Abstract
Objective
To examine whether insulin requirements and diabetes control differ between adolescents and adults with CFRD.
Methods
All CFRD patients on insulin therapy seen at the University of Minnesota outpatient clinic January 1, 2011-June 1, 2012 were identified. HbA1c levels obtained during this period were averaged for each patient and the most recent outpatient insulin dose obtained. In addition, retrospective chart review was performed to obtain longitudinal data on insulin requirements during the transition from adolescence to adulthood.
Results
Eighteen youth age 14-19y and 137 adults age 20-67y were identified as currently on insulin therapy. The average insulin dose was 0.38 ±0.29 units/kg/day in youth and 0.46±0.30 units/kg/day in adults (p=0.20). In adults, insulin doses were significantly higher in transplant recipients: Tx=0.58±0.29, no Tx=0.43 ± 0.30 (p=0.005). Average HbA1c was 6.9±2.1% in youth and 6.9±1.5% in adults (p=0.35). Current adults with diabetes were not on higher doses of insulin compared to when they were adolescents with diabetes.
Conclusion
Modest insulin requirements suggest the persistence of endogenous insulin secretion in both youth and adults with CFRD. In adolescents, residual endogenous insulin secretion likely compensates for the insulin resistance of puberty, keeping insulin requirements low.
Keywords: CFRD, insulin requirements, HbA1c
INTRODUCTION
Cystic fibrosis related diabetes (CFRD) is the most common co-morbidity in persons with CF (1). The pathophysiology of diabetes in CF is complex and not completely understood, but is believed to be related to multiple factors including fibrotic disruption of the pancreatic architecture, genetic factors, and inflammatory stress (2). The hallmark of CFRD is insulin insufficiency, and insulin is the treatment of choice (3). The prevalence of diabetes in persons with CF is higher than any age-matched group; it is found in about 2% of children less than 10 years of age, 15-20% of youth age 10-20 years, and 40-50% of adult patients (1). In type 1 diabetes (T1D), insulin requirements are greater and metabolic control is worse in adolescents compared to adults with diabetes (4; 5). Few studies have specifically addressed diabetes management in CF youth, and, to our knowledge, age-related insulin requirements have not been reported. The University of Minnesota (UM) instituted annual oral glucose tolerance test (OGTT) screening for CFRD in the early 1990's and has followed a large cohort of CFRD patients since that time, providing the opportunity for both cross-sectional and longitudinal assessment. We examined whether insulin requirements, diabetes management, and diabetes control differ between youth and adults with CFRD.
METHODS
At UM, CFRD is diagnosed by standard criteria including persistent random glucose levels ≥200 mg/dl (11.1 mmol/l) in the presence of symptoms, fasting glucose levels ≥126 mg/dl (7.0 mmol/l), or 2-h OGTT glucose levels ≥200 mg/dl (11.1 mmol/l) (3). Patients with CF who are not known to have diabetes are screened annually by OGTT starting at age 6. Diabetes management includes involvement of an endocrinologist, a diabetes nurse educator and a dietitian. Insulin is standard treatment for all patients diagnosed with diabetes.
All CFRD patients on insulin therapy seen in the outpatient clinic January 1, 2011-June 1, 2012 were identified using the UM CF database. The database included all HbA1c levels obtained during this period; these were averaged for each patient. The electronic medical record was used to determine the most recent outpatient insulin dose and relevant clinical information. All CFRD patients followed at UM gave informed consent permitting their records to be reviewed for research purposes.
To explore longitudinal trends during the transition from adolescence to adulthood, current adult CFRD patients who were 10-20 years of age during the years 2005-2010 and who were on insulin therapy at any time during those years were assessed then and now. Th analysis was repeated using only those young adults who were 10-18 years during this time period. The year 2005 was chosen as the earliest limit because this was when UM began an electronic medical record and because all patients with diabetes have been treated with insulin since then. The adolescent baseline was considered the earliest time point between 2005-2010 when a subject had been on insulin therapy for at least 1 year.
Statistical Analyses
Data were analyzed using SAS version 9.3 (SAS, Cary, NC). Data are presented as mean±standard deviation (SD). Insulin requirements and HbA1c levels were compared between adults and children and transplant vs non-transplant recipients using non-parametic (Wilcoxon rank-sum) tests. Insulin dose by age was compared by two methods: (1) by ANOVA comparing average insulin dose by age decade and (2) by regression analyses in adults and in children with and without transplant.
Using the longitudinal data, insulin doses in adults were compared to insulin doses in those same individuals back when they were adolescents. This comparison was performed using the non-parametric Wilcoxon signed rank sum test.
P-values <0.05 were considered statistically significant.
RESULTS
Subjects
Eighteen youth age <20 y (17±2y, range 14-19, 15% of the UM youth population) and 137 adults (36±10y, range 20-67, 38% of the UM adult population) were identified as currently on insulin therapy. During the study period no child less than 10 years of age had a diagnosis of diabetes. Fifty-nine percent of youth and 54% of adults were female. Twelve percent of youth and 22% of adults had received a lung and/or liver transplant. Diabetes duration was 6.3±2.6y (range 1.2-10.1) in youth and 11.6±6.2y (range 1.2-36.0) in adults. Diabetes with fasting hyperglycemia was present in 72% of youth and 73% of adults; the remaining patients had CFRD without fasting hyperglycemia.
Diabetes Management and Metabolic Control
The majority of patients were on intensive insulin regimens with basal/bolus injections (youth-71%, adults-48%) or insulin pumps (youth-18%, adults-29%). The remainder received meal coverage only or once daily basal insulin.
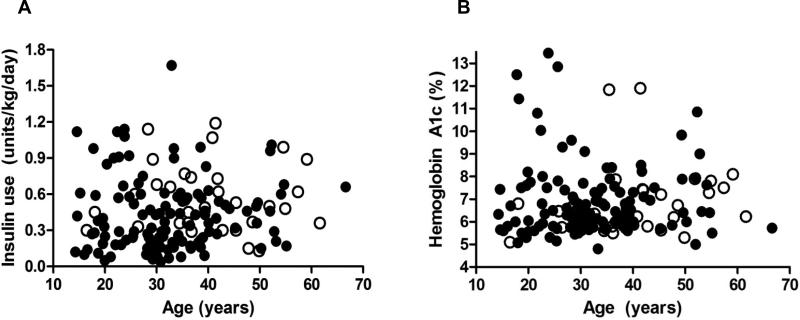
Insulin doses were not different between youth and adults with CFRD (p=0.20), nor did insulin doses differ by decade of age (p=0.29) (Figure 1A). Regression analysis similarly found no significant association between the age of the patient and average daily insulin use. The average insulin dose in youth was 0.38±0.29 units/kg/day (range 0.12-1.12). The average insulin dose in adults was 0.46±0.30 units/kg/day (range 0.05-1.67) (p=0.20). Six percent of both youth (n=1) and adults (n=8) required more than 1 unit/kg/day of insulin, including a 14 year old girl who was also on growth hormone therapy, 2 adults whose BMI was >40 kg/m2, 4 adults with very severe lung disease (2 of whom were listed for transplant), 1 who suffered from lung complications following transplant and required high-dose steroids, and an adult with no obvious explanation for increased insulin needs.
Figure 1.
(A) Insulin use in units/kg/day by patient age and (B) hemoglobin A1c by patient age. Open circles indicate patients with a history of transplant.
There was no significant difference in metabolic control between adolescents and adults with CFRD (Figure 1B). Average HbA1c was 6.9±2.1% (range 5.1-12.5%) in youth and 6.9±1.5% (range 5.2-13.5%) in adults (p=0.35). Three of eighteen youth (17%) and 17/137 adults (12%) had HbA1c levels ≥8.0%. All but two of these were known to struggle with adherence to diabetes therapies as evidenced by failed clinic appointments, insufficient glucose checks by home meter, and/or insufficient insulin boluses recorded on pump downloads. One of the other two patients chose to be hyperglycemic because of an extreme fear of hypoglycemia, while the medical team maintained the other at an HbA1c level just greater than 8.0% because of brittle hypoglycemia unawareness.
There was no difference in insulin dose in children by transplant status: 0.30 and 0.45 units/kg/day in the two patients compared to 0.38±0.31 units/kg/day in children who did not have a transplant history (p=0.62). However, amongst adults, transplant recipients were on significantly more insulin: 0.58±0.29 units/kg/day in transplant recipients compared to 0.43±0.30 units/kg/day in those with no transplant history (p=0.005). Transplantation did not significantly impact HbA1c levels. The 2 children who had received a transplant had HbA1c levels of 5.1% and 6.8% compared to 7.0±2.2% for the 16 children who had not received a transplant, and HbA1c levels averaged 6.9±1.6% in adult patients who had received a transplant compared to 6.8±1.5% in adult patients who had no transplant history (p=0.80).
Longitudinal Assessment of Adolescence Versus Adulthood
Nineteen current adults were identified who were <20y of age and received insulin between 2005-2010. At the current age of 23 years, the insulin dose was 0.45 units/kg/day. When this cohort was, on average, 17 years of age, the average insulin dose was 0.40 units per kg/day (p=0.89). When only the 11 subjects who were <18 years during 2005-2010 were assessed, their average insulin dose as youth was 0.44 units/kg/day compared to 0.50 units/kg/day as adults (p=0.76). Thus, insulin doses were not greater in these subjects when they were adolescents compared to their current young adult doses, over an average of about 6 years.
DISCUSSION
Currently, 155 individuals with CFRD are treated with insulin at UM. Contrary to clinical experience in T1D, insulin requirements are not greater in youth with CFRD compared to adults, nor is metabolic control, as assessed by HbA1c levels, worse in adolescents. Both adolescents and adults with CFRD are on relatively low doses of insulin and there is no decrease in insulin requirements as these individuals transition from adolescence to young adulthood.
In general, daily insulin needs are influenced by several factors including overall health, body weight, level of physical activity, pubertal maturation, and residual beta cell mass and function. Puberty is a time of physiologically increased insulin resistance, requiring a compensatory increase in endogenous insulin secretion (6). In T1D, the requirement for higher exogenous insulin doses during adolescence reflects this physiology. In the modern era, with its focus on good nutrition, the timing of puberty is usually normal in children with CF and, although it has not been directly measured, presumably these patients experience the usual insulin resistance of puberty. Why don't youth with CF require higher insulin doses than adults? The likely explanation is that they produce sufficient endogenous insulin secretion to compensate for pubertal insulin resistance.
Insulin requirements were relatively low in both youth and adults with CF compared to published requirements for subjects with T1D. In T1D, average insulin doses are reported to be 0.66-0.80 units/kg/day in children, 0.74-1.20 units/kg/day in adolescents, and 0.70-0.80 units/kg/day in adults (4; 5; 7). International Society for Pediatric and Adolescent Diabetes (ISPAD) consensus guidelines suggest typical insulin doses of 1-2 units /kg/day during puberty (8). In contrast, both children and adults with CFRD averaged insulin doses <0.5 units/kg/day, a requirement which is more typical of the honeymoon (partial remission) phase of T1D (8), where the presence of endogenous insulin allows patients to maintain good metabolic control at relatively low exogenous insulin doses.
Insulin requirements were modestly higher in CF patients after lung transplantation. These patients require lifelong therapy with glucocorticoids, which increase insulin resistance, and they are often on calcineurin inhibitors, which may decrease beta cell effectiveness. While better lung function and decreased pulmonary infection and inflammation following lung transplantation likely improve insulin sensitivity, it appears that this does not fully offset the stress of transplant medications on the beta cell.
In conclusion, exogenous insulin requirements are modest (<0.5 unit/kg/day) in the majority of both youth and adults with CFRD, indicating the persistence of endogenous insulin secretion throughout the CF lifespan. Youth do not require higher insulin doses than adults, suggesting that residual endogenous insulin secretion can compensate for the insulin resistance of puberty in adolescents with CF.
ABBREVIATIONS
- CF
Cystic fibrosis
- CFRD
Cystic fibrosis related diabetes
- HbA1c
Hemoglobin A1c
- OGTT
Oral glucose tolerance test
- T1D
Type 1 diabetes
- UM
University of Minnesota
Footnotes
CONFLICTS OF INTEREST: None
REFERENCES
- 1.Moran A, Dunitz J, Nathan B, Saeed A, Holme B, Thomas W. Cystic fibrosis related diabetes: current trends in prevalence, incidence and mortality. Diabetes Care. 2009;32:1626–1631. doi: 10.2337/dc09-0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blackman SM, Hsu S, Vanscoy LL, Collaco JM, Ritter SE, Naughton K, Cutting GR. Genetic modifiers play a substantial role in diabetes complicating cystic fibrosis. J Clin Endocrinol Metab. 2009;94:1302–1309. doi: 10.1210/jc.2008-2186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moran A, Brunzell C, Cohen RC, Katz M, Marshall BC, Onaday G, Robinson KA, Sabadosa KA, Stecenko A, Slovis B. Clinical care guidelines for CFRD: recommendations from the Cystic Fibrosis Foundation, the American Diabetes Association and the Pediatric Endocrine Society. Diabetes Care. 2010;33:2697–2708. doi: 10.2337/dc10-1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wiegand S, Raile K, Reinehr T, Hofer S, Nake A, Rabi W, Holl RW, DPV-Wiss Study Group Daily insulin requirement of children and adoelscents with type 1 diabetes: effect of age, gender, body mass index and mode of therapy. Eur J Endocrinol. 2008;158:543–549. doi: 10.1530/EJE-07-0904. [DOI] [PubMed] [Google Scholar]
- 5.Kerouz N, el-Hayek R, Langhough R, MacDonald MJ. Insulin doses in children using conventional therapy for insulin dependent diabetes. Diabetes Res Clin Pract. 1995;29:113–120. doi: 10.1016/0168-8227(95)01122-6. [DOI] [PubMed] [Google Scholar]
- 6.Moran A, Jacobs DR, Steinberger J, Hong C- P, Prineas R, Luepker R, Sinaiko AR. Insulin resistance during puberty. Diabetes. 1999;48:2039–2044. doi: 10.2337/diabetes.48.10.2039. [DOI] [PubMed] [Google Scholar]
- 7.Pankowska E, Syzypowska A, Kipka M. Basal insulin and total daily insulin doses in children with type 1 diabetes using insulin pumps. Pediatr Diabetes. 2008;9:208–213. doi: 10.1111/j.1399-5448.2008.00375.x. [DOI] [PubMed] [Google Scholar]
- 8.Hanas R, Donaghue KC, Klingensmith G, Swift PG. ISPAD clinical practice consensus gudeliness 2009 compendium. Pediatri Diabetes. 2009;10(Suppl 12):1–2. doi: 10.1111/j.1399-5448.2009.00577.x. [DOI] [PubMed] [Google Scholar]