Abstract
Influenza virus entry is mediated by the acidic-pH-induced activation of hemagglutinin (HA) protein. Here, we investigated how a decrease in the HA activation pH (an increase in acid stability) influences the properties of highly pathogenic H5N1 influenza virus in mammalian hosts. We generated isogenic A/Vietnam/1203/2004 (H5N1) (VN1203) viruses containing either wild-type HA protein (activation pH 6.0) or an HA2-K58I point mutation (K to I at position 58) (activation pH 5.5). The VN1203-HA2-K58I virus had replication kinetics similar to those of wild-type VN1203 in MDCK and normal human bronchial epithelial cells and yet had reduced growth in human alveolar A549 cells, which were found to have a higher endosomal pH than MDCK cells. Wild-type and HA2-K58I viruses promoted similar levels of morbidity and mortality in C57BL/6J mice and ferrets, and neither virus transmitted efficiently to naive contact cage-mate ferrets. The acid-stabilizing HA2-K58I mutation, which diminishes H5N1 replication and transmission in ducks, increased the virus load in the ferret nasal cavity early during infection while simultaneously reducing the virus load in the lungs. Overall, a single, acid-stabilizing mutation was found to enhance the growth of an H5N1 influenza virus in the mammalian upper respiratory tract, and yet it was insufficient to enable contact transmission in ferrets in the absence of additional mutations that confer α(2,6) receptor binding specificity and remove a critical N-linked glycosylation site. The information provided here on the contribution of HA acid stability to H5N1 influenza virus fitness and transmissibility in mammals in the background of a non-laboratory-adapted virus provides essential information for the surveillance and assessment of the pandemic potential of currently circulating H5N1 viruses.
INTRODUCTION
Influenza A virus is a negative-sense, single-stranded RNA virus of the family Orthomyxoviridae. Its genome consists of eight segments encoding at least 16 proteins (1–6). Being an RNA virus with a segmented genome, influenza virus is characterized by a high mutation rate and the ability to reassort its genome segments with other viruses (3, 7). These two properties allow the virus to constantly evolve and sustain in its original host and to adapt to new hosts (5, 8). These two properties also contribute to the large diversity among influenza A viruses and their propensity to infect a broad range of hosts, including members of avian (e.g., shorebirds, ducks, chickens, etc.) and mammalian (e.g., horses, pigs, dolphins, seals, humans, etc.) species (5).
Annual outbreaks in humans are currently caused by influenza A viruses of the H1N1 and H3N2 subtypes. Periodically, a new influenza virus subtype crosses the species barrier and causes a pandemic; the 2009 H1N1 pandemic is the most recent example (8, 9). Viruses that occasionally cross the host barrier and cause infections in humans are of concern due to their potential to adapt to humans and become pandemic. H5, H7, and H9 influenza viruses have recently been reported in humans (10–14). Of great concern is avian H5N1 influenza virus.
Since 2003, H5N1 influenza viruses have been actively evolving and diversifying, causing outbreaks in wild and domestic birds in Asia, Africa, and Europe and becoming endemic in poultry in Egypt and Indonesia (15–17). As of 26 April 2013, 628 human infections of H5N1 have been documented, of which approximately 60% have resulted in death (http://www.who.int/influenza/human_animal_interface/). While most of the human cases were due to contact with poultry or consumption of undercooked poultry meat or blood (18), a few cases of human-to-human transmission have been reported (18–20). Despite a limited number of cases of human-to-human transmission, H5N1 influenza virus remains a pandemic threat, and determining the molecular properties that contribute to its ability to adapt to humans is critical for monitoring the virus and implementing effective control measures (e.g., culling birds and selecting vaccine seed stocks). Mutations influencing the interspecies adaptation of H5N1 influenza viruses have been identified in the HA (hemagglutinin), NA (neuraminidase), and PB2 (basic polymerase) proteins (8, 21, 22). Of these, the HA protein is reportedly the most important determinant of host adaptation and transmission of H5N1 influenza virus (21, 23–25) and is an essential component in the emergence of pandemic influenza.
The HA protein is a metastable class I membrane fusion protein. It is posttranslationally cleaved into two subunits: the HA1 subunit, which harbors the receptor binding globular head domain, and the HA2 subunit, which comprises the majority of the fusogenic stalk domain (26–28). During viral entry, the HA protein binds to sialic acid-containing cell-surface receptors, and the virus is internalized into the endosomes (26, 29). Low pH in the endosomes triggers irreversible conformational changes in the HA protein that mediate fusion of the viral and endosomal membranes, enabling delivery of viral RNA into the host cell (26).
For various influenza virus subtypes, mutations altering the pH at which the HA protein is activated for membrane fusion have been associated with altered virulence in mice (30–35) and interspecies adaptation (35–40). Our previous work has shown that efficient growth and transmission of H5N1 influenza viruses in avian species is associated with a relatively high HA activation pH, ranging from pH 5.6 to 6.0 (39, 41, 42). Moreover, we found that an HA2-K58I mutation (K to I at position 58) that decreases the HA activation pH of A/chicken/Vietnam/C58/2004 (H5N1) from 5.9 to 5.4 supports enhanced and prolonged replication in the murine upper respiratory tract (URT) while simultaneously reducing replication and eliminating transmission in mallards (35, 43). Similarly, a decrease in the HA activation pH also coincided with enhanced replication of NS1 deletion mutant H5 and H3 influenza viruses in the URT of mice (44, 45).
Avian influenza viruses such as H5N1 tend to bind preferentially to α(2,3)-linked sialic acid receptors, while human viruses favor sialic acid receptors in an α(2,6) orientation (46–49). Nonetheless, some recent H5N1 viruses have acquired the ability to bind α(2,6)-linked sialic acid receptors while still maintaining high binding affinity to the α(2,3) form (48). A gain of α(2,6) receptor binding specificity alone has not been sufficient to promote H5N1 transmission in ferrets, the standard model for human transmission of influenza viruses (21, 50, 51). A few studies investigated whether a complete switch to α(2,6) binding is sufficient to support efficient airborne transmission of H5N1 influenza virus. Chen et al. showed that, with the proper HA-NA balance, a mutated H5 virus with α(2,6) receptor binding specificity supported only partial transmission via respiratory droplets (21).
Two recent studies showed that efficient airborne transmission of H5-containing influenza viruses occurred following a series of mutations that first switched receptor binding specificity to α(2,6), then deleted a glycosylation site, and last decreased the pH of activation of the HA protein (determined either by direct measurement or by structural considerations) (24, 25). While a decrease in the activation pH of the HA protein was found to be necessary for airborne transmissibility of H5 viruses in ferrets, it is unknown whether this adaptation alone is sufficient to increase the transmissibility of circulating H5N1 influenza viruses in mammals. The goal of the current study was to determine how a single acid-stabilizing HA protein mutation influences in vivo infection in mice and ferrets when introduced into the background of an unmodified H5N1 influenza virus that has not been laboratory adapted, reassorted, or mutated to have α(2,6) receptor binding specificity.
The rationale for this work was to enhance our ability to assess the likelihood that currently circulating avianlike H5N1 influenza viruses may acquire the ability to jump species to humans and potentially cause a pandemic. This is important in conducting surveillance, performing risk assessment of currently circulating viruses, making decisions to quarantine humans, and selecting prepandemic vaccine seed stocks. Furthermore, knowledge of the molecular properties that govern the efficient growth of H5N1 influenza virus in one cell type, tissue, or host species versus another is expected to help optimize vaccine yield and efficacy and may suggest novel ways to treat infection.
MATERIALS AND METHODS
Ethics statement.
All animal studies were approved by the Animal Care and Use Committee of St. Jude Children's Research Hospital (protocol 464) and were performed in compliance with relevant institutional policies, Association for the Accreditation of Laboratory Animal Care guidelines, National Institutes of Health regulations, and local, state, and federal laws.
Plasmids.
pHW2000 plasmids containing individual genome segments of the wild-type (WT) A/Vietnam/1203/04 (H5N1) (VN1203) influenza virus have been described previously (52). The HA2-K58I point mutation was introduced using a QuikChange site-directed mutagenesis kit (Stratagene) according to the manufacturer's instructions. To perform in vitro expression of the surface glycoproteins, the HA and NA genes were subcloned into the pCAGGS expression vector using gene-specific primers, with ClaI and XhoI site overhangs at the 5′ and 3′ end, respectively (43).
Viruses.
rg-VN1203-HA-WT and rg-VN1203-HA2-K58I viruses were generated by using reverse genetics (rg) as previously described (53). Briefly, eight pHW2000 plasmids, each containing an individual gene of the eight influenza A virus genes, were transfected into cocultured MDCK (Madin-Darby canine kidney) and 293T cells. Virus was then harvested, plaque purified on MDCK cells, and propagated in 10-day-old embryonated chicken eggs. Virus identity was confirmed by performing full-genome sequencing at the Hartwell Center for Bio-informatics and Biotechnology at St. Jude Children's Research Hospital.
Transient expression of HA and NA proteins.
Vero cells at 70 to 80% confluence were transfected with pCAGGS HA (1.0 μg) and pCAGGS NA (0.1 μg) plasmids by using a Lipofectamine plus expression system (Invitrogen) (54). The cells were then incubated at 37°C for 4 h before the transfection medium was replaced with Dulbecco's modified Eagle's medium (DMEM) containing 10% fetal bovine serum. The cells were incubated for 16 h at 37°C to allow the expression of the HA and NA proteins.
HA protein activation pH.
Monolayers of Vero cells expressing the HA protein on their surface were washed with phosphate-buffered saline plus calcium and magnesium (PBS+) and treated for 5 min with 500 μl PBS+ that was adjusted to the desired pH using 0.1 M citric acid. The cells were then neutralized with DMEM and incubated for another 2 h at 37°C. The cells were then fixed and stained by using a Hema 3 stat pack staining kit (Fisher) according to the manufacturer's instructions. The pH of conformational change was determined by using Vn04-16 conformation-specific monoclonal antibody as previously described (41, 43).
Total and surface expression.
HA-expressing Vero cells were lysed using radioimmunoprecipitation (RIPA) buffer containing 10 mg/ml iodoacetamide and protease inhibitors (43). Clarified lysates were resolved on 4 to 12% NuPAGE Bis-Tris polyacrylamide-SDS gels (Invitrogen) and transferred onto polyvinylidene difluoride (PVDF) membranes. The membranes were blotted using polyclonal HA antibody A0110 (43), and bands were visualized using horseradish peroxidase (HRP)-conjugated anti-rabbit antibody on X-ray films. Flow cytometric analysis of the surface expression of the HA protein was performed by using VN04-02 monoclonal antibody as described previously (43).
Hemadsorption.
Vero cells expressing the HA protein on their surface were washed two times with PBS+, overlaid with 1% chicken or turkey erythrocytes, and incubated at 37°C for 30 min. Monolayers were washed 3 times with DMEM (phenol red free) to remove unbound red blood cells (RBS) and lysed with RBC lysis buffer. The amount of bound erythrocytes was determined by measuring the absorbance of clarified lysate at 415 nm by using a Synergy-2 multimode microplate reader (BioTek).
Receptor binding specificity assay.
We used a solid-phase binding assay to measure the receptor binding specificity of the HA protein for α(2,3)- or α(2,6)-linked sialic acid. Briefly, plates were coated with 10 mg/ml fetuin (Sigma) overnight at 4°C and then washed with PBS (without calcium and magnesium) and blocked with 0.1 ml of PBS containing 2% bovine serum albumin (Sigma) at room temperature for 1 h. Plates were washed 3 times with PBS and incubated with 100 μl virus (64 HA units) overnight at 4°C to allow binding of the virus to the plates. Unbound virus was aspirated, and the plates were washed three times with PBS before the addition of a biotinylated sialylglycopolymer containing either an α(2,3) (Neu5Acα2,3Galβ1,4GlcNAcβ1-pAP) or an α(2,6) (Neu5Acα2,6Galβ1,4GlcNAcβ1-pAP) sialic acid for 3 h at 4°C. After washing three times with PBS, plates were incubated with horseradish peroxidase (HRP)-conjugated streptavidin (diluted 1:1,000; Invitrogen) for 1 h at room temperature. After washing with PBS 5 times, the plates were incubated with 50 μl of tetramethylbenzidine (TMB) substrate for 10 min at room temperature. The reaction was stopped with 50 μl of 50 mM HCl, and the optical density was measured at 450 nm.
Resistance to acid inactivation.
The acid stabilities of the viruses were measured by determining the susceptibility of each virus to acid inactivation. Virus was diluted in PBS+ adjusted to the desired pH (4.5 to 6.0 pH) by using 0.1 M citric acid. Then, samples were incubated at 37°C for 1 h. The titer of remaining infectious virus was determined in MDCK cells by using the 50% tissue culture infectious dose (TCID50) assay. The method of Reed and Muench was used to estimate the TCID50/ml of virus (55).
In vitro virus growth kinetics.
MDCK (ATCC CRL-2936), A549 (human lung carcinoma; ATCC CCL-185), and NHBE (normal human bronchial epithelium; Lonza CC-2540) cells were infected with WT and HA2-K58I viruses at a multiplicity of infection (MOI) of 0.01 PFU/cell. One hour postincubation, cells were washed twice with PBS+ to remove nonbound virus particles and incubated at 37°C. To compare the growth kinetics of the two viruses, 100-μl samples of culture supernatant were collected at 10, 24, 48, and 72 h postinfection and titrated in MDCK cells by using the TCID50 assay.
Endosomal pH.
The endosomal pHs of MDCK and A549 cell lines were compared by using a pH-sensitive endosomal dye, pHrodo red dextran (Invitrogen), according to the manufacturer's recommendations. Briefly, MDCK or A549 cells were washed and suspended in warm PBS+ buffer. The cells (106) were then incubated at 37°C in the presence of 40 μg/ml of the dye for 15 min. The cells were washed and suspended in warm PBS+ buffer, and the intensity of fluorescence was measured by using flow cytometry. Quantitative measurement of the endosomal pH was performed as previously described (56), with some modifications. Briefly, cells were washed twice with PBS and incubated with 5 mg/ml fluorescein-TMR (tetramethylrhodamine)-tagged dextran (Invitrogen) for 20 min at 37°C, and then cells were washed 5 times with PBS and imaged in phenol red-free DMEM medium. For endosomal pH calibration, after the dye uptake, the cells were incubated in freshly prepared calibration buffer (120 mM KCl, 20 mM NaCl, 1 mM CaCl2, 1 mM Mg2Cl, and 10 mM HEPES for pH values 6.5 to 7.0 or 10 mM MES [morpholineethanesulfonic acid] for pH values 4.0 to 6.0) containing 10 μM nigericin and 10 μM monensin ionophores for 20 min. The cells were imaged on a Nikon TE2000 E2 microscope equipped with a Nikon C2 confocal scan head. Excitation was with 488-nm and 561-nm diode-pumped solid-state (DPSS) lasers, and emission was collected through 515/30 and 605/75 band pass filters. Images were acquired with a Nikon 40× 1.3 numerical aperture Plan Fluor objective and using Nikon NIS Elements software. Cells were maintained at 37°C, 5% CO2 during imaging. The pH was estimated as the intensity ratio of TMR (red) and fluorescein (green) fluorescence. Curve fitting was performed as previously described (56).
Animal experiments.
To determine the 50% mouse lethal dose (MLD50), groups of 7-week-old female C57BL/6J mice (Jackson Laboratory) were intranasally inoculated with 50 μl of 10-fold serial dilutions of WT VN1203 virus. To compare the virulence and replication of the WT and HA2-K58I viruses, mice were infected with 50 μl or 5 μl of PBS+ containing ∼1 MLD50 (∼150 50% egg infectious doses [EID50/ml]). The mice were then weighed and observed daily. Mice showing severe weight loss (>25%) or illness (e.g., hind limb paralysis) were euthanized for humane reasons. To determine virus dissemination, mice were euthanized and tissues, including nasal cavities, trachea, lungs, brain, and kidneys, were collected. Tissues were homogenized in PBS and titrated in 10-day-old embryonated chicken eggs. Viral loads were expressed as EID50/ml, calculated by the method of Reed and Muench (55). For contact transmission experiments, 3-month-old male ferrets (Triple F farms) that were seronegative to influenza A viruses circulating in humans were used. The ferrets were anesthetized with isoflurane and inoculated intranasally with 1,000 TCID50 in 0.5 ml PBS. Twenty-four hours postinfection, two naive ferrets were introduced into a cage containing one inoculated donor ferret. Ketamine was used to induce sneezing in the ferrets to collect nasal washes. The ferrets were observed daily. Ferrets that lost >25% of their starting weight and/or were severely ill (e.g., paralysis) were humanely euthanized. On day 5 postinfection, three directly inoculated ferrets from each virus group were sacrificed and tissues were collected to determine viral loads. All animal experiments were carried out under applicable laws and guidelines and were approved by St. Jude Children's Research Hospital Animal Care and Use Committee.
Serologic testing.
To test for potential seroconversion, serum was collected from contact ferrets on day 20 postcontact. Serum samples were treated with receptor-destroying enzyme (Seiken) overnight at 37°C to destroy nonspecific receptors, heat inactivated at 56°C for 30 min, and tested using the hemagglutination inhibition (HI) assay as described in the WHO animal influenza training manual (57). The HI assay was performed using VN1203 virus and 0.5% chicken red blood cells.
Biosafety and biosecurity.
All work with highly pathogenic H5N1 influenza was performed in an enhanced animal biosafety level 3 (ABSL3+) laboratory that is select agent approved and routinely inspected by both institutional biosafety and USDA officials. The ABSL3+ facility has entry and exit access control with both a card scanner and biometric fingerprint reader. Personnel enter through a shower area and then take off all items and wear a scrub suit, Tyvek suit, disposable outer gown, gloves, and powered air-purifying respirators with HEPA filters for the breathing air. All rooms are under negative air pressure, and there is a double-door autoclave, double-HEPA-filtered air exhaust, and security cameras placed throughout the laboratory. All in vitro work is performed in class II biosafety cabinets, and animal work is performed in negative-pressurized flexible-film isolators. All personnel are required to shower upon exit and comply with a quarantine policy to prevent outside contact with birds or immunocompromised hosts. Only personnel who receive training with highly pathogenic avian H5N1 influenza virus and who receive select agent security clearance can access the facility. ABSL3+ personnel also receive annual refresher training to ensure adherence to regulations. Emergency plans are in place, and annual drills are performed to minimize biological risks and ensure personnel safety. The virus inventory is secured in locked freezers and is under constant security monitoring. The laboratory manager controls access to the virus inventory, and a logbook and database of the inventory are kept up-to-date. The ABSL3+ laboratory is inspected biannually by the USDA, is in compliance with all USDA regulations, and meets or exceeds all standards outlined in Biosafety in Microbiological and Biomedical Laboratories (58).
DUR.
All experiments with ferrets were conducted in 2011 before the moratorium on H5N1 influenza virus research. Before initiation, the Institutional Biosafety Committee of St. Jude Children's Research Hospital reviewed and approved the experiments and recommended mitigation strategies, which were subsequently implemented by the investigators. Upon completion of the studies and also after preparation of the manuscript, an internal Dual-Use Research of Concern (DURC) Committee at St. Jude Children's Research Hospital reviewed this work and concluded that the agents and results described herein are DUR but not DURC. The manuscript was also reviewed by the NIH/NIAID, the funding agency, which likewise judged this work to be DUR but not DURC.
Statistical analysis.
All statistical analyses were performed by using GraphPad Prism5 software. The t test, one-way analysis of variance (ANOVA), two-way ANOVA, or log-rank chi-square test was used to test differences between different groups. P values of <0.05 were considered statistically significant.
RESULTS
An HA2-K58I mutation decreases the HA activation pH without altering other properties.
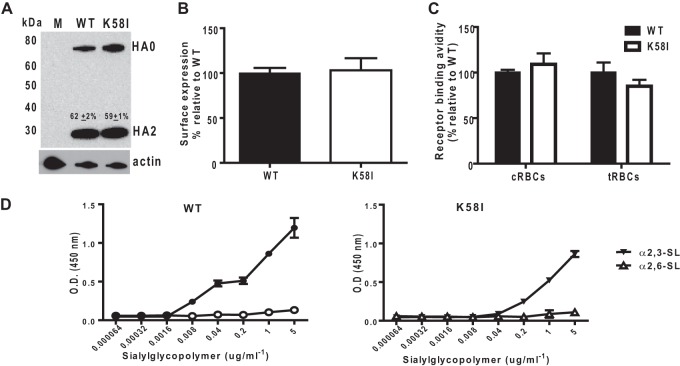
For these studies, we selected the prototypic influenza virus A/Vietnam/1203/2004 (H5N1). VN1203 has avianlike α(2,3) receptor binding specificity and a human-like PB2 K627 polymorphism (52). In ferrets, these two properties of VN1203 contribute to robust virus growth in the lungs and high virulence but no contact or airborne transmission (51, 52). We introduced into the VN1203 HA protein an HA2-K58I mutation, which we previously found to decrease by 0.5 pH units the HA activation pH of the related isolate A/chicken/Vietnam/C58/2004 (H5N1) (39, 43). Wild-type and K58I HA proteins, transiently coexpressed in Vero cells along with the NA protein, had similar levels of total and cell surface HA protein expression as determined by Western blotting and flow cytometry, respectively (Fig. 1A and B). Western blot analysis also showed no significant difference in HA protein cleavage (Fig. 1A). Both HA proteins had similar binding avidities to chicken and turkey red blood cells (Fig. 1C), suggesting similar receptor binding affinities. We compared the receptor binding specificities of the wild-type and K58I HA proteins using a solid-phase binding assay and found that both HA proteins bound exclusively to α(2,3)-linked sialic acid receptors and not to α(2,6)-linked sialic acid (Fig. 1D). Overall, the K58I mutation did not result in substantial differences in HA protein expression, cleavage, or receptor binding.
Fig 1.
Characterization of the WT and HA2-K58I HA proteins. (A) Western blot of HA expression. Values above the HA2 band express the mean percentage of HA cleavage ± standard deviation, estimated by dividing the HA2 band intensity by that of the total HA (i.e., HA0 + HA2). (B) HA surface expression as measured by flow cytometry. (C) Binding avidities of cell surface-expressed HA protein to chicken (cRBCs) or turkey (tRBCs) red blood cells, measured as the amount of hemoglobin released following lysis of bound RBCs. (D) Binding of WT or K58I virus to either an α(2,3) or α(2,6) sialylglycopolymer. O.D. (450 nm), optical density at 450 nm. Error bars show standard deviations.
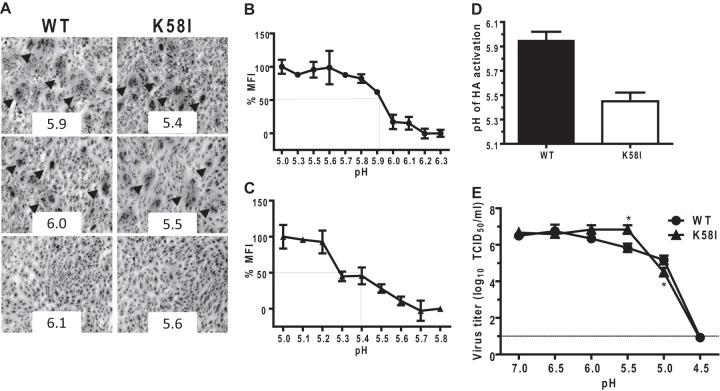
We next compared the activation pH values of the wild-type and K58I HA proteins. Vero cells expressing either the wild-type or K58I HA protein, along with the VN1203 NA protein, were pulsed with pH-adjusted buffers and either allowed to fuse for microscopic examination of syncytia (cell-to-cell fusion) or detached from tissue culture plates for flow cytometric analyses using the HA protein conformation-specific monoclonal antibody Vn04-16 (43, 59). The syncytium assay showed that wild-type HA protein was activated for membrane fusion after buffer pulses of pH 6.0 or lower, while the K58I mutant was not triggered for membrane fusion unless the pH pulse was reduced to pH 5.5 or lower (Fig. 2A). Flow cytometry showed that the midpoint of acid-induced conformational changes for wild-type HA protein was pH 5.9, while the midpoint for the K58I HA protein was reduced to pH 5.4 (Fig. 2B and C). Therefore, the average HA activation pH values for wild-type and K58I HA proteins were 5.95 and 5.45, respectively (Fig. 2D). To probe whether differences in the activation pH values of the HA proteins affected their susceptibilities to acid inactivation, prestandardized reverse genetic-engineered viruses rg-VN1203-WT and rg-VN1203-HA2-K58I were exposed to buffers ranging in pH from 4.5 to 7.0 for 1 h at 37°C. The titers of the remaining infectious virus that survived the pH treatment were quantified using TCID50 (Fig. 2E). The HA2-K58I virus retained its infectivity upon exposure to buffers with pH values as low as 5.5, while the WT virus lost ∼90% (∼1 log10) of its infectious titer at pH 5.5. The infectious titers of both WT and HA2-K58I viruses declined nearly 100-fold after exposure to pH 5.0 buffer and were completely lost after exposure to pH 4.5 buffer. Overall, the results show that the K58I mutation decreases the HA activation pH of the VN1203 HA protein by 0.5 units without altering other biochemical properties, just as was observed when K58I was introduced into the background of the C58 virus isolate (39, 43).
Fig 2.
Acid stabilities of the HA proteins. (A) Micrographs of syncytium formation due to HA protein activation at various pH points in Vero cells. The arrowheads indicate syncytia. (B and C) Quantification of the HA protein conformational change at indicated pH points by using conformation-specific monoclonal antibody (VN04-16) and flow cytometry. MFI, mean fluorescence intensity. (D) Activation pHs of the HA proteins expressed as the average of the pH of syncytium formation and the pH at which 50% conformational change occurs. (E) Residual titers upon treatment of WT or HA2-K58I virus with the indicated pH buffers. Asterisks indicate P values of <0.05 using two-way ANOVA. Error bars show standard deviations.
In vitro growth of HA2-K58I virus is reduced in A549 cells due to a relatively high endosomal pH.
In the background of the C58 strain, we have previously shown that the HA2-K58I mutation attenuates the growth of H5N1 virus in A549 cells (human lung carcinoma cells) but does not alter the virus replication kinetics in MDCK (canine kidney epithelial cell line), NHBE (normal human bronchial epithelial), DF1 (chicken embryo fibroblast), and CCL-141 (duck embryo fibroblast) cells (35, 39). Similarly, we found here that the rg-VN1203-HA2-K58I virus had wild-type-like growth kinetics in MDCK (Fig. 3A) and NHBE (Fig. 3C) cells and yet grew to significantly lower virus titers (P values of <0.01, two-way ANOVA) than the wild-type after 24 h of infection in A549 cells (Fig. 3B). The decreased growth of rg-VN1203-HA2-K58I virus in A549 cells but not in MDCK cells suggested that the two cell lines may differ in their endosomal pHs. To test this hypothesis, we probed MDCK and A549 cell lines using pHrodo red, a pH-sensitive fluorescent dextran conjugate. Upon uptake into the endosomes, the fluorescence intensity of pHrodo increases as endosomal pH decreases. The mean fluorescence intensity of the pHrodo probe was 2-fold higher (P < 0.05, t test) in MDCK cells than in A549 cells (Fig. 4A), suggesting that A549 cells have a higher endosomal pH than MDCK cells. We then determined the endosomal pH quantitatively by using fluorescein-TMR double-conjugated dextran. The intensity of the fluorescein is quenched in a predictable manner under acidic conditions, while that of the TMR remains stable, thus allowing one to track endosomes and measure their pH values. We incubated MDCK and A549 cells with the double-conjugated dextran to allow uptake of the dye and then calibrated the in situ fluorescein emissions as a function of clamped cytoplasmic pH. A plot of the red/green ratio on the calibration curve revealed that MDCK cells had an endosomal pH of 5.4 and A549 cells had an endosomal pH of 5.9 (Fig. 4B). These results are consistent with the HA2-K58I virus, which has a lower HA activation pH than wild-type virus, being attenuated in A549 but not MDCK cells, while the wild-type virus is not attenuated in A549 cells.
Fig 3.
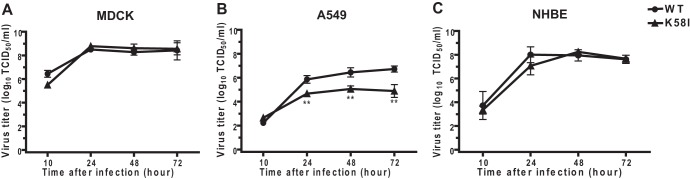
In vitro replication kinetics of rg-VN1203 wild-type (WT) and mutant viruses. MDCK (A), A549 (B), or NHBE (C) cells were infected with rg-VN1203 WT or HA2-K58I virus at an MOI of 0.01 PFU/cell. Virus titers were determined at the indicated time points in MDCK cells by using TCID50 assays. The detection limit was 1 log10 TCID50/ml. Graphs are representative of two independent experiments. Statistical analysis was performed by using two-way ANOVA. Asterisks indicate P values of <0.01. Error bars show standard deviations.
Fig 4.
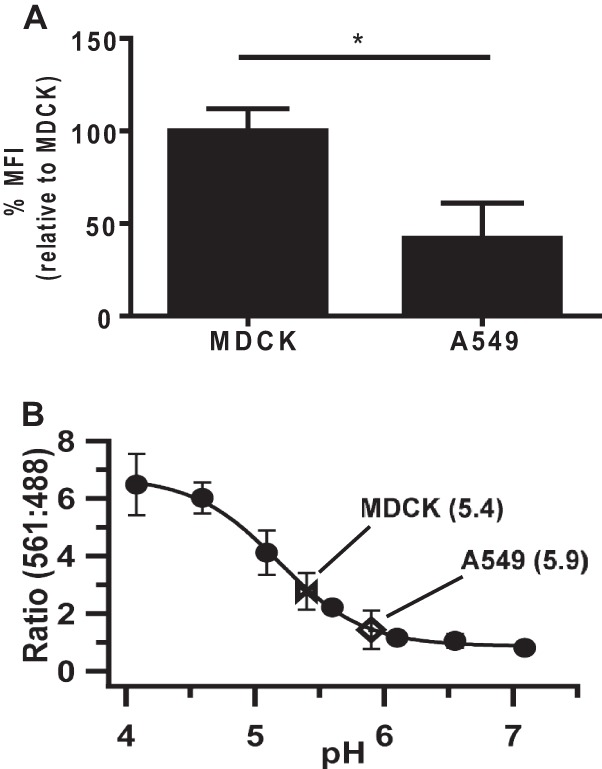
Endosomal acidification of MDCK and A549 cells. (A) pH-sensitive pHrodo dextran was used to compare the endosomal acidity of MDCK and A549 cells. Following uptake of the dye, cells were analyzed using flow cytometry to measure the intensity of pHrodo fluorescence. Data are expressed as the percentage of mean fluorescence intensity (MFI) relative to that of the MDCK cells. A higher fluorescence intensity of pHrodo correlates with a lower pH value. (B) Determination of the endosomal pH of MDCK (bowtie) and A549 (open diamond) cells. Cells were incubated with fluorescein-TMR double-conjugated dextran to allow uptake of the dye into the endosomes and then were washed and imaged by using confocal microscopy. Measurements of pH were done by using in situ calibration of fluorescein emission (closed circles) as a function of clamped endosomal pH. Clamping of endosomal pH was attained by using potassium ionophores as previously described (56). The average red (TMR, 561 nm)/green (fluorescein, 488 nm) intensities were obtained from six fields per cell line. The endosomal pH values of MDCK and A549 cells indicated on the curve were obtained by interpolation. Error bars represent standard deviations.
The HA2-K58I mutation does not alter the virulence of VN1203 in C57BL/6J mice.
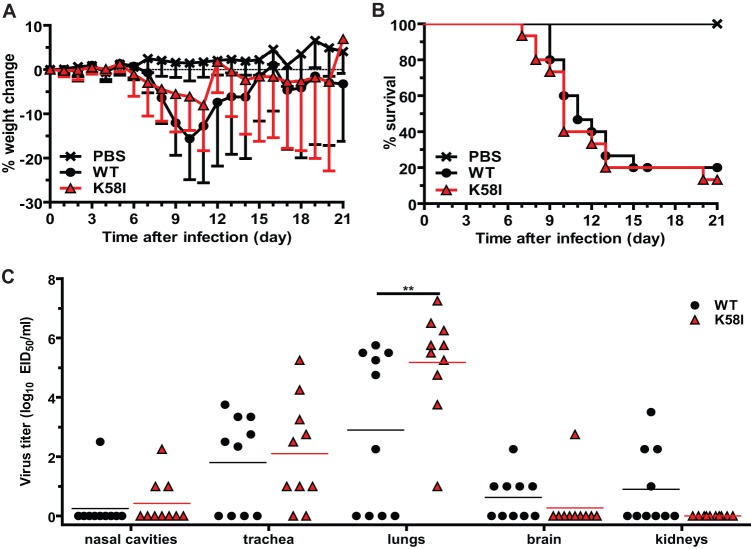
To investigate the effect of the HA2-K58I mutation on VN1203 virulence in mice, we inoculated C57BL/6J mice with 50 μl of PBS containing 150 EID50 of either rg-VN1203-WT or rg-VN1203-HA2-K58I and then either monitored the animals for weight loss and mortality (Fig. 5A and B) or euthanized the mice after 4 days of infection to measure tissue titers (Fig. 5C). Infection with HA2-K58I virus resulted in an average maximum weight loss of 8% after 11 days of infection, compared to an average maximum weight loss of 15% after 10 days of infection with WT virus; however, this difference was not statistically significant (Fig. 5A). Only 13% of mice infected with HA2-K58I virus survived infection, compared to 20% surviving infection with WT virus, a difference that was not statistically significant (Fig. 5B). Four days after the 50-μl inoculation in C57BL/6J mice, the wild-type and HA2-K58I viral loads were similar, and not robust, in the nasal cavity, trachea, and brain (Fig. 5C). Only wild-type virus was detected in the kidneys, although at low levels. In the lungs, significantly higher viral loads were detected in HA2-K58I virus-infected mice than in those infected with wild-type virus (P < 0.01, two-way ANOVA).
Fig 5.
Effect of the K58I mutation on virulence and virus growth in C57BL/6J mice following inoculation with a large volume. (A and B) Mean percentages of weight change (A) and survival (B) of C57BL/6J mice (n = 15) following intranasal inoculation with 50 μl PBS containing 1 MLD50 of the WT or HA2-K58I viruses. The control (PBS) group was inoculated with 50 μl PBS only. Error bars show standard deviations. (C) Replication of the rg-VN1203 WT and HA2-K58I viruses in different mouse tissues. Tissues were harvested from mice (n = 10) on day 4 following infection with 1 MLD50/50 μl, and the EID50/ml titers were determined in 10-day-old embryonated chicken eggs. The detection limit was 1 log10 EID50/ml. Horizontal lines within groups show mean values. Statistical analysis was performed by using two-way ANOVA for comparison of weight loss and virus titers and the log-rank chi-square test for survival curves. Asterisks indicate P values of <0.01.
Low viral loads of rg-VN1203-HA2-K58I in the murine nasal cavity were unexpected, as we had previously found that the HA2-K58I mutation increased the viral load of the C58 isolate in the URT of mice (35). However, the C58 isolate is highly attenuated in mammals compared to the infectivity of VN1203 (52), so our previous studies on rg-C58-HA2-K58I required the inoculation of a more-susceptible strain of mice (DBA/2J) with 50 μl of 2.8 × 104 EID50 of virus to observe >50% mortality (35). We considered one possible explanation for the low virus load of rg-VN1203-HA2-K58I in the nasal cavity in the present study to be the combination of a relatively low virus inoculum (150 EID50) in a rather high volume (50 μl), which would result in the retention of only a small number of infectious particles in the nasal cavity during the initiation of infection.
To investigate further the effect of the HA2-K58I mutation on VN1203 virus growth in the URT of mice, we inoculated C57BL/6J mice with 5 μl PBS containing 150 EID50 of either the WT or HA2-K58I virus. The small volume allowed maximum delivery of the inoculum to the nasal cavity at the expense of delivery to the lungs (60). A 5-μl inoculation with either the WT or HA2-K58I virus resulted in little (<10%) to no weight loss (Fig. 6A). Only one mouse in the HA2-K58I virus-infected group succumbed to infection, due to hind limb paralysis, compared to none in the WT group (Fig. 6B). After the 5 μl-inoculation, systemic spread was only observed for the HA2-K58I virus, which also had significantly higher viral loads (P < 0.05, two-way ANOVA) in the nasal cavity and trachea than did wild-type virus (Fig. 6D). Therefore, when infectious virus was delivered predominantly to the nasal cavity in a 5-μl volume, the HA2-K58I virus was found to enhance VN1203 virus growth in the murine URT.
Fig 6.
Effect of the HA2-K58I mutation on virulence and virus growth in C57BL/6J mice following inoculation with a small volume. (A and B) Mean percentages of weight change (A) and survival (B) of C57BL/6J mice (n = 5) following inoculation with a small volume (5 μl) of PBS containing 1 MLD50 of the rg-VN1203 WT or HA2-K58I virus. The control (PBS) group was inoculated with 5 μl PBS only. Error bars show standard deviations. (C) Replication of WT and HA2-K58I viruses in different mouse tissues. Tissues were harvested from mice (n = 10) on day 4 following infection with 1 MLD50/5 μl, and the EID50/ml titers were determined in 10-day-old embryonated chicken eggs. The detection limit was 1 log10 EID50/ml. Horizontal lines within groups show mean values. Statistical analysis was performed by using two-way ANOVA for comparison of weight loss and virus titers and the log-rank chi-square test for survival curves. *, P < 0.05; **, P < 0.01.
The HA2-K58I mutation enhances early growth of VN1203 in the ferret nasal cavity but does not promote productive contact transmission.
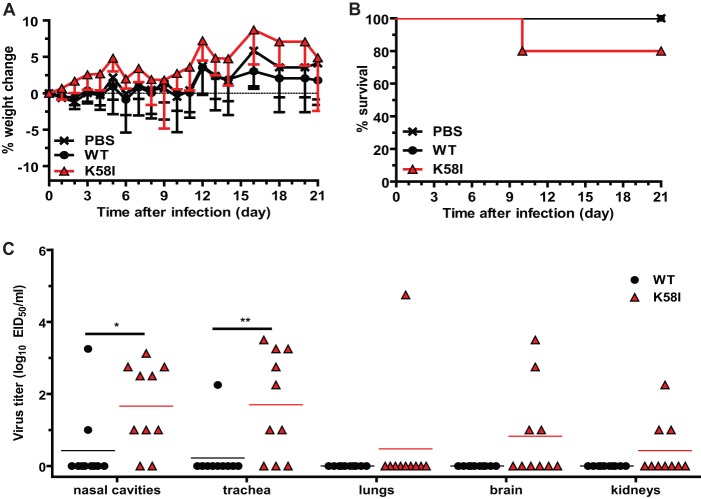
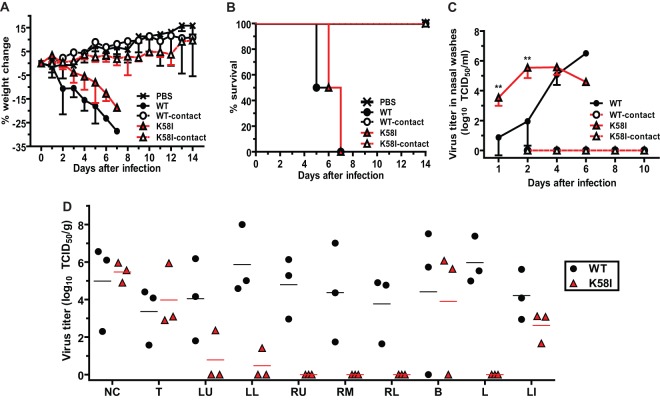
We next investigated the effect of the HA2-K58I mutation on VN1203 virus growth, virulence, and contact transmission in ferrets. For these studies, we inoculated groups of 5 ferrets intranasally with 0.5 ml of PBS containing 1,000 TCID50 of either rg-VN1203-WT or rg-VN1203-HA2-K58I. Nasal washes were performed on all 5 ferrets on days 1, 2, and 4 postinoculation. After 5 days of infection, three of the five directly inoculated ferrets were euthanized so that tissues could be recovered and viral loads could be measured. The other two inoculated ferrets were used as donor animals in contact transmission experiments in which one directly inoculated ferret was cohoused with two naive contact animals 1 day after inoculation. Ferrets directly inoculated with the HA2-K58I virus had slightly less weight loss, albeit not a significant difference, than those directly inoculated with WT virus (Fig. 7A). All ferrets directly inoculated with either virus succumbed to infection within 7 days due to severe weight loss or were euthanized because of hind limb paralysis (Fig. 7B).
Fig 7.
Effects of the K58I mutation on virulence, replication, and contact transmission of H5N1 influenza virus in ferrets. (A and B) Ferrets (n = 5) were inoculated with 0.5 ml PBS containing 103 TCID50 of the WT or HA2-K58I viruses. Two of the 5 directly inoculated ferrets and all contact ferrets (n = 4) were observed for (A) weight loss and (B) survival. (C) Virus replication in the nasal cavities. Nasal washes were collected from all ferrets on the indicated days until death or termination of the experiment. On day 5, 3 of the 5 directly inoculated ferrets were euthanized to collect tissues, and on days 5 and 6, one ferret each from the WT and the HA2-K58I group, respectively, died from illness. (D) Replication of the WT and HA2-K58I viruses in different body tissues on day 5 after infection. The detection limit was 1 log10 TCID50/ml. Closed symbols indicate directly inoculated ferrets. Open symbols indicate contact ferrets. NC, nasal cavities; T, trachea; LU, left lung's upper lobe; LL, left lung's lower lobe; RU, right lung's upper lobe; RM, right lung's middle lobe; RL, right lung's lower lobe; B, brain; L, liver; LI, large intestine. Horizontal lines within groups show mean values. Statistical analysis was performed by using two-way ANOVA for comparison of weight loss and virus titers and the log-rank chi-square test for survival curves. The differences in the titers of WT and HA2-K58I viruses in the left lower lung were statistically significant (P < 0.01). Statistical analyses could not be performed to compare WT and K58I groups in tissues where no K58I was detected, including the liver and right upper, middle, and lower lung.
The viral loads of the HA2-K58I virus in ferret nasal washes were 100- to 1,000-fold higher (P < 0.01) than those of the wild-type virus on days 1 and 2 postinfection (Fig. 7C). Thus, we observed a correlation between increased HA acid stability (or a lower pH of activation) and early H5N1 growth in the ferret URT. By day 4 postinfection, both wild-type and HA2-K58I virus-infected ferrets had similar viral loads in their nasal washes (Fig. 7C), and by day 5 postinoculation, both groups had similar viral loads in the nasal tissues collected from euthanized animals (Fig. 7D). Similarly, the brains and large intestines from the wild-type and HA2-K58I virus-infected ferrets had comparable viral loads on day 5 postinoculation. Relatively large amounts (>104 TCID50/g of tissue) of wild-type VN1203 virus were detected in the lungs and the livers of inoculated ferrets; however, only low levels (<10 TCID50/g of tissue on the average) of HA2-K58I virus were detected in the lungs and no HA2-K58I virus was detected in the livers of inoculated ferrets (Fig. 7D). The low viral loads of HA2-K58I virus in the lungs of ferrets were unexpected, as the mutant virus had greater viral loads in the lungs of C57BL/6J mice (Fig. 5C).
None of the four naive contact ferrets from either the wild-type or the HA2-K58I virus-infected group were observed to lose weight, die, have neurological symptoms, or shed virus (Fig. 7A to C). The absence of weight loss and detectable virus in the nasal washes of contact ferrets suggested that neither wild-type nor HA2-K58I virus was able to efficiently transmit between ferrets. To confirm that contact transmission did not occur even at minimal levels, serum was collected from contact ferrets 20 days after they had first been exposed to directly inoculated animals. For the wild-type group, none of the four contact ferrets seroconverted (limit of detection, anti-H5 titer of 10). In contrast, one of the four contact ferrets in the HA2-K58I group seroconverted, albeit to a low level (anti-H5 titer of 20) that is suggestive of nonproductive contact transmission. As productive transmission between cohoused ferrets was not observed, airborne transmission experiments between separated donor/recipient ferret pairs were not conducted.
DISCUSSION
In this study, we investigated the effect of a single mutation (i.e., HA2-K58I, which decreases the pH of activation of the HA protein) on the growth, virulence, and transmissibility of an H5N1 influenza virus in mice and ferrets. The virus chosen for this work was A/Vietnam/1203/2004 (H5N1). The VN1203 virus was chosen over the previously characterized in A/chicken/Vietnam/C58/2004 (35) due to its ability to replicate and cause disease in ferrets (52). This human isolate from clade 1 has an avian preferred α(2,3) receptor binding specificity but a mammalian-adapted polymerase (i.e., PB2-E627K) (52). As the VN1203 virus was not laboratory adapted or reassorted and contained no mutations other than HA2-K58I, the results described here bear directly on the potential of a single, acid-stabilizing mutation to enhance the capability of a circulating H5N1 virus to grow, disseminate, and transmit in mammalian hosts. Our biochemical analyses showed that the K58I mutation in the HA2 stalk decreases the pH of activation of the VN1203 HA protein from pH 6.0 to 5.5 without affecting HA protein expression, cleavage, or receptor binding. In vitro, the HA2-K58I mutation did not affect VN1203 replication kinetics in MDCK and NHBE cells but was attenuating in A549 cells, which were found to have a higher endosomal pH than MDCK cells. In mice and ferrets, the HA2-K58I mutation did not alter the virulence of VN1203. However, the acid-stabilizing mutation altered the tropism of the virus by promoting 100- to 1,000-fold greater growth in the ferret URT early in infection (days 1 to 2 after inoculation) while simultaneously reducing the viral load 1,000- to 100,000-fold in the lungs later in infection (day 5 after inoculation). Robust influenza virus growth in the URT is necessary for transmission between ferrets (61). Yet, the enhanced growth of VN1203 in the URT due to the acid-stabilizing HA2-K58I mutation was not sufficient to enable productive transmission between contact ferrets. We have found previously that an HA2-K58I mutation in A/chicken/Vietnam/C58/2004 (H5N1) is attenuating in mallards (39) but enhancing in mice (35). Here we report that HA2-K58I enhances the early growth of the related VN1203 virus in the ferret URT. Overall, these studies reveal that a single acid-stabilizing mutation in the HA protein can switch the preference of a nonadapted/nonreassorted H5N1 virus (which has avian preferred receptor binding specificity) from an avian to a mammalian host; however, such an adaptation appears to be insufficient for transmissibility in mammals in the absence of other molecular factors.
For influenza virus to transmit, either by contact or by aerosol, it must efficiently infect, replicate in, and expel from the URT and be stable in the environment and/or respiratory droplets. An E627K mutation in the PB2 protein was found to support H5N1 influenza virus replication in the URT of mammalian species (62, 63). However, the presence of this mutation was not permissive for transmission of VN1203 H5N1 virus among ferrets (51). The HA protein receptor binding preference for α(2,6)-linked sialic acid receptors is considered a requirement for efficient influenza virus transmission between humans (64). A switch from α(2,6)- to α(2,3)-linked sialic acid receptor specificity abolishes the ability of the 1918 pandemic H1N1 influenza virus to transmit among ferrets (65). Despite some recent H5N1 influenza viruses acquiring the ability to bind α-(2,6) receptors (48), these viruses remain unable to transmit among ferrets and, presumably, humans (50, 51). This suggests that a decrease in α(2,3) receptor binding affinity in addition to increased α-2,6 receptor binding affinity may be required for efficient airborne transmission of H5N1 influenza viruses between ferrets or humans. Nonetheless, one study introduced mutations known to switch the receptor binding specificity of the H5 HA protein to α(2,6)-linked sialic acid, and yet the engineered H5N1 virus still failed to transmit, implying that other molecular changes are needed (50). Similarly, another study showed that an H5 virus with α(2,6) binding preference was able to partially transmit among ferrets via respiratory droplets only when it was coupled with a human N2 neuraminidase (21). Another study using an H5 reassortant virus showed that adding an acid-stabilizing HA mutation promoted contact transmission in ferrets (66), although the implications of the study for circulating H5N1 viruses are unclear, as the reassortant virus contained 6 PR8 internal genes, a 2009 H1N1 pandemic NA gene, and an H5N1 HA gene that had α(2,6) receptor specificity and lacked both a polybasic cleavage site and glycosylation on residue 158.
Recently, two laboratories were able to engineer and adapt H5 HA-containing influenza viruses that transmit between ferrets by the airborne route (24, 25). One study used A/Indonesia/5/2005 (H5N1) (24), and the other study used a reassortant virus containing the HA gene from A/Vietnam/1203/04 (H5N1) and the other seven genes from A/California/04/09 (H1N1) (25). In both cases, three sequential groups of mutations were needed before efficient airborne transmissibility was achieved, as follows: (i) two mutations in the HA receptor binding pocket that switched the receptor binding specificity from α(2,3) to α(2,6), (ii) a single mutation that removed a glycosylation site from the top of the HA receptor binding domain, and (iii) a single HA1 mutation in or adjacent to the metastable stalk domain that decreased the pH of activation of the HA protein (either measured directly [25] or as judged by structural considerations [24, 41]). Thus, a decrease in the pH of activation of the H5 HA protein to ∼5.6 (25) was necessary for airborne transmissibility in ferrets. The data from the present study show that a single mutation in the HA protein that lowers the HA activation pH to 5.5 is not sufficient to promote contact transmission in ferrets in the background of a nonreassorted/non-laboratory-adapted H5N1 influenza virus that retains its avian-like α(2,3) receptor binding specificity and intact glycosylation sites.
On one hand, the results from the present study suggest a lower risk that circulating avian-like H5N1 influenza viruses will jump species to humans, as H5N1 viruses are now expected to require more than one acid-stabilizing HA mutation to acquire pandemic potential. Other required changes include the acquisition of α(2,6) receptor binding specificity and/or the deletion of a glycosylation site (24, 25). Furthermore, our previous studies show that circulating avian H5N1 influenza viruses tend to have HA activation pH values ranging from 5.7 to 6.0 (39, 41, 54) and are unlikely to acquire acid-stabilizing mutations that lower the HA activation pH below pH 5.6 in species such as chickens and ducks (39, 41, 42). On the other hand, during H5N1 infection in mammals, the likelihood of a virus acquiring an acid-stabilizing mutation may be relatively high. The present and previous studies (35, 44, 45, 66, 67) show that acid-stabilizing mutations promote H5N1 growth in the URT of mammals. We propose that numerous acid-stabilizing mutations are functionally equivalent, thereby increasing the likelihood of such a mutation being naturally selected. Eight mutations in H5 viruses have already been reported to decrease the HA activation pH: HA1-H18Q (35, 39, 43, 66), HA1-H103Y (24), HA1-D104N/I115T, HA1-E216K, and HA1-S221P (41), HA1-T318I (25), HA2-K58I (35, 39, 44), and HA2-E105K (43). These residues are located throughout the prefusion HA protein in four broad regions that undergo dramatic changes in secondary and tertiary structure after acid-induced, irreversible activation. The four regions include (i) the interface between the HA1 receptor binding domain trimer, (ii) the HA1-HA2 interface, (iii) the spring-loaded HA2 stalk, and (iv) the pocket surrounding the hydrophobic fusion peptide (Fig. 8). Dozens of other acid-stabilizing mutations to numerous H5 HA residues could potentially arise, just as a wide variety of activation pH-altering mutations in these four regions of the HA molecule have been selected for in H3N2 and H7N7 viruses (69–71). As mutations that alter the acid stability of the HA protein appear to be functionally equivalent, we propose that future surveillance efforts to identify H5N1 viruses with increased potential for transmissibility in mammals include functional assays for HA acid stability, in addition to using sequence data to identify known acid stabilizers, such as HA1-H103Y and HA1-T318I.
Fig 8.
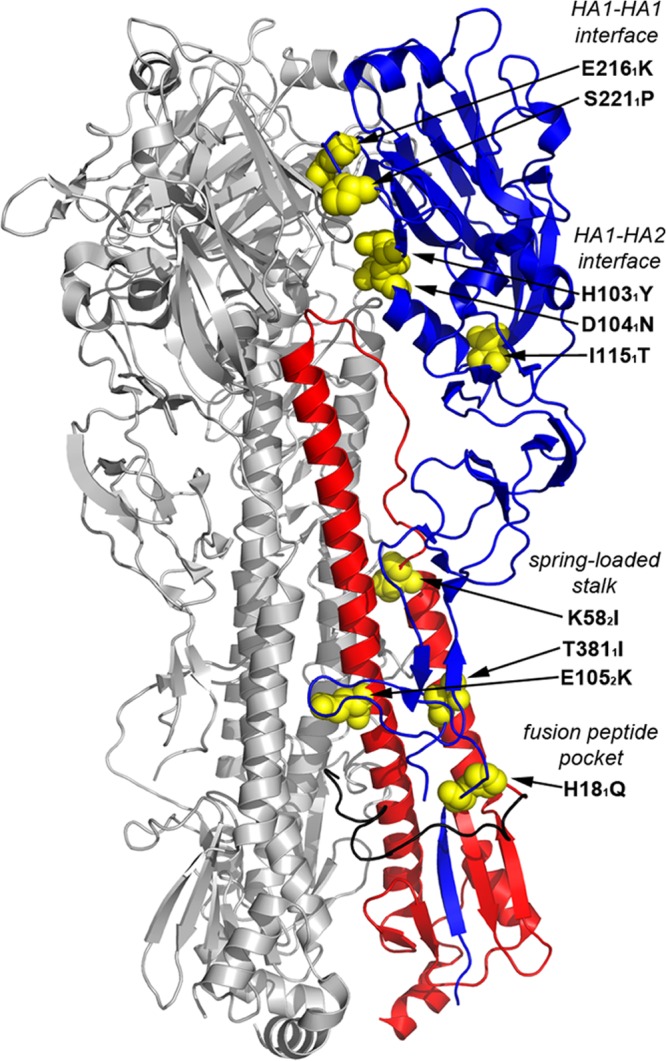
Structure of the H5N1 HA protein, identifying the locations of acid stabilizing mutations. In this crystal structure of the H5N1 HA protein (PDB 3S11), two protomers are colored gray. In the third protomer, residues in the HA1 subunit are colored blue, residues in HA2 are red, and the hydrophobic fusion peptide in HA2 is black. Amino acid residues for which acid stabilizing mutations have been discovered are presented as yellow spheres. The mutations are listed to the right of the molecule, along with the four structural regions that contain the mutations (denoted by italics). H3 numbering is used, and subscripts denote HA1 (1) and HA2 (2) subunits.
Even though the HA2-K58I mutation did not increase the virulence of highly pathogenic H5N1 influenza virus or permit contact transmission in ferrets, this mutation altered the tropism of the VN1203 virus in the ferret respiratory tract and increased the stability of the virus in the presence of acid at pH 5.5. Therefore, HA2-K58I is a gain-of-function mutation, and the results described here qualify as dual-use research (DUR). We do not believe that the VN1203-HA2-K58I virus itself or the results described here could be directly misapplied to pose a significant threat with broad potential consequences to public health and safety or to agriculture. Therefore, we contend that this work is not dual-use research of concern (DURC) (72). The VN1203-HA2-K58I agent itself poses no enhanced risk to public health or agriculture compared to unmodified VN1203 or other circulating H5N1 viruses because (i) the HA2-K58I mutation does not increase virulence or transmissibility in ferrets, a model for infection in humans, and (ii) the HA2-K58I mutation has been shown previously to reduce H5N1 virus growth, virulence, and transmission in mallards, an avian model (39). Additionally, the VN1203-HA2-K58I virus is susceptible to oseltamivir, and a vaccine containing the parental VN1203 HA protein is available (44). The VN1203-HA2-K58I virus was not actively adapted during experiments in ferrets, which were conducted in 2011 before the moratorium on H5N1 research (73), and tissues were destroyed after titers were measured. Knowledge of the HA2-K58I mutation could not be directly misapplied to threaten public health by introducing HA2-K58I into the ferret airborne-transmissible viruses (24, 25), which already have functionally equivalent acid-stabilizing mutations and would most likely be attenuated by the addition of an HA2-K58I mutation (35). These studies have been reviewed and approved before, during, and after completion both internally by the Institutional Biosafety Committee and externally by the funding agency. All work was conducted in a secure biocontainment ABSL3+ facility (see Materials and Methods) by highly qualified and trained scientists who abide by a quarantine policy that prohibits contact with immunocompromised patients, zoos, pet shops, and avian species within 1 week of accessing the ABSL3+ facility.
Highly pathogenic H5N1 influenza viruses continue to circulate in domestic poultry and wild birds, and these viruses occasionally infect humans and other mammals (22). If H5N1 viruses adapt to mammals and acquire the ability for sustained human-to-human transmission, a pandemic will be both inevitable and devastating to public health and economic welfare. Therefore, there is an urgent need and responsibility to assess the risk of this threat and take precautionary steps to prevent, contain, or minimize it. This work describes a mutation and a molecular property that support the adaptation of H5N1 influenza viruses from avian to mammalian hosts and provides a better understanding of the requirements for H5N1 influenza viruses to cross the species barrier.
Knowledge of the results described here may benefit public health in several ways. First, this work provides a mammalian preferred HA activation pH (∼5.5) for H5N1 and specific HA mutations that enhance its acid stability (Fig. 8). This information will enhance the effectiveness of influenza virus surveillance activities. Second, understanding interspecies adaptation will assist in risk assessment, prepandemic vaccine selection, and decisions to cull animals or quarantine humans. Third, the HA2-K58I mutation may be used to engineer vaccines for optimal growth in culture (egg or cell-based) and in vivo, thereby enhancing vaccine production and efficacy, as has already been demonstrated in two proof-of-concept studies (38). Fourth, this work bolsters novel approaches to develop anti-influenza virus inhibitors that prevent or induce HA conformational changes by binding to the stalk domain. Mutations conferring resistance to several experimental fusion inhibitors have been shown to increase the activation pH of the HA protein (74, 75), which the present study suggests may be counterproductive for efficient early growth in the mammalian URT. Finally, the results described here may provide new directions for research on other important human and animal pathogens, such as SARS coronavirus, dengue virus, hepatitis C virus, Epstein-Barr virus, human rhinovirus, vesicular stomatitis virus, and avian leukemia virus, which also contain envelope glycoproteins that are activated by low pH (76). The host range and tropism of these other viruses may also be influenced by mutations that alter the pH of activation of their fusion glycoproteins.
ACKNOWLEDGMENTS
We thank Elena Govorkova for providing the NHBE cells, Patrick Seiler for help with tissue collection, and Beth Little, David Carey, Scott Krauss, and Lisa Kercher for help with animal care and ABSL3+ training and procedures. We thank Deborah Nelson for advice on endosomal pH measurement and Jennifer Peters and Jama Temirov for help with confocal imaging. We thank the Animal Resources Center and the Hartwell Center Macromolecular Synthesis and Sequencing facilities at St. Jude Children's Research Hospital for providing support.
This work was supported by the National Institutes of Health, National Institute of Allergy and Infectious Diseases, Centers of Excellence for Influenza Research and Surveillance (CEIRS), under contract no. HHSN266200700005C and by the Children's Infection Defense Center (CIDC) at St. Jude Children's Research Hospital and the American Lebanese Syrian Associated Charities (ALSAC).
Footnotes
Published ahead of print 3 July 2013
REFERENCES
- 1.Jagger BW, Wise HM, Kash JC, Walters KA, Wills NM, Xiao YL, Dunfee RL, Schwartzman LM, Ozinsky A, Bell GL, Dalton RM, Lo A, Efstathiou S, Atkins JF, Firth AE, Taubenberger JK, Digard P. 2012. An overlapping protein-coding region in influenza A virus segment 3 modulates the host response. Science 337:199–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Muramoto Y, Noda T, Kawakami E, Akkina R, Kawaoka Y. 2013. Identification of novel influenza A virus proteins translated from PA mRNA. J. Virol. 87:2455–2462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nelson MI, Holmes EC. 2007. The evolution of epidemic influenza. Nat. Rev. Genet. 8:196–205 [DOI] [PubMed] [Google Scholar]
- 4.Selman M, Dankar S, Forbes N, Jia JJ, Brown EG. 2012. Adaptive mutation in influenza A virus non-structural gene is linked to host switching and induces a novel protein by alternative splicing. Emerg. Microbes Infect. 1:e42. 10.1038/emi.2012.38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Webster RG, Bean WJ, Gorman OT, Chambers TM, Kawaoka Y. 1992. Evolution and ecology of influenza A viruses. Microbiol. Rev. 56:152–179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wise HM, Foeglein A, Sun J, Dalton RM, Patel S, Howard W, Anderson EC, Barclay WS, Digard P. 2009. A complicated message: identification of a novel PB1-related protein translated from influenza A virus segment 2 mRNA. J. Virol. 83:8021–8031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zaraket H, Saito R, Sato I, Suzuki Y, Li D, Dapat C, Caperig-Dapat I, Oguma T, Sasaki A, Suzuki H. 2009. Molecular evolution of human influenza A viruses in a local area during eight influenza epidemics from 2000 to 2007. Arch. Virol. 154:285–295 [DOI] [PubMed] [Google Scholar]
- 8.Salomon R, Webster RG. 2009. The influenza virus enigma. Cell 136:402–410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neumann G, Kawaoka Y. 2011. The first influenza pandemic of the new millennium. Influenza Other Respi. Viruses 5:157–166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Belser JA, Bridges CB, Katz JM, Tumpey TM. 2009. Past, present, and possible future human infection with influenza virus A subtype H7. Emerg. Infect. Dis. 15:859–865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Butt KM, Smith GJ, Chen H, Zhang LJ, Leung YH, Xu KM, Lim W, Webster RG, Yuen KY, Peiris JS, Guan Y. 2005. Human infection with an avian H9N2 influenza A virus in Hong Kong in 2003. J. Clin. Microbiol. 43:5760–5767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hien ND, Ha NH, Van NT, Ha NT, Lien TT, Thai NQ, Trang VD, Shimbo T, Takahashi Y, Kato Y, Kawana A, Akita S, Kudo K. 2009. Human infection with highly pathogenic avian influenza virus (H5N1) in northern Vietnam, 2004-2005. Emerg. Infect. Dis. 15:19–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Peiris M, Yuen KY, Leung CW, Chan KH, Ip PL, Lai RW, Orr WK, Shortridge KF. 1999. Human infection with influenza H9N2. Lancet 354:916–917 [DOI] [PubMed] [Google Scholar]
- 14.Uyeki TM. 2009. Human infection with highly pathogenic avian influenza A (H5N1) virus: review of clinical issues. Clin. Infect. Dis. 49:279–290 [DOI] [PubMed] [Google Scholar]
- 15.WHO/OIE/FAO H5N1 Evolution Working Group 2012. Continued evolution of highly pathogenic avian influenza A (H5N1): updated nomenclature. Influenza Other Respi. Viruses 6:1–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peiris JS, Yu WC, Leung CW, Cheung CY, Ng WF, Nicholls JM, Ng TK, Chan KH, Lai ST, Lim WL, Yuen KY, Guan Y. 2004. Re-emergence of fatal human influenza A subtype H5N1 disease. Lancet 363:617–619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wei K, Chen Y, Chen J, Wu L, Xie D. 2012. Evolution and adaptation of hemagglutinin gene of human H5N1 influenza virus. Virus Genes 44:450–458 [DOI] [PubMed] [Google Scholar]
- 18.Beigel JH, Farrar J, Han AM, Hayden FG, Hyer R, de Jong MD, Lochindarat S, Nguyen TK, Nguyen TH, Tran TH, Nicoll A, Touch S, Yuen KY. 2005. Avian influenza A (H5N1) infection in humans. N. Engl. J. Med. 353:1374–1385 [DOI] [PubMed] [Google Scholar]
- 19.Eurosurveillance 2006. Avian influenza H5N1 outbreaks in Romanian and Danish poultry, and large H5N1 cluster in an Indonesian family. Euro Surveill. 11:pii=2961 http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=2961 [PubMed] [Google Scholar]
- 20.Ungchusak K, Auewarakul P, Dowell SF, Kitphati R, Auwanit W, Puthavathana P, Uiprasertkul M, Boonnak K, Pittayawonganon C, Cox NJ, Zaki SR, Thawatsupha P, Chittaganpitch M, Khontong R, Simmerman JM, Chunsutthiwat S. 2005. Probable person-to-person transmission of avian influenza A (H5N1). N. Engl. J. Med. 352:333–340 [DOI] [PubMed] [Google Scholar]
- 21.Chen LM, Blixt O, Stevens J, Lipatov AS, Davis CT, Collins BE, Cox NJ, Paulson JC, Donis RO. 2012. In vitro evolution of H5N1 avian influenza virus toward human-type receptor specificity. Virology 422:105–113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Neumann G, Chen H, Gao GF, Shu Y, Kawaoka Y. 2010. H5N1 influenza viruses: outbreaks and biological properties. Cell Res. 20:51–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gao Y, Zhang Y, Shinya K, Deng G, Jiang Y, Li Z, Guan Y, Tian G, Li Y, Shi J, Liu L, Zeng X, Bu Z, Xia X, Kawaoka Y, Chen H. 2009. Identification of amino acids in HA and PB2 critical for the transmission of H5N1 avian influenza viruses in a mammalian host. PLoS Pathog. 5:e1000709. 10.1371/journal.ppat.1000709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Herfst S, Schrauwen EJ, Linster M, Chutinimitkul S, de Wit E, Munster VJ, Sorrell EM, Bestebroer TM, Burke DF, Smith DJ, Rimmelzwaan GF, Osterhaus AD, Fouchier RA. 2012. Airborne transmission of influenza A/H5N1 virus between ferrets. Science 336:1534–1541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, Zhong G, Hanson A, Katsura H, Watanabe S, Li C, Kawakami E, Yamada S, Kiso M, Suzuki Y, Maher EA, Neumann G, Kawaoka Y. 2012. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature 486:420–428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Skehel JJ, Wiley DC. 2000. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu. Rev. Biochem. 69:531–569 [DOI] [PubMed] [Google Scholar]
- 27.Wilson IA, Cox NJ. 1990. Structural basis of immune recognition of influenza virus hemagglutinin. Annu. Rev. Immunol. 8:737–771 [DOI] [PubMed] [Google Scholar]
- 28.Wilson IA, Skehel JJ, Wiley DC. 1981. Structure of the haemagglutinin membrane glycoprotein of influenza virus at 3 A resolution. Nature 289:366–373 [DOI] [PubMed] [Google Scholar]
- 29.Fukuyama S, Kawaoka Y. 2011. The pathogenesis of influenza virus infections: the contributions of virus and host factors. Curr. Opin. Immunol. 23:481–486 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hartley CA, Reading PC, Ward AC, Anders EM. 1997. Changes in the hemagglutinin molecule of influenza type A (H3N2) virus associated with increased virulence for mice. Arch. Virol. 142:75–88 [DOI] [PubMed] [Google Scholar]
- 31.Ilyushina NA, Govorkova EA, Russell CJ, Hoffmann E, Webster RG. 2007. Contribution of H7 haemagglutinin to amantadine resistance and infectivity of influenza virus. J. Gen. Virol. 88:1266–1274 [DOI] [PubMed] [Google Scholar]
- 32.Keleta L, Ibricevic A, Bovin NV, Brody SL, Brown EG. 2008. Experimental evolution of human influenza virus H3 hemagglutinin in the mouse lung identifies adaptive regions in HA1 and HA2. J. Virol. 82:11599–11608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Koerner I, Matrosovich MN, Haller O, Staeheli P, Kochs G. 2012. Altered receptor specificity and fusion activity of the haemagglutinin contribute to high virulence of a mouse-adapted influenza A virus. J. Gen. Virol. 93:970–979 [DOI] [PubMed] [Google Scholar]
- 34.Ward AC, de Koning-Ward TF. 1995. Changes in the hemagglutinin gene of the neurovirulent influenza virus strain A/NWS/33. Virus Genes 10:179–183 [DOI] [PubMed] [Google Scholar]
- 35.Zaraket H, Bridges OA, Russell CJ. 2013. The pH of activation of the hemagglutinin protein regulates H5N1 influenza virus replication and pathogenesis in mice. J. Virol. 87:4826–4834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Giannecchini S, Clausi V, Di Trani L, Falcone E, Terregino C, Toffan A, Cilloni F, Matrosovich M, Gambaryan AS, Bovin NV, Delogu M, Capua I, Donatelli I, Azzi A. 2010. Molecular adaptation of an H7N3 wild duck influenza virus following experimental multiple passages in quail and turkey. Virology 408:167–173 [DOI] [PubMed] [Google Scholar]
- 37.Lin YP, Wharton SA, Martin J, Skehel JJ, Wiley DC, Steinhauer DA. 1997. Adaptation of egg-grown and transfectant influenza viruses for growth in mammalian cells: selection of hemagglutinin mutants with elevated pH of membrane fusion. Virology 233:402–410 [DOI] [PubMed] [Google Scholar]
- 38.Murakami S, Horimoto T, Ito M, Takano R, Katsura H, Shimojima M, Kawaoka Y. 2012. Enhanced growth of influenza vaccine seed viruses in Vero cells mediated by broadening the optimal pH range for virus membrane fusion. J. Virol. 86:1405–1410 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reed ML, Bridges OA, Seiler P, Kim JK, Yen HL, Salomon R, Govorkova EA, Webster RG, Russell CJ. 2010. The pH of activation of the hemagglutinin protein regulates H5N1 influenza virus pathogenicity and transmissibility in ducks. J. Virol. 84:1527–1535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stray SJ, Air GM. 2001. Apoptosis by influenza viruses correlates with efficiency of viral mRNA synthesis. Virus Res. 77:3–17 [DOI] [PubMed] [Google Scholar]
- 41.DuBois RM, Zaraket H, Reddivari M, Heath RJ, White SW, Russell CJ. 2011. Acid stability of the hemagglutinin protein regulates H5N1 influenza virus pathogenicity. PLoS Pathog. 7:e1002398. 10.1371/journal.ppat.1002398 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hulse DJ, Webster RG, Russell RJ, Perez DR. 2004. Molecular determinants within the surface proteins involved in the pathogenicity of H5N1 influenza viruses in chickens. J. Virol. 78:9954–9964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Reed ML, Yen HL, DuBois RM, Bridges OA, Salomon R, Webster RG, Russell CJ. 2009. Amino acid residues in the fusion peptide pocket regulate the pH of activation of the H5N1 influenza virus hemagglutinin protein. J. Virol. 83:3568–3580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Krenn BM, Egorov A, Romanovskaya-Romanko E, Wolschek M, Nakowitsch S, Ruthsatz T, Kiefmann B, Morokutti A, Humer J, Geiler J, Cinatl J, Michaelis M, Wressnigg N, Sturlan S, Ferko B, Batishchev OV, Indenbom AV, Zhu R, Kastner M, Hinterdorfer P, Kiselev O, Muster T, Romanova J. 2011. Single HA2 mutation increases the infectivity and immunogenicity of a live attenuated H5N1 intranasal influenza vaccine candidate lacking NS1. PLoS One 6:e18577. 10.1371/journal.pone.0018577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nakowitsch S, Wolschek M, Morokutti A, Ruthsatz T, Krenn BM, Ferko B, Ferstl N, Triendl A, Muster T, Egorov A, Romanova J. 2011. Mutations affecting the stability of the haemagglutinin molecule impair the immunogenicity of live attenuated H3N2 intranasal influenza vaccine candidates lacking NS1. Vaccine 29:3517–3524 [DOI] [PubMed] [Google Scholar]
- 46.Connor RJ, Kawaoka Y, Webster RG, Paulson JC. 1994. Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology 205:17–23 [DOI] [PubMed] [Google Scholar]
- 47.Shinya K, Ebina M, Yamada S, Ono M, Kasai N, Kawaoka Y. 2006. Avian flu: influenza virus receptors in the human airway. Nature 440:435–436 [DOI] [PubMed] [Google Scholar]
- 48.Stevens J, Blixt O, Chen LM, Donis RO, Paulson JC, Wilson IA. 2008. Recent avian H5N1 viruses exhibit increased propensity for acquiring human receptor specificity. J. Mol. Biol. 381:1382–1394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stevens J, Blixt O, Tumpey TM, Taubenberger JK, Paulson JC, Wilson IA. 2006. Structure and receptor specificity of the hemagglutinin from an H5N1 influenza virus. Science 312:404–410 [DOI] [PubMed] [Google Scholar]
- 50.Maines TR, Chen LM, Matsuoka Y, Chen H, Rowe T, Ortin J, Falcon A, Nguyen TH, Mai le Q, Sedyaningsih ER, Harun S, Tumpey TM, Donis RO, Cox NJ, Subbarao K, Katz JM. 2006. Lack of transmission of H5N1 avian-human reassortant influenza viruses in a ferret model. Proc. Natl. Acad. Sci. U. S. A. 103:12121–12126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yen HL, Lipatov AS, Ilyushina NA, Govorkova EA, Franks J, Yilmaz N, Douglas A, Hay A, Krauss S, Rehg JE, Hoffmann E, Webster RG. 2007. Inefficient transmission of H5N1 influenza viruses in a ferret contact model. J. Virol. 81:6890–6898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Salomon R, Franks J, Govorkova EA, Ilyushina NA, Yen HL, Hulse-Post DJ, Humberd J, Trichet M, Rehg JE, Webby RJ, Webster RG, Hoffmann E. 2006. The polymerase complex genes contribute to the high virulence of the human H5N1 influenza virus isolate A/Vietnam/1203/04. J. Exp. Med. 203:689–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hoffmann E, Mahmood K, Yang CF, Webster RG, Greenberg HB, Kemble G. 2002. Rescue of influenza B virus from eight plasmids. Proc. Natl. Acad. Sci. U. S. A. 99:11411–11416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Galloway SE, Reed ML, Russell CJ, Steinhauer DA. 2013. Influenza HA subtypes demonstrate divergent phenotypes for cleavage activation and pH of fusion: implications for host range and adaptation. PLoS Pathog. 9:e1003151. 10.1371/journal.ppat.1003151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Reed LJ, Muench H. 1938. A simple method of estimating fifty percent endpoints. Am. J. Hygiene 27:493–497 [Google Scholar]
- 56.Di A, Brown ME, Deriy LV, Li C, Szeto FL, Chen Y, Huang P, Tong J, Naren AP, Bindokas V, Palfrey HC, Nelson DJ. 2006. CFTR regulates phagosome acidification in macrophages and alters bactericidal activity. Nat. Cell Biol. 8:933–944 [DOI] [PubMed] [Google Scholar]
- 57.WHO 2002. WHO manual on animal influenza diagnosis and surveillance. World Health Organization, Geneva, Switzerland: http://www.who.int/vaccine_research/diseases/influenza/WHO_manual_on_animal-diagnosis_and_surveillance_2002_5.pdf [Google Scholar]
- 58.Chosewood LC, Wilson DE. (ed). 2009. Biosafety in microbiological and biomedical laboratories, 5th ed. HHS publication no. (CDC) 21-1112. Public Health Service, Centers for Disease Control and Prevention, National Institutes of Health, US Department of Health and Human Services, Washington, DC: http://www.cdc.gov/biosafety/publications/bmbl5/BMBL.pdf [Google Scholar]
- 59.Kaverin NV, Rudneva IA, Govorkova EA, Timofeeva TA, Shilov AA, Kochergin-Nikitsky KS, Krylov PS, Webster RG. 2007. Epitope mapping of the hemagglutinin molecule of a highly pathogenic H5N1 influenza virus by using monoclonal antibodies. J. Virol. 81:12911–12917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Southam DS, Dolovich M, O'Byrne PM, Inman MD. 2002. Distribution of intranasal instillations in mice: effects of volume, time, body position, and anesthesia. Am. J. Physiol. Lung Cell. Mol. Physiol. 282:L833–L839 [DOI] [PubMed] [Google Scholar]
- 61.Sorrell EM, Schrauwen EJ, Linster M, De Graaf M, Herfst S, Fouchier RA. 2011. Predicting ‘airborne' influenza viruses: (trans-) mission impossible? Curr. Opin. Virol. 1:635–642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hatta M, Hatta Y, Kim JH, Watanabe S, Shinya K, Nguyen T, Lien PS, Le QM, Kawaoka Y. 2007. Growth of H5N1 influenza A viruses in the upper respiratory tracts of mice. PLoS Pathog. 3:1374–1379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Steel J, Lowen AC, Mubareka S, Palese P. 2009. Transmission of influenza virus in a mammalian host is increased by PB2 amino acids 627K or 627E/701N. PLoS Pathog. 5:e1000252. 10.1371/journal.ppat.1000252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Chandrasekaran A, Srinivasan A, Raman R, Viswanathan K, Raguram S, Tumpey TM, Sasisekharan V, Sasisekharan R. 2008. Glycan topology determines human adaptation of avian H5N1 virus hemagglutinin. Nat. Biotechnol. 26:107–113 [DOI] [PubMed] [Google Scholar]
- 65.Tumpey TM, Maines TR, Van Hoeven N, Glaser L, Solorzano A, Pappas C, Cox NJ, Swayne DE, Palese P, Katz JM, Garcia-Sastre A. 2007. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science 315:655–659 [DOI] [PubMed] [Google Scholar]
- 66.Shelton H, Roberts KL, Molesti E, Temperton N, Barclay WS. 13 March 2013. Mutations in hemagglutinin that affect receptor binding and pH stability increase replication of a PR8 influenza virus with H5 HA in the upper respiratory tract of ferrets and may contribute to transmissibility. J. Gen. Virol. 10.1099/vir.0.050526-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Imai K, Ogawa H, Bui VN, Inoue H, Fukuda J, Ohba M, Yamamoto Y, Nakamura K. 2012. Inactivation of high and low pathogenic avian influenza virus H5 subtypes by copper ions incorporated in zeolite-textile materials. Antiviral Res. 93:225–233 [DOI] [PubMed] [Google Scholar]
- 68.Imai M, Kawaoka Y. 2012. The role of receptor binding specificity in interspecies transmission of influenza viruses. Curr. Opin. Virol. 2:160–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bullough PA, Hughson FM, Skehel JJ, Wiley DC. 1994. Structure of influenza haemagglutinin at the pH of membrane fusion. Nature 371:37–43 [DOI] [PubMed] [Google Scholar]
- 70.Daniels PS, Jeffries S, Yates P, Schild GC, Rogers GN, Paulson JC, Wharton SA, Douglas AR, Skehel JJ, Wiley DC. 1987. The receptor-binding and membrane-fusion properties of influenza virus variants selected using anti-haemagglutinin monoclonal antibodies. EMBO J. 6:1459–1465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Daniels RS, Downie JC, Hay AJ, Knossow M, Skehel JJ, Wang ML, Wiley DC. 1985. Fusion mutants of the influenza virus hemagglutinin glycoprotein. Cell 40:431–439 [DOI] [PubMed] [Google Scholar]
- 72.Office of Biotechnology Activities, National Institutes of Health 2012. The United States Government Policy for Oversight of Life Sciences Dual Use Research of Concern. National Institutes of Health, Bethesda, MD: http://oba.od.nih.gov/oba/biosecurity/pdf/united_states_government_policy_for_oversight_of_durc_final_version_032812.pdf [Google Scholar]
- 73.Fouchier RA, Garcia-Sastre A, Kawaoka Y, Barclay WS, Bouvier NM, Brown IH, Capua I, Chen H, Compans RW, Couch RB, Cox NJ, Doherty PC, Donis RO, Feldmann H, Guan Y, Katz J, Klenk HD, Kobinger G, Liu J, Liu X, Lowen A, Mettenleiter TC, Osterhaus AD, Palese P, Peiris JS, Perez DR, Richt JA, Schultz-Cherry S, Steel J, Subbarao K, Swayne DE, Takimoto T, Tashiro M, Taubenberger JK, Thomas PG, Tripp RA, Tumpey TM, Webby RJ, Webster RG. 2012. Pause on avian flu transmission research. Science 335:400–401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Russell RJ, Kerry PS, Stevens DJ, Steinhauer DA, Martin SR, Gamblin SJ, Skehel JJ. 2008. Structure of influenza hemagglutinin in complex with an inhibitor of membrane fusion. Proc. Natl. Acad. Sci. U. S. A. 105:17736–17741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vanderlinden E, Goktas F, Cesur Z, Froeyen M, Reed ML, Russell CJ, Cesur N, Naesens L. 2010. Novel inhibitors of influenza virus fusion: structure-activity relationship and interaction with the viral hemagglutinin. J. Virol. 84:4277–4288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Grove J, Marsh M. 2011. The cell biology of receptor-mediated virus entry. J. Cell Biol. 195:1071–1082 [DOI] [PMC free article] [PubMed] [Google Scholar]