Abstract
There are many studies on the prevalence, clinical characteristics, and economic burden of diabetes across the past four decades in Korea. Nonetheless, there is a dearth of nationwide study regarding diabetes encompassing all age group. Eight years ago, the Committee on the Epidemiology of Diabetes Mellitus of Korean Diabetes Association collaborated with Health Insurance Review & Assessment Service to evaluate the status of diabetes care and characteristics in diabetic patients in Korea. In 2007, the collaborative task force team published a comprehensive survey titled "Diabetes in Korea 2007." In this review, we reappraise the diabetic epidemics from the joint report and suggest further studies that are needed to be investigated in the future.
Keywords: Diabetes mellitus, type 2; Epidemiology; Health Insurance Review & Assessment Service; Korea; National survey
INTRODUCTION
Diabetes is an important chronic disease causing economic and social burden around the world [1]. The prevalence of type 2 diabetes has substantially increased and is likely to continue to rise, particularly in developing areas including Asia [2].
In Korea, numerous studies on the prevalence, clinical characteristics and economic burden of diabetes has been performed across the past 40 years [3-7], which has recently extended to the evaluation of genomic features in diabetes. The prevalence of diabetes has increased 6- to 7-fold from 1.5% to 9.9%. Many well-designed population-based cohort studies, medical insurance data study, and reports on specific groups of patients, such as old age and gestational period, have been performed. Nonetheless, a nationwide study of diabetes including all age group is not yet common. Eight years ago, the Korean Diabetes Association (KDA) organized a Committee working on the epidemiology of diabetes mellitus to construct nationwide data about diabetes and its managements in Korea. In 2006, the Committee formed a collaborative agreement with Health Insurance Review & Assessment Service (HIRA), which is one of the several government agency collecting national health insurance data: since then, the name of the joint task force changed to Task Force Team for Basic Statistical Study of Korean Diabetes Mellitus (KDA-TFT for BSS) in 2006.
The strategies of KDA-TFT for BSS were to evaluate current status of diabetes and its managements, to establish a standard care and quality standard, to demonstrate the effect of systematic management about diabetes, and to develop a standard model of chronic disease management. This joint report consists of 1) the validity of health insurance data, 2) the prevalence, incidence, and clinical characteristics of diabetes, 3) complications and diabetes management, and 4) the health outcomes, use of healthcare service, and the cost of healthcare. We endeavored to obtain a comprehensive picture of diabetes from the national data on Korea [8-14].
VALIDITY OF HEALTH INSURANCE DATA
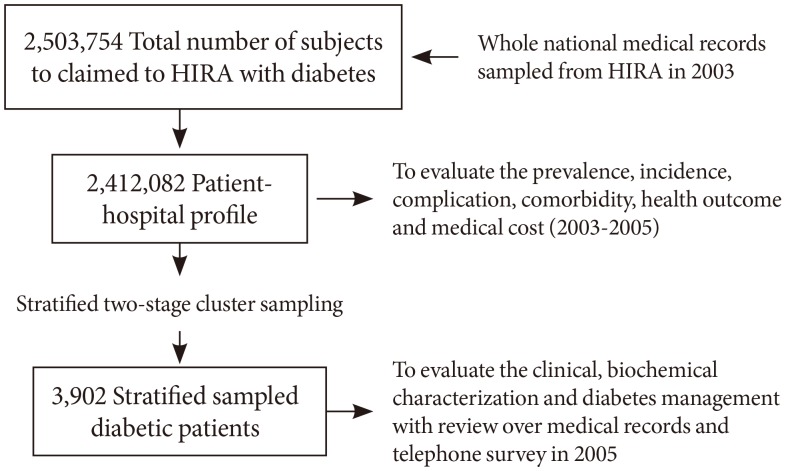
We constructed the profiles of diabetic patients (Fig. 1). First, we analyzed an approximately 250 million medical insurance claim database which has submitted at least once per year to HIRA with diabetes as a primary, secondary, or tertiary diagnostic codes in 2003 (ICD-10 code: E10 to E14). Diabetes was defined as those who have been prescribed diabetes medications between the year 2001 and 2003 or those who have fulfilled the diabetes diagnostic criteria (fasting blood glucose ≥126 or ≥200 mg/dL at a random or 2-hour postprandial blood glucose) on the medical record or those who were determined to be diabetic by physician. Using this database, we constructed a patient-hospital profile encompassing 3,676,164 cases and then transformed it to a patient profile consisting of 2,412,082 observations. The size of the total diabetic population was estimated by weighting the sample survey results. Second, we randomly selected 3,902 subjects out of 2,503,754 subjects with claims with diagnosis of diabetes between January 2003 and December 2003 by using a 2-staged cluster sampling method. Based on the evaluation of sampling design for estimating an epidemiologic volume of diabetes, we chose a target sample number of 4,000. Stratification was made into tertiary hospital:general hospital:hospital:clinic (5:10:10:75) and further into district, city, and county. It was identified that a two-stage cluster sampling with the first stage (random sampling of hospitals within a strata) and the second stage (random sampling of patients in the selected hospital) was accurate and efficient. Detailed sampling method was described in previous study [11].
Fig. 1.
Overview of the study. HIRA, Health Insurance Review & Assessment Service.
A field survey with review of medical records and telephone survey was conducted with standardized record forms developed by KDA-TFT for BSS. Finally, 1,088,564 patients with diagnosis of diabetes or records of diabetes drug prescription in 2002 aged 20 to 79 years old who survived until the end of year 2004 were included (1st nationwide survey).
The diagnosis validity was 87.2% (95% confidence interval [CI], 83.8% to 90.7%) for admission episodes and 72.3% (95% CI, 67.4% to 77.2%) for outpatient cases. In the analysis of the medical records of 3,902 patients sampled with the 2-stage cluster sampling from 2,412,082 patients for whom more than one claim was filed with diabetes, 62.7% (95% CI, 53.3% to 71.2%) was identified as diabetic by the diabetes patient eligibility criteria.
The health insurance data from HIRA is considered slightly less accurate than other research data in terms of substantiality or reliability. However, this is the only data including the entire national population. Such large-size population makes it the best tool available in predicting public health trends.
PREVALENCE AND INCIDENCE
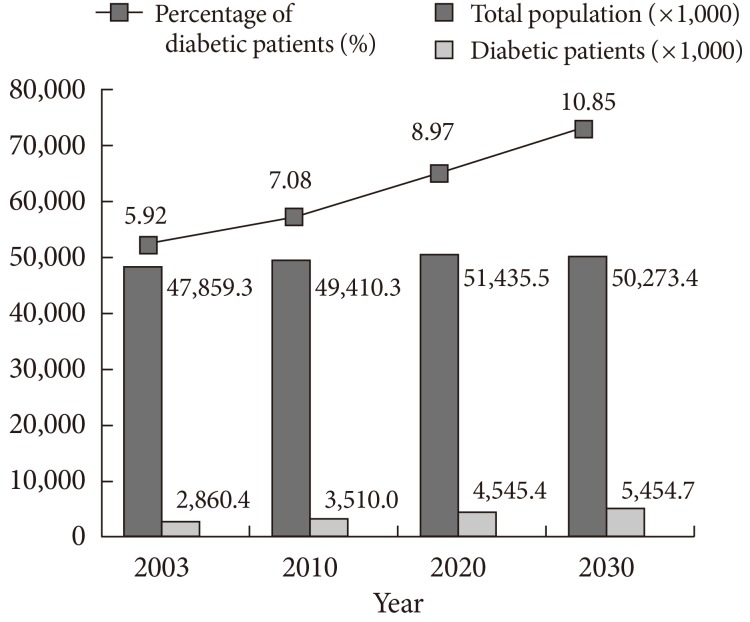
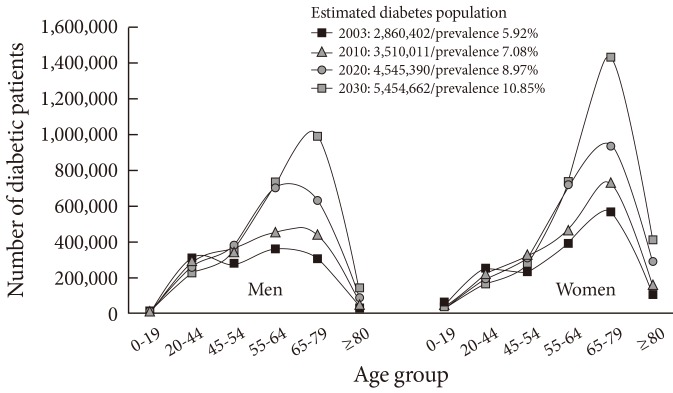
The prevalence of diabetes in the 2003 population was estimated to be 5.92% (n=2,860,402) of the total national population, with the proportion of 5.33% and 6.52% in men and women, respectively. The prevalence was 1.22 times higher in women. In the age group of 20 to 79 years, the prevalence was estimated at 7.7% (n=2,694,220). The present results are similar to other reports [5-7]. If the current trend in growth continues, the number of diabetic patients is likely to soar up to 3.51 million by the year 2010 (7.08% of the estimated total population), 4.55 million (8.97%) by 2020, and 5.45 million (10.85%) by 2030 (Figs. 2, 3). According to the International Diabetes Federation report, Korea ranked 21st among the 30 Organisation for Economic Co-operation and Development (OECD) member countries in terms of the adult (aged 20 to 79) diabetes prevalence. In our TFT results, diabetes prevalence in Korea is estimated to be ranked between 11th and 12th. If the growth rate continues at the current rate, however, Korea may have the highest prevalence of diabetes among the OECD countries by the year 2030.
Fig. 2.
Diabetic population estimates from 2003 to 2030 in Korea.
Fig. 3.
Diabetic population estimates factoring in age structure changes.
The incidence of diabetes (in the 2003 population) was estimated to be 0.57% (n=274,767) of the total population: 0.53% in men and 0.61% in women, respectively. The incidence was 1.16 times higher in women. In the age group of 20 to 79 years, the estimated incidence was 0.76% (n=262,735): 0.73% in men and 0.78% in women, respectively. It is estimated that the diabetic population size would rapidly increase by 10% each year in the future.
CLINICAL CHARACTERISTICS OF DIABETIC PATIENTS
To evaluate the clinical characteristics of diabetic patients, we used the results from the 1st nationwide survey. Patterns and correlations of healthcare use for 2 years (year 2003 and 2004) and outcomes (hospitalization, death, and medical cost) for the following year (2005) were analyzed. Outpatient visit continuance was defined as more than one visit per quarter (3 months) throughout the analysis period with diabetes as principal or secondary diagnosis. Income level was divided into five groups (20 percentile interval) by health insurance premium grades and actual premium amounts. Multivariate analysis was performed with adjustment for gender, age, premium level, residential location, the first year of diagnosis, comorbidities, previous year hospitalization, main healthcare institution of use, prescription continuance, number of institutions visited for outpatient care, and outpatient visit continuance during the previous year.
Our report shows that lower income level is associated with higher likelihood of hospitalization or death. They are also less likely to receive continuous outpatient care. The results show that a comprehensive healthcare service is necessary for low income patients. The 34.6% of the diabetic patients in this analysis had a family history (response rate, 62.7%). Body mass index (BMI) was used as a measurement of obesity. BMI <18.5 kg/m2 was measured in 3.4% of subjects, 18.5 to 24.9 kg/m2 in 57.2%, 25.0 to 29.9 kg/m2 in 34.2%, and ≥30 kg/m2 in 5.3%. Women had significantly higher BMI than men (24.7 kg/m2 vs. 24.2 kg/m2, P<0.05). The results suggest that 39.5% of diabetics in Korea are obese (BMI≥25 kg/m2), which is still a lower proportion compared with Western countries. Current and past smokers accounted for 26.7% and 12.7%, respectively, compared to 60.6% nonsmokers (response rate, 66.7%). Women had a higher percentage of nonsmokers compared with men (90.9% vs. 32.8%, P<0.001). The 41.3% of the diabetic patients consume one or more alcoholic beverages per month in this analysis. In men, this proportion was 61.5% as compared to 19.5% in women, suggesting a higher rate of alcohol drinking in men (response rate, 66.0%).
COMPLICATIONS
To evaluate the foot disease, end-stage renal disease (ESRD) and ophthalmologic disease, we chose subjects different from the aforementioned data. Foot amputated patients were defined as those who made the first claim in 2003 with code Z894-899 as principal or secondary diagnosis or who had the first record of N0571-N0575 between October 2000 and December 2002 in the health insurance claims data. Foot ulcer patients were defined as those who had the first record in 2003 with L97 (ulcer of lower limb) or R02 (gangrene) as principal or secondary diagnosis. ESRD prevalent patients were defined as those who had the record of chronic renal failure (N18 or N19) as principal or secondary diagnosis in their health insurance claims data between January 2001 and December 2003 and who received renal replacement therapy with one of the following disease classification codes; dialysis (Z49), dependence on renal dialysis (Z99.2), kidney transplant status (Z94.0), or with a specific disease code of V001 (hemodialysis), V003 (peritoneal dialysis), V005 (use of post kidney transplant immunosuppressants), or R3280 (renal transplantation). Renal transplant patients were defined as those with claims of any of the following codes: Z94.0, V005, and R3280. New ESRD incident patients were defined as ESRD patients first diagnosed during 2003.
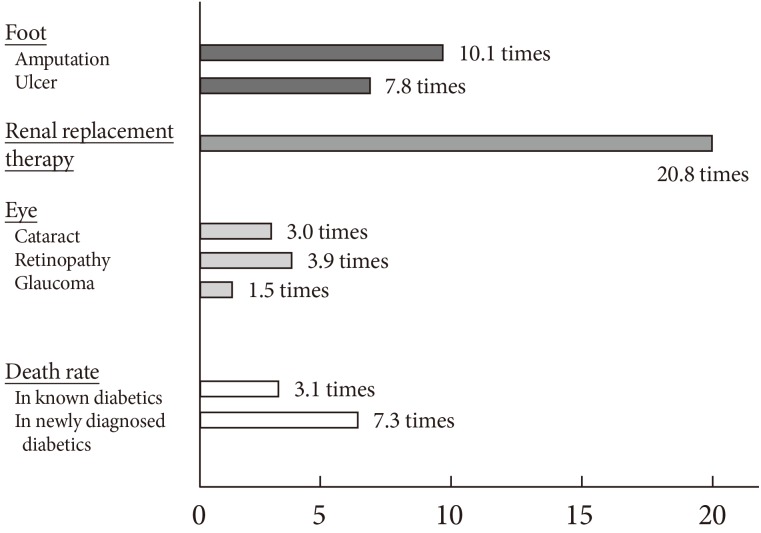
The 44.8% of the foot amputated patients in 2003 were diabetic. Diabetic patients were 10.1 times more likely to undergo foot amputation (4.7 times after standardization for gender and age), and 7.8 times more likely to have foot ulcer (4.4 times after the standardization). Depending on hospitalization/nonhospitalization, diabetic foot amputation was associated with 1.6 or 2.1 times more annual days of healthcare use than nondiabetic foot amputation. Diabetic foot ulcer was associated with 1.4 or 2.0 times more annual days of healthcare use. Depending on hospitalization/nonhospitalization, diabetic foot amputation was associated with 2.0 or 2.3 times higher total medical cost than nondiabetic foot amputation. Diabetic foot ulcer was associated with 1.7 or 3.2 times higher total medical cost. The results suggest that diabetes is a major underlying disease of foot diseases and that loss of human and/or financial resources to diabetic foot disease should not be underestimated.
Diabetes affected 56.7% of the total prevalent ESRD patients (n=41,167) in Korea in 2003. ESRD was 20.8-fold more common in diabetic patients than non-diabetics (Fig. 4). Of those who newly began renal replacement therapy in 2003, 70.5% were diabetics. Diabetic patients were 1.6 times more likely to be hospitalized due to ESRD for a longer duration compared with nondiabetics. They were also likely to suffer 1.6 times higher hospitalization cost. Ophthalmologic disease including cataract (3.0 times), retinopathy (3.9 times), and glaucoma (1.5 times) was 1.9-fold more common in diabetic patients than nondiabetics. Acute stroke was estimated to be 5.2-fold more common in diabetic patients compared to general population from the small case-control study (Fig. 4) [15]. The results suggest that compared to nondiabetics, complications among patients with diabetes are very common, becoming a heavier burden on the society and leading to a greater loss of human and/or financial resources.
Fig. 4.
Relative risk of comorbidities and health outcome compared with nondiabetics by simple comparison.
DIABETES MANAGEMENT
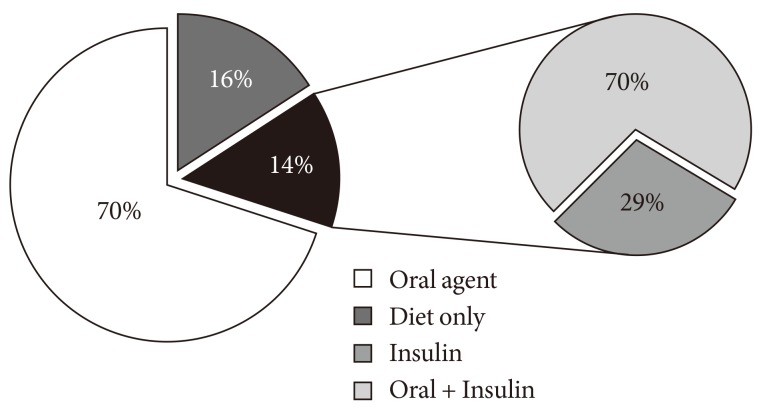
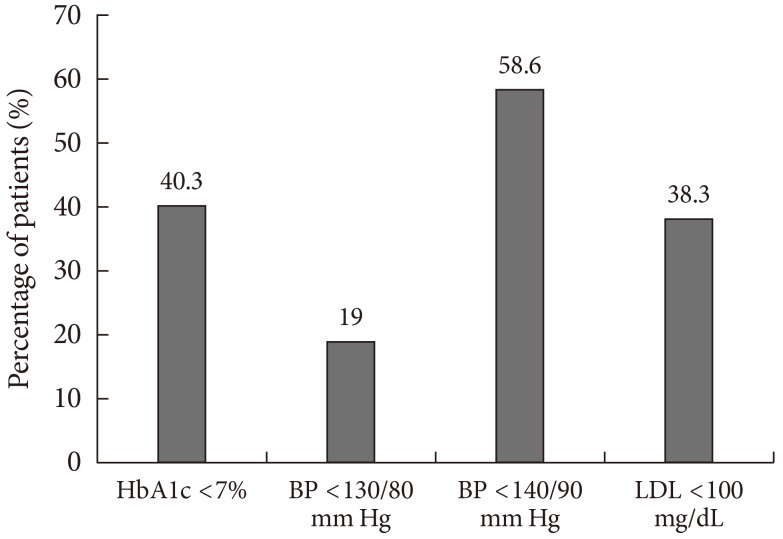
We analyzed the 1st nationwide survey data to evaluate the current status of diabetes management. The medical record fill-out rate for family history, smoking history, and drinking history in diabetes patients was low at about 10%, with tertiary hospitals showing the highest rate of record keeping. Basic tests including BMI (18.0% measured over 6 months), blood pressure (56% over 6 months), lipid profile (46.3% over 1 year), and foot examination (6.1% over 2 years) in diabetes patients were being performed in a low portion of the patients. When classified by the type of health institutions, tertiary hospitals showed the highest test rate, followed by general hospitals, hospitals, and clinics. Blood glucose was self-monitored in 34.9% of the subject patients. The 39.4% received education for diabetes management at least once while 60.6% never received such education. Diabetes was treated with oral hypoglycemics alone in 70.0%, with insulin alone in 4.1%, with combination therapy of oral agents and insulin in 10.1%, and with diet/exercise in 15.8% of the patients (Fig. 5). Nonetheless, only 40.3% had their blood glucose controlled to glycated hemoglobin (HbA1c) <7%. These results on treatment methods or control rate were similar to the reports in the 2005 Korea National Health and Nutrition Examination Survey, where HbA1c <7% was observed in 43.5% of the subjects. The 63% of the adult diabetic patients aged 20 to 79 years received antihypertensive medications for more than 1 day a year. While 86.5% of the diabetic patients with comorbid hypertension were taking antihypertensives, blood pressure of <140/90 mm Hg was achieved in 59% and <130/80 mm Hg in only 19%. Similarly, 70.2% of the diabetic patients with comorbid hyperlipidemia received lipid-lowering agents, but only 38% achieved low density lipoprotein-cholesterol of <100 mg/dL (Fig. 6). Only 21.8% of the subject patients took medications for diabetes on a continuous basis (more than 360 days a year). Of the patients with newly diagnosed diabetes in 2003, 36.2%, and 13.2% were taking antihypertensives and lipid-lowering agents, respectively. On the other hand, the percentage of the patients concomitantly taking aspirin was low at 11.6%, which lower than the proportion reported in the United States. These results indicate that current diabetes treatment is not yet aggressive enough.
Fig. 5.
Blood glucose control methods in the diabetes-eligible patients.
Fig. 6.
Percentage of patients achieving treatment targets (%). HbA1c, glycated hemoglobin; BP, blood pressure; LDL, low density lipoprotein cholesterol.
HEALTH OUTCOME
We reviewed the 1st nationwide survey data to evaluate the death outcome. The 1-, 2-, and 3-year mortality in the diabetes-eligible patients was estimated to be 3.95%, 5.89%, and 8.52%, respectively. In the incident diabetes patients (new patients), the same year mortality was 1.5 to 2 times higher at 7.56%, 9.70%, and 13.11%, respectively. Overall, the mortality due to diabetes was higher in men than women, in newly diagnosed patients than in established patients, and in the age group of 45 to 54 years than the age group of 55 to 64 years. When standard mortality ratio was generated for comparison with the general population, the ratio of diabetes-eligible patients was 3.1, 2.4, and 2.2 at 1, 2, and 3 years, respectively, showing that the gap between the two populations decreased over time. The mortality ratio of the incident diabetes patients was 7.3, 4.9, and 4.2 at 1, 2, and 3 years, respectively, also showing decreasing trend over time. These results suggest that mortality in diabetes patients is 3.1-fold higher than in the general population. The newly diagnosed patients, in particular, shows 7.3-fold higher mortality (adjusted for gender and age difference) (Fig. 4).
USE OF HEALTHCARE SERVICE AND THE COST
The total number of diabetes patients in 2003 was estimated at 2.86 million. Among them, only 52.9% used healthcare service for diabetes at least once a year (48.0% in women, 58.8% in men).
The annual rate of hospitalization in diabetes patients was 10.3%, with an average of 22.4 hospitalization day per year. Patients who received outpatient care made an average of 12.2 visits to health institutions per year. The total medical cost in the adult diabetes patients (aged 20 to 79 years) was 3,185 billion KRW, accounting for about one-fifth (19.2%) of the total cost in the entire adult population. The total medical cost per person in the diabetes patients was 4.6 times higher than the general population. The gap narrowed to a 3-fold difference after adjusting for gender and age. The number of patients who filed insurance claims for diabetes increased by 2.9-fold across a decade, from 800,000 (1.8% of the entire population) in 1995 to 2.33 million (4.8%) in 2005. During the same period, the total medical cost in the patients with diabetes (as principal or secondary diagnosis) increased by as much as 7.99-fold, from 214 billion KRW in 1995 to 1,712 billion KRW in 2005. This large increase was attributable to the increase in the per-capita healthcare service utilization rate to treat diabetes (responsible for 2.09-fold or 35.5% of the increase), population aging (1.40-fold or 16.1%) the increase in healthcare service price index (1.85-fold or 29.7%), and net cost growth after adjustment for the price index (1.48-fold or 18.7%).
These results suggest that the economic burden of diabetes and its management is serious.
CONCLUSIONS
The limitation of this report lies in the inaccuracy of ICD-10 diagnosis code of diabetes. Therefore, the validity of health insurance data is relatively low compared to other well-designed controlled studies. However, we performed face to face field study and telephone survey to randomized samples to overcome the limitation. Despite the slightly low validity, this is the only data to encompass the entire national population. The large size population makes it the best available tool available in foreseeing public health trends.
The prevalence and incidence of diabetes in Korea are predicted to increase until up to year 2030, and the national economic burden subsequently become heavier in the future. A comprehensive effort aiming to decrease the economic burden and comorbidities of diabetes is necessary.
ACKNOWLEDGMENTS
We thank the Health Insurance Review & Assessment Service and all the members of Korea Diabetes Association.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care. 2004;27:1047–1053. doi: 10.2337/diacare.27.5.1047. [DOI] [PubMed] [Google Scholar]
- 2.Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681–1688. doi: 10.1016/S0140-6736(06)69703-1. [DOI] [PubMed] [Google Scholar]
- 3.Kim DJ. The epidemiology of diabetes in Korea. Diabetes Metab J. 2011;35:303–308. doi: 10.4093/dmj.2011.35.4.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cho NH. The epidemiology of diabetes in Korea: from the economics to genetics. Korean Diabetes J. 2010;34:10–15. doi: 10.4093/kdj.2010.34.1.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park Y, Lee H, Koh CS, Min H, Yoo K, Kim Y, Shin Y. Prevalence of diabetes and IGT in Yonchon County, South Korea. Diabetes Care. 1995;18:545–548. doi: 10.2337/diacare.18.4.545. [DOI] [PubMed] [Google Scholar]
- 6.International Diabetes Federation; World Diabetes Foundation. Diabetes atlas. 2nd ed. Brussels: International Diabetes Federation; 2003. [Google Scholar]
- 7.Korea Centers for Disease Control and Prevention. In-depth analyses for diabetes with data of the 3rd Korea National Health and Nutrition Examination Survey (2005) Cheongwon: Korea Centers for Disease Control and Prevention; 2007. pp. 158–204. [Google Scholar]
- 8.Task Force Team for Basic Statistical Study of Korean Diabetes Mellitus. Report of task force team for basic statistical study of Korean diabetes mellitus: diabetes in Korea 2007. 1st ed. Seoul: Goldfishery; 2007. [Google Scholar]
- 9.Park SW, Kim DJ, Min KW, Baik SH, Choi KM, Park IB, Park JH, Son HS, Ahn CW, Oh JY, Lee J, Chung CH, Kim J, Kim H. Current status of diabetes management in Korea using National Health Insurance Database. J Korean Diabetes Assoc. 2007;31:362–367. [Google Scholar]
- 10.Park IB, Kim DJ, Kim J, Kim H, Min KW, Park SW, Park JH, Son HS, Ahn CW, Oh J, Lee S, Lee IB, Lee J, Chung CH, Choi I, Choi KM, Baik SH. Joint research of Korean Diabetes Association-Health Insurance Review and Assessment Service 2004-2007. Clin Diabetes. 2007;8:356–360. [Google Scholar]
- 11.Lee JS, Kim J, Baik SH, Park IB, Lee J. An evaluation of sampling design for estimating an epidemiologic volume of diabetes and for assessing present status of its control in Korea. J Prev Med Public Health. 2009;42:135–142. doi: 10.3961/jpmph.2009.42.2.135. [DOI] [PubMed] [Google Scholar]
- 12.Kim DJ, Kim J, Kim H, Min KW, Park SW, Park IB, Park JH, Baik SH, Son HS, Ahn CW, Oh JY, Lee S, Lee J, Chung CH, Choi KM, Choi I, Kim H. Current status of diabetic end-stage renal disease using Korean Health Insurance database. J Korean Diabetes Assoc. 2006;30:355–362. [Google Scholar]
- 13.Chung CH, Kim DJ, Kim J, Kim H, Kim H, Min KW, Park SW, Park JH, Baik SH, Son HS, Ahn CW, Oh JY, Lee S, Lee J, Choi KM, Choi I, Park IB. Current status of diabetic foot in Korean patients using National Health Insurance database. J Korean Diabetes Assoc. 2006;30:372–376. [Google Scholar]
- 14.Kim J, Kim H, Kim H, Min KW, Park SW, Park IB, Park JH, Baik SH, Son HS, Ahn CW, Oh JY, Lee S, Lee J, Chung CH, Choi KM, Choi I, Kim DJ. Current status of the continuity of ambulatory diabetes care and its impact on health outcomes and medical cost in Korea using National Health Insurance database. J Korean Diabetes Assoc. 2006;30:377–387. [Google Scholar]
- 15.Kim J. Construction of national surveillance system for cardiovascular & cerebrovascular diseases. Seoul: Health Insurance Review & Assessment Service; 2006. [Google Scholar]