Abstract
Obsessive–compulsive disorder (OCD) influences not only patients but also family members. Although the construct of family accommodation has received attention in OCD literature, no measures of overall family functioning are currently available. The OCD Family Functioning (OFF) Scale was developed to explore the context, extent, and perspectives of functional impairment in families affected by OCD. It is a three-part, self-report measure capturing independent perspectives of patients and relatives. A total of 400 subjects were enrolled between 2008 and 2010 from specialized OCD clinics and OCD research studies. Psychometric properties of this scale were examined including internal consistency, test–retest reliability, convergent and divergent validity, and exploratory factor analyses. Both patient and relative versions of the OFF Scale demonstrated excellent internal consistency (Cronbach’s alpha coefficient = 0.96). The test–retest reliability was also adequate (ICC = 0.80). Factor analyses determined that the OFF Scale comprises a family functioning impairment factor and four OCD symptom factors that were consistent with previously reported OCD symptom dimension studies. The OFF Scale demonstrated excellent convergent validity with the Family Accommodation Scale and the Work and Social Adjustment Scale. Information gathered regarding emotional impact and family role-specific impairment was novel and not captured by other examined scales. The OFF Scale is a reliable and valid instrument for the clinical and research assessment of family functioning in pediatric and adult OCD. This will facilitate the exploration of family functioning impairment as a potential risk factor, as a moderator and as a treatment outcome measure in OCD.
Keywords: obsessive–compulsive disorder, family, accommodation, functioning, scale
Obsessive–compulsive disorder (OCD) is a chronic disabling condition characterized by recurrent obsessions and/or compulsions that cause marked distress and significant impairment in daily functions (American Psychiatric Association, DSM–IV, 1994). OCD frequently onsets in childhood, with bimodal peaks of onset around 10 and 23 years of age (Burke et al., 1990). Family functioning impact of OCD appears to be distinct from that of other psychiatric disorders. Due to its early onset and the specific nature of OCD symptoms, parents often become involved in children’s ritualistic behaviors in ways that do not occur with generalized anxiety or other childhood anxiety disorders (Lenane et al., 1990).
The term “family accommodation” is used to describe relatives’ deleterious attempts to assist their OCD-affected relative by enabling avoidance or assisting ritual behaviors. Family accommodation is highly prevalent among relatives of those with OCD, affecting between 96.9%–100% of OCD children and adults, predominantly on a daily basis (Stewart et al., 2008; Storch et al., 2007). Currently only one measure, the Family Accommodation Scale (Calvocoressi et al., 1995), addresses family accommodation in OCD. This clinician-administered, 13-item scale was designed to assess the nature and frequency of accommodating behaviors by family members’ of those affected by OCD. Family accommodation is associated with important clinical correlates such as OCD severity, functional impairment and treatment outcomes (Merlo, Lehmkuhl, Geffken, & Storch, 2009; Peris et al., 2008; Stewart et al., 2008; Storch et al., 2007; Storch et al., 2010; Van Noppen & Steketee, 2009). However, studies that focus on the broader aspects of family functioning in OCD (Cooper, 1996; Erol et al., 2007; Sukhodolsky et al., 2005) remain sparse. Moreover, no specific measure of family functioning in OCD has been reported.
The development of an assessment tool to specifically address components of family functioning from complementary perspectives of the OCD-affected individual and their relatives is important for several reasons. First, such a measure may provide an efficient means of elucidating the extent and context of family functioning impairment within a busy clinical setting, to contribute valuable insights for guiding clinical intervention. After sufficiently quantifying domains of family functioning impairment, their correlations with OCD treatment outcome may also be explored. Moreover, family functioning impairment may be used as an outcome variable itself to examine treatments such as family therapy. Second, recognition of perceptual discrepancies between patients and their family members is necessary to optimize treatment strategies. The fact that children with anxiety and behavioral disorders have illness-related views that contrast from their family members has been well-documented (Nauta et al., 2004). Discordant parent–child reports at both diagnosis and symptom levels have been observed in OCD (Canavera et al., 2009; Piacentini et al., 2007). In the present study, it is hypothesized that patients and their relatives will also conceptualize family functioning differently, thus leading to distinct response patterns.
This study was undertaken to validate a new measure entitled the OCD Family Functioning (OFF) Scale, for use in both adult and pediatric OCD. Ideally, the symptom-specific domains of impairment in the OFF Scale would correspond to previous studies reporting the underlying construct of OCD symptom dimensions. A recent meta-analysis of OCD symptom dimension studies revealed a robust four-factor structure (Bloch et al., 2008; Stewart et al., 2007). Despite the multitude of analyses in search of associations between OCD symptom dimensions, clinical and biological variables (Stern, 2008), no literature to date addresses potential associations between symptom dimensions and family functioning impairment. The results of psychometric and exploratory factor analyses of the newly developed OFF Scale are presented here.
Materials and Method
Enrollment
OCD-diagnosed subjects between seven and 75 years of age were recruited between 2008 and 2010 from the MGH Pediatric Psychopharmacology Clinic, the McLean/MGH OCD Institute, and an ongoing research study at MGH, the OCD Collaborative Genetics Association Study (OCGAS). Inclusion criteria required a definitive diagnosis of OCD according to Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria (American Psychiatric Association, DSM–IV, 1994), informed consent/assent, and participation of the OCD-affected individual and at least one relative. A total of 150 OCD-affected individuals and 250 of their first or second relatives were enrolled. In addition, a subset of 20% of enrolled subjects was selected for test–retest reliability analyses. For pragmatic reasons related to study implementation, the retest time interval varied by subject. Given concerns that an extended time period would increase the risk of actual changes in family functioning (rather than subjective reports of change), all subjects who completed OFF retest scales after 120 days were excluded from this part of analyses. The mean time interval for remaining subjects was found to be equal to 80.6 days. Subjects enrolled in this study were not routinely exposed to any treatment or intervention between test and retest.
Measurement
The OCD Family Functioning (OFF) Scale is a 42-item self-report questionnaire consisting of three major sub-scales: Part 1—family functioning impairment subscale, Part 2—symptom-specific impairment subscale, and Part 3—family role-specific impairment subscale.
(Please e-mail Dr. S. Evelyn Stewart for a copy of the OFF Scales at sevelynstewart@gmail.com)
Scoring
A total potential score of 100 is calculated by summing the three subscales, the first of which has the highest weighting as it most directly probes family functioning. The score of the Part 1—family functioning impairment subscale (items 1–21) is calculated by summing the scores of each item (subscale total range 0 – 63). For each item, the respondent is asked to report on frequency of OCD-related impairment on a scale between 0 and 3 (0 = never, 1 = monthly, 2 = weekly, 3 = daily). The last two subscales (items 22–37, 38 – 42) are dichotomized for scoring purposes only. “No” is scored with a value of zero, and is considered as a negative response. Other scores (1, 2, or 3) are considered as a positive response. A weighted score of two is given for each positive response in the Part 2—symptom-specific impairment subscale (items 22–37; subscale score range 0–32) and a score of one is given for each positive response in the Part 3—family role-specific impairment subscale (items 38 – 42; subscale total range 0–5). Despite the fact that full Likert scale information for Parts 2 and 3 are not used in calculating the final OFF total score, Likert scales are retained to provide more detailed information for clinicians and future modeling analyses.
Versions
The OFF Scale has distinct versions for OCD-affected individuals and their family members. These two versions are identical with the exception of two items in the social and occupational impact. Both scale versions inquire about family functioning impairment at the time of scale completion and at the time of “worst ever” OCD severity.
Analyses
Demographic
Demographic information including age at assessment and age of OCD onset were compared by gender via t test. All tests were 2-tailed, with a defined alpha level of 0.05. Other descriptive sample data including relative status, and medication and behavioral therapy treatment history were also calculated.
Reliability
The two primary reliability properties examined in our analyses include internal consistency and test–retest reliability (Wolf, 2000). Cronbach’s coefficient alpha (Cronbach, 1951) was used to examine internal consistency. In addition to the overall reliability, alpha coefficients were calculated for different subgroups categorized by age, age of onset, and gender. On the other hand, intraclass correlation coefficient (ICC) was used to compute both test–retest reliability and patient-relative agreement (Leark, Wallace, & Fitzgerald, 2004).
Construct Validity
Principal components analyses were conducted on the first two OFF subscales (items 1–37) as an extraction method to determine the frequency and content of specific factors. Factor analyses were conducted separately on the Part 1—family functioning impairment subscale (items 1–21), on the Part 2—symptom-specific impairment subscale (items 22–37), and on combined Part 1 and Part 2 subscales (items 1–37). The “current OCD” data was utilized for these analyses rather than “worst ever OCD” data to limit potential impacts of recall bias.
To assist with interpretation of results, promax rotation with Kaiser normalization was used when the emergent number of factors was greater than one. Promax rotation is an oblique rotation used as a transformation to simple structure that allows the factors to be intercorrelated (DeVellis, 2003). To determine inclusion in the factors, a score of at least 0.50 on the primary loadings of items after rotation was used as a cutoff. The pattern matrix was used to derive loading values. Another commonly used approach to select the number of factors, known as Kaiser’s criterion (Kaiser, 1960), includes those with an eigenvalue greater than one. Analyses were performed using SPSS 17.0 (Norušis & SPSS Inc., 1991).
Convergent and Discriminant Validity
Using subjects with available data and controlling for age and gender (N = 64), correlation coefficients were computed to demonstrate convergent and discriminant validity of the OFF Scale in comparison with the Yale-Brown Obsessive Compulsive Scale (YBOCS, Goodman et al., 1989), the Work and Social Adjustment (WSA) Scale (Mundt, Marks, Shear, & Greist, 2002), and the Family Accommodation Scale (FAS, Calvocoressi et al., 1995).
Comparison of Patient and Relative Versions
Correlation coefficients were calculated to assess agreement between patients’ versus family members’ reports of family functioning. Separate factor analyses were conducted to assess general validity in both versions.
Results
Demographics
Among OCD-affected individuals and their relatives, 53.3% (80/150) and 46.8% (117/250) were male, respectively. For OCD-affected individuals, the mean age was 27.0 years old (SD 16.5) and the mean age of OCD onset was 12.1-year-old (SD 8.9). With respect to treatment history reports, 84% (N = 126) had medication treatment and 64% (N = 96) had behavioral therapy. Nearly one half of patients (44%; N = 66) reported a positive family history of OCD. Among relatives, the mean age was 50.0 years old (SD 13.2). Most of the relatives were mothers (39.6%, N = 99) and fathers (35.2%, N = 88). Sibling, child, spouse, and “other” relative types accounted for between 4 and 10% of the relative sample. There were no significant gender differences with respect to age (t = 1.09; p = .28) or age of reported OCD onset (t = 0.14; p = .89).
Reliability
Internal Consistency
Internal consistency of respective patient and relative versions, as measured via the Cronbach’s alpha coefficient, was 0.95 and 0.96 for the overall OFF Scale (items 1–42); 0.96 and 0.95 for Part 1—family functioning impairment subscale (items 1–21); 0.92 and 0.90 for Part 2—symptom-specific impairment subscale (items 22–37); and 0.85 and 0.89 for Part 3—family role-specific impairment subscale (items 38 – 42). Subgroup analyses by age, gender, and age of onset groups demonstrated excellent internal consistency estimates ranging between 0.90 and 0.97 (Table 1).
Table 1.
Reliability of Total OFF Scale Score (Items 1–42) Across Gender, Age, and Age of Onset Subgroups
| The OFF scale reliability by subgroup type | Sample size | Cronbach’s alpha coefficient |
|---|---|---|
| Males | 197 | 0.966 |
| Females | 186 | 0.959 |
| Age < 16 y/o | 286 | 0.957 |
| Age > 16 y/o | 104 | 0.959 |
| Age of OCD onset < 16 y/o | 106 | 0.968 |
| Age of OCD onset > 16y/o | 248 | 0.960 |
Test–Retest Reliability
Test–retest reliability was calculated on a subset of 80 participants, which comprised 20% of the total sample. The mean time interval between the first and second measurements was 80.6 days (SD 48.9). According to Kaufman’s criteria (Kaufman & Kaufman, 2002), test–retest reliability (ICC = 0.83) was defined as sufficient for the overall OFF Scale (items 1–42) and for each subscale, as follows: Part 1—family functional impairment subscale (items 1–21; ICC = 0.83), Part 2—symptom-specific impairment subscale (items 22–37; ICC = 0.83), and Part 3—family role-specific impairment subscale (items 38 – 42; ICC = 0.79).
Construct Validity (Factor Analyses)
A total of 400 subjects were analyzed to conduct three factor analyses for each the following: Part 1, Part 2, and combined Parts 1 and 2.
Part 1—family functioning impairment subscale (items 1–21) demonstrated a one-factor structure, since all 21 items loaded well on the first factor (loadings > 0.50). However, three subfactors could be potentially selected if Kaiser’s criteria (eiganvalue > 1.0) were used. Following promax rotation, the three potential “subfactors” were daily life impact, social and occupational impact, and emotional impact (see Table 2).
Table 2.
Promax-Rotated Principal Component Loadings From the Family Functioning Impairment Subscale (Items 1–21)
| Part 1 subscale content/theme | Subscale items | Factors (% variance)
|
||
|---|---|---|---|---|
| 1
|
2
|
3
|
||
| 53.2% | 8.1% | 6.9% | ||
| Daily Life Impact | 1. Morning routines | .423 | .410 | −.037 |
| 2. Lateness to work | .579 | .316 | −.084 | |
| 3. Mealtimes | .617 | .196 | .057 | |
| 4. Social/family function | .697 | .123 | .117 | |
| 5. Planning/scheduling | .649 | .140 | .125 | |
| 6. Going to restaurants | 1.031 | −.222 | −.014 | |
| 7. Shopping/going to the mall | .964 | −.120 | .024 | |
| 8. Trips/vacations | .934 | −.178 | .091 | |
| 9. Keeping appointments | .845 | .092 | −.076 | |
| 10. Bedtime routines | .484 | .260 | .095 | |
| 11. Religious/spiritual worship | .687 | .065 | −.199 | |
| Social and Occupational Impact | 12. Specific relative social life impact | .071 | .680 | .167 |
| 13. Other family members’ social life impact | .130 | .835 | −.084 | |
| 14. Patient’s social life impact | .161 | .503 | .203 | |
| 15. Specific relative work performance | −.121 | .969 | −.055 | |
| 16. Other family members’ work performance | −.086 | 1.014 | −.127 | |
| 17. Patient’s work performance | −.094 | .521 | .411 | |
| Emotional Impact | 18. Stressed/anxious | .003 | −.005 | .872 |
| 19. Frustrated/angry | .086 | −.013 | .767 | |
| 20. Sad | −.108 | .029 | .932 | |
| 21. Guilty | −.021 | −.128 | .858 | |
Note. Factor loadings with an absolute value greater than or equal to 0.50 are shown in bold. Eigenvalue for the fourth component = 0.865.
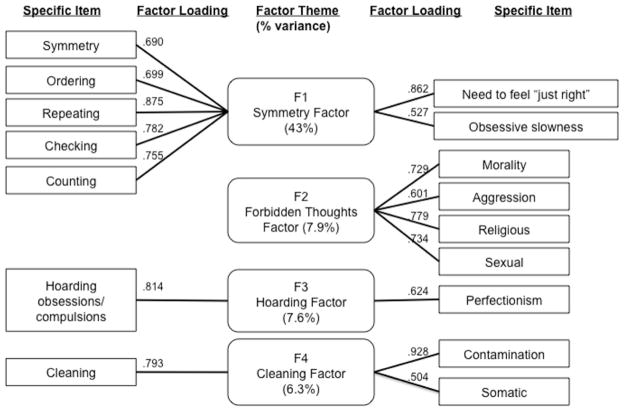
Part 2—symptom-specific impairment subscale (items 22–37) demonstrated a four-factor structure, including: (a) a symmetry/repeating factor, which contains symmetry, ordering, repeating, checking, counting; (b) a forbidden thoughts factor, which contains scrupulosity, aggressive, religious, and sexual obsessions; (c) a cleaning/contamination factor; and (d) a hoarding obsession/compulsion factor (see Figure 1). The resultant four-factor structure accounts for 63.8% of the total variance explained, which is in the upper range compared to previous OCD factor analyses results, 42–66% (Stewart et al., 2007).
Figure 1.
Four-factor structure of the symptom-specific impairment subscale (Items 22–37).
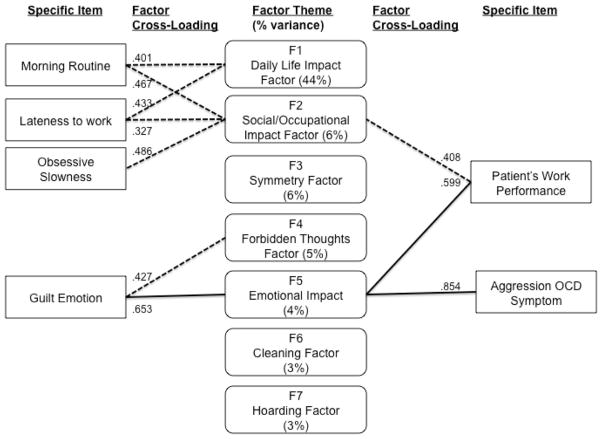
Combined subscales 1 and 2 (items 1–37) demonstrated a seven-factor structure, explaining 70.5% of the total variance (see Figure 2). The seven factors comprised the four previously defined symptom-specific factors and the three family functioning ‘subfactors’. In contrast to results from the separate factor analyses of Parts 1 and 2, several items concurrently loaded (‘cross-loaded’) on more than one factor in the combined factor analyses, suggesting cross-factor correlations. These results are presented in Table 3.
Figure 2.
Item cross-loading of the seven-factor structure for the first two subscales (Items 1–37).
Table 3.
Promax-Rotated Component Loadings Calculated From Principal Component Analyses of the First Two Combined Subscales (Items 1–37)
| Subscale | Subscale items | Factors (% variance)
|
||||||
|---|---|---|---|---|---|---|---|---|
| 1
|
2
|
3
|
4
|
5
|
6
|
7
|
||
| 44% | 6.3% | 5.7% | 4.6% | 3.9% | 3.1% | 3.0% | ||
| Part 1 — Family Functioning Impairment | 1. Morning routines | .401 | .467 | .209 | −.116 | .059 | −.136 | −.148 |
| 2. Lateness to work | .433 | .327 | .090 | −.037 | −.018 | .043 | −.036 | |
| 3. Mealtimes | .782 | .122 | −.035 | .070 | −.123 | .151 | −.127 | |
| 4. Social/family function | .773 | .070 | .064 | −.054 | .062 | .014 | −.050 | |
| 5. Planning/scheduling | .842 | −.010 | .065 | .009 | .146 | −.019 | −.168 | |
| 6. Going to restaurants | .972 | −.151 | −.024 | .111 | −.029 | −.113 | .122 | |
| 7. Shopping/going to the mall | .838 | −.065 | −.099 | .152 | −.040 | −.042 | .270 | |
| 8. Trips/vacations | .810 | −.020 | −.177 | .171 | −.009 | −.075 | .294 | |
| 9. Keeping appointments | .729 | .092 | −.018 | .104 | −.074 | .061 | .123 | |
| 10. Bedtime routines | .515 | .092 | .294 | −.013 | .139 | −.085 | −.076 | |
| 11. Religious/spiritual worship | .455 | −.071 | −.067 | .703 | .031 | .048 | −.086 | |
| 12. Specific relative’s social life impact | .116 | .796 | .008 | −.020 | −.005 | −.052 | .136 | |
| 13. Other family members’ social life impact | .047 | .897 | −.012 | −.025 | −.115 | .038 | .110 | |
| 14. Patient’s social life impact | .166 | .525 | −.076 | −.013 | .348 | −.041 | −.037 | |
| 15. Specific relative’s work performance | −.103 | .934 | −.041 | .060 | .042 | −.032 | .099 | |
| 16. Other family members’ work performance | −.138 | 1.022 | −.011 | .022 | .023 | −.049 | −.010 | |
| 17. Patient’s work performance | .053 | .408 | −.028 | −.048 | .599 | −.001 | −.145 | |
| 18. Stressed/anxious | .147 | −.054 | .084 | −.181 | .316 | .409 | .270 | |
| 19. Frustrated/angry | .068 | −.018 | .231 | −.193 | .117 | .303 | .462 | |
| 20. Sad | .203 | .043 | −.140 | −.199 | .558 | .104 | .309 | |
| 21. Guilty | .090 | −.064 | −.136 | .214 | .668 | .077 | .168 | |
| Part 2 — Symptom-specific Impairment | 22. Cleaning | .297 | −.044 | .149 | −.108 | −.123 | .642 | .074 |
| 23. Contamination | −.174 | −.046 | −.039 | .088 | .002 | .951 | .087 | |
| 24. Hoarding/collecting things | .067 | .074 | .250 | .287 | −.276 | .051 | .326 | |
| 25. Scrupulosity/morality/right and wrong | −.125 | .079 | .206 | .610 | .234 | .020 | .211 | |
| 26. Intrusive unwelcome thoughts | −.162 | −.085 | .259 | .232 | .854 | −.149 | .038 | |
| 27. Perfectionism | .210 | −.036 | .462 | −.018 | −.004 | −.162 | .504 | |
| 28. Symmetry/making things even or balanced | .097 | −.092 | .801 | −.097 | .134 | −.309 | .313 | |
| 29. Ordering | −.041 | .032 | .745 | −.131 | −.053 | −.118 | .418 | |
| 30. Repeating | −.108 | −.113 | .833 | .134 | .206 | .137 | −.028 | |
| 31. Checking | .108 | −.133 | .650 | .087 | .050 | .312 | −.086 | |
| 32. Counting | −.127 | .094 | .674 | .314 | −.043 | .022 | .003 | |
| 33. Religious | .146 | −.003 | .044 | .802 | .142 | −.044 | .038 | |
| 34. Somatic/body or illness worriers | −.024 | .152 | .172 | .082 | .131 | .159 | .374 | |
| 35. Sexual | −.134 | .186 | −.190 | .247 | .269 | .182 | .499 | |
| 36. Need to do things until they feel “just right” | −.044 | .195 | .686 | −.025 | −.154 | .176 | −.023 | |
| 37. Obsessive slowness | .068 | .392 | .246 | .128 | −.251 | .088 | .166 | |
Note. Factor loadings with an absolute value greater than or equal to 0.50 are shown in bold. Eigenvalue for the fourth component = 0.980.
Convergent Validity
After controlling for age and gender, the OFF Scale was highly correlated with the FAS score (coefficient = 0.518, p < .001) and the WSA score (coefficient = 0.501, p < .001), but not with the YBOCS score (coefficient = 0.240, p = .053). The OFF subscales, including the Part 1—family functioning impairment subscale (p < .001) and the Part 2—symptom-specific impairment subscale (p < .001), were correlated with the FAS. At an item level, eight of the FAS items were highly correlated (p < .01) with the OFF scale, including those focusing on modification (Albert et al., 2010).
Discriminant Validity
Discriminant validity of the OFF scale was identified with respect to social, occupational and emotional impacts of family functioning impairment. Social and occupational impacts were not adequately captured by the FAS (p > .05) and emotional impacts were not captured by either the WSA or the FAS (p > .05). The OFF scale did not capture (nor was it designed to capture) some of the family members’ accommodation strategies probed in the initial half of the FAS (i.e., those related to participation). At an item level, several OFF questions probed unique information that was not captured by any of the scales including the Y-BOCS, the FAS, or the WSA. These included daily impact items (planning/scheduling, restaurant dining, shopping/going to malls, trips/vacations, bedtime routines), all emotional impact items, and all family role-specific items.
Comparison of Patient and Relative Versions
The patient-relative agreement for reported family functioning impairment was very low (ICC = 0.50; 95% confidence interval = 0.47–0.57). In contrast, agreement was high for less subjective items of the OFF Scale, such as demographic information (ICC = 0.97, 95% confidence interval = 0.97–0.97).
Discussion
In brief, this study reports on a new scale development and its psychometric properties to measure family functioning impairment in the OCD context. From population health and health economics perspectives, a growing recognition has addressed disease impacts that extend beyond an individual’s symptoms (Kindig & Stoddart, 2009). On the other hand, contemporary scales in existence mainly probe OCD-specific family accommodation (Calvocoressi et al., 1995), and OCD-related functional impacts (e.g., the Child OCD Impairment Scale Piacentini et al., 2007). Both scales have been valuable to OCD clinical and research communities by demonstrating correlations with patients’ disease severity, family organization, and treatment response (Peris et al., 2008). However, neither of the scales fully captures the deleterious functional effects of OCD as they extend to other individuals within the family system.
Therefore, the OFF Scale was developed based on the logic that: (a) general and symptom-specific impairment extends beyond the OCD patients onto their family members and onto the family system; and (b) patients’ versus family members’ perspectives, in combination, provide a unique comprehensive reflection of overall family functioning impairment. Its design will facilitate the exploration of family functioning impairment as a potential risk factor, as a moderator and as a treatment outcome measure in OCD.
Several aspects of this study are worthy of discussion. In assessing the scale’s psychometric properties, new knowledge enriches current literature to better understand OCD impacts at both individual and family levels. This study’s sample size is more than adequate to assess psychometric properties of the OFF scale (N = 400). Our approach of combining data from patients and relatives was adopted in an effort to optimize identification of the underlying construct for OCD-related family functioning impairment. Thus, the Part 1—family functioning impairment subscale demonstrated that all items loaded within a single factor, reflecting that it captured a single focused construct based upon multiple perspectives. Moreover, the four-factor structure of Part 2—symptom-specific impairment subscale was nearly identical to previous literature descriptions (Bloch et al., 2008). This strengthens the evidence that incorporating multiple perspectives within an OCD-affected family adequately captures related constructs.
With respect to reliability indicators, the overall internal consistency of both patient and relative versions of the OFF Scale (items 1–42) is excellent (Cronbach’s alpha coefficient > 0.9) as defined objectively by Cicchetti’s criteria (Cicchetti, 1994). Each of the three subscales demonstrated at least good (Cronbach’s alpha coefficient > 0.8) internal consistency, suggesting that the OFF Scale items are highly inter-correlated. These results also imply that OFF Scale items capture family functioning impairment, as a single construct. These results also provide information regarding the temporal stability of the OFF Scale. The OFF Scale has sufficient test–retest reliability at a mean interval of 80.6 days (ICC = 0.83) according to Kaufman’s criteria (ICC > 0.70).
With respect to validity indicators, construct validity, and convergent and divergent validity were presented. The OFF Scale demonstrated excellent convergent validity with the FAS and the WSA, by capturing behavioral changes within the family system. Divergent validity of the OFF scale from other previously developed scales was also identified. The OFF Scale provided additional information about daily family life impact, emotional impact, and family role-specific impairment that remains uncaptured by other scales.
Construct validity was assessed via factor analyses, whose results were interpreted based upon the following logic. The Part 1—family functioning impairment sub-scale demonstrated a strong one-factor structure in the unrotated principal component analyses (total variance explained = 52.7%, eiganvalue = 11.06). However, the second (emotional impact) and the third (social and occupational impact) factors did not appear to be entirely random noise, as they made sense from a clinical perspective, and as the cross-loadings were greater than 0.35. Indeed, if oblique rotation were conducted, three subfactors would be identified, including those for daily life impact, social and occupational impact, and emotional impact. Yet, rotation is a statistical strategy used to assist in interpretation of the data, and is unnecessary given the single factor solution for family functioning impairment. Current findings provide best solid evidence to support the concept of a one-factor Part 1—family functioning impairment subscale structure, which may have substructures. As described above with respect to combining patient and relative data, factor analyses of Part 2—symptom-specific impairment subscale items identified core OCD symptom dimensions that are consistent with previous factor analytic studies. This consistency implies that the OFF Scale adequately captures the underlying construct of OCD symptoms as these pertain to family functioning.
The factor analyses of the combined first two subscales (items 1–37) identified a seven-factor structure (Figure 2), including a daily life impact factor, a social/occupational impact factor, an emotional impact factor, and the four OCD symptom factors. In exploring cross-loading of items onto separate factors within this seven factor structure, three instances are noteworthy of discussion. First, the social/occupational impact factor is associated with morning routine, lateness to school/work, and obsessive slowness factor items. This result contradicts the notion that home routines have little influence on functioning outside of the home. Obsessive slowness has also been associated with more severe functional impairment in OCD (Veale, 1993). This suggests that cognitive–behavioral therapies focusing on morning routine, lateness to school/work, and obsessive slowness may substantially improve an OCD-affected family’s social and occupational functioning.
The second incidence of cross-loading was identified between OCD-triggered guilt and scrupulosity/religious symptoms (part of the forbidden thoughts factor). To date, most OCD studies related to relatives’ emotions have focused on expressed emotion, such as criticism, hostility, or emotional over-involvement (Hibbs et al., 1991), while limited studies examine guilt among relatives or OCD-affected individuals (Shapiro & Stewart, 2011). Macini et al. have described an association between “not just right experiences” (NJREs), also named “sensory phenomenon”, and guilty feelings (Mancini, Gangemi, Perdighe, & Marini, 2008). Of note, guilt is not associated with sensory phenomena in our study, but rather with morality/religious symptoms. This implies that OCD patients with morality/religious symptom-specific impairment possess unique emotional characteristics such that guilt may serve as a proxy to relieve anxiety. Further research is warranted to explore this hypothesis.
The third aspect of factor analysis results that contributes to current understanding of OCD is the cross-loading that occurred between aggressive obsessions (part of the forbidden thoughts factor) and both the “emotional impact” and “social and occupational impact” factors. This result is reminiscent of the finding by Storch et al., reporting that contamination/cleaning and aggressive/checking symptoms were the only symptom dimensions associated with functional impairment. Moreover, Bloch et al. reported that aggressive obsessions were often included in the cleaning factor, checking factor, or forbidden thoughts factor. The present study finding adds to the current literature and implies that aggressive obsessions (also named “intrusive” thoughts) may affect functioning more than other symptom presentations. This knowledge is clinically useful, as it suggests that aggressive obsessions should not be overlooked in treatment due to their pronounced impact on functioning.
In short, these results of cross-loadings may be used to guide selection of proper interventions according to symptom presentations. OCD treatment strategies should address minimization of disturbed morning routine, lateness to school/work, obsessive slowness, and aggressive obsessions. Moreover, the identified connection between guilt and OCD symptoms including scrupulosity or sexual obsessions may provide clinicians with insight into emotional regulation management in this OCD subtype.
With respect to overall patient-relative agreement, correlation coefficients between these two versions are low (ICC = 0.5). In psychiatric assessment, notoriously poor agreement between parent versus child reports has been problematic, with correlations demonstrated to be as low as 0.25 in some scales of child behavior problems (Canavera et al., 2009; Nauta et al., 2004). In terms of the agreement on OCD symptom-specific impairment, factor analyses of data from each group separately replicated a similar four-factor symptom structure. However, family members of OCD-affected individuals appeared to have difficulties recognizing the extent of internalized symptoms. This is in alignment with the previous reported findings that parent–child agreement increases with observable behavior and decreases with internalizing symptoms (Piacentini et al., 2007). Both analyses in the present study contribute to this area of research by supporting the hypothesis that OCD patients and their relatives have different perspectives of family functioning impairment.
Certain methodological limitations warrant consideration. First, this is an observational study. Subjects were enrolled in the study if they met DSM–IV criteria for OCD and if they were concurrently enrolled in either the OCD Institute or one of selected OCD studies. Subjects with other psychiatric disorders were not excluded given the very high comorbidity rates in this population (Ruscio et al., 2010). The present sample consisted of primarily Caucasian, treatment-seeking young adults or children and our results may not be fully generalizable to a broader community population. However, they are likely to be highly applicable to clinical settings representative of workplaces for the readership of this journal. Second, the final subscale, Part 3—family role-specific impairment, is an information-gathering subsection of the OFF Scale to facilitate clinical understanding of role-specific impairment. In the future, larger sample sizes may allow stratification analyses of family role-specific impairment. This subscale is not included in current factor analyses due to power limitations.
Conclusion
Family functioning is an important and underappreciated construct to consider in OCD assessment and management. The OCD Family Functioning (OFF) Scale represents a reliable and valid instrument for the functional assessment of families affected by OCD. This new instrument aims to provide unique and valuable information on the family context and on diverse familial perspectives, to be used in conjunction with complementary OCD-specific measures. It is expected to provide both clinical and research utility by efficiently measuring family functioning as an outcome and as an outcome mediator. Specifically, the OFF Scale will be available for use in family focused treatment (Barret et al., 2008) trials, to better understand the mechanisms of response for family intervention in the context of OCD.
Acknowledgments
S. Evelyn Stewart, Harvard Medical School and OCD Research Program, University of British Columbia, Vancouver, Canada; Yu-Pei Hu, Abby Lamstein, and Christina Gironda, OCD Institute, Mclean Hospital, Belmont, Massachusetts; Dianne M. Hezel, Rachel Proujansky, Casey Walsh, and Elana Pearl Ben-Joseph, Department of Psychiatry, Massachusetts General Hospital, Boston, Massachusetts; Michael Jenike, Harvard Medical School and OCD Institute, McLean Hospital, Belmont, Massachusetts; Daniel A. Geller and David L. Pauls, Massachussetts General Hospital, Boston, Massachussetts, Harvard Medical School.
The authors would like to acknowledge the invaluable assistance of Lee Baer, PhD, as a statistical consultant, and of Annie Kuan in manuscript preparation. The authors are also grateful for the following funding supporting this work: the American Academy of Child and Adolescent Psychiatry (AACAP) Junior Investigator Award (Stewart); the Anxiety Disorders Association of America (ADAA) Early Investigator Award (Stewart); R01MH79489-4 (Pauls, Geller, Ben-Joseph, Stewart); and the Judah OCD Research Fund (Gironda, Hezel, Hu, Jenike, Stewart).
Dr. Daniel Geller MD receives/d over last three years (to April 2010), Research support: Eli Lilly and Co., BoehringerIngelheim, Otsuka, Pediatric Obsessive Compulsive and Related Disorders fund (philanthropic), Speaker Honoraria: Eli Lilly, Medical Advisory Boards/Consulting: Eli Lilly, Lundbeck, Private Foundations: Wallace Foundation, McIngvale Family Foundation, Rogers Memorial Hospital: Honorarium for Educational Consultant/Guest Lecture, Network for Continuing Medical Education: Neuroscience e journal club lecturer, NIH: National Institute of Mental Health, National Institute of Neurological Disorders and Stroke, American Psychiatric Publishing: Honorarium for textbook
Contributor Information
S. Evelyn Stewart, Harvard Medical School and OCD Research Program, University of British Columbia, Vancouver, Canada.
Yu-Pei Hu, OCD Institute, McLean Hospital, Belmont, Massachusetts.
Dianne M. Hezel, Massachusetts General Hospital, Boston, Massachusetts
Rachel Proujansky, Massachusetts General Hospital, Boston, Massachusetts.
Abby Lamstein, OCD Institute, McLean Hospital, Belmont, Massachusetts.
Casey Walsh, Massachusetts General Hospital, Boston, Massachusetts.
Elana Pearl Ben-Joseph, Massachusetts General Hospital, Boston, Massachusetts.
Christina Gironda, OCD Institute, McLean Hospital, Belmont, Massachusetts.
Michael Jenike, Harvard Medical School and OCD Institute, McLean Hospital, Belmont, Massachusetts.
Daniel A. Geller, Massachusetts General Hospital, Boston, Massachusetts, and Harvard Medical School
David L. Pauls, Massachusetts General Hospital, Boston, Massachusetts, and Harvard Medical School
References
- Albert U, Bogetto F, Maina G, Saracco P, Brunatto C, Mataix-Cols D. Family accommodation in obsessive–compulsive disorder: Relation to symptom dimensions, clinical and family characteristics. Psychiatry Research. 2010;179:204–211. doi: 10.1016/j.psychres.2009.06.008. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Task Force on DSM–IV. Diagnostic and statistical manual of mental disorders: DSM–IV. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Barrett PM, Farrell L, Pina AA, Peris TS, Piacentini J. Evidence-based psychosocial treatments for child and adolescent obsessive-compulsive disorder. Journal of Clinical Child & Adolescent Psychology. 2008;37:131–155. doi: 10.1080/15374410701817956. [DOI] [PubMed] [Google Scholar]
- Bloch MH, Landeros-Weisenberger A, Rosario MC, Pittenger C, Leckman JF. Meta-analysis of the symptom structure of obsessive-compulsive disorder. American Journal of Psychiatry. 2008;165:1532–1542. doi: 10.1176/appi.ajp.2008.08020320. Appi.ajp.2008.08020320[pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke KC, Burke JD, Jr, Regier DA, Rae DS. Age at onset of selected mental disorders in five community populations. Archives of General Psychiatry. 1990;47:511–518. doi: 10.1111/j.1469-7610.1996.tb01457.x. [DOI] [PubMed] [Google Scholar]
- Calvocoressi L, Lewis B, Harris M, Trufan SJ, Goodman WK, McDougle CJ, Price LH. Family accommodation in obsessive-compulsive disorder. American Journal of Psychiatry. 1995;152:441–443. doi: 10.1176/ajp.152.3.441. [DOI] [PubMed] [Google Scholar]
- Canavera KE, Wilkins KC, Pincus DB, Ehrenreich-May JT. Parent-child agreement in the assessment of obsessive-compulsive disorder. Journal of Clinical Child & Adolescent Psychology. 2009;38:909–915. doi: 10.1080/15374410903258975. 916813329[pii] [DOI] [PubMed] [Google Scholar]
- Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychological Assessment. 1994;6:284–290. [Google Scholar]
- Cooper M. Obsessive-compulsive disorder: Effects on family members. American Journal of Orthopsychiatry. 1996;66:296–304. doi: 10.1037/h0080180. [DOI] [PubMed] [Google Scholar]
- Cronbach LJ. Coefficient Alpha and the Internal Structure of Tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- DeVellis RF. Scale development: Theory and applications. 2. Thousand Oaks, CA: Sage; 2003. [Google Scholar]
- Erol A, Yazici F, Toprak G. Family functioning of patients with an eating disorder compared with that of patients with obsessive compulsive disorder. Comprehensive Psychiatry. 2007;48:47–50. doi: 10.1016/j.comppsych.2006.05.004. S0010-440X(06)00075–7[pii] [DOI] [PubMed] [Google Scholar]
- Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Charney DS. The Yale-Brown Obsessive-Compulsive Scale I: Development, use, and reliability. Archives of General Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Hibbs ED, Hamburger SD, Lenane M, Rapoport JL, Kruesi MJP, Keysor CS, Goldstein MJ. Determinants of expressed emotion in families of disturbed and normal children. Journal of Child Psychology and Psychiatry. 1991;32:757–770. doi: 10.1111/j.1469-7610.1991.tb01900.x. [DOI] [PubMed] [Google Scholar]
- Kaiser HF. The application of electronic computers to factor analysis. Educational and Psychological Measurement. 1960;20:141–151. doi: 10.1177/001316446002000116. [DOI] [Google Scholar]
- Kaufman AS, Kaufman NL. Assessment of children: Cognitive applications. Contemporary Psychology-APA Review of Books. (4) 2002;47:394–397. [Google Scholar]
- Kindig D, Stoddart G. What is population health? American Journal of Public Health. 2009;93:380–383. doi: 10.2105/ajph.93.3.380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leark RA, Wallace DR, Fitzgerald R. Test-retest reliability and standard error of measurement for the test of variables of attention (T. O. V. A.) with healthy school-age children. Assessment. 2004;11:285–289. doi: 10.1177/1073191104269186. 11/4/285[pii] [DOI] [PubMed] [Google Scholar]
- Lenane MC, Swedo SE, Leonard H, Pauls DL, Sceery W, Rapoport JL. Psychiatric disorders in first degree relatives of children and adolescents with obsessive compulsive disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 1990;29:407–412. doi: 10.1097/00004583-199005000-00012. S0890-8567(09)65148–0[pii] [DOI] [PubMed] [Google Scholar]
- Mancini F, Gangemi A, Perdighe C, Marini C. Not just right experience: Is it influenced by feelings of guilt? Journal of Behavior Therapy & Experimental Psychiatry. 2008;39:162–176. doi: 10.1016/j.jbtep.2007.02.002. S0005-7916(07)00006–7[pii] [DOI] [PubMed] [Google Scholar]
- Merlo LJ, Lehmkuhl HD, Geffken GR, Storch EA. Decreased family accommodation associated with improved therapy outcome in pediatric obsessive-compulsive disorder. Journal of Consulting and Clinical Psychology. 2009;77:355–360. doi: 10.1037/a0012652. 2009 – 03774-016 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mundt JC, Marks IM, Shear MK, Greist JM. The Work and Social Adjustment Scale: A simple measure of impairment in functioning. British Journal of Psychiatry. 2002;180:461–464. doi: 10.1192/bjp.180.5.461. [DOI] [PubMed] [Google Scholar]
- Nauta MH, Scholing A, Rapee RM, Abbott M, Spence SH, Waters A. A parent-report measure of children’s anxiety: Psychometric properties and comparison with child-report in a clinic and normal sample. Behavior Research and Therapy. 2004;42:813–839. doi: 10.1016/S0005-7967(03)00200-6. [DOI] [PubMed] [Google Scholar]
- Norušis MJ SPSS Inc. The SPSS guide to data analysis for SPSS/PC+ 2. Chicago: SPSS; 1991. [Google Scholar]
- Peris TS, Bergman RL, Langley A, Chang S, McCracken JT, Piacentini J. Correlates of accommodation of pediatric obsessive-compulsive disorder: Parent, child, and family characteristics. Journal of the American Academy of Child & Adolescent Psychiatry. 2008 doi: 10.1097/CHI.0b013e3181825a91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piacentini J, Peris TS, Bergman RL, Chang S, Jaffer M. Functional impairment in childhood OCD: Development and psychometrics properties of the Child Obsessive-Compulsive Impact Scale-Revised (COIS-R) Journal of Clinical Child & Adolescent Psychology. 2007;36:645–53. doi: 10.1080/15374410701662790. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Stein DJ, Chiu WT, Kessler RC. The epidemiology of obsessive-compulsive disorder in the National Comorbidity Survey Replication. Molecular Psychiatry. 2010;15:53–63. doi: 10.1038/mp.2008.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shapiro LJ, Stewart ES. Pathological guilt: A persistent yet overlooked treatment factor in obsessive-compulsive disorder. Annuals of Clinical Psychiatry. 2011;23:63–70. [PubMed] [Google Scholar]
- Stern TA Massachusetts General Hospital. Massachusetts General Hospital comprehensive clinical psychiatry. 1. Philadelphia, PA: Mosby/Elsevier; 2008. [Google Scholar]
- Stewart SE, Beresin C, Haddad S, Egan Stack D, Fama J, Jenike M. Predictors of family accommodation in obsessive-compulsive disorder. Annuals of Clinical Psychiatry. 2008;20:65–70. doi: 10.1080/10401230802017043. 793374409[pii] [DOI] [PubMed] [Google Scholar]
- Stewart SE, Rosario MC, Brown TA, Carter AS, Leckman JF, Sukhodolsky D, Pauls DL. Principal components analysis of obsessive-compulsive disorder symptoms in children and adolescents. Biological Psychiatry. 2007;61:285–291. doi: 10.1016/j.biopsych.2006.08.040. [DOI] [PubMed] [Google Scholar]
- Storch EA, Geffken GR, Merlo LJ, Jacob ML, Murphy TK, Goodman WK, Grabill K. Family accommodation in pediatric obsessive-compulsive disorder. Journal of Clinical Child & Adolescent Psycholology. 2007;36:207–216. doi: 10.1080/15374410701277929. [DOI] [PubMed] [Google Scholar]
- Storch EA, Larson MJ, Muroff J, Caporino N, Geller D, Reid JM, Murphy TK. Predictors of functional impairment in pediatric obsessive-compulsive disorder. Journal of Anxiety Disorder. 2010;24:275–283. doi: 10.1016/j.janxdis.2009.12.004. S0887-6185(09)00239–4[pii] [DOI] [PubMed] [Google Scholar]
- Sukhodolsky DG, do Rosario-Campos MC, Scahill L, Katsovich L, Pauls DL, Peterson BS, Leckman JF. Adaptive, emotional, and family functioning of children with obsessive-compulsive disorder and comorbid attention deficit hyperactivity disorder. American Journal of Psychiatry. 2005;162:1125–1132. doi: 10.1176/appi.ajp.162.6.1125. 162/6/1125[pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Noppen B, Steketee G. Testing a conceptual model of patient and family predictors of obsessive compulsive disorder (OCD) symptoms. Behavior Research & Therapy. 2009;47:18–25. doi: 10.1016/j.brat.2008.10.005. S0005-7967(08)00206–4[pii] [DOI] [PubMed] [Google Scholar]
- Veale D. Classification and treatment of obsessional slowness. British Journal of Psychiatry. 1993;162:198–203. doi: 10.1192/bjp.162.2.198. [DOI] [PubMed] [Google Scholar]
- Wolf S. A compendium of neuropsychological tests: Administration, norms, and commentary. Integrative Physiological and Behavioral Science. 2000;35:70–71. [Google Scholar]