Abstract
Background
Doxorubicin (DOXO) is an effective anthracycline chemotherapeutic, but its use is limited by cumulative dose-dependent cardiotoxicity. Neuregulin-1β (NRG1B) is an ErbB receptor family ligand that is effective against DOXO-induced cardiomyopathy in experimental models but is also pro-neoplastic. We previously showed that an engineered bivalent neuregulin-1β (NN) has reduced pro-neoplastic potential compared to the epidermal growth factor (EGF)-like domain of NRG1B (NRG), an effect mediated by receptor biasing towards ErbB3 homotypic interactions uncommonly formed by native NRG1B. Here, we hypothesized that a newly formulated, covalent NN would be cardioprotective with reduced pro-neoplastic effects compared to NRG.
Methods and Results
NN was expressed as a maltose-binding protein fusion in E. coli. As established previously, NN stimulated anti-neoplastic or cytostatic signaling and phenotype in cancer cells, whereas NRG stimulated pro-neoplastic signaling and phenotype. In neonatal rat cardiomyocytes (NRCM), NN and NRG induced similar downstream signaling. NN, like NRG, attenuated the double-stranded DNA breaks associated with DOXO exposure in NRCM and human cardiomyocytes derived from induced pluripotent stem cells. NN treatment significantly attenuated DOXO-induced decrease in fractional shortening as measured by blinded echocardiography in mice in a chronic cardiomyopathy model (57.7% ± 0.6% vs. 50.9% ± 2.6%, P=0.004), whereas native NRG had no significant effect (49.4% ± 3.7% vs. 50.9% ± 2.6%, P=0.813).
Conclusions
NN is a cardioprotective agent that promotes cardiomyocyte survival and improves cardiac function in DOXO-induced cardiotoxicity. Given the reduced pro-neoplastic potential of NN versus NRG, NN has translational potential for cardioprotection in cancer patients receiving anthracyclines.
Keywords: anthracycline, cardioprotection, protein engineering, translational cancer therapy, therapeutic protein
The anthracycline doxorubicin (DOXO) is a widely used chemotherapeutic that is particularly efficacious against the subset of breast cancers that overexpress the ErbB2 (HER2) receptor1. Limiting its clinical use, however, is a cumulative dose-related cardiotoxicity characterized by left ventricular dysfunction that can ultimately culminate in congestive heart failure2. Oncologists now limit dosage of DOXO, and thus DOXO-induced cardiomyopathy is no longer a widespread clinical problem. However, this dose limitation is potentially deleterious for cancer patients for whom DOXO is the most effective therapy. Therefore, approaches to mitigate the cardiotoxic effects of DOXO to enable increased dosing to combat malignancies remain an unmet clinical need.
Sawyer and others have described the potential of Neuregulin-1β (NRG1B), a ligand of the ErbB receptor family, for therapeutic application against DOXO-induced cardiotoxicity3-8. NRG1B binds ErbB3 and ErbB4, predominantly inducing heterotypic interactions with ErbB2, which has no known ligand9. ErbB2 and ErbB4, but not ErbB3, are expressed in the postnatal heart, and are both critical for cardiac development and cardiac function3. NRG1B, a key mediator of endothelial-cardiomyocyte crosstalk9-11, has been shown to protect ventricular myocytes from anthracycline-induced apoptosis5-7. Systemic administration of the epidermal growth factor (EGF)-like domain of NRG1B (NRG) leads to improved survival in animal models of ischemic, viral, and dilated cardiomyopathy6 and has demonstrated cardioprotective efficacy in clinical trials12.
However, despite its efficacy, NRG is not clinically relevant as a therapeutic for DOXO-induced cardiomyopathy due to its well-established role in pro-neoplastic signaling13-16. We have previously designed an engineered bivalent neuregulin-1β (NN) that demonstrates reduced pro-neoplastic potential compared to NRG17. Whereas NRG is widely reported to participate in malignant signaling pathways via induction of ErbB2/3 heterotypic interactions13-16, NN biases signaling away from these and towards ErbB3 homotypic interactions in high ErbB3- and low ErbB4-expressing cancer cells17. Because ErbB3 is a very weak18 or inactive19 kinase, ErbB3 homotypic interactions can result in a cytostatic or anti-neoplastic phenotype17.
If NN retains similar cardioprotective properties compared to NRG without the pro-neoplastic properties of NRG, then NN could represent a more translationally relevant therapy for DOXO-induced cardiomyopathy. We hypothesized that NN would promote cardioprotection in a manner similar to NRG, provided that NN-induced biasing to exclude ErbB2 participation in cardiomyocyte signaling was not extreme. Although the role of ErbB2 in chemotherapy-related cardiotoxicity remains unclear, substantial inhibition of ErbB2 signaling may impair cardiac function, as observed in patients receiving concurrent treatment with anthracyclines and the ErbB2 antibody trastuzumab2, 20. We tested the stated hypothesis in vitro in rat and human cardiomyocytes and in vivo in randomized and blinded mouse models of acute and chronic DOXO-induced cardiomyopathy. Our results indicate that NN induces anti-neoplastic or cytostatic responses in cancer cells that are stimulated toward known malignant signaling pathways and phenotypes by NRG – endowing NN with a reduced pro-neoplastic profile compared to NRG – and that NN is cardioprotective, working through similar mechanisms as NRG, and holds promise as a novel therapeutic for cancer patients receiving anthracyclines.
METHODS
Protein Design and Purification
The amino acid sequence for NN comprises two NRG domains separated by a hydrophilic, protease-resistant spacer (Figure 1A). The full sequence of NN is as follows: SHLVKCAEKEKTFCVNGGECFMVKDLSNPSRYLCKCPNEFTGDRCQNYVMASFYKHLGIEFMEAEASGAGGSEGGGSEGGTSGATASGAGGSEGGGSEGGTSGATASGAGGSEGGGSEGGTSGATGGSHLVKCAEKEKTFCVNGGECFMVKDLSNPSRYLCKCPNEFTGDRCQNYVMASFYKHLGIEFMEAE. Additional information is available in the Online-only Data Supplement.
Figure 1.
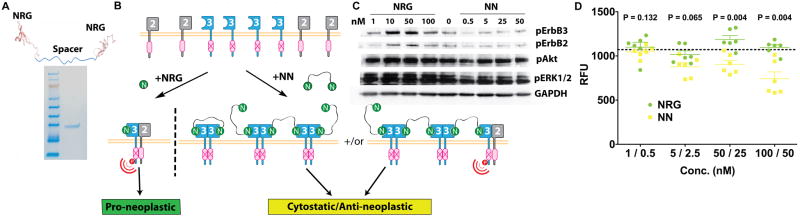
Design of covalently linked bivalent neuregulin-1β (NN) and validation of its reduced pro-neoplastic potential compared to neuregulin-1β (NRG). (A) NN was produced via covalent linkage of two NRG domains separated by a flexible, protease-resistant spacer. Purity was indicated by Coomassie-stained gel. (B) Schematic of expected differential ErbB receptor complexation induced by NRG compared with NN in doxorubicin-sensitive breast cancer cells expressing ErbB2 and ErbB3. NRG is predicted to predominantly promote ErbB2/3 heterotypic interactions whereas NN is predicted to induce increased ErbB3 homotypic interactions. (C) Immunoblot analysis of ErbB2, ErbB3, Akt, and ERK1/2 phosphorylation in lysates from doxorubicin-sensitive human mammary ductal carcinoma cell line MDA-MB-175VII stimulated for 15min by NRG or NN. GAPDH expression was measured as a loading control. Data are representative of 3 independent experiments. (D) Cell number was assessed by measurement of DNA content via fluorescence (CyQUANT assay, ex = 485nm, em = 530nm) following stimulation of MDA-MB-175VII cells by control media (indicated by dashed line) or the indicated doses of NRG (left of slash) or NN (right of slash) (n=6). P values were calculated using a Wilcoxon rank-sum test. RFU = relative fluorescence units.
Immunoblot and proteomic array analyses, cell culture procedures, and in vitro functional assays are described in the Online-only Data Supplement. Molecules used for stimulation included DOXO (doxorubicin hydrochloride, Sigma-Aldrich, solubilized in sterile saline), NRG (EGF-like domain, Peprotech) or NN. In general, NN was used at one-half the molar dose of NRG because NN contains two NRG domains; therefore this dosing scheme should result in approximately equivalent doses.
In Vivo Studies
Two different randomized and blinded mouse models of DOXO-induced cardiomyopathy, acute and chronic, were used. For the acute model, 8-12-week-old male C57BL/6 mice (total of 33, Charles River) were administered a single DOXO injection (20mg/kg intraperitoneal (ip); Sigma-Aldrich). Selections of DOXO dose and route of administration were based on previous studies7, 21. NRG (100μg/kg ip) or NN (100μg/kg ip) was administered daily starting 3d before and for 4d following DOXO administration. The timing and dosage of treatment injections were based on a previous study7. Controls were treated with vehicle (0.2% bovine serum albumin in PBS) only. Baseline echocardiography was performed on all animals two days prior to initial treatment injection and animals were randomized into groups based on fractional shortening (FS) values. Blinded echocardiography was performed after final treatment injection. Mice were anesthetized with pentobarbital (30-70 mg/kg). The left ventricle (LV) was imaged in the short-axis view at the mid-papillary muscle, and two-dimensional measurements of LV end-diastolic diameter (LVEDD) and LV end-systolic diameter (LVESD) were recorded. FS was then calculated (FS = (100*(LVEDD-LVESD)/LVEDD)). Heart rates were determined using M-mode images. Animals were sacrificed following final echocardiogram and hearts excised and flash frozen prior to thawing and homogenization in lysis buffer for immunoblot analysis.
For the chronic model, 8-12-week-old female C57BL/6 mice (total of 44, Charles River) were administered serial DOXO injections (4mg/kg intraperitoneal (ip); Sigma-Aldrich). Mice were injected once weekly for 5 consecutive weeks at the initiation of the study (weeks 0-4) and then again for 5 weeks beginning 16 weeks after the initial injection (weeks 16-20). Selection of DOXO dose and route of administration was based on a previous study22. NRG (50μg/kg ip) or NN (50μg/kg ip) was administered daily for 1 week starting on the day of the first DOXO injection (week 0) and again daily for 1 week during week 16. Vehicle-only treated animals were used as controls (0.2% bovine serum albumin in PBS). Animals were randomized as in the acute model. Blinded echocardiography was performed 6, 12, 22, and 24 weeks after initial DOXO injection. Anesthesia and analysis were identical to those used in the acute model. Animals were sacrificed following final echocardiogram and hearts were excised and fixed in 4% paraformaldehyde overnight prior to dehydration, rehydration, and fixation in paraffin by standard methods. 5μm sections were cut and stained with hematoxylin and eosin or Masson’s trichrome. All animal protocols were approved by the Harvard IACUC and performed in an AALAC-certified facility.
Statistical Analysis
All data are shown as mean ± s.e.m. unless stated. Statistical significance was calculated using non-parametric analyses as indicated in the figure legends. Additional information is available in the Online-only Data Supplement.
RESULTS
Design of Covalently-Linked NN and Validation of its Reduced Pro-Neoplastic Potential Compared to NRG
We previously reported the development of bivalent ligands consisting of a non-covalent linkage of two monomeric receptor-binding domains separated by a flexible, protease-resistant spacer and a high-affinity coiled-coil domain17. In order to reduce the possibility for dissociation of ligands and thereby promoting the potential for clinical translation, a new covalently linked NN was engineered without a coiled-coil domain and with a corresponding increase in the length of the spacer (Figure 1A). Purity of the final product was verified by observation of a single band on a Coomassie-stained gel (Figure 1A).
Binding of NRG1B to ErbB3 and the subsequent formation of ErbB2/3 heterotypic interactions are associated with pro-neoplastic signaling in a wide range of cancers, including DOXO-sensitive breast cancers14, 16, 23. We previously demonstrated that NN promotes sequestration of ErbB3 into weak/non-signaling homotypic interactions, resulting in a cytostatic or anti-neoplastic phenotype17 (summarized schematically in Figure 1B). Here we used the DOXO-sensitive, human mammary ductal carcinoma cell line MDA-MB-175VII24, which is stimulated by a Neuregulin-1 autocrine loop whereby ErbB2 and ErbB3 are phosphorylated25, 26, to assess whether NN would exhibit reduced pro-neoplastic characteristics compared to native NRG. When stimulated for 15min with NRG, MDA-MB-175VII cells exhibited dose-dependent phosphorylation of ErbB2 and ErbB3, as expected (Figure 1C). Stimulation with NN for 15min, on the other hand, resulted in levels of phospho-ErbB2 and phospho-ErbB3 that were lower than or similar to control levels, even at the highest tested doses of NN (Figure 1C). Furthermore, phosphorylation of downstream effectors Akt and ERK1/2 – known mediators of proliferation, migration, and survival in cancer cells – was also modestly increased upon stimulation by NRG but unchanged or decreased by stimulation with NN compared to control levels (Figure 1C). Additionally, NRG stimulation promoted maintenance or growth of MDA-MB-175VII, whereas stimulation with an equivalent dosage of NN resulted in reduced cell viability compared to native NRG at dosages at or above 50nM (Figure 1D). Thus, these data confirm the bioactivity of NN and reinforce its reduced pro-neoplastic potential as compared to NRG in DOXO-sensitive breast cancer cells17.
NN Stimulates ErbB Receptor Phosphorylation on Cardiomyocytes
Given the well-established roles for NRG in cardioprotection6, 11, 27-30 and as a potential therapy for DOXO-induced cardiomyopathy3-8, we wanted to test whether NN, with its reduced pro-neoplastic potential compared to NRG, stimulated cardioprotective signaling in a manner similar to NRG. Postnatal cardiomyocytes express ErbB2 and ErbB4, but not ErbB39. ErbB4, unlike ErbB3, has a fully active kinase domain and can participate in signaling when complexed with either ErbB2 or ErbB49. NRG stimulation of cardiomyocytes results predominantly in the formation of ErbB2/4 heterotypic interactions9, initiating downstream signaling (Figure 2A). We predicted that NN stimulation would induce biasing away from ErbB2/4 interactions towards ErbB4 homotypic interactions, which would result in active downstream signaling which may or may not differ from that induced by ErbB2/4 interactions (Figure 2A).
Figure 2.
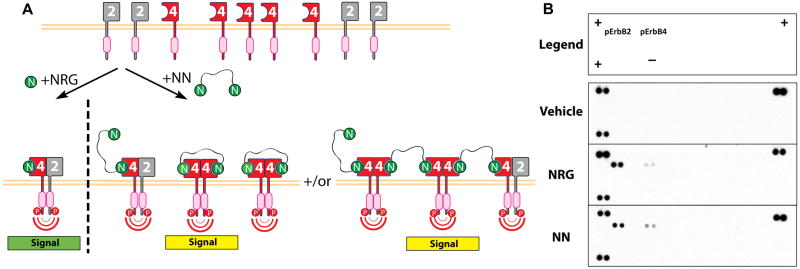
Bivalent neuregulin-1β (NN) stimulates ErbB receptor phosphorylation on cardiomyocytes. (A) Schematic of expected differential ErbB receptor complexation induced by neuregulin-1β (NRG) compared with NN on cardiomyocytes. NRG is predicted to predominantly promote formation of ErbB2/4 heterotypic interactions whereas NN is predicted to induce increased ErbB4 homotypic interactions. (B) Phospho-receptor tyrosine kinase array analysis of neonatal rat cardiomyocytes stimulated for 15min by 10nM NRG or NN or serum-free media (Vehicle). Data are representative of 3 independent experiments. Legend indicates relative locations of positive control (+), negative control (-), phospho-ErbB2 (pErbB2) and phospho-ErbB4 (pErbB4) spots on array membrane.
In order to assess the effect of NN on ErbB receptor phosphorylation on cardiomyocytes, NRCM were stimulated for 15min with either 10nM of NRG or NN and lysates were analyzed using phospho-receptor tyrosine kinase arrays that enabled simultaneous evaluation of phosphorylation of all ErbB receptors. Stimulation with NN resulted in apparent increased ErbB4 phosphorylation and decreased ErbB2 phosphorylation as compared to NRG, although ErbB2 phosphorylation still occurred with NN stimulation (Figure 2B). Thus, we established that while NN stimulation results in ErbB receptor phosphorylation on cardiomyocytes consistent with the generation of increased ErbB4 homotypic interactions compared to stimulation with NRG, inhibition of ErbB2 phosphorylation is not extreme.
NN Induces Intracellular Signaling Similar to NRG and Phosphorylates Known Mediators of Cardioprotection
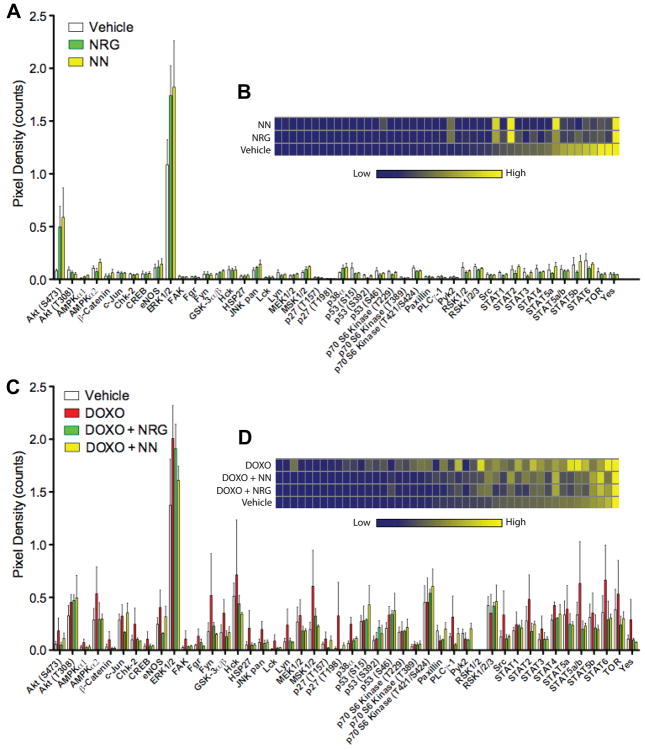
To assess whether ErbB receptor phosphorylation on cardiomyocytes associated with NN induced different downstream signaling compared to NRG, NRCM lysates prepared using the same conditions as described for Figure 2 were analyzed with intracellular phospho-kinase arrays (Figure 3). Array analysis revealed substantial phosphorylation of Akt (S473) and ERK1/2, known mediators of cardioprotective effects5, 7, 27, at similar levels for both NRG and NN stimulation (Figure 3A). Overall, no significant difference between NRG-treated cells and NN-treated cells was observed (Figure 3B). The same analysis was performed on lysates made 24h following stimulation by proteins or control media in the presence of 1μM DOXO. A distinction between the signaling profiles of NRCM stimulated with control media with DOXO (DOXO) and without DOXO (Control) was evident (Figures 3C,D). NRCM stimulated with DOXO and NRG (DOXO + NRG) or DOXO and NN (DOXO + NN) had profiles that were generally more similar to Control – indicative of cardioprotective signaling – and that did not vary from each other in a statistically significant way (Figures 3C,D). Additional analyses of Akt and ERK1/2 phosphorylation at different doses and time points revealed no significant differences between NRG- and NN-induced effects. Overall, these data support the conclusions that NN is capable of inducing canonical cardioprotective signaling in cardiomyocytes and that downstream signaling induced by NN is similar to that induced by NRG in vitro in cardiomyocytes.
Figure 3.
Bivalent neuregulin-1β (NN) induces intracellular signaling similar to NRG and phosphorylates known mediators of cardioprotection. (A) Expression data from phospho-kinase array of neonatal rat cardiomyocytes (NRCM) stimulated for 15min by 50nM NRG or 25nM NN, Vehicle = serum-free media (n=3). (B) Pathway analysis of data from (A) demonstrates similar protein phosphorylation patterns induced by NN and NRG. Data were thresholded to y-axis=0.20 and displayed in order of relative expression in Vehicle group from low to high as indicated. (C) Expression data from phospho-kinase array of neonatal rat cardiomyocytes (NRCM) stimulated for 24h by 50nM NRG or 25nM NN concurrently exposed to 1μM doxorubicin (DOXO), Vehicle = serum-free media, (n=3). (D) Pathway analysis of data from (C) demonstrates differential protein phosphorylation stimulated by DOXO compared to Vehicle. NN + DOXO and NRG + DOXO induced similar patterns that indicate significant regulation of numerous factors from their DOXO-induced state towards the Vehicle state, indicative of cardioprotective signaling. Data were thresholded to y-axis=0.75 and displayed in order of relative expression in Vehicle group from low to high as indicated.
NN is Cardioprotective from DOXO In Vitro
Because stimulation with NRG or NN resulted in similar downstream signaling profiles, we hypothesized that NN would retain similar cardioprotective qualities to NRG in the setting of DOXO-induced toxicity. To test this, we assessed phenotype and signaling in response to DOXO exposure. Stimulation with 100nM NRG in the presence of 1μM DOXO resulted in a significant increase in NRCM viability as compared to DOXO-only treated cells, as expected (Figure 4A, P=0.013). Surprisingly, stimulation with 50nM NN resulted in significantly greater preservation of NRCM viability compared to an approximately equivalent dosage of 100nM NRG (Figure 4A, P=0.038). Additionally, stimulation with 25nM of NN significantly reduced NRCM apoptosis associated with DOXO, and did so more effectively than stimulation with 50nM of NRG (Figure 4B, P=0.002). Taken together, these data indicate that NN is cardioprotective from DOXO in vitro with comparable or enhanced potency as compared to NRG.
Figure 4.
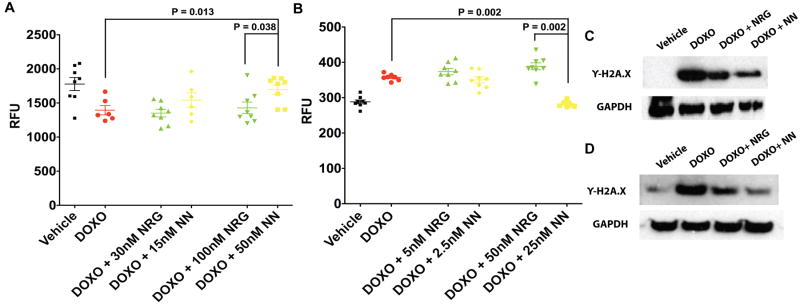
Bivalent neuregulin-1β (NN) has similar cardioprotective qualities to neuregulin-1β (NRG) in vitro. (A) Neonatal rat cardiomyocytes (NRCM) were exposed to 1μM doxorubicin (DOXO) and were stimulated with the indicated concentrations of NRG or NN in serum-free conditions for 24h. The control condition was NRCM in serum-free media (Vehicle). Cell viability was quantified via fluorescence (CyQUANT assay, ex = 485nm, em = 530nm) (n=8). (B) Presence of cleaved caspase-3/7 was assessed in NRCM after exposure to 1μM DOXO and stimulation with NRG or NN for 24h via fluorescence (SensoLyte assay, ex = 354nm, em = 442nm) (n=8). The control condition was NRCM in serum-free media (Vehicle). For A and B, P values were determined using a Wilcoxon rank-sum test with a Bonferroni correction following an initial Kruskal-Wallis test to determine statistical significance; data are representative of at least 2 independent experiments; RFU = relative fluorescence units. (C) Immunoblot analysis of γ-H2A.X in NRCM stimulated with NRG (100nM) or NN (50nM) concurrently exposed to 1μM DOXO for 24h. NRCM were incubated with treatments for 24h prior to DOXO addition (48h total treatment time). (D) Immunoblot analysis of γ-H2A.X in human induced pluripotent stem cell-derived cardiomyocytes (iPSC-CM) stimulated with NRG (100nM) or NN (50nM) concurrently exposed to 10μM DOXO for 24h. iPSC-CM were incubated with treatments for 24h prior to DOXO addition (48h total treatment time). For C and D, GAPDH expression was assessed as a protein loading control, data are representative of 3 independent experiments, and the control condition was NRCM in serum-free media (Vehicle).
One validated mechanism for the cardiotoxicity of DOXO is the generation of double stranded-DNA breaks (DSDBs), ultimately leading to cell death31. Phosphorylation of the histone H2A.X, which yields γ-H2A.X, occurs in response to DSDBs and is a very early indicator of DNA damage32. Exposure of NRCM to 1μM DOXO and of human induced pluripotent stem cell-derived cardiomyocytes (iPSC-CM) to 10μM DOXO resulted in increased γ-H2A.X signal (Figures 4C,D). The increase in γ-H2A.X was similarly attenuated when stimulated with approximately equivalent concentrations of NRG (100nM) or NN (50nM) (Figures 4C,D). Thus the cardioprotective effect of both NRG and NN may be explained by an attenuation of the DSDBs induced by DOXO.
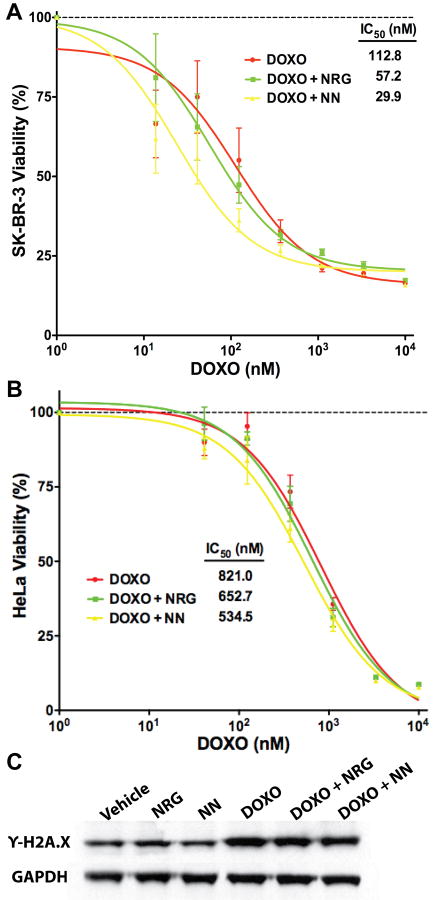
NN Does Not Interfere with DOXO Activity on Anthracycline-Sensitive Cancer Cells
One possibility for the apparent effects of NN in counteracting DOXO-induced cardiomyocyte toxicity is non-specific interference with DOXO by NN. To examine whether NN interfered with the cytotoxic action of DOXO, DOXO-sensitive mammary adenocarcinoma line SK-BR-3 cells and HeLa cells were concurrently exposed to increasing doses of DOXO and a static dose of either 50nM NRG or 25nM NN. NN did not interfere with the cytotoxic action of DOXO at the assessed doses, indicating that the protective effects of NN on cardiomyocytes were not the result of inactivation of DOXO (Figures 5A,B). Additionally, γ-H2A.X expression was unchanged in HeLa cells concurrently exposed to DOXO and NRG or NN (Figure 5C), further supporting the conclusion that NN does not interfere with DOXO activity and thus that any effects observed in cardiomyocytes are likely the result of stimulation of ErbB receptors and not of non-specific DOXO inhibition.
Figure 5.
Bivalent neuregulin-1β (NN) does not interfere with doxorubicin (DOXO) activity on anthracycline-sensitive cancer cells. (A) Mammary adenocarcinoma line SK-BR-3 cells were concurrently exposed to DOXO at the indicated concentrations and stimulated with 50nM NRG or 25nM NN. Cell viability relative to control (serum-free media; 100%) was quantified via fluorescence (CyQUANT assay, ex = 485nm, em = 530nm) (n=5, data are representative of 3 independent experiments). IC50 values were calculated based on the best-fit line generated with GraphPad Prism software. (B) Identical experimental conditions were used with HeLa cells. (C) HeLa cells were exposed to serum-free media (Vehicle) with or without 1μM DOXO for 24h with concurrent stimulation by 50nM NRG or 25nM NN as indicated and immunoblot analysis of γ-H2A.X was performed on lysates. GAPDH expression was assessed as a protein loading control. Data are representative of 3 independent experiments.
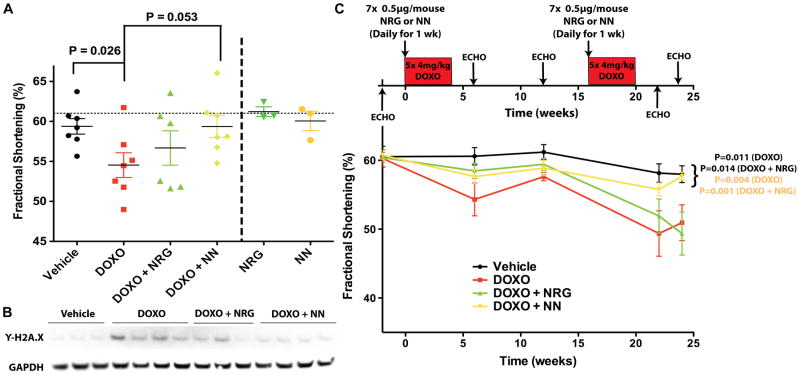
NN Confers Functional Protection from DOXO Toxicity In Vivo
To assess the efficacy of NN in vivo, we performed a pilot study applying a previously-described model of acute DOXO-induced cardiomyopathy7, 21. Indicative of impaired left ventricular function, we observed a trend toward a decrease in fractional shortening (FS) – as detected by blinded echocardiography – of mice treated with DOXO only (DOXO) as compared to animals that did not receive DOXO (Vehicle) (Figure 6A, 59.4% ± 1.0% vs. 54.5% ± 1.6%, P=0.026). Animals treated with NN displayed a trend towards attenuation of the decrease in FS associated with DOXO exposure (Figure 6A, 59.4% ± 1.4% vs. 54.5% ± 1.6%, P=0.053). FS was not affected by treatment with NRG or NN alone. Additionally, analysis of cross-sectional heart lysates from NN-treated study animals exhibited a decrease in γ-H2A.X expression as compared to DOXO-treated animals (Figure 6B), suggesting that the beneficial effect of NN in DOXO-exposed animals could at least be partially due to reduced DSDBs in the heart.
Figure 6.
Bivalent neuregulin-1β (NN) confers functional protection from doxorubicin (DOXO) toxicity in vivo. (A) Acute cardiomyopathy was induced with a single 20mg/kg intraperitoneal (ip) injection of DOXO. Mice were treated for 7d with Vehicle (0.2% BSA in PBS), neuregulin-1β (NRG), or NN at 100μg/kg ip per day, with 3 injections occurring prior to DOXO administration. Mice given the same NRG or NN treatments without DOXO injection were used as controls and are shown to the right of the vertical dashed line. Fractional shortening (FS) as assessed by blinded echocardiography at 7d is shown. The horizontal dotted line indicates the average FS of all animals at baseline echocardiography performed 2d prior to initial injection. P values were determined using a Wilcoxon rank-sum test with a Bonferroni correction (α=0.0125) following an initial Kruskal-Wallis test to determine statistical significance; no P values in this panel meet the criteria for statistical significance. (B) Immunoblot analysis of γ-H2A.X in cross-sectional heart lysates of study animals. GAPDH expression was assessed as a protein loading control. (C) Chronic DOXO-induced cardiomyopathy was induced with weekly serial 4mg/kg intraperitoneal (ip) injections of DOXO as shown. Beginning on the day of the initial DOXO injection for each 4-week series, mice were injected daily for 7d with the vehicle solution, 0.2% BSA in PBS (DOXO), neuregulin-1β (NRG), or NN at 50μg/kg ip per day. Mice that were not injected with DOXO (Vehicle) were used as controls. Fractional shortening (FS) as assessed by blinded echocardiography 2wks prior to initial DOXO injection and 6, 12, 22 and 24wks following initial DOXO injection, respectively, is shown. Only endpoint values (24wks) were analyzed; P values were determined using a Wilcoxon rank-sum test with a Bonferroni correction (α=0.0125) following an initial Kruskal-Wallis test to determine statistical significance. For this panel, P values less than 0.0125 are considered statistically significant.
The efficacy of NN as a cardioprotective agent in vivo was further assessed using a randomized and blinded mouse model of chronic DOXO-induced toxicity. Compared to the acute model, this model is more representative of the clinical administration profile of DOXO. A significant decrease in FS of DOXO-treated mice (DOXO) compared vehicle control (Vehicle) was observed at 24 weeks following initial DOXO injection (Table 1 and Figure 6C, 58.0% ± 1.2% vs. 50.9% ± 2.6%, P=0.011). A significant increase in end-systolic diameter and significantly lower body weight were also associated with DOXO treatment at 24 weeks (Table 1). Indicative of cardioprotection, animals treated with NN had a significant attenuation of the decrease in FS associated with DOXO exposure at 24 weeks (Table 1 and Figure 6C, 57.7% ± 0.6% vs. 50.9% ± 2.6%, P=0.004). In this model, NRG treatment had no effect on FS (49.4% ± 3.7% vs. 50.9% ± 2.6%, P=0.813), and NN treatment led to a significantly higher FS compared to NRG (57.7% ± 0.6% vs. 49.4% ± 3.7%, P=0.001). NN-treated mice also exhibited, in comparison to mice given DOXO only (DOXO), a trend towards increased posterior wall thickness and significantly decreased end systolic diameter at 24 weeks (Table 1), similar to the Vehicle group values and indicative of a protective effect of NN on the heart. Histological analysis of tissue from study animals revealed pockets of necrotic tissue and fibrosis in DOXO only animals, with these being less prevalent in NRG and NN treated animals (Figure I in the Online-only Data Supplement). Additionally, all animals treated with DOXO showed similar weight loss compared to the Vehicle control group (Table 1), and thus the systemic effects of DOXO were not inhibited by NN even though cardiac function was improved, further evidence that NN is not an inhibitor of DOXO activity but rather a counteracting factor that works through a different mechanism; namely, ErbB receptor stimulation. This was further confirmed by detection of ErbB2 and ErbB4 phosphorylation in mouse hearts following injection of NN or NRG (Figure II in the Online-only Data Supplement). Overall, these data support the conclusion that NN is cardioprotective from DOXO.
Table 1.
Echocardiographic Parameters Following Serial Doses of Doxorubicin in Mice
| Treatment | Baseline | 24wks | P (24wks vs. DOXO) | |
|---|---|---|---|---|
| n | Vehicle | 8 | 7† | ----- |
| DOXO | 12 | 7 | ----- | |
| DOXO + NRG | 12 | 10 | ----- | |
| DOXO + NN | 12 | 9† | ----- | |
|
| ||||
| Anterior wall thickness (mm) | Vehicle | 1.12 ± 0.07 | 1.15 ± 0.03 | 0.249 |
| DOXO | 1.12 ± 0.05 | 1.20 ± 0.11 | ----- | |
| DOXO + NRG | 1.12 ± 0.04 | 1.17 ± 0.05 | 0.922 | |
| DOXO + NN | 1.13 ± 0.02 | 1.17 ± 0.12 | 0.817 | |
|
| ||||
| Posterior wall thickness (mm) | Vehicle | 0.91 ± 0.08 | 0.99 ± 0.02 | 0.141 |
| DOXO | 0.89 ± 0.06 | 0.91 ± 0.12 | ----- | |
| DOXO + NRG | 0.89 ± 0.06 | 0.96 ± 0.12 | 0.353 | |
| DOXO + NN | 0.92 ± 0.06 | 1.01 ± 0.06 | 0.054 | |
|
| ||||
| End-systolic diameter (mm) | Vehicle | 1.08 ± 0.06 | 1.20 ± 0.05 | 0.002* |
| DOXO | 1.05 ± 0.11 | 1.49 ± 0.26 | ----- | |
| DOXO + NRG | 1.10 ± 0.05 | 1.44 ± 0.74 | 0.536 | |
| DOXO + NN | 1.06 ± 0.06 | 1.24 ± 0.13 | 0.029 | |
|
| ||||
| End-diastolic diameter (mm) | Vehicle | 2.76 ± 0.32 | 2.86 ± 0.20 | 0.11 |
| DOXO | 2.66 ± 0.23 | 3.04 ± 0.17 | ----- | |
| DOXO + NRG | 2.78 ± 0.16 | 2.83 ± 0.07 | 0.07 | |
| DOXO + NN | 2.72 ± 0.14 | 2.93 ± 0.25 | 0.247 | |
|
| ||||
| Fractional shortening (%) | Vehicle | 60.53 ± 4.26 | 57.99 ± 3.21 | 0.011* |
| DOXO | 60.28 ± 4.21 | 50.94 ± 6.88 | ----- | |
| DOXO + NRG | 60.41 ± 2.45 | 49.37 ± 9.91 | 0.813 | |
| DOXO + NN | 60.74 ± 2.24 | 57.69 ± 1.74 | 0.004* | |
|
| ||||
| Left ventricular mass (g) | Vehicle | 93.74 ± 15.78 | 112.26 ± 11.19 | 1 |
| DOXO | 88.27 ± 11.03 | 114.30 ± 15.57 | ----- | |
| DOXO + NRG | 94.10 ± 10.44 | 104.99 ± 14.94 | 0.23 | |
| DOXO + NN | 93.32 ± 8.01 | 114.44 ± 17.78 | 0.867 | |
|
| ||||
| Body weight (g) | Vehicle | 20.30 ± 0.75 | 31.98 ± 4.53 | 0.0006* |
| DOXO | 20.21 ± 0.92 | 23.46 ± 2.53 | ----- | |
| DOXO + NRG | 21.00 ± 1.03 | 23.97 ± 2.84 | 0.807 | |
| DOXO + NN | 21.74 ± 0.77 | 23.88 ± 2.14 | 0.955 | |
|
| ||||
| Heart rate (bpm) | Vehicle | 536 ± 49 | 519 ± 81 | 0.331 |
| DOXO | 515 ± 70 | 561 ± 54 | ----- | |
| DOXO + NRG | 574 ± 66 | 447 ± 100 | 0.028 | |
| DOXO + NN | 548 ± 45 | 484 ± 84 | 0.072 | |
Data are mean ± standard deviation. Vehicle = vehicle injections (0.2% BSA in PBS, no doxorubicin); DOXO = 4mg/kg doxorubicin IP injections weekly during weeks 0-4 and 16-20; DOXO + NRG = 4mg/kg doxorubicin IP injections weekly during weeks 0-4 and 16-20 with concurrent daily 50μg/kg IP injections of NRG during weeks 0 and 16; DOXO + NN = 4mg/kg doxorubicin IP injections weekly during weeks 0-4 and 16-20 with concurrent daily 50μg/kg IP injections of NN during weeks 0 and 16.
P<0.0125 was considered statistically significant following Wilcoxon rank-sum test with Bonferroni correction
1 animal from the Vehicle group and 2 animals from DOXO + NN group were sacrificed during the first 8 weeks of the study due to wounds suffered from fighting
DISCUSSION
NRG1B is a promising cardiovascular therapeutic, but has limited relevance for cardioprotection against anthracycline-induced cardiotoxicity due to its pro-neoplastic potential. We previously reported the development of NN, an engineered bivalent protein that can induce cytostatic and/or anti-neoplastic phenotypes in numerous cancer cell lines, including DOXO-sensitive breast cancer cells17. Here, we show that a newly formulated NN retains these qualities and is also cardioprotective. Thus NN may attenuate anthracycline-mediated cardiovascular toxicity, without simultaneously promoting cancer growth, supporting its potential as a therapeutic adjunct to anthracyclines in cancer patients.
These data are timely given the recent report of efficacy of NRG as a cardiovascular therapeutic in clinical trials12, as well as the initiation of clinical trials with another NRG1B molecule, Glial Growth Factor 2 (GGF2)30. The differences between NRG and GGF2 may help to explain the apparent superior cardioprotection induced by NN compared to NRG despite the similarities in their cardiomyocyte signaling profiles. Compared to NRG, GGF2 is a larger protein that contains an immunoglobulin (Ig)-like domain. This Ig-like domain may enhance the duration of effects of GGF2 versus NRG via interactions with matrix molecules that prolong tissue residence times30. Thus the differences in potency between NN and NRG in our experiments may be the result of increased cell or tissue interactions with NN due to its larger size or differences in receptor trafficking due to the tethered nature of the NRG domains on NN. It also remains to be explored whether NN has a differential effect compared to NRG on putative vascular and/or cardiac progenitor cells, which are reported to be specifically adversely affected by anthracycline exposure33, 34. Though the role of these cells in cardiac repair and regeneration is still unclear, a distinct effect of NN on them could potentially account for the differences observed in cardioprotection between NN and NRG in this study. In addition, it is possible that NN could stimulate cardiac regeneration via division of pre-existing cardiomyocytes, as suggested for native NRG28. A difference in the efficiency or efficacy of stimulation of regenerative pathways could lead to the differential protective effects observed in these studies. Finally, we cannot rule out a differential effect of NN compared to NRG owing to differences in the regulation of expression of topoisomerase-IIβ (Top2b), which was recently identified as an essential mediator of DOXO-induced cardiotoxicity35. Further exploration of differential gene expression associated with NN and NRG may yield data to support or refute the potential association of NN and/or NRG with Top2b expression.
In general, these data are congruent with previous work demonstrating the cardioprotective potential of NRG. Both the phosphoinositide-3 kinase/Akt and mitogen-activated protein kinase/ERK1/2 signaling pathways have previously been identified as critical mediators of NRG effects on cardiomyocytes that are not completely dependent upon ErbB2 participation in signaling27. Thus the ability of NN to activate these pathways (Figure 3), despite inducing relatively less ErbB2 phosphorylation than NRG (Figure 2), is not surprising. It is important to note, however, that the approach to manipulating ErbB receptor interactions with bivalent NN described here is fundamentally different from conventional receptor blocking or deletion approaches. It is well known that complete exclusion of ErbB2 from cardiac signaling – via either conditional knockout preclinical studies36 or clinically via the ErbB2-targeted antibody trastuzumab20 – is deleterious, especially so in conjunction with anthracycline exposure. NN induced partial biasing of ErbB receptor interactions and activation, but substantial ErbB2 phosphorylation was still observed (Figure 2 and Figure II in the Online-only Data Supplement), and so the negative effects associated with ErbB2 blockade are avoided.
In summary, the data show that NN is protective from DOXO-induced cardiotoxicity in vitro in rat and human cardiomyocytes and in vivo in a mouse model. Based on these results, NN may have therapeutic potential in other cardiac pathologies, including acute or chronic ischemic heart disease. Additional results from ongoing clinical trials with NRG and GGF2 will help clarify the translational potential of NN.
Supplementary Material
Acknowledgments
The authors thank Jun Yoshioka for advice and assistance with in vivo studies; Sachiko Kanki, Francesco Loffredo, Sam Senyo, Samuel Lee, Will Chutkow, Andrew Krueger and Caitlin O’Meara for technical assistance and reagents; Jen Lin for critical review of the manuscript, Lei Cai and Cathy MacGillivray for preparing and staining histological sections, and Harvard Catalyst for biostatistical consultation.
Funding Sources: Funding was provided by a U.S. Department of Defense CDMRP Breast Cancer Research Program Postdoctoral Fellowship (W81XWH-11-1-0035) to S.M.J., by NIH grants HL112905 (S.M.J.), DK090147 (M.L.S), AG032977 (R.T.L.), DE019523 and U54-CA112967 (L.G.G.), EB003805 (L.G.G. and R.T.L.), by a U.S. Department of Defense CDMRP Orthopedic Research Program Career Development Award (W81XWH-11-1-0821) to L.M.A., by a Sarnoff Fellowship to A.C.M., by a Hertz Fellowship to L.M.A., and by the Harvard Stem Cell Institute to J.R.W., C.A.M. and R.T.L.
Footnotes
Conflict of Interest Disclosures: Brigham and Women’s Hospital (BWH) and the Massachusetts Institute of Technology have filed for patents pertaining to the described bivalent ligand technology, listing L.M.A., S.M.J., R.T.L., and L.G.G. as inventors. R.T.L. is a co-founder and co-owner of Provasculon, Inc. R.T.L. is a paid consultant to the company and serves on its Board of Directors. Provasculon has interests in regenerative cell therapy, an area related to the research. R.T.L.’s interests were reviewed by BWH and Partners HealthCare.
References
- 1.Gennari A, Sormani MP, Pronzato P, Puntoni M, Colozza M, Pfeffer U, Bruzzi P. HER2 Status and Efficacy of Adjuvant Anthracyclines in Early Breast Cancer: A Pooled Analysis of Randomized Trials. J Natl Cancer Inst. 2008;100:14–20. doi: 10.1093/jnci/djm252. [DOI] [PubMed] [Google Scholar]
- 2.Wouters KA, Kremer LCM, Miller TL, Herman EH, Lipshultz SE. Protecting against anthracycline-induced myocardial damage: a review of the most promising strategies. Br J Haematol. 2005;131:561–578. doi: 10.1111/j.1365-2141.2005.05759.x. [DOI] [PubMed] [Google Scholar]
- 3.Zhao YY, Sawyer DR, Baliga RR, Opel DJ, Han X, Marchionni MA, Kelly RA. Neuregulins promote survival and growth of cardiac myocytes. Persistence of ErbB2 and ErbB4 expression in neonatal and adult ventricular myocytes. J Biol Chem. 1998;273:10261–10269. doi: 10.1074/jbc.273.17.10261. [DOI] [PubMed] [Google Scholar]
- 4.Sawyer DB, Zuppinger C, Miller TA, Eppenberger HM, Suter TM. Modulation of anthracycline-induced myofibrillar disarray in rat ventricular myocytes by neuregulin-1beta and anti-erbB2: potential mechanism for trastuzumab-induced cardiotoxicity. Circulation. 2002;105:1551–1554. doi: 10.1161/01.cir.0000013839.41224.1c. [DOI] [PubMed] [Google Scholar]
- 5.Fukazawa R, Miller TA, Kuramochi Y, Frantz S, Kim YD, Marchionni MA, Kelly RA, Sawyer DB. Neuregulin-1 protects ventricular myocytes from anthracycline-induced apoptosis via erbB4-dependent activation of PI3-kinase/Akt. J Mol Cell Cardiol. 2003;35:1473–1479. doi: 10.1016/j.yjmcc.2003.09.012. [DOI] [PubMed] [Google Scholar]
- 6.Liu X, Gu X, Li Z, Li X, Li H, Chang J, Chen P, Jin J, Xi B, Chen D, Lai D, Graham RM, Zhou M. Neuregulin-1/erbB-activation improves cardiac function and survival in models of ischemic, dilated, and viral cardiomyopathy. J Am Coll Cardiol. 2006;48:1438–1447. doi: 10.1016/j.jacc.2006.05.057. [DOI] [PubMed] [Google Scholar]
- 7.Bian Y, Sun M, Silver M, Ho KKL, Marchionni MA, Caggiano AO, Stone JR, Amende I, Hampton TG, Morgan JP, Yan X. Neuregulin-1 attenuated doxorubicin-induced decrease in cardiac troponins. Am J Physiol Heart Circ Physiol. 2009;297:H1974–H1983. doi: 10.1152/ajpheart.01010.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Timolati F, Ott D, Pentassuglia L, Giraud MN, Perriard JC, Suter TM, Zuppinger C. Neuregulin-1 beta attenuates doxorubicin-induced alterations of excitation-contraction coupling and reduces oxidative stress in adult rat cardiomyocytes. J Mol Cell Cardiol. 2006;41:845–854. doi: 10.1016/j.yjmcc.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 9.Fuller SJ, Sivarajah K, Sugden PH. ErbB receptors, their ligands, and the consequences of their activation and inhibition in the myocardium. J Mol Cell Cardiol. 2008;44:831–854. doi: 10.1016/j.yjmcc.2008.02.278. [DOI] [PubMed] [Google Scholar]
- 10.Lemmens K, Segers VF, Demolder M, De Keulenaer GW. Role of neuregulin-1/ErbB2 signaling in endothelium-cardiomyocyte cross-talk. J Biol Chem. 2006;281:19469–19477. doi: 10.1074/jbc.M600399200. [DOI] [PubMed] [Google Scholar]
- 11.Hedhli N, Huang Q, Kalinowski A, Palmeri M, Hu X, Russell RR, Russell KS. Endothelium-derived neuregulin protects the heart against ischemic injury. Circulation. 2011;123:2254–2262. doi: 10.1161/CIRCULATIONAHA.110.991125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gao R, Zhang J, Cheng L, Wu X, Dong W, Yang X, Li T, Liu X, Xu Y, Li X, Zhou M. A Phase II, randomized, double-blind, multicenter, based on standard therapy, placebo-controlled study of the efficacy and safety of recombinant human neuregulin-1 in patients with chronic heart failure. J Am Coll Cardiol. 2010;55:1907–1914. doi: 10.1016/j.jacc.2009.12.044. [DOI] [PubMed] [Google Scholar]
- 13.Stove C, Bracke M. Roles for neuregulins in human cancer. Clin Exp Metastasis. 2004;21:665–684. doi: 10.1007/s10585-004-6917-6. [DOI] [PubMed] [Google Scholar]
- 14.Li Q, Ahmed S, Loeb JA. Development of an autocrine neuregulin signaling loop with malignant transformation of human breast epithelial cells. Cancer Res. 2004;64:7078–7085. doi: 10.1158/0008-5472.CAN-04-1152. [DOI] [PubMed] [Google Scholar]
- 15.Soler M, Mancini F, Meca-Cortes O, Sanchez-Cid L, Rubio N, Lopez-Fernandez S, Lozano JJ, Blanco J, Fernandez PL, Thomson TM. HER3 is required for the maintenance of neuregulin-dependent and -independent attributes of malignant progression in prostate cancer cells. Int J Cancer. 2009;125:2565–2575. doi: 10.1002/ijc.24651. [DOI] [PubMed] [Google Scholar]
- 16.Hsieh SY, He JR, Hsu CY, Chen WJ, Bera R, Lin KY, Shih TC, Yu MC, Lin YJ, Chang CJ, Weng WH, Huang SF. Neuregulin/erythroblastic leukemia viral oncogene homolog 3 autocrine loop contributes to invasion and early recurrence of human hepatoma. Hepatology. 2011;53:504–516. doi: 10.1002/hep.24083. [DOI] [PubMed] [Google Scholar]
- 17.Jay SM, Kurtagic E, Alvarez LM, de Picciotto S, Sanchez E, Hawkins JF, Prince RN, Guerrero Y, Treasure CL, Lee RT, Griffith LG. Engineered bivalent ligands to bias ErbB receptor-mediated signaling and phenotypes. J Biol Chem. 2011;286:27729–27740. doi: 10.1074/jbc.M111.221093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shi F, Telesco SE, Liu Y, Radhakrishnan R, Lemmon MA. ErbB3/HER3 intracellular domain is competent to bind ATP and catalyze autophosphorylation. Proc Natl Acad Sci U S A. 2010;107:7692–7697. doi: 10.1073/pnas.1002753107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Citri A, Yarden Y. EGF-ERBB signalling: towards the systems level. Nat Rev Mol Cell Biol. 2006;7:505–516. doi: 10.1038/nrm1962. [DOI] [PubMed] [Google Scholar]
- 20.Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, Fleming T, Eiermann W, Wolter J, Pegram M, Baselga J, Norton L. Use of Chemotherapy plus a Monoclonal Antibody against HER2 for Metastatic Breast Cancer That Overexpresses HER2. N Engl J Med. 2001;344:783–792. doi: 10.1056/NEJM200103153441101. [DOI] [PubMed] [Google Scholar]
- 21.Bien S, Riad A, Ritter CA, Gratz M, Olshausen F, Westermann D, Grube M, Krieg T, Ciecholewski S, Felix SB, Staudt A, Schultheiss HP, Ewert R, Volker U, Tschope C, Kroemer HK. The endothelin receptor blocker bosentan inhibits doxorubicin-induced cardiomyopathy. Cancer Res. 2007;67:10428–10435. doi: 10.1158/0008-5472.CAN-07-1344. [DOI] [PubMed] [Google Scholar]
- 22.Neilan TG, Blake SL, Ichinose F, Raher MJ, Buys ES, Jassal DS, Furutani E, Perez-Sanz TM, Graveline A, Janssens SP, Picard MH, Scherrer-Crosbie M, Bloch KD. Disruption of nitric oxide synthase 3 protects against the cardiac injury, dysfunction, and mortality induced by doxorubicin. Circulation. 2007;116:506–514. doi: 10.1161/CIRCULATIONAHA.106.652339. [DOI] [PubMed] [Google Scholar]
- 23.Sheng Q, Liu X, Fleming E, Yuan K, Piao H, Chen J, Moustafa Z, Thomas RK, Greulich H, Schinzel A, Zaghlul S, Batt D, Ettenberg S, Meyerson M, Schoeberl B, Kung AL, Hahn WC, Drapkin R, Livingston DM, Liu JF. An activated ErbB3/NRG1 autocrine loop supports in vivo proliferation in ovarian cancer cells. Cancer Cell. 2010;17:298–310. doi: 10.1016/j.ccr.2009.12.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guo P, You JO, Yang J, Moses MA, Auguste DT. Using breast cancer cell CXCR4 surface expression to predict liposome binding and cytotoxicity. Biomaterials. 2012;33:8104–8110. doi: 10.1016/j.biomaterials.2012.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schaefer G, Fitzpatrick VD, Sliwkowski MX. Gamma-heregulin: a novel heregulin isoform that is an autocrine growth factor for the human breast cancer cell line, MDA-MB-175. Oncogene. 1997;15:1385–1394. doi: 10.1038/sj.onc.1201317. [DOI] [PubMed] [Google Scholar]
- 26.Wilson TR, Lee DY, Berry L, Shames DS, Settleman J. Neuregulin-1-mediated autocrine signaling underlies sensitivity to HER2 kinase inhibitors in a subset of human cancers. Cancer Cell. 2011;20:158–172. doi: 10.1016/j.ccr.2011.07.011. [DOI] [PubMed] [Google Scholar]
- 27.Kuramochi Y, Guo X, Sawyer DB. Neuregulin activates erbB2-dependent src/FAK signaling and cytoskeletal remodeling in isolated adult rat cardiac myocytes. J Mol Cell Cardiol. 2006;41:228–235. doi: 10.1016/j.yjmcc.2006.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bersell K, Arab S, Haring B, Kuhn B. Neuregulin1/ErbB4 signaling induces cardiomyocyte proliferation and repair of heart injury. Cell. 2009;138:257–270. doi: 10.1016/j.cell.2009.04.060. [DOI] [PubMed] [Google Scholar]
- 29.Jabbour A, Hayward CS, Keogh AM, Kotlyar E, McCrohon JA, England JF, Amor R, Liu X, Li XY, Zhou MD, Graham RM, Macdonald PS. Parenteral administration of recombinant human neuregulin-1 to patients with stable chronic heart failure produces favourable acute and chronic haemodynamic responses. Eur J Heart Fail. 2011;13:83–92. doi: 10.1093/eurjhf/hfq152. [DOI] [PubMed] [Google Scholar]
- 30.Sawyer DB, Caggiano A. Neuregulin-1beta for the treatment of systolic heart failure. J Mol Cell Cardiol. 2011;51:501–505. doi: 10.1016/j.yjmcc.2011.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.L’Ecuyer T, Sanjeev S, Thomas R, Novak R, Das L, Campbell W, Heide RV. DNA damage is an early event in doxorubicin-induced cardiac myocyte death. Am J Physiol Heart Circ Physiol. 2006;291:H1273–1280. doi: 10.1152/ajpheart.00738.2005. [DOI] [PubMed] [Google Scholar]
- 32.Chowdhury D, Keogh MC, Ishii H, Peterson CL, Buratowski S, Lieberman J. gamma-H2AX dephosphorylation by protein phosphatase 2A facilitates DNA double-strand break repair. Mol Cell. 2005;20:801–809. doi: 10.1016/j.molcel.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 33.De Angelis A, Piegari E, Cappetta D, Marino L, Filippelli A, Berrino L, Ferreira-Martins J, Zheng H, Hosoda T, Rota M, Urbanek K, Kajstura J, Leri A, Rossi F, Anversa P. Anthracycline cardiomyopathy is mediated by depletion of the cardiac stem cell pool and is rescued by restoration of progenitor cell function. Circulation. 2010;121:276–292. doi: 10.1161/CIRCULATIONAHA.109.895771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Huang C, Zhang X, Ramil JM, Rikka S, Kim L, Lee Y, Gude NA, Thistlethwaite PA, Sussman MA, Gottlieb RA, Gustafsson AB. Juvenile exposure to anthracyclines impairs cardiac progenitor cell function and vascularization resulting in greater susceptibility to stress-induced myocardial injury in adult mice. Circulation. 2010;121:675–683. doi: 10.1161/CIRCULATIONAHA.109.902221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhang S, Liu X, Bawa-Khalfe T, Lu LS, Lyu YL, Liu LF, Yeh ET. Identification of the molecular basis of doxorubicin-induced cardiotoxicity. Nat Med. 2012;18:1639–1642. doi: 10.1038/nm.2919. [DOI] [PubMed] [Google Scholar]
- 36.Crone SA, Zhao YY, Fan L, Gu Y, Minamisawa S, Liu Y, Peterson KL, Chen J, Kahn R, Condorelli G, Ross J, Jr, Chien KR, Lee KF. ErbB2 is essential in the prevention of dilated cardiomyopathy. Nat Med. 2002;8:459–465. doi: 10.1038/nm0502-459. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.