Abstract
Objective
To examine interstate variation in US HIV case-fatality rates, and compare them with corresponding conventional HIV death rates.
Design
Cross-sectional analysis using data on deaths due to HIV infection from the National Vital Statistics System and data on persons 15 years or older living with HIV infection in 2001—2007 in 37 U.S. states from the national HIV/AIDS Reporting System.
Methods
State rankings by age-adjusted HIV case-fatality rates (with HIV-infected population denominators) were compared with rankings by conventional death rates (with general population denominators). Negative binomial regression determined case-fatality rate ratios (RRs) among states, adjusted for age, sex, race/ethnicity, year, and state-level markers of late HIV diagnosis.
Results
Based on 3,096,729 HIV-infected person-years, the overall HIV case-fatality rate was 20.6/1,000 person-years (95% confidence interval [CI], 20.3–20.9). Age-adjusted rates by state ranged from 9.6 (95% CI 6.8–12.4) in Idaho to 32.9 (95% CI 29.8–36.0) in Mississippi, demonstrating significant differences across states, even after adjusting for race/ethnicity (p<0.0001). Many states with low conventional death rates had high case-fatality rates. Nine of the ten states with the highest case-fatality rates were located in the U.S. South.
Conclusions
Case-fatality rates complement and are not entirely concordant with conventional death rates. Interstate differences in these rates may reflect differences in secondary and tertiary prevention of HIV-related mortality among infected persons. These data suggest that state-specific contextual barriers to care may impede improvements in quality and disparities of health-care without targeted interventions.
Keywords: case fatality rate, geographic factors, healthcare disparities, mortality, excess, mortality determinants, surveillance, United States
INTRODUCTION
In the United States (US), human immunodeficiency virus (HIV) infection remains a major public health concern. About 50,000 new infections continue to occur annually[1], and while deaths due to HIV infection declined dramatically after the introduction of highly active antiretroviral therapy (HAART) in the late 1990s[2], continued mortality reductions have been small in recent years[3]. The National HIV/AIDS Strategy for the United States has prioritized the reduction of health disparities among demographic groups[4]. Examining disparities by geography is important, since they may suggest reducible contextual barriers to health care for HIV-infected persons[5–7]. Interstate disparities may be particularly informative, because health care access varies with state policies regarding insurance for healthcare and prescription drugs. Yet few studies have examined interstate disparities in HIV-related outcomes in the HAART era. Two cross-sectional studies from the late 1990s found substantial state-level variation in the use of services, length of stay, and inpatient mortality among hospitalized HIV-infected patients in 10 states[8, 9]. Annual national vital statistics also report wide differences in rates of death due to HIV disease by state (range: 0.8—8.3 per 100,000 in 2007)[10].
The choice of the measure used to describe state-based disparities is underappreciated. “Conventional” death rates include both HIV-infected and uninfected individuals in the denominator to quantify HIV mortality in a population overall. However, these rates may obscure important distinctions by reflecting the underlying prevalence and, indirectly, the incidence, of HIV infection in the general population. Thus, higher death rates may be due, in part, to failures of primary prevention of HIV infection, which can confound the analysis of factors important for secondary or tertiary prevention of death among people already infected with HIV. In contrast, case-fatality rates assess mortality in only the HIV-infected population, and thus are more useful for identifying determinants of the availability, utilization, timeliness, and quality of care for that population.
Using national population-based data, we compared HIV case-fatality rates in 37 US states in 2001—2007 to conventional HIV death rates based on general population denominators. We also compared case-fatality rates among states, controlling for age, sex, race/ethnicity, year, and state-level markers of late HIV diagnosis. Lastly, to explore the potential consequences that interventions could have if they lowered state case-fatality rates enough to eliminate the interstate differences, we calculated the number of excess deaths associated with living in states with higher case-fatality rates.
METHODS
Study population and data sources
HIV case-fatality rate denominators (reported per 1,000 HIV-infected person-years) were computed using data from all persons aged 15 years and older alive during 2001—2007 who were reported to the national HIV/AIDS Reporting System (HARS) by December 31, 2009[11] and met the surveillance case definition of HIV infection[12].
Analysis was restricted to persons who at diagnosis were residents of the 37 states that had confidential name-based reporting of HIV infection for at least four years by 2010, because four years has been found long enough for reliable determination of trends after such reporting has been implemented in a state[13]. State surveillance programs ascertained deaths by linking cases with death registries (state vital statistics, National Death Index, or Social Security Death Master File). Persons were presumed alive if not found to be dead. Numbers in each state were adjusted for reporting delays[13].
Case-fatality numerators used HIV deaths from death certificate data files of the National Vital Statistics System for 2001—2007[14]. These files contain individual-level information on all deaths reported to state or local health departments. HIV deaths were defined as those for which the underlying cause was determined to be HIV disease, as indicated by ICD-10 codes B20 through B24[15].
For comparison, we calculated conventional HIV death rates (per 100,000 population person-years) for each state using the same numerator data but denominators derived using data from the annual US Census Bureau population estimates[16]. For this measure, we included all persons aged 15 and older who lived in the same states in 2001—2007.
Statistical analysis
Direct standardization was used for age-adjustment based on the 2000 US Standard Population[17]. States were ranked based on each of the age-adjusted rates calculated for the full study period. Five states contributed data only in later years due to newly implemented confidential name-based HIV reporting: New York (2002—2007); Georgia (2005—2007); and Connecticut, Kentucky, and New Hampshire (2006—2007).
We compared HIV case-fatality rates among states using negative binomial regression. We used the state with the lowest overall case-fatality rate as the reference group and controlled for age, sex, race/ethnicity, and year. We explored the possibility that late HIV diagnosis at the state level could account for differences in HIV case-fatality rates by further controlling for two markers of late HIV diagnosis in each state: the median CD4+ T-lymphocyte count at HIV diagnosis in 2005—2007 and the percent of all HIV diagnoses considered to be late (i.e., diagnosed within 12 months of initial HIV diagnosis) in 2007[18]. These measures of late HIV diagnosis were included as random effects, in order to properly account for clustering within states, in models that also controlled for the previously mentioned characteristics.
To assess potential mortality reductions if interventions could reduce case-fatality rates in higher mortality states to those in lower mortality states, we calculated the population attributable fraction (PAF), i.e., the proportion of deaths hypothetically prevented by eliminating the causal effects of a given exposure[19]. We defined PAF as 1−Σ(pdi/RRi), where pdi represents the proportion of HIV deaths in each quartile i of state case-fatality rates and RRi represents the adjusted relative case-fatality rate for i compared with the lowest quartile[19]. We calculated excess HIV deaths that could be prevented by multiplying the PAF in each quartile by the number of observed deaths and then summing[20]. 95% CIs were constructed based on 1,000 parametric bootstrap samples. Sensitivity analyses examined how the PAF and excess deaths would change if alternate reference groups were chosen.
RESULTS
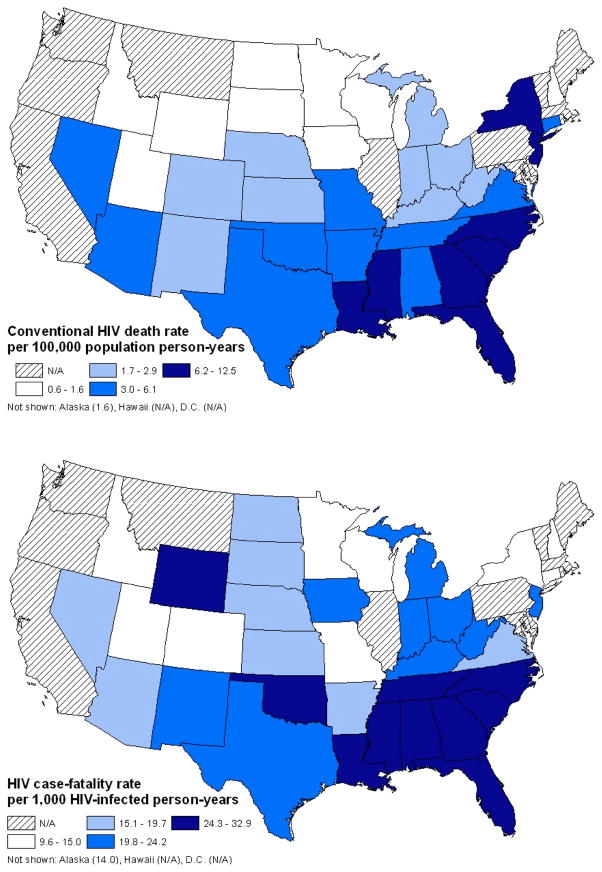
The analysis included 3,096,729 HIV-infected person-years during 2001—2007 from 37 states. Overall, the age-adjusted HIV case-fatality rate was 20.6/1,000 HIV-infected person-years (95% CI 20.3—20.9). The corresponding conventional HIV death rate (using the general population denominator) was 5.8/100,000 person-years (95% CI 5.7—5.8). Figure 1 displays maps of the two rates in each state, showing generally higher values for both in the South.
Figure 1.
Maps of conventional HIV death rate per 100,000 population person-years and HIV case-fatality rate per 1,000 HIV-infected person-years, 37 US states, 2001–2007.
Table 1 provides HIV case-fatality rates and conventional death rates, with corresponding rankings for each state, highlighting those with more discordant rankings. The ranks of certain states changed substantially when moving from the conventional death rate to the case-fatality rate. For example, Wyoming’s rank moved up 27 places (from 36 to 9) and Iowa’s 17 places (from 34 to 17). Similarly, the ranks of New York and Connecticut moved down 27 places (from 3 to 30) and 23 places (from 12 to 35), respectively. In contrast, other states demonstrated no major change in ranks. For example, Louisiana had the second highest rate regardless of the denominator used.
Table 1.
HIV mortality rates and associated rankings by state of residence, 37 US states, 2001–2007.
|
Conventional HIV death rate |
HIV case-fatality rate | |||||||
|---|---|---|---|---|---|---|---|---|
| State | HIV deaths | Person- years | Rate per 100,000 p- y (95% CI) | Ranking | Person- years | Rate per 1,000 p-y (95% CI) | Ranking | Difference in ranking |
| Wyoming | 19 | 2,829,013 | 0.7 (0.4, 1.0) | 36 | 1,064 | 24.3 (0.8, 47.8) | 9 | +27 |
| Iowa | 144 | 16,527,812 | 0.9 (0.8, 1.1) | 34 | 8,083 | 20.1 (13.9, 26.3) | 17 | +17 |
| Oklahoma | 627 | 19,532,857 | 3.4 (3.1, 3.7) | 17 | 26,502 | 29.8 (25.0, 34.6) | 3 | +14 |
| Kentucky* | 135 | 6,779,940 | 2.0 (1.6, 2.3) | 24 | 7,811 | 23.3 (15.5, 31.0) | 13 | +11 |
| West Virginia | 175 | 10,383,505 | 1.8 (1.5, 2.1) | 25 | 8,294 | 23.2 (16.8, 29.6) | 14 | +11 |
| South Dakota | 39 | 4,293,592 | 1.0 (0.7, 1.3) | 33 | 2,055 | 19.3 (10.6, 28.1) | 22 | +11 |
| North Dakota | 19 | 3,609,298 | 0.6 (0.3, 0.8) | 37 | 897 | 15.2 (8.1, 22.4) | 27 | +10 |
| New Mexico | 247 | 10,372,810 | 2.5 (2.2, 2.8) | 20 | 12,798 | 24.1 (18.2, 30.1) | 11 | +9 |
| Mississippi | 1,279 | 15,752,311 | 8.5 (8.1, 9.0) | 7 | 46,914 | 32.9 (29.8, 36.0) | 1 | +6 |
| Nebraska | 160 | 9,628,516 | 1.8 (1.5, 2.1) | 26 | 8,312 | 19.6 (13.8, 25.4) | 20 | +6 |
| North Carolina | 3,033 | 47,766,115 | 6.4 (6.1, 6.6) | 8 | 123,187 | 28.8 (26.9, 30.6) | 4 | +4 |
| Tennessee | 1,988 | 33,184,818 | 6.1 (5.8, 6.4) | 9 | 80,323 | 27.0 (24.7, 29.3) | 5 | +4 |
| Indiana | 800 | 34,381,740 | 2.4 (2.2, 2.5) | 23 | 47,183 | 19.7 (16.8, 22.5) | 19 | +4 |
| New Hampshire* | 22 | 2,136,165 | 1.0 (0.6, 1.4) | 32 | 2,101 | 15.0 (1.6, 28.4) | 28 | +4 |
| Alabama | 1,345 | 25,237,736 | 5.5 (5.2, 5.8) | 11 | 58,116 | 25.0 (22.6, 27.4) | 8 | +3 |
| Michigan | 1,540 | 55,867,002 | 2.8 (2.6, 2.9) | 19 | 76,226 | 20.9 (18.9, 22.8) | 16 | +3 |
| Ohio | 1,514 | 63,829,345 | 2.4 (2.3, 2.5) | 21 | 87,552 | 19.8 (17.8, 21.9) | 18 | +3 |
| Kansas | 235 | 15,093,032 | 1.6 (1.4, 1.8) | 27 | 14,294 | 15.3 (11.6, 18.9) | 26 | +1 |
| Louisiana | 2,626 | 24,358,737 | 11.2 (10.8, 11.6) | 2 | 93,984 | 32.5 (30.1, 34.9) | 2 | 0 |
| South Carolina | 1,971 | 23,520,693 | 8.6 (8.2, 9.0) | 6 | 83,839 | 25.2 (23.3, 27.1) | 7 | −1 |
| Georgia* | 2,034 | 21,777,350 | 9.2 (8.8, 9.6) | 4 | 81,333 | 25.6 (23.9, 27.4) | 6 | −2 |
| Texas | 7,183 | 120,840,116 | 6.0 (5.9, 6.2) | 10 | 338,818 | 23.5 (22.5, 24.5) | 12 | −2 |
| Idaho | 58 | 7,560,110 | 0.8 (0.6, 1.0) | 35 | 4,149 | 9.6 (6.8, 12.4) | 37 | −2 |
| Alaska | 61 | 3,547,757 | 1.6 (1.2, 2.0) | 28 | 3,567 | 14.0 (8.3, 19.7) | 31 | −3 |
| Wisconsin | 427 | 30,868,031 | 1.4 (1.3, 1.5) | 29 | 27,861 | 13.9 (11.4, 16.5) | 32 | −3 |
| Minnesota | 364 | 28,253,963 | 1.3 (1.2, 1.4) | 30 | 33,475 | 13.5 (10.5, 16.6) | 33 | −3 |
| Utah | 141 | 12,692,988 | 1.3 (1.1, 1.5) | 31 | 12,638 | 12.8 (7.7, 17.9) | 34 | −3 |
| Arkansas | 542 | 15,289,098 | 3.8 (3.5, 4.1) | 15 | 27,966 | 19.6 (16.6, 22.5) | 21 | −6 |
| Arizona | 1,037 | 31,575,121 | 3.5 (3.2, 3.7) | 16 | 64,371 | 16.4 (14.6, 18.2) | 24 | −8 |
| Florida | 11,814 | 98,709,697 | 12.5 (12.3, 12.7) | 1 | 515,228 | 24.2 (23.5, 24.9) | 10 | −9 |
| Virginia | 1,761 | 41,737,691 | 4.2 (4.0, 4.4) | 14 | 114,858 | 16.8 (15.5, 18.2) | 23 | −9 |
| New Jersey | 4,505 | 48,003,059 | 9.1 (8.8, 9.3) | 5 | 216,067 | 21.1 (20.0, 22.2) | 15 | −10 |
| Missouri | 918 | 32,069,892 | 2.9 (2.8, 3.1) | 18 | 65,114 | 15.0 (13.2, 16.8) | 29 | −11 |
| Nevada | 547 | 12,736,382 | 4.3 (3.9, 4.6) | 13 | 38,137 | 15.5 (13.1, 18.0) | 25 | −12 |
| Colorado | 625 | 25,617,008 | 2.4 (2.2, 2.6) | 22 | 64,147 | 9.8 (8.4, 11.3) | 36 | −14 |
| Connecticut* | 264 | 5,634,702 | 4.4 (3.9, 4.9) | 12 | 21,223 | 12.2 (9.8, 14.5) | 35 | −23 |
| New York* | 10,024 | 93,312,262 | 10.7 (10.5, 10.9) | 3 | 678,242 | 14.7 (14.2, 15.2) | 30 | −27 |
Abbreviations: CI = confidence interval, HIV = human immunodeficiency virus, p-y = person-years.
Rates restricted to persons age 15 and older and age-adjusted to the 2000 US Standard Population.
Fewer than seven years of data used to calculate rates.
Table 2 shows results from regression models examining characteristics associated with HIV case-fatality rate ratios (RRs). Overall, differences by state were statistically significant when initially adjusting for age only and after adjusting for sex, race/ethnicity, and calendar year also (both p<0.0001). Compared with Colorado, which had the lowest rate in the fully adjusted model, 12 of the 14 states representing the South had case-fatality rates at least twice as high, illustrating substantial variation in rates by state (e.g., RR for Georgia: 2.53, 95% CI 2.27—2.80). Other characteristics significantly associated with increases in case-fatality rates included older age and non-Hispanic black race/ethnicity. In addition, case-fatality rates declined over time (RR 0.91 per year, 95% CI 0.90—0.91). Including state-level measures of late HIV diagnosis in models did not change the rate ratios or overall rankings of state case-fatality rates appreciably (data not shown).
Table 2.
Factors associated with HIV case-fatality rate, 37 US states, 2001–2007.
| Variable | Age-adjusted rate ratio (95% CI) | P-value | Fully-adjusted* rate ratio (95% Cl) | P-value |
|---|---|---|---|---|
| Age, per 10 years | 1.35 (1.33, 1.37) | <0.001 | 1.36 (1.35, 1.37) | <0.001 |
| Calendar year | 0.91 (0.90, 0.92) | <0.001 | 0.91 (0.90, 0.91) | <0.001 |
| Race/ethnicity (ref. = non-Hispanic other) | ||||
| Non-Hispanic black | 1.47 (1.42, 1.52) | <0.001 | 1.43 (1.40, 1.47) | <0.001 |
| Hispanic | 0.95 (0.90, 0.99) | 0.03 | 1.00 (0.97, 1.04) | 0.86 |
| Female sex (ref. = male) | 1.06 (1.02, 1.10) | <0.01 | 1.03 (1.00, 1.05) | 0.02 |
| State of residence (ref. = Colorado†) | ||||
| Alaska | 1.54 (1.16, 2.05) | <0.01 | 1.65 (1.27, 2.16) | <0.001 |
| Alabama | 2.32 (2.03, 2.64) | <0.001 | 2.09 (1.88, 2.32) | <0.001 |
| Arkansas | 2.06 (1.78, 2.39) | <0.001 | 1.92 (1.70, 2.17) | <0.001 |
| Arizona | 1.66 (1.44, 1.90) | <0.001 | 1.72 (1.54, 1.92) | <0.001 |
| Connecticut | 1.11 (0.92, 1.34) | 0.26 | 1.39 (1.19, 1.62) | <0.001 |
| Florida | 2.13 (1.90, 2.40) | <0.001 | 2.03 (1.86, 2.23) | <0.001 |
| Georgia | 2.31 (2.01, 2.65) | <0.001 | 2.53 (2.27, 2.80) | <0.001 |
| Iowa | 1.74 (1.41, 2.14) | <0.001 | 1.83 (1.52, 2.21) | <0.001 |
| Idaho | 1.33 (0.99, 1.77) | 0.06 | 1.44 (1.10, 1.90) | 0.01 |
| Indiana | 1.75 (1.52, 2.02) | <0.001 | 1.72 (1.53, 1.92) | <0.001 |
| Kansas | 1.66 (1.38, 1.98) | <0.001 | 1.69 (1.45, 1.98) | <0.001 |
| Kentucky | 1.84 (1.46, 2.33) | <0.001 | 2.17 (1.78, 2.64) | <0.001 |
| Louisiana | 2.80 (2.47, 3.17) | <0.001 | 2.52 (2.28, 2.78) | <0.001 |
| Michigan | 1.99 (1.74, 2.26) | <0.001 | 1.79 (1.62, 1.99) | <0.001 |
| Minnesota | 1.12 (0.95, 1.32) | 0.17 | 1.09 (0.95, 1.26) | 0.19 |
| Missouri | 1.49 (1.30, 1.72) | <0.001 | 1.38 (1.23, 1.54) | <0.001 |
| Mississippi | 2.76 (2.41, 3.15) | <0.001 | 2.42 (2.18, 2.69) | <0.001 |
| North Carolina | 2.42 (2.14, 2.74) | <0.001 | 2.17 (1.97, 2.39) | <0.001 |
| North Dakota | 1.60 (1.00, 2.55) | 0.05 | 1.67 (1.06, 2.65) | 0.03 |
| Nebraska | 1.95 (1.60, 2.38) | <0.001 | 1.99 (1.67, 2.38) | <0.001 |
| New Hampshire | 0.97 (0.61, 1.53) | 0.89 | 1.30 (0.84, 2.00) | 0.24 |
| New Jersey | 1.89 (1.67, 2.13) | <0.001 | 1.76 (1.60, 1.93) | <0.001 |
| New Mexico | 1.90 (1.59, 2.27) | <0.001 | 2.06 (1.76, 2.40) | <0.001 |
| Nevada | 1.46 (1.25, 1.69) | <0.001 | 1.45 (1.28, 1.64) | <0.001 |
| New York | 1.37 (1.22, 1.54) | <0.001 | 1.35 (1.23, 1.48) | <0.001 |
| Ohio | 1.74 (1.52, 1.98) | <0.001 | 1.66 (1.50, 1.84) | <0.001 |
| Oklahoma | 2.47 (2.13, 2.87) | <0.001 | 2.48 (2.20, 2.79) | <0.001 |
| South Carolina | 2.29 (2.01, 2.60) | <0.001 | 2.00 (1.81, 2.21) | <0.001 |
| South Dakota | 1.68 (1.19, 2.36) | <0.01 | 1.77 (1.28, 2.46) | <0.001 |
| Tennessee | 2.63 (2.31, 2.99) | <0.001 | 2.35 (2.13, 2.60) | <0.001 |
| Texas | 2.26 (2.01, 2.54) | <0.001 | 2.14 (1.95, 2.34) | <0.001 |
| Utah | 1.09 (0.88, 1.35) | 0.41 | 1.21 (1.00, 1.46) | 0.05 |
| Virginia | 1.50 (1.32, 1.71) | <0.001 | 1.35 (1.22, 1.49) | <0.001 |
| Wisconsin | 1.50 (1.28, 1.75) | <0.001 | 1.46 (1.28, 1.67) | <0.001 |
| West Virginia | 2.00 (1.64, 2.43) | <0.001 | 2.02 (1.70, 2.40) | <0.001 |
| Wyoming | 1.41 (0.89, 2.26) | 0.15 | 1.50 (0.95, 2.38) | 0.08 |
Abbreviation: CI = confidence interval, HIV = human immunodeficiency virus. *Adjusted for age, calendar year, race/ethnicity, and sex.
Colorado was chosen as the reference group because it was the state of residence with the lowest case-fatality rate after adjusting for all other characteristics.
The PAF attributable to living in states with case-fatality rates higher than those in the lowest quartile was 0.269 (95% CI 0.253—0.286) (Table 3). This translates to 5,669 excess deaths (95% CI 5,331—6,076) that hypothetically could have been eliminated if an intervention reduced case-fatality rates in states with higher rates to rates of states in the lowest quartile, or 809 deaths annually. Sensitivity analyses using alternate reference groups to target mortality reduction goals resulted in the hypothetical elimination of 291—913 excess deaths annually (Appendix Table 1).
Table 3.
Population attributable fraction and excess HIV deaths associated with living in states with higher HIV case-fatality rates, 37 US states, 2001–2007.
| Quartile of state HIV case-fatality rate | Rate ratio* (95% CI) | HIV deaths | Proportion of deaths | Population attributable fraction (95% CI) | Excess HIV deaths (95% CI) |
|---|---|---|---|---|---|
| Quartile 1 | 1.76 (1.70–1.82) | 14,922 | 0.25 | 0.107 (0.101–0.114) | 1,602 (1,508–1,670) |
| Quartile 2 | 1.49 (1.44–1.53) | 27,257 | 0.45 | 0.146 (0.135–0.157) | 3,987 (3,761–4,312) |
| Quartile 3 | 1.22 (1.17–1.27) | 5,140 | 0.09 | 0.016 (0.012–0.019) | 80 (62–94) |
| Quartile 4 | Reference | 12,904 | 0.21 | Reference | Reference |
|
| |||||
| Overall | - | 60,223 | 1.00 | 0.269 (0.253–0.286) | 5,669 (5,331–6,076) |
Abbreviation: CI = confidence interval, HIV = human immunodeficiency virus.
Adjusted for age, calendar year, race/ethnicity, and sex.
Appendix Table 1.
Sensitivity analysis showing differences in population attributable fraction and excess HIV deaths due to living in states with higher HIV case-fatality rates, based on different scenarios.
| Quantile of state HIV case-fatality rate | Rate ratio* (95% CI) | HIV deaths | Proportion of deaths | Population attributable fraction (95% CI) | Excess HIV deaths (95% CI) |
|---|---|---|---|---|---|
| Scenario 1: Reduce rate in Quartiles 1–2 to rate in Quartile 3 | |||||
| Quartile 1 | 1.44 (1.39–1.50) | 14,922 | 0.25 | 0.077 (0.069–0.084) | 1,143 (1,031–1,231) |
| Quartile 2 | 1.22 (1.18–1.27) | 27,257 | 0.45 | 0.081 (0.067–0.095) | 2,207 (1,870–2,609) |
| Quartile 3 | Reference | 5,140 | 0.09 | Reference | Reference |
| Quartile 4 | 0.82 (0.79–0.86) | 12,904 | 0.21 | N/A | N/A |
|
| |||||
| Overall | 60,223 | 1.00 | 0.158 (0.138–0.177) | 3,350 (2,901–3,840) | |
|
| |||||
| Scenario 2: Reduce rate in Quintiles 1–4 to rate in Quintile 5 | |||||
| Quintile 1 | 1.94 (1.84–2.04) | 13,558 | 0.23 | 0.109 (0.101–0.116) | 1,473 (1,380–1,570) |
| Quintile 2 | 1.67 (1.59–1.76) | 25,423 | 0.42 | 0.168 (0.154–0.182) | 4,271 (3,964–4,636) |
| Quintile 3 | 1.47 (1.39–1.56) | 4,739 | 0.08 | 0.025 (0.022–0.029) | 119 (104–137) |
| Quintile 4 | 1.17 (1.11–1.24) | 14,563 | 0.24 | 0.036 (0.025–0.048) | 531 (352–673) |
| Quintile 5 | Reference | 1,940 | 0.03 | Reference | Reference |
|
| |||||
| Overall | 60,223 | 1.00 | 0.338 (0.306–0.369) | 6,394 (5,800–7,016) | |
|
| |||||
| Scenario 3: Reduce rate in Quintiles 1–3 to rate in Quintile 4 | |||||
| Quintile 1 | 1.65 (1.60–1.70) | 13,558 | 0.23 | 0.089 (0.083–0.094) | 1,199 (1,134–1,273) |
| Quintile 2 | 1.43 (1.38–1.47) | 25,423 | 0.42 | 0.125 (0.114–0.135) | 3,170 (2,968–3,425) |
| Quintile 3 | 1.25 (1.20–1.30) | 4,739 | 0.08 | 0.016 (0.013–0.019) | 75 (104–137) |
| Quintile 4 | Reference | 14,563 | 0.24 | Reference | Reference |
| Quintile 5 | 0.85 (0.81–0.90) | 1,940 | 0.03 | N/A | N/A |
|
| |||||
| Overall | 60,223 | 1.00 | 0.229 (0.214–0.244) | 4,444 (4,206–4,835) | |
|
| |||||
| Scenario 3: Reduce rate in Quintiles 1–3 to rate in Quintile 4 | |||||
| Quintile 1 | 1.32 (1.27–1.37) | 13,558 | 0.23 | 0.054 (0.047–0.062) | 736 (641–829) |
| Quintile 2 | 1.14 (1.10–1.18) | 25,423 | 0.42 | 0.051 (0.037–0.065) | 1,301 (942–1,646) |
| Quintile 3 | Reference | 4,739 | 0.08 | Reference | Reference |
| Quintile 4 | 0.80 (0.77–0.83) | 14,563 | 0.24 | N/A | N/A |
| Quintile 5 | 0.68 (0.64–0.72) | 1,940 | 0.03 | N/A | N/A |
|
| |||||
| Overall | 60,223 | 1.00 | 0.105 (0.085–0.125) | 2,037 (1,583–2,475) | |
Abbreviations: CI = confidence interval, HIV = human immunodeficiency virus, N/A = not applicable.
Adjusted for age, calendar year, race/ethnicity, and sex.
DISCUSSION
We identified significant interstate differences in US HIV case-fatality rates, with rates in many southern states being more than twice as great as those in other states even after adjusting for differences in racial/ethnic and age distributions. Substantial rank differences between case-fatality rates and conventional death rates in some states imply important differences in primary versus secondary and tertiary HIV prevention in these areas. For example, New York’s conventional HIV death rate was the third highest among the states examined, attributable in part to its high HIV prevalence[21]. Its comparatively low case-fatality rate rank (30th out of the 37 states) suggests good secondary and tertiary prevention of HIV disease, which could be due in part to earlier screening or entry into care, better adherence to medical instructions, or better care, compared to many other states. In contrast, Wyoming has a relatively low conventional HIV death rate, ranking 36th, owing to its low HIV prevalence. However, its high HIV case-fatality rate rank (9th) suggests that services to those with HIV may be inadequate.
The elimination of HIV-related health disparities is a national priority[4]. Our study shows that state of residence should be considered as a geographic unit of analysis when assessing disparities, in addition to categorizations like sex, race/ethnicity, and transmission category. Our findings also support earlier work identifying disparities in the southern US for earlier consequences of HIV infection, namely AIDS diagnosis[22]. Examination of these rate disparities is a crucial step in addressing their causes, and can guide policymakers to consider area-level factors as well as individual factors when choosing interventions[23].
Why do HIV case-fatality rates vary among states? Delayed diagnosis of HIV infection, which has been found to differ by state of residence[18], may be attributed to geographic differences in the patient perception of risk for HIV and the benefits of testing, in how screening is done[24], or both. However, our analyses found that case-fatality rate rankings did not change substantively after controlling for available measures of late diagnosis, suggesting that the role of late diagnosis may be less important at the state level than other factors. However, future work with more complete data on late diagnosis should explore this relationship further. Following diagnosis, differences in the receipt of HAART could play a role, given known regional disparities in medical care among those with HIV infection[25]. Potential drivers for these differences include socioeconomic status[26], the prevalence of drug abuse or other psychopathologic impediments to utilization of available care[27], and state health programs such as Medicaid and AIDS Drug Assistance Programs (ADAPs)[28, 29].
Because public health insurance programs vary among US states, geographic disparities in morbidity and mortality may be more pronounced in the US than in resource-rich countries with geographically uniform national health insurance programs. We could not easily find information on population-based case-fatality rates in the literature or on government websites at similar jurisdictional levels for other countries such as Canada, Australia, or the United Kingdom. We speculate that this is because of limited data availability at this level or a perception that such jurisdictional boundaries may not be relevant in these countries. Such data are even scarcer in resource-poor countries. In the absence of these data, HIV case-fatality rates based on cohort studies in other resource-rich countries during a similar time period fall in the lower quartiles of the US rates calculated in our study. For example, crude rates reported based on cohorts in Australia and in Europe were 5.9 and 15 per 1,000 person-years, respectively[30, 31], compared with our overall rate of 20.6/1,000 person-years. It is likely that differences in the characteristics of patients participating in cohort studies versus those assessed through surveillance contribute to these disparities, but other factors such as differences in health care systems may also play a role.
There are some limitations to our analysis. First, data from 13 US states and the District of Columbia were not included because confidential name-based reporting of HIV infection had not yet been fully established in these areas. However, the analysis covers over two-thirds of the 50 states, representing 70% of the US population, to provide timely information for current efforts to prevent morbidity and mortality. Second, only limited data were available to assess potential contributors to the association between state of residence and HIV case-fatality rates. Many known characteristics were adjusted for, but data on other characteristics associated with HIV-related mortality, such as socioeconomic status, type of health insurance, and risk behaviors (e.g., drug abuse), were unavailable. Third, like all PAF analyses, we make an assumption that interventions to reduce state homogeneity would have a causal impact on the case-fatality rate[32]. The conclusions from these analyses should be considered exploratory.
Another possible limitation is that the calculations may be inaccurate if our data on the numbers of HIV-related deaths or the numbers of persons living with HIV infection were inaccurate. For instance, rates could be overestimated if denominators were undercounted. Our method takes into account state differences in reporting delay[33], but not incomplete reporting. While reporting of HIV infection diagnoses in the US has been found to be reasonably complete[34], surveillance does not capture the estimated 20% of living HIV-infected persons who are undiagnosed[35], which could disproportionately include certain populations (e.g., foreign-born persons)[36]. Conversely, rates could be underestimated if the denominator were overcounted because some reported HIV-infected persons were erroneously assumed to be still living in a particular state when they had moved to another state, or their deaths were not reported to HARS. We believe such errors to be small, given existing knowledge about migration patterns among HIV-infected persons[37] and the comprehensiveness of death ascertainment procedures[38]. Finally, rates could be underestimated if the numerator were undercounted because HIV infection was wrongly not reported on some death certificates. Failure to report HIV on death certificates rarely happens, however, when they mention an AIDS-defining disease (e.g., pneumocystosis). Unpublished data on causes of death for HIV cases in HARS registries of two states found that 85% of case death certificates that mentioned an AIDS-defining disease also mentioned HIV.
Ultimately, monitoring state-specific HIV case-fatality rates could contribute to improved allocation of national and state resources for HIV-related care by focusing attention on states where better secondary and tertiary prevention of HIV disease is needed, such as those in the southern US. Effective interventions are needed to address these interstate disparities as part of a comprehensive approach to controlling the HIV epidemic[4, 39].
Acknowledgments
This analysis was funded in part by National Institutes of Health (NIH) grants F31-DA-030254, U01-AI-042590, and U01-AI-069918. The findings and conclusions are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
We thank the health departments of the 37 US states that contributed data to this analysis. This analysis was funded in part by National Institutes of Health grants F31-DA-030254, U01-AI-042590, and U01-AI-069918. The funding groups had no role in the study or the decision to approve publication of the finished manuscript.
D.B.H. conceived and designed the study, acquired the NVSS data, conducted the main analysis, and drafted the article. R.M.S. and S.J.G. provided advice on the study design. T.T. converted the individual-level HARS data to summary counts for the analyses. All authors contributed substantially to the interpretation of the data, revised the article critically for important intellectual content, and gave approval of the final version. D.B.H. had full access to all the data in the study, except for individual-level HARS data, and takes responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1.Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F, et al. Estimated HIV incidence in the United States, 2006–2009. PLoS One. 6:e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Palella FJ, Jr, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338:853–860. doi: 10.1056/NEJM199803263381301. [DOI] [PubMed] [Google Scholar]
- 3.French AL, Gawel SH, Hershow R, Benning L, Hessol NA, Levine AM, et al. Trends in mortality and causes of death among women with HIV in the United States: a 10-year study. J Acquir Immune Defic Syndr. 2009;51:399–406. doi: 10.1097/QAI.0b013e3181acb4e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Office of National AIDS Policy. [Accessed 15 Jul 2010];National HIV/AIDS Strategy for the United States. http://www.whitehouse.gov/administration/eop/onap/nhas.
- 5.Cunningham PJ, Kemper P. Ability to obtain medical care for the uninsured: how much does it vary across communities? JAMA. 1998;280:921–927. doi: 10.1001/jama.280.10.921. [DOI] [PubMed] [Google Scholar]
- 6.Lochner K, Pamuk E, Makuc D, Kennedy BP, Kawachi I. State-level income inequality and individual mortality risk: a prospective, multilevel study. Am J Public Health. 2001;91:385–391. doi: 10.2105/ajph.91.3.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xu KT. State-level variations in income-related inequality in health and health achievement in the US. Soc Sci Med. 2006;63:457–464. doi: 10.1016/j.socscimed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 8.Hellinger FJ, Fleishman JA. Location, race, and hospital care for AIDS patients: An analysis of 10 states. Inquiry. 2001;38:319–330. doi: 10.5034/inquiryjrnl_38.3.319. [DOI] [PubMed] [Google Scholar]
- 9.Fleishman JA, Hellinger FH. Recent trends in HIV-related inpatient admissions 1996–2000: a 7-state study. J Acquir Immune Defic Syndr. 2003;34:102–110. doi: 10.1097/00126334-200309010-00015. [DOI] [PubMed] [Google Scholar]
- 10.Xu JQ, Kochanek KD, Murphy SL, Tejada-Vera B. Deaths: Final data for 2007. Natl Vital Stat Rep. 2010;58:1–135. http://www.cdc.gov/NCHS/data/nvsr/nvsr58/nvsr58_19.pdf. [PubMed] [Google Scholar]
- 11.Glynn MK, Lee LM, McKenna MT. The status of national HIV case surveillance, United States 2006. Public Health Rep. 2007;122 (Suppl 1):63–71. doi: 10.1177/00333549071220S110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention. Guidelines for national human immunodeficiency virus case surveillance, including monitoring for human immunodeficiency virus infection and acquired immunodeficiency syndrome. MMWR Recomm Rep. 2009;48(RR-13):1–31. [PubMed] [Google Scholar]
- 13.Song R, Hall HI, Frey R. Uncertainties associated with incidence estimates of HIV/AIDS diagnoses adjusted for reporting delay and risk redistribution. Stat Med. 2005;24:453–464. doi: 10.1002/sim.1935. [DOI] [PubMed] [Google Scholar]
- 14.National Center for Health Statistics. [Accessed 8 Nov 2009];National Vital Statistics System: NCHS data release and access policy for micro-data and compressed vital statistics files. http://www.cdc.gov/nchs/about/major/dvs/NCHS_DataRelease.htm.
- 15.World Health Organization. [Accessed 22 Jun 2010];International Classification of Diseases (ICD) http://www.who.int/classifications/icd/en/
- 16.U.S. Census Bureau. [Accessed 31 Jan 2010];Population estimates. http://www.census.gov/popest/estimates.html.
- 17.Heron M, Hoyert DL, Murphy SL, Xu J, Kochanek KD, Tejada-Vera B. Deaths: Final data for 2006. Natl Vital Stat Rep. 2009;57:1–135. http://www.cdc.gov/nchs/data/nvsr/nvsr57/nvsr57_14.pdf. [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Vital signs: HIV testing and diagnosis among adults--United States, 2001–2009. MMWR Morb Mortal Wkly Rep. 2010;59:1550–1555. [PubMed] [Google Scholar]
- 19.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health. 1998;88:15–19. doi: 10.2105/ajph.88.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Graubard BI, Flegal KM, Williamson DF, Gail MH. Estimation of attributable number of deaths and standard errors from simple and complex sampled cohorts. Stat Med. 2007;26:2639–2649. doi: 10.1002/sim.2734. [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention. [Accessed 22 Jun 2010];HIV Surveillance Report. 2008 20 http://www.cdc.gov/hiv/surveillance/resources/reports/2008report/index.htm. [Google Scholar]
- 22.Peterman TA, Lindsey CA, Selik RM. This place is killing me: a comparison of counties where the incidence rates of AIDS increased the most and the least. J Infect Dis. 2005;191 (Suppl 1):S123–126. doi: 10.1086/425284. [DOI] [PubMed] [Google Scholar]
- 23.Morin SF, Kelly JA, Charlebois ED, Remien RH, Rotheram-Borus MJ, Cleary PD. Responding to the National HIV/AIDS Strategy: Setting the research agenda. J Acquir Immune Defic Syndr. 2011 doi: 10.1097/QAI.0b013e318222c0f9. Epub ahead of print 2011 May 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55:1–17. [PubMed] [Google Scholar]
- 25.Shapiro MF, Morton SC, McCaffrey DF, Senterfitt JW, Fleishman JA, Perlman JF, et al. Variations in the care of HIV-infected adults in the United States: Results from the HIV Cost and Services Utilization Study. JAMA. 1999;281:2305– 2315. doi: 10.1001/jama.281.24.2305. [DOI] [PubMed] [Google Scholar]
- 26.McDavid Harrison K, Ling Q, Song R, Hall HI. County-level socioeconomic status and survival after HIV diagnosis, United States. Ann Epidemiol. 2008;18:919–927. doi: 10.1016/j.annepidem.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 27.Lucas GM, Gebo KA, Chaisson RE, Moore RD. Longitudinal assessment of the effects of drug and alcohol abuse on HIV-1 treatment outcomes in an urban clinic. AIDS. 2002;16:767–774. doi: 10.1097/00002030-200203290-00012. [DOI] [PubMed] [Google Scholar]
- 28.Bhattacharya J, Goldman D, Sood N. The link between public and private insurance and HIV-related mortality. J Health Econ. 2003;22:1105–1122. doi: 10.1016/j.jhealeco.2003.07.001. [DOI] [PubMed] [Google Scholar]
- 29.Johri M, David Paltiel A, Goldie SJ, Freedberg KA. State AIDS Drug Assistance Programs: Equity and efficiency in an era of rapidly changing treatment standards. Med Care. 2002;40:429–441. doi: 10.1097/00005650-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Petoumenos K, Law MG. Risk factors and causes of death in the Australian HIV Observational Database. Sex Health. 2006;3:103–112. doi: 10.1071/sh05045. [DOI] [PubMed] [Google Scholar]
- 31.Mocroft A, Ledergerber B, Katlama C, Kirk O, Reiss P, d'Arminio Monforte A, et al. Decline in the AIDS and death rates in the EuroSIDA study: an observational study. Lancet. 2003;362:22–29. doi: 10.1016/s0140-6736(03)13802-0. [DOI] [PubMed] [Google Scholar]
- 32.Levine BJ. The other causality question: estimating attributable fractions for obesity as a cause of mortality. Int J Obes (Lond) 2008;32 (Suppl 3):S4–7. doi: 10.1038/ijo.2008.81. [DOI] [PubMed] [Google Scholar]
- 33.Green TA. Using surveillance data to monitor trends in the AIDS epidemic. Stat Med. 1998;17:143–154. doi: 10.1002/(sici)1097-0258(19980130)17:2<143::aid-sim757>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 34.Hall HI, Song R, Gerstle JE, 3rd, Lee LM. Assessing the completeness of reporting of human immunodeficiency virus diagnoses in 2002–2003: capture-recapture methods. Am J Epidemiol. 2006;164:391–397. doi: 10.1093/aje/kwj216. [DOI] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. HIV prevalence estimates--United States, 2006. MMWR Morb Mortal Wkly Rep. 2008;57:1073–1076. [PubMed] [Google Scholar]
- 36.Chen NE, Gallant JE, Page KR. A systematic review of HIV/AIDS survival and delayed diagnosis among Hispanics in the United States. J Immigr Minor Health. 2011 doi: 10.1007/s10903-011-9497-y. Epub Jul 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Agee BS, Funkhouser E, Roseman JM, Fawal H, Holmberg SD, Vermund SH. Migration patterns following HIV diagnosis among adults residing in the nonurban Deep South. AIDS Care. 2006;18 (Suppl 1):S51–58. doi: 10.1080/09540120600839355. [DOI] [PubMed] [Google Scholar]
- 38.Hanna DB, Pfeiffer MR, Sackoff JE, Selik RM, Begier EM, Torian LV. Comparing the National Death Index and the Social Security Administration's Death Master File to ascertain death in HIV surveillance. Public Health Rep. 2009;124:850–860. doi: 10.1177/003335490912400613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Frieden TR, Das-Douglas M, Kellerman SE, Henning KJ. Applying public health principles to the HIV epidemic. N Engl J Med. 2005;353:2397–2402. doi: 10.1056/NEJMsb053133. [DOI] [PubMed] [Google Scholar]