ≥75 years. Some of these elderly patients may have falsely high eGFR as a result of low muscle mass with attendant low creatinine production for their age.2 This sarcopenia is associated with higher comorbidity and poor quality of life. Thus, waiting to initiate dialysis until the eGFR is <10 ml/min per 1.73 m2, even if falsely high, may still be an appropriate course of action.
KDIGO 2013 also strongly advocates the development of a comprehensive conservative management program.13 Conservatively managed patients may not have a survival advantage over elderly patients who consent to a dialysis therapy approach. Nevertheless, evidence suggests that these conservatively managed patients may have a better quality of life with fewer remaining life-years in the hospital or involved with dialysis treatment. A nondialytic approach may be associated with a better preservation of functional status and residual renal function.5,7 Most of the elderly dialysis population dies in acute care facilities.6 If these patients are educated about a potential for a poor life quality on dialysis and the option for an intensive conservative care management program with more quality time at home, many may choose conservative management.5,7
One problem regarding conservative nondialytic management is the lack of adequate funding in the United States for “dialysis” medications and close follow-up.6 A second problem is the lack of adequate training in palliative care for nephrology trainees.6 One could envision funding options that would cover all of the medical needs of these conservatively managed patients, thus creating a financial incentive to appropriately balance the use of conservative versus dialytic therapy.
Conclusions
The rising tide of early dialysis initiation may have ended, as evidenced by the recent decrease in RRT incidence in the over-65 populations in the United States and Canada, coupled with a declining mean starting eGFR for new dialysis starts in the United States. These trends may be reinforced by the secular changes that emphasize geriatric and palliative care, as well as recommendations by KDIGO and the American Society of Nephrology concerning later dialysis starts and more extensive use of conservative care, especially in elderly patients with advanced CKD and high comorbidity. The competing factors of growth of the elderly United States and Canadian population that will provide a larger base for dialysis starts versus a trend for later start of dialysis and greater acceptance of conservative care for elderly patients with advanced CKD will have a large impact on the future United States and Canadian RRT population. For patients of all ages with a 6- to 12-month life expectancy, adequately funded maximum conservative management may become a preferred clinical pathway for many patients and nephrologists.
Disclosures
None.
Acknowledgments
We are grateful to Paul Eggers, Director of Kidney and Urology Epidemiology, National Institute of Diabetes and Digestive and Kidney Diseases, for the updated USRDS data and help with data interpretation.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
References
- 1.Rosansky SJ, Clark WF, Eggers P, Glassock RJ: Initiation of dialysis at higher GFRs: Is the apparent rising tide of early dialysis harmful or helpful? Kidney Int 76: 257–261, 2009 [DOI] [PubMed] [Google Scholar]
- 2.Rosansky S, Glassock RJ, Clark WF: Early start of dialysis: A critical review. Clin J Am Soc Nephrol 6: 1222–1228, 2011 [DOI] [PubMed] [Google Scholar]
- 3.Couchoud C, Guihenneuc C, Bayer F, Stengel B, REIN Registry : The timing of dialysis initiation affects the incidence of renal replacement therapy. Nephrol Dial Transplant 25: 1576–1578, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Renal Data System: ESRD Quarterly Update. National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2012. Available at: http://www.usrds.org/qtr/default.aspx Accessed April 4, 2013
- 5.Carson R: Deny dialysis or “D-NI” dialysis? The case for “do not initiate; do not ignore” orders. Clin J Am Soc Nephrol 7: 1924–1926, 2012 [DOI] [PubMed] [Google Scholar]
- 6.Davison SN: The ethics of end-of-life care for patients with ESRD. Clin J Am Soc Nephrol 7: 2049–2057, 2012 [DOI] [PubMed] [Google Scholar]
- 7.Schmidt RJ: Informing our elders about dialysis: Is an age-attuned approach warranted? Clin J Am Soc Nephrol 7: 185–191, 2012 [DOI] [PubMed] [Google Scholar]
- 8.Canadian Institute for Health Information: Canadian Organ Replacement Register Annual Report, Ottawa, ON, 2012
- 9.Ellwood AD, Jassal SV, Suri RS, Clark WF, Na Y, Moist LM: Early dialysis initiation and rates and timing of withdrawal from dialysis in Canada. Clin J Am Soc Nephrol 8: 265–270, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosansky SJ: Renal function trajectory is more important than chronic kidney disease stage for managing patients with chronic kidney disease. Am J Nephrol 36: 1–10, 2012 [DOI] [PubMed] [Google Scholar]
- 11.Moranne O, Couchoud C, Vigneau C, PSPA Study Investigators : Characteristics and treatment course of patients older than 75 years, reaching end-stage renal failure in France. The PSPA study. J Gerontol A Biol Sci Med Sci 67: 1394–1399, 2012 [DOI] [PubMed] [Google Scholar]
- 12.U.S. Bureau of the Census. U.S. Census Bureau Projections Show a Slower Growing, Older, More Diverse Nation a Half Century from Now. December 12, 2012 Available at: http://www.census.gov/newsroom/releases/archives/population/cb12-243.html Accessed April 4, 2013
- 13.Eggers PW: Has the incidence of end-stage renal disease in the USA and other countries stabilized? Curr Opin Nephrol Hypertens 20: 241–245, 2011 [DOI] [PubMed] [Google Scholar]
- 14.Williams AW, Dwyer AC, Eddy AA, Fink JC, Jaber BL, Linas SL, Michael B, O’Hare AM, Schaefer HM, Shaffer RN, Trachtman H, Weiner DE, Falk AR, American Society of Nephrology Quality, and Patient Safety Task Force : Critical and honest conversations: The evidence behind the “Choosing Wisely” campaign recommendations by the American Society of Nephrology. Clin J Am Soc Nephrol 7: 1664–1672, 2012 [DOI] [PubMed] [Google Scholar]
- 15.KDIGO 2012 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease Chapter 5: Referral to specialists and models of care. Kidney Int Suppl 3: 112–119, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]