Abstract
Objective
The Health Maintenance Consortium (HMC) is a multisite Grantee Consortium funded by the National Institutes of Health from 2004–2009. The goal of HMC is to enhance understanding of the long-term maintenance of behavior change, as well as effective strategies for achieving sustainable health promotion and disease prevention.
Methods
This introductory research synthesis prepared by the Resource Center gives context to this theme issue by providing an overview of the HMC and the articles in this journal.
Results
It explores the contributions to our conceptualization of behavior change processes and intervention strategies, the trajectory of effectiveness of behavioral and social interventions, and factors influencing the long-term maintenance of behavioral and social interventions.
Conclusions
Future directions for furthering the science of maintaining behavior change and reducing the gaps between research and practice are recommended.
Keywords: behavior change, maintenance, research consortia, physical activity, smoking, dietary behaviors, substance abuse, translational research, intervention research
The now classic Institute on Medicine (IOM) Report on Health and Behavior can be credited for bringing needed attention to a new field of research.1 The popular Roadmap metaphor is appropriate for a retrospective review of roads well-traveled as well as pointing to uncharted new territories.2 Over the past three decades, behavioral and social researchers have identified multi-level determinants of health,3,4 examined the complex processes linking health to behavior,1,5 and explored the efficacy of different intervention strategies for fostering healthful behaviors and environments.6–8 This knowledge has been accelerated by the funding of Research Consortia by the Office of Behavior and Social Research and other Institutes and Centers at the National Institutes of Health (NIH).9 For example, the Behavioral Change Consortium10 helped generate a body of knowledge about the effectiveness of different theory-based interventions on healthful lifestyle behaviors such as tobacco cessation, dietary behaviors, and physical activity.11–14
Knowing about strategies for initiating recommended health behaviors is a necessary first step toward achieving positive health outcomes. However, given that initially achieved gains often diminish after the conclusion of active intervention phases, understanding how to maintain gains over time is critical for promoting sustained population health benefits.13,15–21 Practical strategies and theoretical mechanisms for sustaining health behaviors over the life span are not well established or understood, but maintenance studies are necessary for translating behavior-change research into practice and reducing the burden of disease and health disparities.20 Just as medications for chronic illnesses are generally prescribed for long periods, health-behavior interventions may require long periods of active treatment.15,22 Of the maintenance studies available, primarily in the weight-loss field, there is clear evidence that few improvements are sustained long term,23–27 and this research area is characterized by scattered findings that are difficult to interpret.28,29
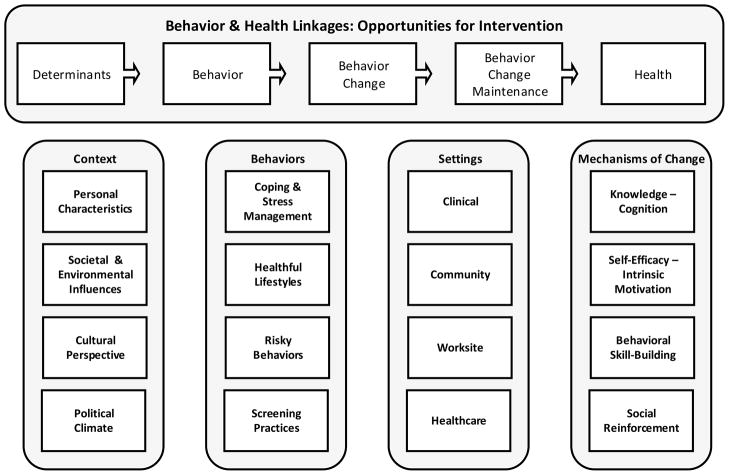
Figure 1 provides a conceptual framework for the processes linking behavior to health outcomes. Each point along the continuum from determinants, to behavior, to behavior change, to behavior change maintenance provides an opportunity for naturally occurring or planned intervention. Behavioral change maintenance requires an understanding of the surrounding context that can either facilitate or impede the behavior change process, the specifics of the behavior(s) being targeted, the intervention settings, and the mechanisms of change.
Figure 1.
Determinants and Processes of Health Behavior Change
In recognition of the need for a concentrated research effort to address the practical problems of sustaining behavioral changes in everyday life, the Health Maintenance Consortium (HMC) was created specifically to develop the science of maintaining healthful behavior.30 In 2003, the Office of Behavioral and Social Sciences Research mobilized several collaborating Institutes to amass resources to fund 19 projects and a Resource Center, with the common purpose of either furthering understanding about the processes of behavior change, or designing theory-based intervention strategies to achieve long-term maintenance of behavior change. After this initial funding, two more related studies became affiliated with HMC. Several communication strategies were implemented to help coordinate efforts and build synergies. This included semi-annual meetings of investigators between 2004 and 2009, the establishment of several “cross-cutting” workgroups, and a centralized website for sharing materials.
Table 1 provides a brief overview of the 21 funded studies and indicates the funded institutions, behavior change targets, target populations, intervention settings, utilized strategies, and study durations.
Table 1.
Health Maintenance Consortium Site and Study Information
| Study Investigators | Behavior Change Target (Study Type)a | Target Population (n) | Intervention Settingsb | Strategies Utilized | Follow-Up* (Yrs) |
|---|---|---|---|---|---|
| Behavioral Health Research Center of SW | Alcohol use (NH) | Convicted drunk-driving offenders (583) | N/A | Court mandated screening and referralc | 15 |
| Boston Medical Center | Fruit & vegetable consumption (I) | Adults (397) | C | 6 month telephony counseling based on Social Cognitive Theory; 6 month telephony counseling based on Goal Systems Theory | 2 |
| Brown Medical School, The Miriam Hospital | Diet, physical activity, & weight loss(NH) | Adults (542) | A | No intervention | 5+ |
| Drexel University | Diet & weight loss (I) | Primary care patients (280) | C | Meal replacements; Reduced Energy Density Eating Program | 2 |
| Emory University | Safer sex & HIV prevention (I) | African-American female adolescents (701) | B, C | 18 phone contacts with an individually tailored plan for participants | 3 |
| Fred Hutchison Cancer Research Center | Fruit & vegetable consumption (NH) | Employees in blue collar worksites (2018) | E | Four phase multi-level intervention with workplace events employee newsletters, self-help manual, constant inescapable messagesc | 4.5 |
| Friends Research Institute | Drug abstinence (I) | Methamphetamine-dependent individuals (118) | B, C | (0, 1, 2, and 4 months) of established contingency management program delivered with treatment program | 1 |
| Friends Research Institute | Drug abstinence (I) | Methamphetamine-dependent individuals (119) | B, C | 12 weeks of contingency management program: continuous; intermittent predictable; and intermittent unpredictable | 1 |
| HealthPartners Research Foundation | Physical activity (I) | Older adults (1,049) | C | Interactive telephone and mail based support | 2 |
| Lawrence Berkeley National Laboratory | Physical activity (I) | Walkers and runners (35,000) | C | Internet support resource | 4 |
| Oregon Health & Science University | Diet, physical activity, & weight loss (I) | Fire fighters (599) | E | Team-centered curriculum; motivational interviewingc | 5 |
| Oregon Research Institute | Multi-behavioral risk (NH) | Postmenopausal women with T2DM (279) | A | Comprehensive lifestyle change interventionc | 5 |
| Stanford University | Tobacco abstinence (NH) | Adult smokers (301) | C | Brief relapse counseling, written guides, telephone counseling | 1 |
| Treatment Research Institute | Drug abstinence (I) | Cocaine dependent methadone patients or cocaine dependent outpatients (130) | A, B | Extended duration of contingency management | 2 |
| University of Connecticut | Diet, physical activity, & weight loss (I) | Overweight and obese individuals (201) | B, C | Modifications to the home environment | 1.5 |
| University of Illinois - Chicago | Physical activity (I) | Older adults with osteoarthritis (419) | A | Negotiated maintenance plans; mainstreaming into ongoing facility-based program; Tapering telephone reinforcement | 1.5 |
| University of North Carolina - Chapel Hill | Screening mammography (I) | Middle-aged & older women (3,547) | C | Annual print or automated telephone reminders, tailored priming letters plus telephone counseling for women who became non-adherent in any year | 3.5 |
| University of Pennsylvania | Alcohol use (I) | Alcohol dependent patients (252) | B, C | Telephone monitoring and feedback; telephone monitoring and feedback plus counseling | 1.5 |
| University of Rochester | Tobacco abstinence (I) | Adult Smokers (836) | A | Training important others to be autonomy supportive, prescription medications to those with and without a quit date | 2 |
| University of Tennessee | Tobacco abstinence (I) | Adult smokers (406) | B | Increased behavioral and pharmological care | 2 |
| University of Washington | Suicide risk behaviors (NH) | Suicide vulnerable adolescents (615) | C, D | Parent and youth behavioral skills building curriculumc | 6 |
Note.
Refers to the follow-up assessment period after the initial intervention
NH=Natural History (includes process studies as well as follow-ups from prior interventions), I=Intervention (testing within HMC period)
A = Community, B = Health facility (e.g., clinic, hospital), C = Home, D = School, E = Workplace
Initial study
Although more detailed information can be found on the HMC website31 and in the articles of this Special Journal Issue,32 a few brief summary observations will be provided as an overview for this Special Journal Issue. Populations were targeted based on age-groups, health conditions, risk behaviors, or intervention delivery settings. Nearly 50,000 individuals from adolescence to adulthood to old age were involved in this HMC supported research, making this the largest group of studies of behavior change maintenance funded to date.
Consistent with the research solicitation, two different types of studies were funded: 1) “process studies” to understand basic processes involved in naturalistic behavior change and 2) “intervention studies” to examine impacts of planned change. Within the latter category, some were “natural history studies” that examined how long effects of earlier interventions could be maintained without any follow-up, and others were “maintenance intervention studies” that tested strategies for enhancing longer term maintenance of the behavior with extended follow-up and attendant outcomes. All studies had at least one-year follow-ups after the active intervention, but some which were funded previously were able to observe follow-up behaviors over five years and longer. These studies in particular provide rare opportunities to document the “natural history” of maintenance of effects (which are not well understood), identify theoretically important mediating mechanisms underlying these phenomena, and lay the groundwork for translating research into practice.
In contrast to the previous Behavior Change Consortium,10 a wider range of behaviors were examined in the HMC. Four categories were included: healthful lifestyle practices (eg, physical activity, eating behaviors); risky behaviors (e.g., alcohol consumption, illicit substance abuse, tobacco use, suicidal risk behaviors); coping and stress management; and cancer prevention screening behaviors. Another advantage of the HMC was its ability to examine behavior change maintenance in a wide variety of settings including home, community, school, health care, and work place. Given the variety of behaviors, settings, and populations, it is not surprising that different strategies of varying intensities and durations were utilized to help promote longer term maintenance. However, there were also similarities in strategies, which reflect the popular follow-up procedures of contingency management, telephone reinforcement, and print reminders, as well as more individually tailored approaches.
This Special Journal Issue will advance knowledge about long-term maintenance of behavior change interventions by drawing conceptual frameworks and empirical research from a subset of HMC investigators. It is organized into three major sections: 1) introductory material to set the stage for understanding the current state of behavior change research, including an NIH perspective on the history and importance of this research area; a Guest Editors’ perspective on the science of behavior change with an overview of HMC research as related to the Special Journal Issue manuscripts; and two frameworks for understanding the different terminology for various maintenance concepts and methods; 2) original research article contributions that reflect the natural history of behavior change maintenance; the successes and challenges in designing specific maintenance interventions; and mediators and moderators of intervention outcomes; and 3) cross-cutting manuscripts that address a taxonomy for reporting intervention components; strategies for making interventions more culturally relevant; and research translation issues related to the dissemination and sustainability of efficacious behavior maintenance strategies.
Setting the Stage: Defining and Measuring Maintenance Concepts
The articles in this Special Journal Issue reflect novel insights about processes and outcomes of interventions aiming to sustain post-treatment behavioral changes over extended time periods. Despite the recent attention given to behavioral change maintenance, it is important to note that synthesis in the field has been limited by a lack of consistent definitions or constructs for measuring maintenance across behaviors. The article by Seymour and colleagues33 describes work by the HMC Maintenance Workgroup to provide a baseline assessment of how maintenance and maintenance-related constructs were viewed by HMC investigators. While both commonalities and differences were noted within and across behaviors, a major contribution of this group was a consensus statement on basic terminology and operational definitions. Such standardization (eg, differentiating maintenance from adherence, and specifying important maintenance-related constructs such as grace period, relapse, and reactivation) is a first step in advancing the quality of transbehavioral research.
The paper by Gierisch et al33 offers a conceptual framework for understanding adherence to infrequent, repeated health behaviors such as screening mammography and HPV vaccination regimen, which was not examined by the HMC Maintenance Workgroup. Greater attention to these infrequent but repeated behaviors is relevant to understanding the extent to which many preventive screening guidelines are met. Gierisch and colleagues conceptualize these behaviors as being arrayed across an adherence continuum identified by initiating behavior (initiation), adherence to most recent opportunity (on-schedule), or timely adherence across multiple behaviors (maintenance or completion). As behaviors become more widely adopted, the research focus is likely to shift from attention on initiation to on-schedule to maintenance behaviors. Consistent with the more frequent lifestyle behaviors examined by the HMC Maintenance Workgroup, the standardization of adherence terminology for infrequent, but repeated health behaviors can facilitate comparisons across studies.
Empirical Findings from HMC Studies: Building the Knowledge Base
We briefly overview the findings presented in this volume, which indicate major contributions to further the science of behavior change research and suggest areas for future research.
Long-term intervention effects on improving healthful behaviors
A fundamental research question in behavior change research is how long positive gains can be sustained without additional long-term support. In most cases this is unknown because studies only track maintenance for a year or two after the post-intervention phase. Three articles examined the long-term maintenance effects of behavioral interventions that initially produced immediate positive outcomes in randomized controlled trials. These studies provide insights into behavioral trajectories over time. In the majority of cases, intervention effects on lifestyle behaviors are often strongest in the one or two years closest to active intervention. Without additional support, positive effects tend to diminish over time, or treatment differences vanish.
Toobert and colleagues34 provide unique evidence to determine the extent to which the effects of a multiple behavioral intervention can be sustained five years post-treatment. In this study, 279 postmenopausal women with type 2 diabetes at risk for heart disease were exposed to a two-year intervention with assessments at 6, 12, and 24 months, and then followed for five more years. The researchers investigated the long-term effects of an initial trial targeting healthful eating, physical activity, stress management, and supportive resources. Although behavioral changes among women were successfully achieved during the first two years of the program, the study documents that with no additional maintenance treatment, multiple behaviors in intervention and control participants were only partially sustained through the 84-month assessment.
This article raises the practical question of whether or not it is realistic to expect long-term maintenance of benefits attributed to initial intervention strategies. Calling for a broader view of strategies for achieving longer term maintenance, Toobert and colleagues suggest moderate-intensity behavioral interventions may need to be coupled with more environmental changes to sustain long-term effects. Additionally, the field can benefit from examining subgroup patterns (eg, assessing factors associated with participants who show no gains, those who start off with gains then decline, those who do manage to sustain behavioral changes and benefits over time).
Two other studies focus on work settings reporting follow-up data after exposure to nutrition and exercise programs. In the study by MacKinnon et al,35 599 healthy firefighters were exposed to one of two behavioral interventions (ie, either a social influences team-centered curriculum, an individually based motivational intervention approach). During the first two years of active and booster intervention phases, both approaches produced significant positive behavioral changes in dietary and physical activity behaviors, although some differences were noted in specific outcomes. However, the researchers found that most differences in behavioral changes between treatment and control groups diminished over the four additional waves of annual follow-ups. A closer examination revealed the importance of looking at behavioral trajectories over time. Positive gains by all groups suggest a diffusion effect across different firefighter worksites rather than the typical assumptions of a loss of intervention group gains. MacKinnon and colleagues add to the behavior change literature by calling attention to the value of studying a concept they refer to as the “behavioral tipping” point (ie, examining whether there is a point where incremental change past a threshold level can produce sustained effects).
Beresford et al36 also examined sustained nutrition changes in a work setting with blue-collar employees in small to medium sized businesses. The initial intervention strategy focused on collaborations with employee advisory boards to sponsor work-site events and provide tailored newsletters promoting more healthful eating. Although the average long-term program effects were not large (ie, 0.25 servings a day), the program showed a statistically significant increase in fruit and vegetable intake in blue-collar worksites two years after the program ended. This research emphasizes that behavioral change with low-intensity interventions is often a gradual process whereby small gains among many people can result in public health improvements.
Work-sites can be an ideal setting for broader dissemination and further research is needed to determine characteristics of worksites that might make them especially effective in promoting behavior change. Beresford and colleagues suggest that “social facilitation maintenance” may be a key behavior change strategy,37 which is difficult to detect in the typical short term intervention study. Consistent with the firefighter workplace study,35 a diffusion of intervention effects may have also been present in this study with some companies continuing to engage in intervention processes on their own and changing social norms influencing healthful food consumption patterns over time. Future behavioral research should acknowledge and build upon naturally occurring opportunities for disseminating health promotion messages and supportive strategies throughout entire organizational settings.
Long-term intervention effects on decreasing unhealthy behaviors
Two studies examine the long-term impacts of early prevention and referral interventions to reduce risky behaviors that may persist over time as individuals transition into different life-course stages. Examining whether early interventions can ease the transition between adolescence and adulthood among youth participants identified as “suicide vulnerable adolescents,” Hooven and colleagues38 confirm the long-term value of early intervention efforts that are designed to reduce suicide risk behaviors, anger, and depression. An examination of outcomes for this brief adolescent suicide prevention intervention shows remarkably long-term results, with positive changes to suicide risk behaviors sustained across the transition to young adulthood. These effects were accomplished by helping youth and their parents develop personal and social skills to meet life challenges through appropriate help-seeking, support activation, and problem awareness. This study contributes to the behavioral change maintenance literature by illustrating how latent class growth models can identify different patterns of change to further explicate the generally positive results found for early screening and intervention for adolescent distress. Following over 500 youth for up to a 72-month follow-up period, the investigators reveal that initial risk levels and intervention types seem to make a difference with those at lowest levels of initial suicide behavior and substance use, those having access to the most intensive interventions (eg, combined parent and youth interventions), and those doing better earlier over the follow-up period. These findings suggest the importance of considering a stepped intervention approach of providing more intensive interventions for those with higher initial risk profiles.
The long-term effects of court-mandated screening and referral for first time offenders for driving while intoxicated was also examined, echoing many similar themes found in the suicide prevention intervention described above. Following 583 first driving while impaired (DWI) offenders with substance use disorders for 15 years to study the natural history of drinking and drug abuse, Lapham and Skipper39 report the persistence of substance use disorders and driving over the alcohol limit for a large subgroup of these offenders. These authors add to our understanding of on the usefulness of initial screening classification, coupled with data on client compliance with court mandates, in predicting long term outcomes. Referring convicted DWI offenders to a screening program assessing the severity of substance abuse disorders and providing treatment referrals can be a useful tool to refer offenders to specialized, appropriate services for their risk profiles. Future interventions should be guided by closer attention to initial risk factors resulting in more effective triage to specialized services. The noncompliant offenders who did not complete the screening program had the highest rates of substance use disorders and utilized more treatment resources over the ensuing years than other groups. This finding indicates a need for close monitoring of noncompliant offenders and raises the possibility that screening programs should develop special sanctions or monitored treatment programs for these individuals. It also raises the possibility that the screening services may have served as a brief intervention that was beneficial to those who completed the screening process. A randomized study of the beneficial effects of screening is greatly needed.
Bolstering behavior change maintenance for physical activity
Two studies on physical activity with older populations explored strategies that bolster and mediate behavior change maintenance. Hughes and colleagues40 assessed ways to bolster maintenance of physical activity in 259 older adults 18 months after completion of an 8-week multi-component exercise/behavior change program designed for older adults with osteoarthritis. The positive effects of the evidence-based Fit and Strong! program on exercise maintenance as well as improvements in physical functioning were sustained over this period of time. This study adds to the limited knowledge about the relative effectiveness of different mechanisms for bolstering long-term maintenance. Effective bolstering strategies reported in this study included negotiated follow up plans with and without telephone reinforcement compared to referral to an ongoing class with and without reinforcement calls. Although there was variation by different study outcomes, negotiated follow-up, in combination with telephone reinforcement, was associated with the most positive outcomes. The negotiated condition (ie, developing an individualized maintenance plan toward the end of the active intervention phase) is a strategy that could easily become part of other behavior change interventions. Including follow-up phone calls can be an effective, low-cost adjunct to achieving longer term benefits.
In the behavioral research field, mediational analyses have typically focused on understanding mechanisms of behavioral initiation with factors such as self efficacy, behavioral processes of change, and social support. Crain et al41 provide unique insights on the role of mediating factors in physical activity maintenance achieved through the Keep Active Minnesota. This program demonstrated positive two-year maintenance effects for physically active adults (ie, age 50–70 years) who participated in an interactive telephone and mail-based physical activity support intervention. Structural equation modeling was utilized to examine direct and indirect influences on physical activity maintenance. Incorporation of physical activity into the self concept emerged as the strongest predictor, with self-efficacy having a major indirect influence confirming it as an important predictor for both behavioral initiation and maintenance. In understanding why maintenance interventions work, the authors conclude that no single mediator makes a large impact; rather, there is a “long and winding road” with maintenance achieved through a multitude of modest interrelated meditational pathways from behavioral initiation to maintenance. Additionally, given the complexities of maintenance processes, it is important to examine multiple and recursive relationships between predictors and outcomes over time.
Factors affecting successful substance abuse interventions
Three articles in this Special Journal Issue present valuable data to address two significant questions in substance abuse treatment: Is it possible to sustain initial changes in high risk substance abuse behaviors? What are potential moderators or predictors of maintained abstinence? Behavior change and maintenance in substance abusing populations are especially challenging and often rely on different intervention strategies than typically seen in physical activity or nutrition lifestyle interventions.
Researchers in the substance abuse field have implemented contingency management interventions for about three to six months to develop and reinforce new abstinent behaviors.42,43 However, longer durations of abstinence during treatment predict better maintenance of abstinence afterwards,44 suggesting that longer durations of contingency management treatment may improve maintenance. A study by Carpenedo et al45 with 130 cocaine users in methadone maintenance treatment assessed whether (nine months) of voucher-based reinforcement therapy (VBRT) increased long-term abstinence compared to standard (3 months) durations of VBRT. These researchers found extended VBRT was helpful in initiating abstinence in the first year, but it was not a factor in predicting longer-term abstinence after removal of the voucher contingencies in the second year. Longer periods of abstinence during the first year predicted abstinence in the second year, suggesting the importance of intervention focus on achieving early abstinence. This finding also suggests that outside variables may be contributing to both success in VBRT and to longer-term maintenance of abstinence. Thus, future research might focus on the types of naturally-occurring outside variables that operate during treatment and recovery, and whether these naturally occurring reinforcers might be better utilized to improve maintenance of abstinence.
Continuing care programs are often recommended for heavy drinkers who tend to relapse after primary treatment. Lynch et al46 evaluated the benefits of adding 18-month telephone interventions to standard continuing care for alcoholic patients in intensive outpatient programs and examined potential moderators. Prior research47,48 confirmed that telephone follow-up that combined monitoring, feedback, and counseling was the most effective strategy for achieving better alcohol use outcomes in 252 alcohol dependent patients who had initially engaged in an intensive outpatient program. The current article addresses the important moderator research question: Are there certain types of patients who are most likely to achieve intervention benefits? At least in the current study, none of the variables examined moderated the effect favoring the extended telephone continuing care intervention over standard care. Therefore, the effects of this intervention were relatively robust and it can be recommended for alcohol dependent patients regardless of their personal characteristics (eg, gender, substance use history, early treatment response, craving levels, motivation for change, appraisals of harms and benefits, self-efficacy). Conversely, a second telephone-based intervention evaluated in the study that consisted of monitoring and feedback only, without counseling, showed to be more effective than standard care only for women and those with low motivation for change at baseline.
Moderator analyses were also the focus of a study predicting factors associated with treatment response for a successful smoking cessation program. In prior research, Killen and colleagues49 demonstrated the effectiveness of extended cognitive behavioral therapy in maintaining smoking abstinence for adults. Conducting a secondary analysis from this study of 301 adult smokers, Bailey et al tested two models using signal detection analysis.50 Although each model identified factors that created algorithms for classifying smokers into different subgroups based on their rates of maintained abstinence through a one-year follow-up, the distinguishing subgroup characteristics differed between the two models. In the first model which focused on pretreatment factors, predictors of maintained smoking abstinence included lower nicotine dependence, lower depressive symptoms, and higher body mass index. In the second model which also included clinical data measured during treatment, self-efficacy was the strongest predictor of maintained abstinence. While there have now been several studies using signal detection type methodologies to define subgroups based on different treatment outcomes, this is one of the first studies to include both pretreatment and treatment process variables. Signal detection can be a useful tool for helping interventionists tailor treatment research protocols based on treatment responses.
Cross-cutting Issues in Health Maintenance Research
In addition to defining and measuring maintenance concepts (see articles by Seymour et al; Gierisch et al),33,51 behavioral change research can benefit from more standardization of intervention modalities and transbehavioral outcomes. The multi-site nature of HMC provides a unique opportunity to move beyond the typical single study focus to address the practice and policy relevant question of “what works” to maintain healthy behaviors across different populations and settings. There is also the opportunity to explore what works among or across different behaviors, dependent upon the availability of common endpoints. This became the focus of the Transbehavioral Outcome Workgroup.
The identification of essential features of an intervention is important for the development, implementation, and evaluation of interventions designed to enhance long-term behavioral maintenance. Toward this end, a HMC Treatment Modalities workgroup was established to provide a comprehensive inventory of interventions for all projects involved in the HMC as an initial step in the examination of outcome results based on comparable intervention components. Schulz et al52 build on this categorization of interventions and collaboration among projects to further enhance the understanding of the role that different intervention strategies play in the long-term maintenance of behavior change.
The development of a common lexicon presupposes a taxonomy for characterizing intervention elements that enables researchers to share and replicate findings. The HMC taxonomy includes attention to both delivery characteristics (eg, mode, materials, location, scheduling, scripting, sensitivity to participant characteristics, interventionist characteristics, adaptability, treatment options) and the content and goals of the intervention (e.g., treatment content strategies, mechanisms of action). The iterative process which included both behavioral scientists and interventionists resulted in a framework that goes beyond existing taxonomies and better captures the complexity of intervention designs for long-term maintenance.
Attention to cultural sensitivity is one intervention element in the HMC taxonomy that is examined in fuller detail in the article by Mier et al.53 While all NIH studies are required to report on gender and minority representation, less is known about how concepts of cultural sensitivity are incorporated into intervention designs. Working with the HMC Modality Workgroup, Mier and colleagues explored the extent to which, and processes by which, HMC investigators engaged in cultural tailoring for ethnic minority groups and how tailoring might facilitate better long-term maintenance.
Behavior and social researchers in general and within the HMC set of investigations have adopted principles of intervention tailoring. However, this adoption is more in terms of general tailoring to meet particular needs of the targeted population (eg, access to classes, transportation, schedules, literacy levels) versus specific cultural tailoring (eg, consideration of the norms, cultural beliefs and values, behavior patterns, histories of a specific population). The examples provided by four case studies that engaged in cultural tailoring provide strategies that can be used by other investigators to make their interventions more culturally sensitive. It is important to note lessons learned from HMC researchers: 1) cultural tailoring is on a continuum—it is not a “yes or no” issue; 2) it has to be individually oriented; 3) it should be congruent with participants’ demographics, cultural norms, and social context; and 4) it is time consuming and requires an explicit commitment. Given the growing diversity of America, it is important to build cultural tailoring into intervention designs as a way of helping to reduce ethnic disparities in health behaviors and related health outcomes.
The initial goal of the HMC initiative was to examine behavioral processes or intervention strategies related to achieving long-term behavioral maintenance. But just like behaviors, research emphases and priorities can change over time, both in natural and planned ways.
There were two notable shifts in the research enterprise over the course of funding for these HMC projects. After the projects were funded, it was evident that more attention needed to be paid toward the role of the larger environment in facilitating or hindering long-term behavior change. Hence, an Environmental Workgroup was formed to assess naturally occurring or planned environmental influences that may be part of the intervention; consequences of the intervention (spread of effect); or confounders or facilitators to the intervention as they affect either behavioral maintenance or program sustainability. A second theme, promoted by the then NIH Director, Elias Zerhouni, that emerged after initial funding was the importance of research translation.
Russell Glasgow54 focuses on both of these themes in his closing commentary reflecting on factors making interventions “real and taking them to scale”. Putting dissemination and implementation into practice within the NIH research agenda is important for ensuring that research findings make a difference in people’s everyday lives. This is particularly relevant for knowledge about intervention strategies for sustaining positive intervention benefits. Glasgow rightly calls for more attention to the context in which social and behavioral interventions are being conducted, additional research aimed at reducing recalcitrant disparities in health and health behaviors, and valuing replication studies that can unravel the complexities underlying intervention successes or failures. What is especially valuable about Glasgow’s commentary is his concrete suggestions for moving the field forward by changing the research paradigm from a primarily individually or institution-specific one to a broader community of scholars. Sharing research data and intervention protocols, engaging in research networks that can promote attention to intervention successes, and establishing new partnerships can all help jump start new research and/or identify interventions ready for application.
Toward a new decade of behavioral research
This Special Journal Issue makes a fundamental contribution to our conceptualization of behavior change processes and intervention strategies, the trajectory of effectiveness of behavioral and social interventions, and factors influencing the long-term maintenance of initially positive behavioral and social interventions. As we embark on a new decade, we know much more about sustaining long-term behavior than we did at the start of the health maintenance consortium. Yet, we can point to many questions that remain to be answered.
This Special Journal Issue highlights both commonalities and differences in treatment response across behaviors, populations, and settings. We are hopeful that the information provided about standardizing definitions and measures of maintenance and treatment modality terminology will help to advance the field. There lacks consensus about whether different factors predict behavioral initiation and maintenance, as some mediators such as self-efficacy appear to be important for both processes. There was also a lack of consistency on the importance of moderators for determining treatment response, suggesting the robustness of some behavioral interventions across populations, or alternatively the lack of variability in who is participating in intervention studies. Future research efforts should continue to employ new methodological approaches for untangling the complex web of interactions linking both moderators and mediators to treatment outcomes over long periods of time.
We are just beginning to appreciate the importance of addressing multiple behaviors concurrently, but more attention must be given to the advantages and disadvantages of multi-behavioral intervention approaches, and how they can most effectively be implemented.14,55,56 It is still unclear, for example, whether simultaneous attention to different interrelated behaviors results in building behavioral synergies that make it easier to change behaviors or if these efforts overload the individual’s capacity to make changes. A major limitation in evaluating multi-behavior intervention approaches is that our outcomes are typically behavior-specific, as well as population-specific (e.g., success is often different for youth versus adults versus older adults). The HMC Outcomes Workgroup, like the BCC predecessor group was unable to reach consensus about uniform metrics for assessing transbehavioral outcomes. This group has identified different metrics that reflect disciplinary perspectives, and continues to explore if a uniform metric is an attainable, or even desirable, goal.
Individual tailoring or adaptation is a major theme in many of the HMC research studies, with several systematically examining the value of staged or stepped care approaches dependent upon previous successes or failures. While behavioral scientists promote individual tailoring as an important intervention ingredient, our intervention paradigms are still research-driven. That is, we randomize participants into “artificial” groups and then expend substantial effort tailoring to participant’s preferences and needs. An alternative approach might be to allowing participants to select the intervention strategy that best resonates with them, and explore why participants choose different approaches, and if those allowed to choose have better outcomes than those assigned to pre-determined intervention options.57
The Health Maintenance Consortium can point to many accomplishments over its five year history. In our opinion, one of the biggest successes was having a safe spot for researchers to exchange preliminary research and discuss such issues that are at the heart of advancing the science of sustaining behavior change. This Special Journal Issue is one product we are especially pleased to share with others interested in health behavior research. We invite readers to visit the HMC website (http://hmcrc.srph.tamhsc.edu) where they can learn more about all of the HMC research projects and remain abreast of new publications from HMC investigators.
Contributor Information
Marcia G. Ory, Email: MOry@srph.tamhsc.edu.
Matthew Lee Smith, Email: matlsmit@tamu.edu.
Nelda Mier, Email: nmier@srph.tamhsc.edu.
Meghan M. Wernicke, Email: MMWernicke@srph.tamhsc.edu.
References
- 1.Institute of Medicine. Health and Behavior: The Interplay of Biological, Behavioral, and Societal Influences. Washington, DC: National Academies Press; 2001. [PubMed] [Google Scholar]
- 2.Zerhouni E. Medicine. The NIH Roadmap. Science. 2003 Oct 3;302(5642):63–72. doi: 10.1126/science.1091867. [DOI] [PubMed] [Google Scholar]
- 3.McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988 Winter;15(4):351–377. doi: 10.1177/109019818801500401. [DOI] [PubMed] [Google Scholar]
- 4.National Research Council. Committee on Future Directions for Behavioral and Social Sciences Research at the National Institutes of Health, Singer BH, Ryff CD, (Eds) Washington, D.C: The National Academies Press; 2001. New Horizons in Health: An Integrative Approach. [PubMed] [Google Scholar]
- 5.Hamburg DA, Elliott GR, Parron DLE. Frontiers of research in the biobehavioral science. Washington, D.C: National Academy Press; 1982. Health and Behavior. [Google Scholar]
- 6.Rowe JW, Kahn RL. Successful Aging. New York: Pantheon Books; 1998. [Google Scholar]
- 7.National Research Council. Promoting Health: Intervention Strategies from Social and Behavioral Research. In: Smedley BD, Syme SL, editors. Committee on Capitalizing on Social Science and Behavioral Research to Improve the Public’s Health, Division of Health Promotion and Disease Prevention. Washington, D.C: National Academies Press; 2000. [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. [Accessed March 2, 2010];The Community Guide to Preventive Services (on-line) Available at: http://www.thecommunityguide.org/index.html.
- 9.National Institutes of Health. [Accessed March 2, 2010];Office of Behavioral and Social Sciences Research (on-line) Available at: http://obssr.od.nih.gov.
- 10.Ory MG, Jordan PJ, Bazzarre T. The Behavior Change Consortium: setting the stage for a new century of health behavior-change research. Health Educ Res. 2002 Oct;17(5):500–511. doi: 10.1093/her/17.5.500. [DOI] [PubMed] [Google Scholar]
- 11.Toobert DJ, Strycker LA, Glasgow RE, et al. Effects of the mediterranean lifestyle program on multiple risk behaviors and psychosocial outcomes among women at risk for heart disease. Ann Behav Med. 2005 Apr;29(2):128–137. doi: 10.1207/s15324796abm2902_7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elliot DL, Goldberg L, Kuehl KS, et al. The PHLAME (Promoting Healthy Lifestyles: Alternative Models’ Effects) firefighter study: outcomes of two models of behavior change. J Occup Environ Med. 2007 Feb;49(2):204–213. doi: 10.1097/JOM.0b013e3180329a8d. [DOI] [PubMed] [Google Scholar]
- 13.Williams GC, Niemiec CP, Patrick H, et al. The importance of supporting autonomy and perceived competence in facilitating long-term tobacco abstinence. Ann Behav Med. 2009 Jun;37(3):315–324. doi: 10.1007/s12160-009-9090-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nigg CR, Allegrante JP, Ory M. Theory-comparison and multiple-behavior research: common themes advancing health behavior research. Health Educ Res. 2002 Oct;17(5):670–679. doi: 10.1093/her/17.5.670. [DOI] [PubMed] [Google Scholar]
- 15.Norris SL, Lau J, Smith SJ, et al. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002 Jul;25(7):1159–1171. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- 16.Hajek P, Stead LF, West R, et al. Relapse prevention interventions for smoking cessation. Cochrane Database Syst Rev. 2009;(1):CD003999. doi: 10.1002/14651858.CD003999.pub3. [DOI] [PubMed] [Google Scholar]
- 17.Williams DM, Lewis BA, Dunsiger S, et al. Comparing psychosocial predictors of physical activity adoption and maintenance. Ann Behav Med. 2008 Oct;36(2):186–194. doi: 10.1007/s12160-008-9054-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Muller-Riemenschneider F, Reinhold T, Nocon M, Willich SN. Long-term effectiveness of interventions promoting physical activity: a systematic review. Prev Med. 2008 Oct;47(4):354–368. doi: 10.1016/j.ypmed.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 19.Rothman AJ. Toward a theory-based analysis of behavioral maintenance. Health Psychol. 2000 Jan;19(1 Suppl):S64–S69. doi: 10.1037/0278-6133.19.suppl1.64. [DOI] [PubMed] [Google Scholar]
- 20.Glasgow RE, Klesges LM, Dzewaltowski DA, et al. The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Ann Behav Med. 2004 Feb;27(1):3–12. doi: 10.1207/s15324796abm2701_2. [DOI] [PubMed] [Google Scholar]
- 21.Ryan RM, Patrick H, Deci EL, Williams GC. Facilitating health behaviour change and its maintenance: Interventions based on self-determination theory. The European Health Psychologist. 2008;10:2–5. [Google Scholar]
- 22.Turk MW, Yang K, Hravnak M, et al. Randomized clinical trials of weight loss maintenance: a review. J Cardiovasc Nurs. 2009 Jan-Feb;24(1):58–80. doi: 10.1097/01.JCN.0000317471.58048.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kumanyika SK, Van Horn L, Bowen D, et al. Maintenance of dietary behavior change. Health Psychol. 2000 Jan;19(1 Suppl):S42–S56. doi: 10.1037/0278-6133.19.suppl1.42. [DOI] [PubMed] [Google Scholar]
- 24.Pavlou KN, Krey S, Steffee WP. Exercise as an adjunct to weight loss and maintenance in moderately obese subjects. Am J Clin Nutr. 1989 May;49(5 Suppl):S1115–S1123. doi: 10.1093/ajcn/49.5.1115. [DOI] [PubMed] [Google Scholar]
- 25.Wing RR, Papandonatos G, Fava JL, et al. Maintaining large weight losses: the role of behavioral and psychological factors. J Consult Clin Psychol. 2008 Dec;76(6):1015–1021. doi: 10.1037/a0014159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wing RR, Tate DF, Gorin AA, et al. A self-regulation program for maintenance of weight loss. N Engl J Med. 2006 Oct 12;355(15):1563–1571. doi: 10.1056/NEJMoa061883. [DOI] [PubMed] [Google Scholar]
- 27.Wing RR, Tate DF, Gorin AA, et al. STOP regain: are there negative effects of daily weighing? J Consult Clin Psychol. 2007 Aug;75(4):652–656. doi: 10.1037/0022-006X.75.4.652. [DOI] [PubMed] [Google Scholar]
- 28.Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005 Feb;6(1):67–85. doi: 10.1111/j.1467-789X.2005.00170.x. [DOI] [PubMed] [Google Scholar]
- 29.Pi-Sunyer X, Blackburn G, Brancati FL, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care. 2007 Jun;30(6):1374–1383. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nilsen WJ, Haverkos L, Nebeling L, Vogel Taylor M. Maintenance of long-term behavior change. Am J Health Behav. 2010 doi: 10.5993/ajhb.34.6.1. In press. [DOI] [PubMed] [Google Scholar]
- 31.The Health Maintenance Consortium Resource Center. [Accessed March 2, 2010];Health Maintenance Consortium Resource Center (HMCRC) (online) Available at: http://hmcrc.srph.tamhsc.edu.
- 32.Ory M, Smith ML, Mier N. Health Maintenance Consortium special issue behavior maintenance programs: successes, collaborations, and future directions. Am J Health Behav. 2010 In press. [Google Scholar]
- 33.Seymour RB, Hughes SL, Ory MG, et al. Commonalities and differences in measuring maintenance of behavior change. Am J Health Behav. 2010 doi: 10.5993/ajhb.34.6.3. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Toobert DJ, Strycker LA, Barrera M, Glasgow RE. Seven-year follow-up of a multiple-health-behavior diabetes intervention. Am J Health Behav. 2010 doi: 10.5993/ajhb.34.6.5. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.MacKinnon DP, Elliot DL, Thoemmes F, et al. Long-term effects of a worksite health promotion program for firefighters. Am J Health Behav. 2010 doi: 10.5993/ajhb.34.6.6. In press. [DOI] [PubMed] [Google Scholar]
- 36.Beresford SA, Thompson B, Bishop S, et al. Long term fruit and vegetable change in worksites: Seattle 5 a Day Follow-up. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wilfley DE, Stein RI, Saelens BE, et al. Efficacy of maintenance treatment approaches for childhood overweight: a randomized controlled trial. JAMA. 2007 Oct 10;298(14):1661–1673. doi: 10.1001/jama.298.14.1661. [DOI] [PubMed] [Google Scholar]
- 38.Hooven C, Herting JR, Snedker KA. Long-term outcomes for the promoting CARE suicide prevention program. Am J Health Behav. 2010 doi: 10.5993/ajhb.34.6.8. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lapham SC, Skipper BJ. Does screening classification predict long-term outcomes of DWI offenders? Am J Health Behav. 2010 doi: 10.5993/ajhb.34.6.9. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hughes SL, Seymour RB, Campbell RT, et al. Fit and Strong!: bolstering maintenance of physical activity among older adults with lower-extremity osteoarthritis. Am J Health Behav. 2010 doi: 10.5993/ajhb.34.6.10. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Crain AL, Martinson BC, Sherwood NE, O’Connor PJ. The long and winding road to physical activity maintenance. Am J Health Behav. 2010 doi: 10.5993/ajhb.34.6.11. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Higgins ST, Budney AJ, Bickel WK, et al. Incentives improve outcome in outpatient behavioral treatment of cocaine dependence. Arch Gen Psychiatry. 1994 Jul;51(7):568–576. doi: 10.1001/archpsyc.1994.03950070060011. [DOI] [PubMed] [Google Scholar]
- 43.Chambless DL, Ollendick TH. Empirically supported psychological interventions: controversies and evidence. Annu Rev Psychol. 2001;52:685–716. doi: 10.1146/annurev.psych.52.1.685. [DOI] [PubMed] [Google Scholar]
- 44.Higgins ST, Badger GJ, Budney AJ. Initial abstinence and success in achieving longer term cocaine abstinence. Exp Clin Psychopharmacol. 2000 Aug;8(3):377–386. doi: 10.1037//1064-1297.8.3.377. [DOI] [PubMed] [Google Scholar]
- 45.Carpenedo CM, Kirby KC, Dugosh KL, et al. Extended voucher-based reinforcement therapy for long-term drug abstinence. Am J Health Behav. 2010 doi: 10.5993/ajhb.34.6.12. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lynch KG, Van Horn D, Drapkin M, et al. Moderators of response to telephone continuing care for alcoholism. Am J Health Behav. 2010 doi: 10.5993/ajhb.34.6.13. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McKay JR, Lynch KG, Shepard DS, Pettinati HM. The effectiveness of telephone-based continuing care for alcohol and cocaine dependence: 24-month outcomes. Arch Gen Psychiatry. 2005 Feb;62(2):199–207. doi: 10.1001/archpsyc.62.2.199. [DOI] [PubMed] [Google Scholar]
- 48.McKay JR, Lynch KG, Shepard DS, et al. The effectiveness of telephone-based continuing care in the clinical management of alcohol and cocaine use disorders: 12-month outcomes. J Consult Clin Psychol. 2004 Dec;72(6):967–979. doi: 10.1037/0022-006X.72.6.967. [DOI] [PubMed] [Google Scholar]
- 49.Killen JD, Fortmann SP, Schatzberg AF, et al. Extended cognitive behavior therapy for cigarette smoking cessation. Addiction. 2008 Aug;103(8):1381–1390. doi: 10.1111/j.1360-0443.2008.02273.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bailey SR, Hammer SA, Bryson SW, et al. Using treatment process data to predict maintained smoking abstinence. Am J Health Behav. 2010 doi: 10.5993/ajhb.34.6.14. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gierisch JM, Reiter PR, Rimer BK, Brewer NT. Standard definitions of adherence for infrequent yet repeated health behaviors. Am J Health Behav. 2010 doi: 10.5993/ajhb.34.6.4. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Schulz R, Czaja SJ, McKay JR, et al. Intervention Taxonomy (ITAX): describing essential features of interventions. Am J Health Behav. 2010 doi: 10.5993/ajhb.34.6.15. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Mier N, Ory MG, Toobert DJ, et al. A qualitative case study examining intervention tailoring for minorities. Am J Health Behav. 2010 In press. [PMC free article] [PubMed] [Google Scholar]
- 54.Glasgow RE. HMC research translation: speculations about making it real and going to scale. Am J Health Behav. 2010 doi: 10.5993/ajhb.34.6.17. In press. [DOI] [PubMed] [Google Scholar]
- 55.Prochaska JJ, Nigg CR, Spring B, et al. The benefits and challenges of multiple health behavior change in research and in practice. Prev Med. 2010 Jan-Feb;50(1–2):26–29. doi: 10.1016/j.ypmed.2009.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Prochaska JJ, Spring B, Nigg CR. Multiple health behavior change research: an introduction and overview. Prev Med. 2008 Mar;46(3):181–188. doi: 10.1016/j.ypmed.2008.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Glasgow RE, Edwards LL, Whitesides H, et al. Reach and effectiveness of DVD and in-person diabetes self-management education. Chronic Illn. 2009 Dec;5(4):243–249. doi: 10.1177/1742395309343978. [DOI] [PubMed] [Google Scholar]