Abstract
Sequence variation in the asparagine/aspartate-rich domain of pfmdr1 in 215 isolates of Plasmodium falciparum from three African countries was compared with published data. The role of this domain in modulating antimalarial sensitivity has not been established. The pfmdr1 86Y allele was significantly associated with different configurations of the Asn/Asp-rich domain in West and East Africa. In Kenya, a specific form of the Asn/Asp-rich domain was significantly linked to the 86Y, 184Y, and 1246Y haplotype of pfmdr1.
TEXT
The malaria parasite Plasmodium falciparum is becoming less sensitive to the artemisinin class of drugs in Asia (1, 2), and variable responses in East Africa have been reported (3). Artemisinin is a component of all current combination therapies, and while their clinical efficacy remains high, understanding of parasite genetic factors that contribute to variation in artemisinin sensitivity is essential. Variants of the pfmdr1 gene of P. falciparum (PF3D7_0523000) have been associated with increased probability of parasite survival after artemisinin combination therapy (4, 5). The locus encodes the ABC transporter, PgH1, comprising nine trans-membrane domains interrupted by an asparagine-rich (Asn-R) “hinge” domain known to exhibit length polymorphism (6–9).
Asn-R domains have been shown, in homologous ABC transporters of other taxa, to mediate ubiquitination and protein turnover (10, 11). Conversely, Asn repeats in the proteasome lid regulatory subunit 6 protein of P. falciparum, Rpn6, appear to be nonessential during intraerythrocytic growth in vitro (12), although similar data are not available for any other parasite ABC transporter. In this report, we present an analysis of the extent of sequence diversity in the pfmdr1 Asn-R domain in samples from four countries where malaria is endemic and explore associations with resistance-associated polymorphisms at codons 86, 184, and 1246 of pfmdr1.
Clinical samples were obtained from Mbita, Kenya, in 2009 (a random sample of 80 pretreatment isolates from a total of 300 enrollees) (13), Gedaref, Sudan, in 2006 (all 47 pretreatment DNA samples) (4), and Bobo-Dioulasso, Burkina Faso, between Oct 2009 and Jan 2010 (random sample of ∼25% of available DNA extracts) (I. Zongo, P. Milligan, Y. D. Compaore, A. F. Some, B. M. Greenwood, J. Tarning, P. J. Rosenthal, C. J. Sutherland, F. Nosten, and J.-B. Ouedraogo, unpublished data). Published sequence data on 26 isolates collected in The Gambia in 1996 were also included in the analyses (7). Permission for parasite genotyping studies was obtained from the relevant Ethics Committees. The Asn-R domain was amplified using primers and cycling conditions described elsewhere (7). Ten reference laboratory strains were included for comparison. Genotypes with resistance-associated polymorphisms at codons 86, 184, and 1246 were available from previous analyses. The sequences were determined with an ABI Prism 3730 DNA analyser (Applied Biosystems, United Kingdom) and analyzed using SeqMan (DNAStar Lasergene 7; Madison, WI) and BioEdit version 7.0.9. Amino acid haplotype diversity (Hs) and Wright's F statistic (FST) were determined using DnaSP version 5.10 (13). Associations between pfmdr1 codons 86, 184, and 1246 and Asn-R domain polymorphisms were assessed for statistical significance using the χ2 distribution, or Fisher's exact test where appropriate, using STATA (College Station, TX, USA).
Sequences of the Asn-R domain of pfmdr1 were determined successfully in 215 samples from the three African studies and compared to data from a Gambian report (7). A high level of diversity in the Asn-R domain was evident (Table 1). When Gambian data were included, a significant association was observed between the pfmdr1 86Y allele and a linker region configuration of 8-2-8/9/10 (P = 0.008 by the χ2 test). However, after stratification by population, this association persisted only in Gambian (P = 0.006 by Fisher's exact test) and Burkina Faso (odds ratio [OR] of 38.5; 95% confidence interval [95% CI] of 7.01 to 253; P < 0.001) data, consistent with previous findings in West Africa (6). No Sudanese isolate bore this particular linker configuration. In Kenya, pfmdr1 86Y was instead significantly associated with the 7-2-10 profile (OR, 8.75; 95% CI, 1.72 to 14.6; P = 0.001). Regarding pfmdr1 184F, the only significant association was observed in Kenya with the form 7-0-4 (P = 0.0006). A third polymorphism in pfmdr1, D1246Y, is common in East Africa (5) and was included in the analysis for Mbita, Kenya, and Gedaref, Sudan. The 1246Y allele, which is rare in West Africa, was present in 30 (37.5%) isolates from Mbita, Kenya, where it was significantly associated with the 7-2-10 configuration of the Asn-R domain (OR, 4.03; 95% CI, 1.40 to 11.8; P = 0.0035). Of these 30 isolates, 24 harbored the YYY haplotype at pfmdr1 codons 86, 184, and 1246, previously associated with resistance to amodiaquine (5). Two isolates from Gedaref, Sudan (4.4%) also harbored the 1246Y allele, one of which displayed both the YYY haplotype and the 7-2-10 Asn-R domain configuration, as seen in Kenya.
Table 1.
Polymorphisms in the linker region sequence of 215 P. falciparum isolates and the proportion in each class linked to the codon 86Y, codon 184F, and codon 1246Y allelesa
| Asn-Asp-Asnb | No. of polymorphisms in the linker region sequence of isolates from the following country: |
Proportion (%) in each class linked to the following pfmdr1 allelec: |
||||||
|---|---|---|---|---|---|---|---|---|
| Sudan | Kenya | Burkina | The Gambia | All four countries (total) | 86Y | 184F | 1246Yd | |
| 7-2-09 | 39 | 10 | 29 | 4 | 82 | 52 | 73 | 4 (47) |
| 7-2-10 | 6 | 34 | 12 | 1 | 53 | 65 | 22 | 50 (40) |
| 7-2-07 | 0 | 8 | 12 | 0 | 20 | 0 | 55 | 0 (8) |
| 8-2-09 | 0 | 3 | 13 | 0 | 16 | 69 | 88 | 0 (3) |
| 7-2-08 | 0 | 1 | 4 | 6 | 11 | 18 | 64 | 0 (1) |
| 7-0-02 | 0 | 7 | 2 | 0 | 9 | 33 | 44 | 0 (7) |
| 7-0-04 | 0 | 8 | 0 | 0 | 8 | 50 | 100 | 50 (8) |
| 7-0-01 | 1 | 6 | 0 | 0 | 7 | 86 | 14 | 71 (7) |
| 7-2-11 | 0 | 1 | 6 | 0 | 7 | 14 | 57 | 100 (1) |
| 7-2-06 | 0 | 0 | 1 | 5 | 6 | 0 | 83 | |
| 8-2-08 | 0 | 0 | 0 | 5 | 5 | 100 | 100 | |
| 8-1-09 | 0 | 0 | 2 | 1 | 3 | 0 | 0 | |
| 5-2-09 | 0 | 0 | 2 | 0 | 2 | 0 | 0 | |
| 7-0-03 | 1 | 0 | 1 | 0 | 2 | 50 | 50 | 0 (1) |
| 7-0-00 | 0 | 0 | 0 | 1 | 1 | 0 | 100 | |
| 7-0-06 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 (1) |
| 7-1-11 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 (1) |
| 7-2-01 | 0 | 0 | 0 | 1 | 1 | 0 | 0 | |
| 7-2-04 | 0 | 0 | 1 | 0 | 1 | 0 | 100 | |
| 7-2-05 | 0 | 0 | 0 | 1 | 1 | 0 | 100 | |
| 7-2-12 | 0 | 0 | 1 | 0 | 1 | 100 | 100 | |
| 7-2-15 | 0 | 0 | 1 | 0 | 1 | 0 | 100 | |
| 8-0-00 | 0 | 0 | 0 | 1 | 1 | 100 | 100 | |
| 8-2-10 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | |
| Total | 47 | 80 | 88 | 26 | 241 | 236 | 234 | 125 |
The total number of linker region sequences determined from the different countries and the total number of samples evaluated for each pfmdr1 allele are shown in boldface type.
Numbers of Asn, Asp, and Asn residues in the linker sequence, respectively.
Sequence data at each codon were not available for all isolates. Thus, the denominator for the codon analyses is less than 236 in each case. For codon 1246, only samples from Kenya and Sudan were included in the analysis (see the text).
The number of samples is shown in parentheses.
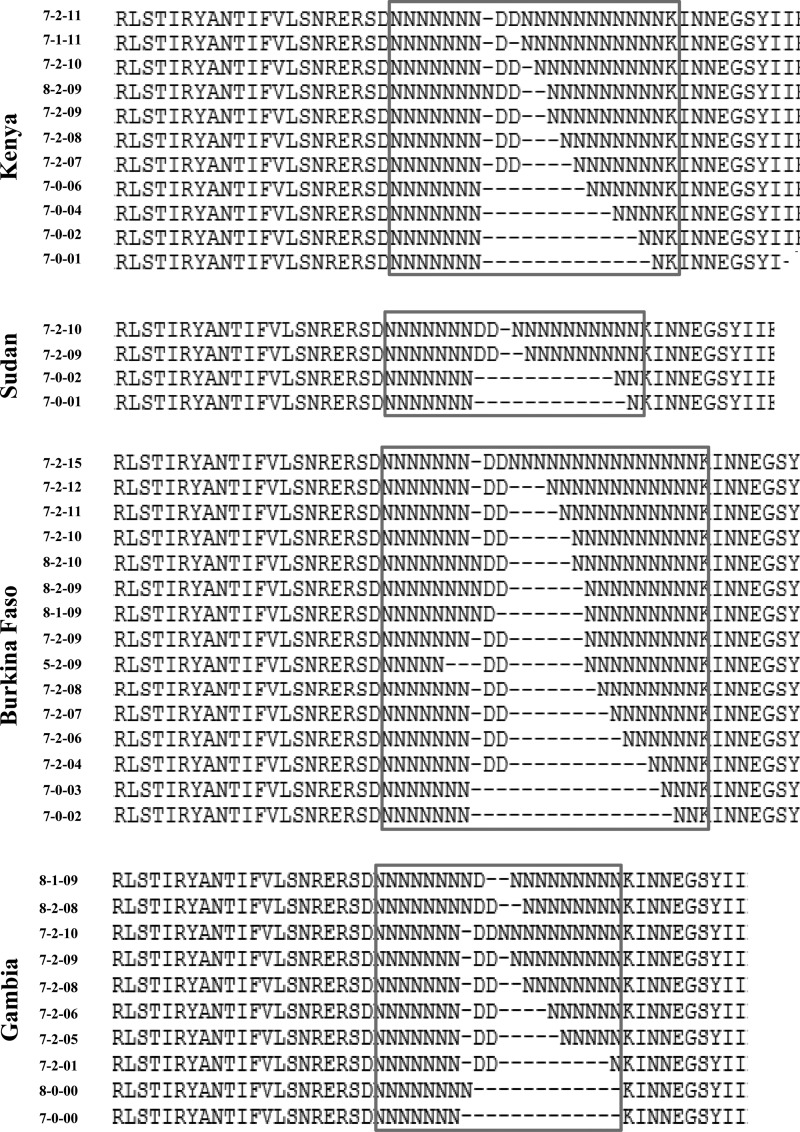
Compared to previous reports, our study has demonstrated a greater diversity at the Asn-R domain of pfmdr1 (Fig. 1), with 24 distinct Asp-R haplotypes in four populations. We observed very low levels of genetic differentiation between The Gambia and Burkina Faso, with an FST value (14) of 0.07 (Table 2). This was less than the differentiation between the two East African sites (FST = 0.19). Differences in diversity between Kenya and Sudan in the east and the West African populations could reflect the profound seasonality in transmission in The Gambia and Burkina Faso (15–17). In Kenya, Mbita is characterized by a high and perennial malaria transmission with entomologic inoculation rates of approximately six infectious bites per person per month (18), consistent with high genetic diversity. The low diversity in Sudan was unsurprising due to low transmission over a very short wet season in Gedaref, Sudan (19) and consequently more frequent self-fertilization within the parasite population. Our data suggest independent evolution of the pfmdr1 locus in East and West Africa. Antimalarial use and resistance allele frequencies are substantially different between these settings, and both are strongly affected by seasonality in The Gambia and Sudan (20, 21).
Fig 1.
ClustalW alignment output of all the representative profiles of the P. falciparum clinical isolates from three different countries and published Gambian data. Each group represents all sequence profiles identified in the country (indicated), and the variations are highlighted in the rectangular grid. The greatest variation was observed in Burkina Faso with 15 out of the 24 distinct sequence profiles observed in all the populations, while Sudan was the least diverse with only 4 of the 24 profiles.
Table 2.
Matrix of genetic differentiation showing pairwise FST values for the polymorphic linker domain in the four populations
| Countrya |
FST value for comparison of pairs of populations |
||
|---|---|---|---|
| Burkina Faso | The Gambia | Kenya | |
| Burkina Faso (88) | |||
| The Gambia (26) | 0.07089 | ||
| Kenya (83) | 0.10839 | 0.06075 | |
| Sudan (47) | 0.05791 | 0.17261 | 0.18974 |
The sample size for each location is given in parentheses.
The linker domain of ABC transporters has been shown to mediate ubiquitination and control of protein turnover (10, 11), two processes implicated in mechanisms of drug resistance in Plasmodium (22, 23). The association of pfmdr1 86Y with particular linker polymorphisms is not uniform, being found with 7-2-10 in Kenya and 8-2-8/9/10 in West Africa. This inconsistency may imply that the Asn-R domain is not involved in modulating antimalarial resistance but rather is passively carried, due to linkage, by selective sweeps around codons 86 and 184. However, our demonstration that the 1246Y mutation, rare in West Africa, was also strongly associated with the 7-2-10 form in Kenya provides an alternative explanation—that in fact the pfmdr1 alleles are distinct in the two regions, with little mixing. Thus, the 7-2-10 form of the Asp-R domain may be required to maintain the YYY haplotype of pfmdr1 in the Kenyan P. falciparum population. Further studies in West Africa, where the 1246Y allele is present but very rare, could seek evidence of the spread of this haplotype, together with the 7-2-10 Asp-R domain, from East Africa.
We have demonstrated substantial diversity in the Asp-R domain of pfmdr1 and significant within-population associations between this domain and resistance-associated single nucleotide polymorphisms in four P. falciparum populations. Our results suggest that the pfmdr1 locus has evolved separately in East and West Africa, reflecting differences in transmission, seasonality, and histories of antimalarial use. Any functional role of the Asn-R domain, a potential marker for both resistance and population diversity, remains to be determined.
Nucleotide sequence accession numbers.
Sequences described are available in GenBank under accession numbers KC573528 to KC573687.
ACKNOWLEDGMENTS
This work was supported by a Wellcome Trust/Association of Physicians of Great Britain and Ireland scholarship, awarded to J.O., and the EU FP7-funded MALACTRES Consortium. C.J.S. is supported by the Public Health England.
We thank David Warhurst and Manoj Duraisingh for helpful discussions.
Footnotes
Published ahead of print 8 July 2013
REFERENCES
- 1.Noedl H, Se Y, Schaecher K, Smith BL, Socheat D, Fukuda MM, Artemisinin Resistance in Cambodia 1 (ARC1) Study Consortium 2008. Evidence of artemisinin-resistant malaria in western Cambodia. N. Engl. J. Med. 359:2619–2620 [DOI] [PubMed] [Google Scholar]
- 2.Dondorp AM, Nosten F, Yi P, Das D, Phyo AP, Tarning J, Lwin KM, Ariey F, Hanpithakpong W, Lee SJ, Ringwald P, Silamut K, Imwong M, Chotivanich K, Lim P, Herdman T, An SS, Yeung S, Singhasivanon P, Day NP, Lindegardh N, Socheat D, White NJ. 2009. Artemisinin resistance in Plasmodium falciparum malaria. N. Engl. J. Med. 361:455–467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Borrmann S, Sasi P, Mwai L, Bashraheil M, Abdallah A, Muriithi S, Frühauf H, Schaub B, Pfeil J, Peshu J, Hanpithakpong W, Rippert A, Juma E, Tsofa B, Mosobo M, Lowe B, Osier F, Fegan G, Lindegårdh N, Nzila A, Peshu N, Mackinnon M, Marsh K. 2011. Declining responsiveness of Plasmodium falciparum infections to artemisinin-based combination treatments on the Kenyan coast. PLoS One 6:e26005. 10.1371/journal.pone.0026005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gadalla NB, Adam I, Elzaki SE, Bashir S, Mukhtar I, Oguike M, Gadalla A, Mansour F, Warhurst D, El-Sayed BB, Sutherland CJ. 2011. Increased pfmdr1 copy number and sequence polymorphisms in Plasmodium falciparum isolates from Sudanese malaria patients treated with artemether-lumefantrine. Antimicrob. Agents Chemother. 55:5408–5411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Humphreys GA, Merinopoulos I, Ahmed J, Whitty CJM, Mutabingwa TK, Sutherland CJ, Hallett RL. 2007. Amodiaquine and artemether-lumefantrine select distinct alleles of the Plasmodium falciparum mdr1 gene in Tanzanian children treated for uncomplicated malaria. Antimicrob. Agents Chemother. 51:991–997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Basco LK, Le Bras J, Rhoades Z, Wilson CM. 1995. Analysis of pfmdr1 and drug susceptibility in fresh isolates of Plasmodium falciparum from sub-Saharan Africa. Mol. Biochem. Parasitol. 74:157–166 [DOI] [PubMed] [Google Scholar]
- 7.Duraisingh MT, Jones P, Sambou I, von Seidlein L, Pinder M, Warhurst DC. 2000. The tyrosine-86 allele of the pfmdr1 gene of Plasmodium falciparum is associated with increased sensitivity to the anti-malarials mefloquine and artemisinin. Mol. Biochem. Parasitol. 108:13–23 [DOI] [PubMed] [Google Scholar]
- 8.Foote SJ, Kyle DE, Martin RK, Oduola AM, Forsyth K, Kemp DJ, Cowman AF. 1990. Several alleles of the multidrug-resistance gene are closely linked to chloroquine resistance in Plasmodium falciparum. Nature 345:255–258 [DOI] [PubMed] [Google Scholar]
- 9.Wilson CM, Volkman SK, Thaithong S, Martin RK, Kyle DE, Milhous WK, Wirth DF. 1993. Amplification of pfmdr 1 associated with mefloquine and halofantrine resistance in Plasmodium falciparum from Thailand. Mol. Biochem. Parasitol. 57:151–160 [DOI] [PubMed] [Google Scholar]
- 10.Kolling R, Losko S. 1997. The linker region of the ABC-transporter Ste6 mediates ubiquitination and fast turnover of the protein. EMBO J. 16:2251–2261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sato T, Kodan A, Kimura Y, Ueda K, Nakatsu T, Kato H. 2009. Functional role of the linker region in purified human P-glycoprotein. FEBS J. 276:3504–3516 [DOI] [PubMed] [Google Scholar]
- 12.Muralidharan V, Oksman A, Iwamoto M, Wandless TJ, Goldberg DE. 2011. Asparagine repeat function in a Plasmodium falciparum protein assessed via a regulatable fluorescent affinity tag. Proc. Natl. Acad. Sci. U. S. A. 108:4411–4416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sawa P, Shekalaghe SA, Drakeley CJ, Sutherland CJ, Mweresa CK, Baidjoe AY, Manjurano A, Kavishe RA, Beshir KB, Yussuf RU, Omar SA, Hermsen CC, Okell L, Schallig HD, Sauerwein RW, Hallett RL, Bousema T. 2013. Malaria transmission after artemether-lumefantrine and dihydroartemisinin-piperaquine: a randomized trial. J. Infect. Dis. 207:1637–1645 [DOI] [PubMed] [Google Scholar]
- 14.Librado P, Rozas J. 2009. DnaSP v5: a software for comprehensive analysis of DNA polymorphism data. Bioinformatics 25:1451–1452 [DOI] [PubMed] [Google Scholar]
- 15.Drakeley CJ, Akim NI, Sauerwein RW, Greenwood BM, Targett GA. 2000. Estimates of the infectious reservoir of Plasmodium falciparum malaria in The Gambia and in Tanzania. Trans. R. Soc. Trop. Med. Hyg. 94:472–476 [DOI] [PubMed] [Google Scholar]
- 16.Dunyo S, Milligan P, Edwards T, Sutherland C, Targett G, Pinder M. 2006. Gametocytaemia after drug treatment of asymptomatic Plasmodium falciparum. PLoS Clin. Trials 1:e20. 10.1371/journal.pctr.0010020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Habluetzel A, Cuzin N, Diallo DA, Nebié I, Belem S, Cousens SN, Esposito F. 1999. Insecticide-treated curtains reduce the prevalence and intensity of malaria infection in Burkina Faso. Trop. Med. Int. Health 4:557–564 [DOI] [PubMed] [Google Scholar]
- 18.Mutero CM, Ouma JH, Agak BK, Wanderi JA, Copeland RS. 1998. Malaria prevalence and use of self-protection measures against mosquitoes in Suba District, Kenya. East Afr. Med. J. 75:11–15 [PubMed] [Google Scholar]
- 19.Babiker HA, Walliker D. 1997. Current views on the population structure of Plasmodium falciparum: implications for control. Parasitol. Today 13:262–267 [DOI] [PubMed] [Google Scholar]
- 20.Abdel-Muhsin AMA, Mackinnon MJ, Ali E, Nassir EKA, Suleiman S, Ahmed S, Walliker D, Babiker HA. 2004. Evolution of drug-resistance genes in Plasmodium falciparum in an area of seasonal malaria transmission in Eastern Sudan. J. Infect. Dis. 189:1239–1244 [DOI] [PubMed] [Google Scholar]
- 21.Ord R, Alexander N, Dunyo S, Hallett R, Jawara M, Targett G, Drakeley CJ, Sutherland CJ. 2007. Seasonal carriage of pfcrt and pfmdr1 alleles in Gambian Plasmodium falciparum imply reduced fitness of chloroquine-resistant parasites. J. Infect. Dis. 196:1613–1619 [DOI] [PubMed] [Google Scholar]
- 22.Deplaine G, Lavazec C, Bischoff E, Natalang O, Perrot S, Guillotte-Blisnick M, Coppée JY, Pradines B, Mercereau-Puijalon O, David PH. 2011. Artesunate tolerance in transgenic Plasmodium falciparum parasites overexpressing a tryptophan-rich protein. Antimicrob. Agents Chemother. 55:2576–2584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hunt P, Afonso A, Creasey A, Culleton R, Sidhu AB, Logan J, Valderramos SG, McNae I, Cheesman S, do Rosario V, Carter R, Fidock DA, Cravo P. 2007. Gene encoding a deubiquinating enzyme is mutated in artesunate- and chloroquine-resistant rodent malaria parasites. Mol. Microbiol. 65:27–40 [DOI] [PMC free article] [PubMed] [Google Scholar]