Abstract
Neurofibromatosis, which was first described in 1882 by Von Recklinghausen, is a genetic disease characterized by a neuroectodermal abnormality and by clinical manifestations of systemic and progressive involvement which mainly affect the skin, nervous system, bones, eyes and possibly other organs. The disease may manifest in several ways and it can vary from individual to individual. Given the wealth of information about neurofibromatosis, we attempted to present this information in different ways. In the first part of this work, we present a chronological history, which describes the evolution of the disease since the early publications about the disorder until the conclusion of this work, focusing on relevant aspects which can be used by those wishing to investigate this disease. In the second part, we present an update on the various aspects that constitute this disease.
Keywords: Genes, neurofibromatosis 1; Neurofibromatoses; Neurofibromatosis 1
Abstract
A neurofibromatose, descrita inicialmente em 1882 por Von Recklinghausen, é uma doença genética caracterizada por uma anormalidade neuroectodérmica e por manifestações clínicas de envolvimento sistêmico e progressivo, que acometem principalmente a pele, o sistema nervoso, ossos, olhos e eventualmente outros órgãos, podendo apresentar uma grande diversidade de manifestações que variam de indivíduo para indivíduo. Diante da riqueza de informações encontradas a respeito da neurofibromatose, buscamos apresentá-la sob diversos aspectos, organizando os conhecimentos a respeito dessa doença. Na primeira parte desse trabalho, apresentamos um histórico cronológico, relatando a evolução dessa doença desde os primórdios das publicações a ela referentes até o momento do término desse trabalho, dando ênfase aos fatos relevantes ao seu conhecimento e que possam ser utilizados por aqueles que pretendam pesquisar a respeito dessa afecção. Na segunda parte, apresentamos uma atualização sobre os diversos aspectos que compõem essa doença.
PART ONE
HISTORY OF NEUROFIBROMATOSIS: A CHRONOLOGICAL REPORT
In the XIII and XVI centuries, the oldest cases about the disease appear in the literature, described by Madigan, Schaw, and Masello on "Neurofibromatosis in the 13th Century and Report of NF-Like Case - Monstrorum History" - in Neurofibromatosis, vol.1 and 2, 1988.1,2
1785 - Mark Akensidi presents major reports about a patient nicknamed "wart man", with skin nodules, skin patches on his legs, bed sores, pruritus and a huge head.3
1803 - Odier introduces the term neuroma to emphatically describe the involvement of the nerve network associated with the tumor.4
1830 - Schwann describes the predominance of nerve sheath cells in neurofibromas.5
1847 - Virchow reported neuromas in several members of one family and, in 1863, classified the tumors of peripheral nerves into true neuromas (which contain nerve elements) and false neuromas (originating in the connective tissue of the nerve sheath).4
1849 - Robert Smith reports two cases of patients with neuromas, similar to those described by von Recklinghausen in 1882.6
1870 - Genersick publishes the report of a case of multiple neuromas associated with cutaneous and visceral (kidneys, ureters, and stomach) lesions, and kyphoscoliosis.7
1873 - Von Michel first reported the case of a patient with optic glioma.5
1878 - For the first time, Gerhardt reports the involvement of the urinary tract in patients with generalized neurofibromas.5
1880 - Marchand and, in 1881, Weischselbaum, two pathologists, reported adrenal gland tumors associated with pigmentations suggestive of patients with neurofibromas (NF).8 Weischselbaum based his conclusions on the autopsy of a 76-year-old patient with multiple neuromas, finding a ganglioneuroma in the adrenal gland and interpreting this tumor as a product of embryonic tissue growth.8
1882 - Friederich Daniel Von Recklinghausen recognized NF as a nosological entity by describing two cases of multiple neurofibromatosis, one of which was diagnosed at autopsy. He postulated that tumors along major peripheral nerves and also false skin neuromas originate from the connective tissue of nerve sheaths and nerve plexuses, particularly perinerve and endonerve. He also described pigmented skin areas, but he apparently did not include "café au lait" spots as part of the disease. He stressed that central nervous system tumors were rarely accompanied by skin manifestations. None of the patients had neurological manifestations, except for a low level of intelligence.4
1884 - Sir Frederick Treves described, in great detail, the life of his patient Joseph Carey.
Merrick, a 22-year-old man with skin and bone deformities, was cruelly presented in circuses as the "elephant man". He was misdiagnosed for decades as having an atypical form of NF. His story was the theme of the book and movie titled "The Elephant Man", which tells the sad story of a deformed man who has a repugnant appearance, but who is inteligente and devoid of love and affection. Later, it became clear that hedid not have NF but Proteus Syndrome. This sad fact stigmatized NF as the disease of the "elephant man".9
1892 - Hamilton, in his book "Lectures on Tumors from a Clinical Standpoint", 2nd ed.Detroit GSDavis, published the first illustration of NF.5
1896 - Marie & Barnard and Chauffard were pioneers in indicating macular pigmentation as a sign beyond neurofibroma.10
1900 - Thomson emphasizes the hereditary nature of NF.5
1901 - Adrian described the hereditary transmission of NF in 20% of the cases he investigated.5
1909 - Suzuki was the first to point out the association of NF with pheochromocytoma.5
1910 - Verocay suggested that these nerve tumors be called neurinomas and postulated that they originate from neuroectodermal cells, capable of causing the various types of tumors of Von Recklinghausen disease.11
1911 - Greggio reports the presence of large numbers of mast cells in neurofibromas.12
1916 - Henshen identified the high incidence of bilateral acoustic neuromas as part of the disease.5
1917 - Cushing established multiple meningiomas and bilateral acoustic neuromas as components of NF.5
1918 - Preiser and Davenport established that the disease was not sex-linked and followed Mendel's Law of inheritance, having a dominant character.4
1924 - Brooks and Lehman first classified skeletal changes in the American literature.5
1924 - Harrison identified the origin of Schwann cells in the neural crest.5
1931 - Hosoi, based on literature data, calculated the incidence of malignant degeneration in about 13% of cases published and tabulated principles for the surgical treatment of NF: 1. partial excision of the neurofibroma can stimulate its malignancy 2. after complete excision of a neurofibrosarcoma, another neurofibroma may become malignant; 3. after surgery, local or regional recurrences are common, and 4. distant metastases are rare.13
1933 - Pohl reports the case of a patient with thoracic meningocele and NF. 5
1937 - Lisch describes another clinical manifestation of NF: nodules in the surface of the iris. They are melanocytic hamartomas, varying in color from clear yellow to brown, that appear as well-defined, dome-shaped elevations projecting from the surface of the iris. They were deservedly named after Lisch: Lisch nodules.3
1937 - In a first report, Ducroquet (apud Klatte et al., 1976) associates the pseudoarthrosis he found in nine out of eleven patients with NF.14
1940 - Davis established optic glioma as part of the disease.5
1940 - Reubi and Feyrter recognized a direct relationship between NF and vascular injury, as a proliferative tendency of non-nervous tissues or a blastomatous development of vessels within nerves. According to Reubi, a vascular injury would result from a general proliferation of nonnervou tissues, whereas Feyrter believed that it represented a blastomatous development of vessels within nerves. More recently, ultrastructural investigations have suggested that vascular injuries may be due in part to a mesodermal dysplasia (Greene et al. 1974).15,16
1952 - Glenn et al. described a patient with NF and hypertension and abdominal aortic coarctation.17
1959 - Szabo microscopically recognized giant pigmented granules in melanocytes as a characteristic of the disease. 5
1963 - Israel-Asselain and Devies identified cystic changes and pulmonary fibrosis as part of the disease.5
1963 - Russel and Rubenstein noted that two morphologic types of neoplasms, neurofibroma and schwannoma, can be found together (fused) in a single large mass, and that each component can show histological evidence of malignancy.18
1965 - Halpern and Currarino reported renal stenosis as a cause of hypertension in NF. 19
1967 - Rosman and Pearce identified changes in cortical architecture associated with mental impairment in patients with NF. 20
1972 - Brasfield and Das Gupta, in a study of 110 patients, identified 29% of malignant transformation of the nerve sheath and 15% of epithelial tumors. There was equal distribution between sexes.21 Other authors had previously observed a higher incidence in males (Preiser and Davenport, 1918 and Canale et al., 1972).4
1972 - Bricaire et al. report that the merit for the association of acromegaly and NF is unequivocally due to De Castro (1934). De Castro described the case of a 33-year-old man with multiple cutaneous neurofibromas (approximately 67 tumors), acromegalias of the face and hands and evident scoliosis. Suspicion of a brain tumor was based on complaints of headaches associated with glycosuria, eye disorders with bilateral optic atrophy, and radiograph showing enlarged sella turcica in all directions. Autopsy confirmed the existence of a pituitary tumor forming a bulge within the cranial cavity.8
1972 - Chaves et al. studied dermatoglyphics of the fingers of two patients and found a loop pattern in 90% (ulnar loop 50% and radial loop pattern 40%) and 10% arch pattern. Compared with normal controls, they reported a predominance of the radial loop pattern followed by the arch pattern, but they did not conclude anything due to the very small number of patients studied.22
1974 - Schenkein et al. identified nerve growth stimulating activity in the serum of patients with the disease.5
1976 - Isaacson studied the concentration and distribution of mast cells in 132 cases of benign tumors derived from the nerve sheath and found that, with rare exceptions, neurofibromas are characterized by a high concentration of mast cells diffusely distributed.23
1977 - Jurecka et al. indicated that, histopathologically, the nuclei of mast cells represent approximately 5% of all nuclei present in neurofibromas.24
1980 - Gholam et al. reported their experience in the treatment of congenital glaucoma in NF, which is the same as the one used for other types of congenital glaucoma, but with worse results. They emphasize that congenital glaucoma was first reported as a complication of NF two years after Von Recklinghausen established it as a nosological entity.25
1982 - Riccardi classified NF into eight types with designations, clinical features and patterns of inheritance.26
1986 - Carey et al. proposed that NF be classified into only five types based on distinct clinical characteristics and genetic implications for the patient.27
1987 - Riccardi suggests that the release of substances from mast cells contributes to tumor growth and associated symptomatology, and that the use of drugs which block this secretion may retard such growth.28
1987 - Barker et al. and Seizinger et al. mapped the NF-1 gene in the pericentromeric region of chromosome 17.29,30
1988 - The National Institute of Health (NIH) established diagnostic criteria for NF. 31
1989 - Collins et al., Diehel et al., Fountain et al., O'Connell et al., and Stephens et al. determined the region in which the NF1 gene is located, on the long arm of chromosome 17.32-36
1990 - Cawthon et al. Viskochil et al. and Wallace et al. mapped the gene to 17q11.2 and conducted studies that facilitated the isolation, cloning and characterization of the gene.37,38,39
1990 - Rouleau et al. and Wolf et al. located the NF2 gene on the q.1.2 arm of chromosome 22 and assumed that it acts as a suppressor gene.40,41
1993 -Rouleau et al. and Trofatter et al. cloned the NF2 gene.42,43
1993 - Legius et al. and Andersen et al. concluded that NF is a suppressor gene.44.45
1994 - Collins et al., on more specific studies, more precisely mapped the NF1 gene to 17q11.2.46
1994 - Goloni-Bertollo, Antonio JR et al., in a review article on the clinical- genetic evaluation of NF, highlighted that there are at least three levels of variation regarding expression and heterogeneity:temporal expression, progressive clinical features;
individual expression, highly variable in its manifestations from one individual to another, and
pathophysiological or genetic heterogeneity, large differences between the manifestations in some patients or family members.
They recognized the importance of a more specific diagnosis for the different types which comprise categories with similar clinical-genetic characteristics.47
1994 - Goloni-Bertollo, on his PhD dissertation, evaluated clinical and cytogenetic changes in patients with NF.48
1994 - Huson classified the clinical features of NF in "major", "minor" and associated complications based on diagnostic criteria from the NationalInstitute of Health (1988).49
1996 - Valerio, on his Master's dissertation, proposed a psychosocial classification of NF.50
1998 - Cnossem et al. reported that minor signs of NF1are useful in predicting disease diagnosis in children under 6 years with insufficient diagnostic criteria.51
1998 - Cnossem et al. found an association between the behavioral problems of children with NF1 and the presence of disease complications, reporting that the problems can be a consequence of these complications.52
1998 - Kaste E Pivnik described bone changes to the orbital morphology of NF1 patients; the most common were increased transorbital diameter and interorbital distance, features that contribute to the presence of hypertelorism in these patients.53
1998 - Howell et al. indicated that growth hormone replacement therapy in patients with NF1, and biochemical evidence of deficiency of this hormone, resulted in a moderate height increase in these individuals.54
1998 -Machado, on his Master's dissertation, conducted a clinical, cytogenetic and molecular evaluation of patients with NF. 55
1999 - Nielsen et al. concluded that the malignant transformation of NF1 is associated with loss of expression of the p16 protein, which is secondary to CDKN2A/p16 gene deletion, suggesting that inactivation of this gene occurs during the malignant transformation of neurofibromas.56
1999 - Teixeira, on his Master's dissertation, assessed ocular changes in patients with NF type 1.57
2000 - John et al. were the first to characterize both the somatic and germinal mutations in the plexiform neurofibromas of patients with NF1.58
2000 - Szudek, Birch E Friedman suggested that short stature and macrocephaly are characteristics that can affect all patients with NF1 and are not limited to specific subgroups.59
2000 - Ferner et al. reported that fluorodeoxyglucose positron emission tomography (FDG PET) has proved to be an auxiliary tool for determining malignant changes in plexiform neurofibromas in NF1 patients.60
2000 - De Bella, Szudek E Friedman reported that 46% of children with NF1 failed to meet the diagnostic criteria of the National Institude of Health (NIH) at age 1, but 97% of them met this criterion at 8 years of age, and 100% of them at age 20. Therefore, they suggested the need to modify the diagnostic criteria for children under 8 years old.61
2001 - Rasmussen, Yang and Friedman, by evaluating the mortality rate in NF1, concluded that patients with the disease have a lower life expectancy compared to that of the general population.In addition, brain tumors and tumors of connective tissue and soft tissue are the most frequent causes of death in these patients.62
2001 - Illes et al. observed that there is a decrease in bone mineral density in the lumbar spine of NF1 patients and scoliosis compared to the general population.63
2001 - Antonio JR: on his doctoral thesis on the theme "genetic-clinical study and quantitative assessment of mast cells and extracellular matrix components in neurofibromas", based on the large number of mast cells present in neurofibromas and on the possibility that they contribute to tumor growth, considered the use of drugs whose mechanism of action is to stabilize or block the degranulation of mast cells, so that they can prevent the release of histamine from granules and inhibit the metabolism of its development.64
2002 - Mautner et al. showed a high incidence of hyperactivity disorders and attention deficit in children with NF1, reporting an association between these disorders and social and cognitive problems in patients with this disease.65
2002 Guillamo et al. concluded in a retrospective study that the prognosis of patients with NF1 associated with central nervous system (CNS) tumors depends on the age of the patient, presence of tumor-related symptoms and extra-optic tumor.66
2002 - Evans et al. established that NF1 patients are at an 8 to 13% risk for the development of malignant peripheral nerve tumors throughout their lives.67
2002 - Singhal et al. noted that optic gliomas in NF1 patients may lead to the development of secondary CNS tumor.68
2003 - Ars et al. reported that the presence of recurrent mutations of the NF1 gene are common in patients with NF1.69
2003 - De Raedt et al. reported that NF1 patients with NF1 microdeletion have a higher risk of developing malignant peripheral nerve turmors than patients with the disease without this gene microdeletion.70
2003 - Cunha, Barboza and Fonseca reported that most NF1 patients have receptors for the growth hormone (GH) localized in neurofibromas, suggesting that GH may play a role in their development.71
2004 - Ozerdem showed that angiogenesis is accelerated in NF1 patients due to hyperproliferation of endothelial cells and pericytes in the tumors of these patients, and they may also be potential targets for treatment of NF1.72
2004 - Kuorilehto et al. studied 26 postmenopausal women with NF1, revealing that all of them had osteoporosis or osteopenia.73
2004 - Mattocks et al. showed that mutations of the neurofibromatosis gene are distributed along the sequence of the NF1 gene codes and are not grouped in the domain related to GTPase activation.74
2004 - Yang et al. indicated that the suppression of the NF1 gene may also contribute to the molecular pathogenesis of acute myeloid leukemia, a disease with a greater risk of incidence in these patients.75
2004 - Venturin et al. concluded that the presence of dimorphisms, cardiac abnormalities and mental retardation are signs that, when present in patients with NF1, should raise suspicion of microdeletions involving the NF1 gene and contiguous genes.76
2004 - Ferner et al. reported that neurofibromatous neuropathy occurs in approximately 1.3% of NF1 patients, and may be the result of inappropriate signaling between Schwann cells, perineural cells and fibroblasts.77
2004 - Muniz, on his doctoral thesis, investigated the bone lesions of patients with NF for the diagnosis of neurofibromatosis.78
2005 - Tucker et al. concluded that the presence of malignant peripheral nerve tumors in patients with NF1 is strongly associated with the presence of internal neurofibromas (subcutaneous), suggesting that patients with benign tumors require greater attention in relation to malignancy.79
2005 - Johannessen et al. suggested that rapamycin may be a viable treatment for NF1 by inhibiting mTOR (mammalian target of rapamycin), which is quite active in NF1 gene -deficient cells.80
2006 - De Schepper et al. observed that café au lait spots have a higher number of melanocytes in NF1 patients than in subjects without the disease.81
2006 - Page et al. reported that NF1 impacts the lives of patients in many ways, but mainly emotionally. In fact, patients with more visible lesions reported a greater impairment in quality of life than those with subtle lesions.82
2006 - Levine et al. found cognitive deficiencies, slightly decreased IQ and a higher rate of attention deficit in patients with NF1.83
2006 - Rubben, Bausch and Nikkels revealed, through PCR, inactivation of the neurofibromatosis gene in the superficial melanoma of a patient with NF1. Therefore, they suggested that the genetic basis of NF1 was responsible for the melanoma in this patient, recommending the establishment of melanoma screening in NF1 patients.84
2006 - Lim et al. concluded that superficial neurofibromas have different characteristics on MRI when compared to deep neurofibromas in NF1 patients.85
2006 - Muniz et al. reviewed the importance of performing radiography and computed tomography in NF1 patients with bone changes to identify patients at a higher risk of debilitating bone abnormalities and the need for early treatment.86
2007 - Yoshida et al. had positive results in treating pigmented lesions of NF1 with intense pulsed light (IPL-RF) and a topical ointment with vitamin D3.87
2007 - Hanemann, Hayward and Hilton reported the case of a patient with NF1 and recurrent gastrointestinal symptoms. The patient was subjected to laparotomy and histopathological examination revealed dysplasia of the enteric nervous system. Thus, the authors attributed gastrointestinal symptoms in patients with NF1 to abnormalities of enteric nerves.88
2007 - Stevenson et al. reported that children and adolescents with NF1 have decreased bone mineral density when compared to the general population, which in turn may predispose adults with NF1 to osteoporosis and fractures.89
2007 -Brems et al. described a disorder with cutaneous manifestations (café au lait spots and axillary freckling) and phenotype similar to that of NF1, but with another causative gene (SPRED1).90
2008 - Brunetti-pierre et al. showed that patients with NF1 have a reduction in bone mass and that the lumbar spine is affected more severely.91
2008 - Carroll and Ratner stated that the formation of neurofibromas in NF1 is associated with the signalling of some cell types and growth factor acting together in combination with the absence of expression of neurofibrina in Schwann cells.92
2008 - Mc Keever et al. reported that the main complications of NF1 in children under 16 years old were learning difficulties and malignancy (especially optic glioma and CNS tumors).93
2008 - Krab et al. showed that treatment of NF1 patients with simvastatin (HMG-CoA reductase) to improve cognitive performance showed no results.94
2008 - Stevenson et al. showed that children with NF1 have a higher urinary excretion of collagen degradation products, reflecting an increase in bone resorption and contributing to the abnormal bone remodeling and skeletal defects present in this disease.95
2009 - Boley et al. suggested that UV exposure has an effect on the pathogenesis of Lisch nodules which, associated with haploinsufficiency of the NF1 gene, is sufficient and necessary for the formation of these nodules in patients with NF1.96
2009 - Brems et al. demonstrated that the presence of glomus tumors in patients with NF1 is secondary to the bi-allelic inactivation of the NF1gene and that loss of function of neurofibrina is essential to its pathogenesis.97
2010 - Boyd et al. concluded that café au lait spots in NF1 patients present variations in pigmentation, not only among patients but also in a single individual, and that this variation is not related to sun exposure.98
2010 -Turbyville et al. discovered that the Schweinfurthin A (SA) molecule inhibits the growth of tumor cells in NF1 patients.99
2010 - Johnson et al. identified delays in motor proficiency in children with NF1.100
2011 - Kolanczyk et al. established the Mia gene (melanoma-inhibitory activity / cd-rap) as a potential tumor biomarker in patients with NF1, and it may be used in disease follow-up and treatment monitoring.101
2011 - Duong et al. studied mortality in patients with NF1 in France, establishing a higher mortality rate than that of the general population and indicating cancer as the predominant cause.102
2011 - Sbidian et al. showed that patients with subcutaneous neurofibromas are at high risk for the development of internal neurofibromas with a tendency to transform into malignant tumors. They are also associated with neuropathy.103
2011 - Pasmant et al. confirmed that patients with NF1 microdeletion have an increased incidence of learning disabilities and facial dysmorphism when compared to patients with an intragenic mutation of this gene.104
2012 - Upadhyaya et al. studied the number of gene copies per microarray in NF1 patients and revealed the association of genes via Rho-GTPase in the tumorigenesis process associated with NF.105
2012 - Kantaputra et al. identified a new mutation in the NF1 gene, c.4821delA, which results in truncation of the neurofibromin protein.106
2012 - Chaudhary et al. showed the efficacy of metronomic therapy to treat tumors related to NF when chemotherapy does not work.107
2012 - Gong et al. reported reduced expression of microRNA miR-204 as a new biomarker for tumors in NF1. 108
DEFINITION
Neurofibromatosis (NF), a disease described in 1882 by Friedrich Daniel Von Recklinghausen, is a neuroectodermal abnormality constituted by a set of clinical symptoms that compromise the skin, nervous system, bones, eyes and other sites. Symptoms manifest differently in each patient, even those within the same family, with a highly variable expression.
EPIDEMIOLOGY
Neurofibromatosis type 1, which is more frequent in the population, has an estimated incidence of one case per 3,000 inhabitants. It affects all races and both sexes, with half of the cases presenting a family history, while in the other half the disease emerged as the result of a new mutation.109,110 It is believed that at least one million individuals worldwide are living with NF.111
NF is an autosomal dominant disease, considered one of the most common hereditary disorders in humans with this inheritance pattern. 112
ETIOPATHOGENESIS
The gene responsible for neurofibromatosis type 1, designated NF1, is located on the long arm of chromosome 17 at 17q11.2 and encodes a protein having 2818 amino acids and a molecular mass of 327 kDa (kilo Dalton) called neurofibromin. 113,114 This protein is predominantly expressed in neurons, Schwann cells, oligodendrocytes and astrocytes.115 Nordlund et al. detected the presence of neurofibromin in all parts of the brain, particularly in neurons with extended projections, such as pyramidal and Purkinje cells.116
A central region of neurofibromin is structurally and functionally homologous to GTPase-activating proteins (GAPs) in mammals, which accelerate the hydrolysis of p21Ras-GTP to p21Ras-GDP, thus converting it from the active to the inactive form .This central region, known as NF1-GRD, extends for approximately 360 amino acids, corresponding to the 20-27a exons of the gene.117
Family members of the p21ras proteins are encoded by the H-Ras, K-Ras and N-ARs genes, oscilate between the active (p21ras-GTP) and inactive (p21 ras-GDP) states and play a central role in cell differentiation and growth, transducing signals from the plasma membrane to the nucleus through its effectors.118
Oncogenic mutations in Ras genes or inactivation of NF1 favor the active state (p21ras -GTP) and, consequently, result in the permanent stimulation of a cascade of signals and excessive cell division. Loss of neurofibromin, in a variety of tumors and cells of NF1- deficient mice, is associated with elevated levels of p21ras -GTP and subsequent activation of its secondary effectors.119 These findings and the frequent presence of neoplasms in patients with neurofibromatosis type 1 occur because the NF1 gene is a tumor and neurofibromin supressor and participates in the process of tumorigenesis by inactivating both alleles of the gene.120
CLINICAL ASPECTS
The clinical manifestations found in NF1 can be summarized as follows: in the skin, neurofibromas, cafe au lait spots or macules (CALM) and axillary freckling; in the eyes, Lisch nodules and optic gliomas; in the central nervous system, vascular defects, brain tumors, macrocephaly and subsequent learning disabilities, mental retardation, epilepsy and headache;iIn the bones, scoliosis, pectus excavatum, para-spinal tumors, pseudoarthrosis, genu valgus and genu varus and, finally, other manifestations such as speech problems, precocious or delayed puberty, hypertension, intestinal neurofibromas and bowel function disorders caused by plexiform neurofibromas.
The skin manifestations of NF1 are classically characterized by the clinical presence of neurofibromas and café au lait spots variably distributed throughout the skin (Figure 1). 121
FIGURE 1.

Café au lait spots and neurofibromas typical of NF patients at Centro de Pesquisa e Atendimento em Neurofibromatose (CEPAN) - Faculdade de Medicina de São José do Rio Preto (FAMERP)
Café au lait spots are brownish macules that occur in 95% of patients with NF. They often precede cutaneous tumors and may be present at birth or appear later on, increasing in number and size during the first decade of life, especially in the first two years ( Figure 2).122,123
FIGURE 2.

Café au lait spots present at birth, CEPAN - FAMERP
Although few café au lait spots may exist among individuals without NF, the presence of more than six spots greater than 0.5 cm in diameter before puberty or greater than 1.5 cm in diameter after puberty is suggestive of NF.123 Their presence in the axillary region, constituting the so-called ephelides or axillary freckling, is considered pathognomonic of this disease (Figure 3). 124
FIGURE 3.

Café au lait spots, axillary freckling and neurofibromas - Dermatology Service, FAMERP
Another type of hyperpigmented spot occurs over the entire length of plex neurofibromas, which have a darker color than that of café au lait spots.125
Solitary or multiple neurofibromas are dysplastic tumors formed by axonal processes, Schwann cells, fibroblasts, perineural cells and mast cells.126 They have a soft texture, can be semiglobulus or pedunculated, are violet or skin colored and vary in number - they can be scarce and unique or cover the entire body - and size - from punctiform to masses of 5 or more cm in diameter (Figures 4 and 5).They are usually asymptomatic, but they can be itchy, painful and sensitive to touch.121
FIGURE 4.

Disseminated neurofibromas and a giant plexiform in the sacral region covering the buttocks - Dermatology Service, FAMERP
FIGURE 5.

Neurofibromas of various sizes in a widespread distribution - Dermatology Service, FAMERP
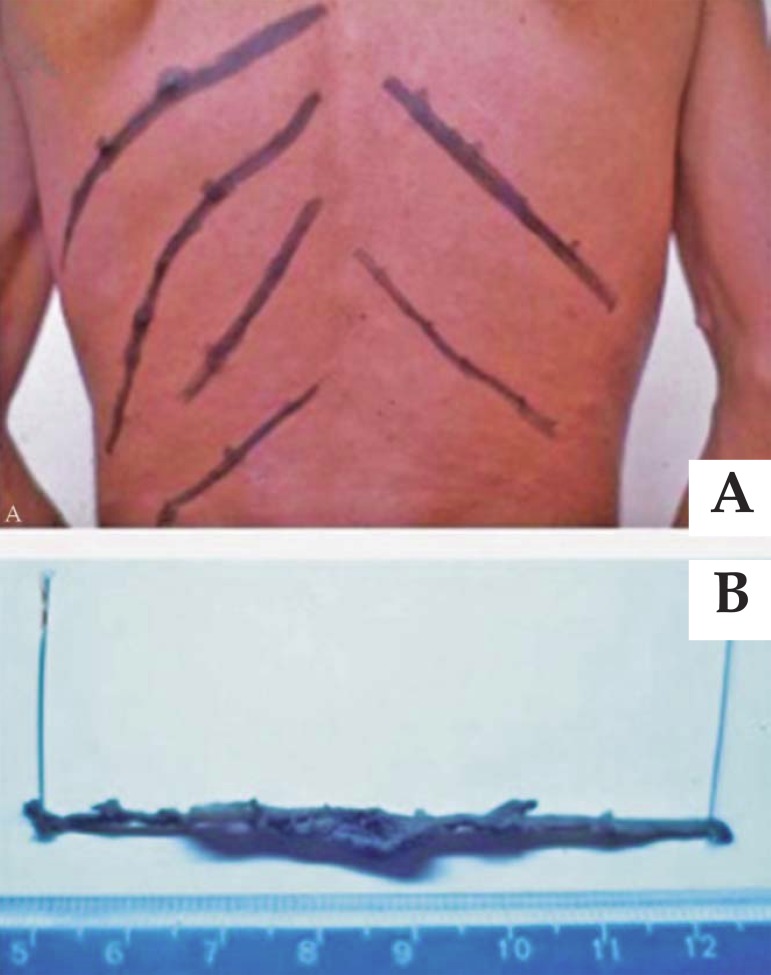
Neurofibromas are located along the nerves, especially in subcutaneous tissues (Figure 6). In some cases, they follow the nerve affecting large areas, being denominated plexiform neurofibromas (Figure 7). 127
FIGURE 6.
A. Subcutaneous nodules in intercostal spaces, delimited by palpation and marked with black ink. B. Macroscopic view of these subcutaneous nodules following the path of the nerve surgically removed
FIGURE 7.

Plexiform neurofibroma - Dermatology Service, FAMERP
There are four types of neurofibromas: superficial cutaneous neurofibromas, soft and buttonous; subcutaneous neurofibromas - deeper, in the dermis adjacent to subcutaneous nerves with direct involvement of the nerve roots and routes, and which are often accompanied by localized pain; nodular plexiform neurofibromas - they form an extensive network in the subcutaneous tissue, and diffuse plexiform neurofibromas - they compromise all layers of the skin and can penetrate deep into the muscles, bones and also involve, depending on location, the viscera.3,101
We studied 55 individuals from 35 families. All of them had café au lait spots, but there was great interindividual variability. The vast majority had café au lait spots disseminated throughout the body and of small size, ranging from 1 to 2 mm to 5 cm. Some had fewer café au lait spots, but they were larger in size.47 Axillary freckling was present in 77.5% of informative cases. Of five patients with plexiform neurofibromas, four showed hyperpigmentation throughout the tumor.
Of all ophthalmic manifestations, the most important is the Lisch nodule, which was described in 1937 by K. Lisch. They are well-defined, dome-shaped hamartomatous lesions of a gelatinous aspect projecting from the surface of the iris, varying in color from clear yellow to brown.121 The presence of Lisch nodules is a characteristic that appears to be unique to NF. They are asymptomatic and are only useful for diagnosis.128
Gordon (1966) observed that macrocrania and macrocephaly occurred in most children with NF.129 CT scans were normal, suggesting an increased size of the brain proportional to the size of the skull.130 Low stature occurs due to changes in development (growth impairment) and bone structures. Scoliosis is observed in almost half of the patients and generally affects the backbone, often presenting a pronounced angle that may be accompanied by kyphosis, especially more pronounced in the cervical spine.56,59
According to Muniz et al., kyphosis, kyphoscoliosis, cervical spine anomalies and erosion of the vertebral bodies are also common (Figure 8). Pseudoarthrosis of long bones, subperiosteal bone proliferation, bone tumors and intrathoracic meningocele also occur. Deformities of the spine and tibia pseudoarthrosis are the most frequent findings. Pectus excavatum and genu valgus and genu varus are described.86
FIGURE 8.
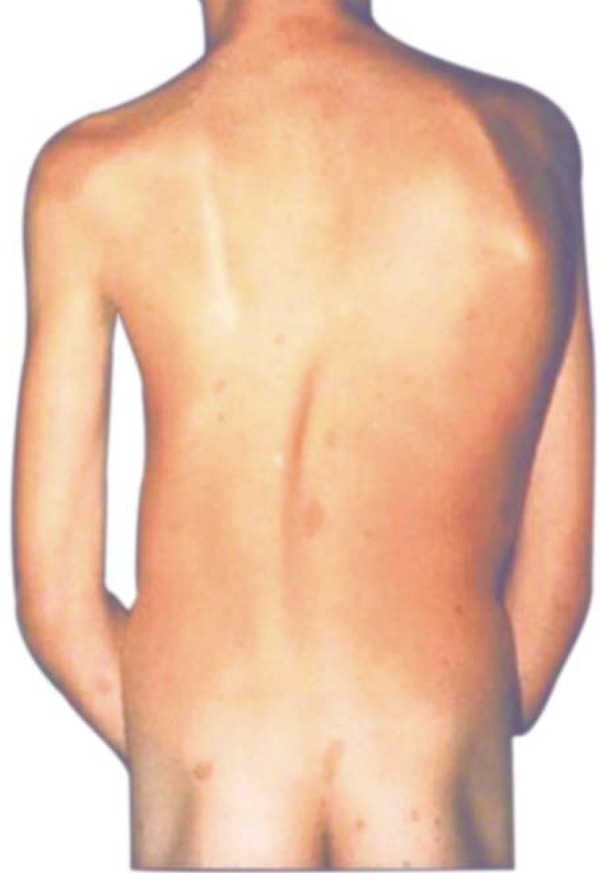
Scoliosis at the bottom of the spine and café au lait spots in the skin - Dermatology Service, FAMERP
Intrathoracic meningocele, described in patients with NF, is usually asymptomatic and may present posterior mediastinal masses on chest radiograph, which are often misinterpreted as neurofibromas.131 Radiolucent bone lesions are often found in the skull. They are irregular and rounded and most commonly seen along the left lambdoid sutures.132
Changes in other bones occur in less than 10% of cases. These changes are erosion of the periosteum by neurofibromas or in adjacent soft tissues, solitary cystic lesions or within the bone, disorders such as growth stunting or gigantism, increased striatal density of tubular bones, thinning and springing of the ribs and long bones, which can occur in a complication of NF as a separate nosological entity. Half of the patients with pseudarthrosis manifest other signs of NF.133
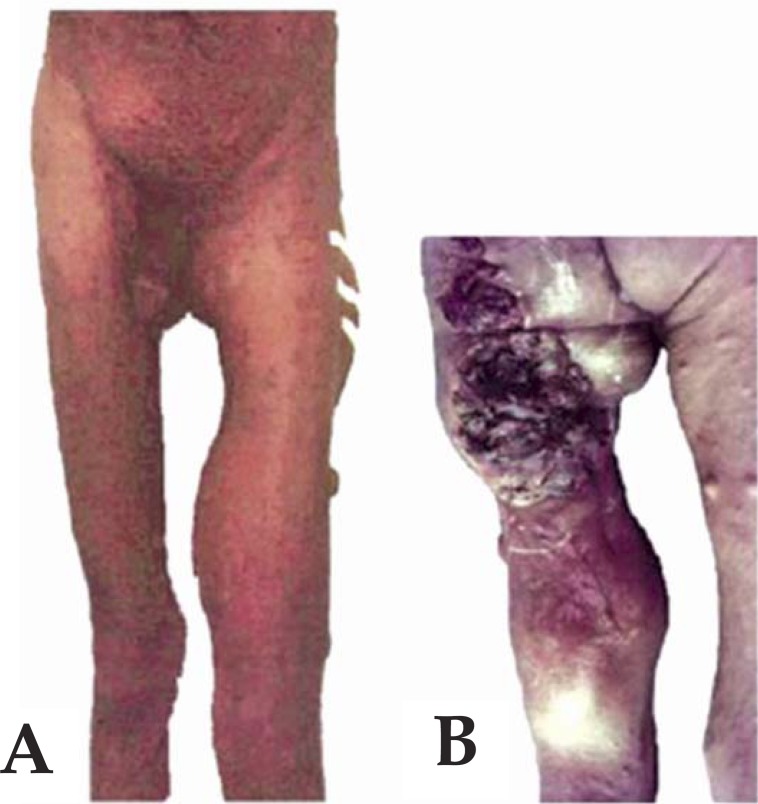
Malignancy is the most serious complication of NF, and the most common malignancy is neurofibrosarcoma or malignant schwannoma134 (Figure 9).
FIGURE 9.
A. Neurofibrosarcoma or malignant schwannoma in the buttock and left leg. B. Neurofibrosarcoma or malignant schwannoma compromising the buttock and left leg (dorsal view)
CLASSIFICATION
RICCARDI (1982) classified NF into eight types, whose designations, clinical features and patterns of inheritance are listed in table 1.26
Table 1.
Classification of neurofibromatosis (RICCARDI, 1982)
| Type | Inheritance Pattern | Clinical Characteristics |
| Neurofibromatosis (NF1) | AD | CLS, neurofibromas, Lisch nodules, axillary freckling, bone and neurological alterations, benign and malignant neoplasms |
| Acoustic (NF2) | AD | Bilateral acoustic neuromas, few CLS and neurofibromas |
| Mixed (NF3) | AD | Combination of 1 and 2 |
| Variant (NF4) | Unknown | Variations in CLS, neurofibromas, CNS neoplasms, Lisch nodules |
| Segmental (NF5) | Non-inheritable | Segmental neurofibromas and/ or CLS |
| Familial CLS (NF6) | Unknown | CLS |
| Late onset (NF7) | Unknown | After the third decade of life, neurofibromas, few CLS |
| Unspecified (NF8) | Unknown | Variable signs |
AD = autosomal dominant CLS = familial cafe au lait spots
Shortly after, Carey et al. (1986) proposed that NF be classified into only five types, based on distinct clinical features and genetic implications for the patient, as follows: NF1 - classical, NF2-acoustic, NF3segmental, NF4 - CALM - familial and NF5- NF-Noonan phenotype. This latter type has some common features with classical NF such as neurofibromas, café au lait spots, axillary freckling and Lisch nodules, as well as some features present in Noonan syndrome such as ptosis, malar hypoplasia, palpebral fissures, ocular hypertelorism, short neck, low implantation of nape hair, short stature, congenital heart defects, mental retardation and hypotonia. This suggests a new type of NF which was termed NF associated with Noonan phenotype.13
The most common type is NF1, and it justifies more than 90% of all cases. Previously known as Von Recklinghausen's disease, also peripheral or "usual" NF, it features café au lait spots, neurofibromas and multiple Lisch nodules.135
The clinical manifestations of neurofibromatosis were classified by Huson (1994) in "major", "minor" and associated complications.49 The "major" manifestations are specific to NF, affect most patients and are the basis of the diagnostic criteria of the National Institute of Health (1988).31 They are constituted by café au lait spots, axillary freckling, peripheral neurofibromas and Lisch nodules. The "minor" manifestations are specific to NF and also appear at a high frequency in those affected, but they are not used as diagnostic criteria. Macrocephaly and short stature are considered "minor" characteristics. The associated complications are those that involve the nervous, skeletal, genitourinary, endocrine, cardiovascular, respiratory, gastrointestinal and hematopoietic systems and the skin.48
DIAGNOSIS
The diagnosis of NF1 is basically clinical, and the criteria for diagnosing the disease were established in more detail in 1987, on the occasion of the "National Institute of Health Conference "in Bethesda, 31,136 It was established that, for NF diagnosis in its classic form, the presence of at least two or more of the following is necessary: six or more café au lait spots, two or more neurofibromas, at least one plexiform neurofibroma, axillary and inguinal freckling, optic glioma, two or more hamartomas in the iris (Lisch nodules), a typical bone lesion, and family recurrence in at least one first-degree relative.
PROGNOSIS
Patients with neurofibromatosis have a higher mortality rate when compared to the general population. Most deaths are related to the malignant transformation of tumors. In patients with NF1, mortality is higher in patients aged from 10 to 40 years and tends to be higher in women than in men.102
TREATMENT
Continuous research of the functions of the gene products of NF1 and NF2 have enabled better diagnosis and monitoring of affected individuals; however, despite advances, no medical treatment is available to prevent or reverse the typical lesions of neurofibromatosis. Instead, medical care is centered on genetic counseling and the early detection of complications that can be treated.
Excision of skin tumors and clinical or surgical treatment of injuries to other organ systems affected by the disease should be performed.
Based on the number of mast cells present in neurofibromas and on the fact that they may contribute to tumor growth, we can consider the use of drugs whose mechanism of action is to stabilize or block the degranulation of mast cells, so that they can prevent the release of histamine from granules and inhibit the metabolism of its development.64 With the use of these drugs, reduced pruritus, pain, and consistency of the tumor, as well as decreased tumor growth were observed. Consequently, the use of these drugs may, in clinical practice, hinder the development and growth of neurofibroma, especially in individuals who are diagnosed early.
QUESTIONS
1. It is incorrect to state the following about the development of malignant tumors in patients with neurofibromatosis type 1:
a) Patients with NF1 microdeletion have a higher risk of developing malignant peripheral nerve tumors compared to patients without this microdeletion.
b) They are associated with the presence of internal neurofibromas.
c) They are the leading cause of mortality in these patients.
d) The risk that these patients develop malignant peripheral nerve tumors throughout their lives is around 45% to 50%.
2. The inheritance pattern of neurofibromatosis is:
a) Autosomal recessive
b) Autosomal dominant
c) Sex-linked
d) Polygenic
3. It is correct to state the following about NF1:
a) All cases of NF1 have a family history.
b) The NF1 gene is located on the long arm of chromosome 17.
c) Clinical manifestations are very similar in a single family affected.
d) There is increased production of neurofibromin.
4. It is incorrect to state the following about café au lait spots in NF1:
a) When they occur in the axilla, they are called ephelides and are pathognomonic of NF1.
b) Presence of more than six spots greater than 0.5 cm in diameter before puberty or greater than 1.5 cm in diameter after puberty is suggestive of NF.
c) They are present at birth and do not increase in number - only in size- - over the years.
d) They occur in approximately 95% of patients.
5. It is correct to state the following about neurofibromas in NF1:
a) They are always multiple in patients with this disease.
b) Diffuse plexiform neurofibromas involve all layers of the skin and can penetrate deep into the muscles, reach the bone and, depending on location, affect the viscera.
c) They are exclusively formed by axonal processes.
d) Subcutaneous neurofibromas are rarely associated with pain.
6. It is incorrect to state the following about Lisch nodules in NF1:
a) They are hamartomatous lesions and are located on the surface of the iris.
b) They are associated with visual alterations in patients with NF1.
c) It is a major clinical manifestation with diagnostic significance.
d) It is a specific manifestation of NF1.
7. It is incorrect to state the following about bone changes in NF1:
a) Short stature and macrocephaly are minor characteristics of NF1.
b) Scoliosis is the most common spinal problem, being found in about half of the patients.
c) Meningocele may be present and is often asymptomatic.
d) Short stature is only associated to changes in bony structures, as NF1 patients show no associated growth disorders.
8. It is correct to state the following about the classification of neurofibromatosis:
a) NF1 is also known as peripheral NF and is responsible for about 90% of cases.
b) The classification by Riccardi was based on clinical criteria, not taking into account the inheritance pattern of various types of NF1.
c) NF2 was initially described as Von Recklinghausen's disease.
d) NF4 presents some characteristics that are common to classical NF and others associated with Noonan Syndrome.
9. It is correct to state the following about the diagnostic criteria for NF1:
a) They were established by the National Institute of Health (NIH), and presence of at least five characteristics of the disease are necessary to establish the diagnosis.
b) Short stature is a characteristic for the diagnosis of the disease.
c) Café au lait spots are considered diagnostic criteria when they are present in numbers greater than six.
d) Family recurrence in a first-degree relative is not a characteristic for the diagnosis of NF1.
10. It is correct to state the following about the prognosis of NF1:
a) The life expectancy of patients with this disease is equal to that of the general population.
b) Most patients develop malignant tumors throughout their lives.
c) Internal neurofibromas increase the risk of malignization.
d) Patients with a familial history of the disease have a better prognosis than those with spontaneous mutation.
11. It is correct to state the following about the treatment of NF1:
a) Tumor exeresis should not be performed as it stimulates new tumor development.
b) Drugs that block mast cell degranulation are associated with reduced pruritus, pain, and consistency of the tumor, as well as decreased tumor growth.
c) Medical monitoring is not required in the initial phase of the disease, being restricted to complications, since preventive treatments do not exist.
d) Genetic counseling may help prevent the development of malignant tumors.
12. It is incorrect to state the following about neurofibromatosis type 1:
a) It was initially described as Von Recklinghausen's disease.
b) It occurs due to inactivation of the NF1 gene.
c) It is one of the most prevalent autosomal recessive diseases in humans.
d) Its clinical manifestations mainly affect the skin, nervous system, bones and eyes.
13. It is incorrect to state the following about neurofibromatosis in children:
a) Clinical manifestations may be present at birth.
b) They generally have a low coefficient of intelligence and attention deficit.
c) Most of them have a short stature.
d) The presence of a single café au lait spot in childhood is a "major" diagnostic criterion.
14. Where is the NF1 gene located?
a) Chromosome 27
b) Chromosome 22
c) Chromosome 16
d) Chromosome 17
15. Which of the following is not considered a "major" characteristic of NF1?
a) Ephelides
b) Short stature
c) Neurofirbromas
d) Café au lait spots
16. Which of the following findings complete the diagnosis of NF1 according to the National Institute of Health Conference?
a) Two café au lait spots and scoliosis.
b) A subcutaneous neurofibroma and a first-degree relative.
c) Low Coefficient of Intelligence and two Lisch nodules
d) Ephelides and a plexiform neurofibroma
17. The following are typical of the NF1 gene, except:
a) Tumor suppression
b) Production of neurofibromin
c) Stimulation of cell division
d) Induction of neurofibroma formation when inactivated.
18. It is a pathognomonic sign of NF1:
a) Axillary freckling
b) Neurofibromas
c) Café au lait spots
d) Optic Glioma
19. It is correct to state the following about NF2:
a) It has some characteristics of NF associated with some features of Noonan Syndrome.
b) It represents the pathology of the "Elephant Man"
c) It presents bilateral acoustic neuromas as clinical features.
d) It has an unknown inheritance pattern.
20. It is INCORRECT to state the following about NF1:
a) NF1 has the following major characteristics: café au lait spots, axillary freckling, Lisch nodules and peripheral neurofibromas.
b) The "minor" characteristics of NF1 do not constitute diagnostic criteria of the disease.
c) Disease diagnosis is accomplished by the presence of two "major" characteristics or one "major" characteristic associated with a "minor" characteristic or two "minor" characteristics only.
d) Short stature and macrocephaly are "minor" characteristics of NF1.
| Answer key | |||
| Inherited epidermolysis bullosa: clinical and therapeutic aspects. An Bras Dermatol. 2013;88(2):185-98. | |||
| 1) b | 6) d | 11) b | 16) a |
| 2) d | 7) c | 12) b | 17) d |
| 3) a | 8) b | 13) b | 18) b |
| 4) a | 9) a | 14) d | 19) d |
| 5) b | 10) b | 15) c | 20) d |
Papers
Information for all members: The EMC-D questionnaire is now available at the homepage of the Brazilian Annals of Dermatology: www.anaisdedermatologia.org.br. The deadline for completing the questionnaire is 30 days from the date of online publication.
Footnotes
Work conducted at Faculdade de Medicina de São José do Rio Preto (FAMERP) - São José do Rio Preto (SP), Brazil.
Financial Support: None.
Conflict of Interests: None.
REFERENCES
- 1.Madigan P, Shaw RV. Neurofibromatosis in 13th century Austria? Neurofibromatosis. 1988;1:339–341. [PubMed] [Google Scholar]
- 2.Madigan P, Masello MJ. Report of neurofibromatosis - like case: Monstrorum Historia, 1642. Neurofibromatosis. 1988;2:53–56. [PubMed] [Google Scholar]
- 3.Riccardi VM. Neurofibromatosis: phenotype natural history and pathogenesis. 2. Baltimore: Johns Hopkins University Press; 1992. pp. 86; 498. [Google Scholar]
- 4.Canale DJ, Bebin J. Von Recklinghausen disease of the nervous system. In: Vinken PJ, Bruyn GW, editors. Handbook of clinical neurology. Vol. 14. Amsterdam: Holland Publishing Company; 1972. pp. 132–162. [Google Scholar]
- 5.Wander JV, Das Gupta TK. Neurofibromatosis. Curr Probl Surg. 1977;14:1–81. doi: 10.1016/s0011-3840(77)80002-6. [DOI] [PubMed] [Google Scholar]
- 6.Smith RW Jr. The dermal oleastoses. Arch Dermatol. 1963;88:382–392. doi: 10.1001/archderm.1963.01590220014002. [DOI] [PubMed] [Google Scholar]
- 7.Schmitt J. Vinken PJ, Bruyn GW. Handbook of clinical neurology. Vol. 14. Amsterdam: Holland Publishing Company; 1972. Visceral aspects of the phakomatosis; pp. 668–691. [Google Scholar]
- 8.Bricaire H, Fardeau M, Mazet PR. Endocrine disorders associated with the Phakomatosis. In: Vinken PJ, Bruyn GW, editors. Handbook of clinical neurology. Vol. 14. Amsterdam: Holland Publishing Company; 1972. pp. 731–744. [Google Scholar]
- 9.Treves F. A case of congenital deformity. Trans Pathol Soc Lond. 1885;36:494–498. [Google Scholar]
- 10.Murger A. Dermatological aspects of the phakomatosis. In: Vinken PJ, Bruyn GW, editors. Handbook of clinical neurology. Amsterdam: Holland Publishing Company; 1972. pp. 562–572. [Google Scholar]
- 11.Verocay J. Zur kenntnis der neurofibrome. Beitr Pathol Anat Allg Pathol. 1910;48:1–69. [Google Scholar]
- 12.Greggio H. Les cellules granuleuses (Mastzellen) dans les tissues normaux et dans certaines maladies churgicales. Arch Med Exp. 1911;23:323–323. [Google Scholar]
- 13.Hosoi K. Multiple neurofibromatosis (von Recklinghausen disease) with special reference to malignant transformation. Arch Surg. 1931;22:258–281. [Google Scholar]
- 14.Klatte EC, Franken EA, Smith JA. The radiographic spectrum in neurofibromatosis. Semin Roentgenol. 1976;11:17–33. doi: 10.1016/0037-198x(76)90061-4. [DOI] [PubMed] [Google Scholar]
- 15.Reubi F. Les vaisseaux et les glands endocrine dans la neurofibromatoses: le syndrome sympathicontonique dans la maladie de Recklinghausen. Schweiz Z Pathol Bacteriol. 1944;7:168–239. [Google Scholar]
- 16.Greene JF Jr, Fitzwater JE, Burgess J. Arterial hipertension associated with neurofibromatosis. Am J Clin Pathol. 1974;62:481–487. doi: 10.1093/ajcp/62.4.481. [DOI] [PubMed] [Google Scholar]
- 17.Schurch W, Messerli FH, Genest J, Lefebure R, Roy P, Cartier P, et al. Arterial hipertension and neurofibromatosis: renal artery stenosis and coarctation of abdominal aorta. Cand Med Assoc J. 1975;113:879–885. [PMC free article] [PubMed] [Google Scholar]
- 18.Russel DS, Rubenstein IJ. Pathology of tumors of the nervous system. Baltimore: Willians and Wilkins Co.; 1963. [Google Scholar]
- 19.Halpern M, Currarino G. Vascular lesion causing hypertension in neurofibromatosis. N Engl J Med. 1965;273:248–252. [Google Scholar]
- 20.Rosman NP, Pearce J. The brain in multiple neurofibromatosis (von Recklinghausen's disease): a suggested neuropathological basis for the associated mental defects. Brain. 1967;90:829–838. doi: 10.1093/brain/90.4.829. [DOI] [PubMed] [Google Scholar]
- 21.Brasfield JF, Das Gupta TK. Von Recklinghausen Disease: a clinicopathological study. Ann Surg. 1972;175:86–104. doi: 10.1097/00000658-197201000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chaves C, Bieler J, Morettor R. Neurofibromatose de von Recklinghausen. Rev Med HSE. 1972;24:177–201. [Google Scholar]
- 23.Isaacson P. Mast cells in benign nerve sheat tumours. J Pathol. 1976;119:193–196. doi: 10.1002/path.1711190402. [DOI] [PubMed] [Google Scholar]
- 24.Jurecka W, Lassmann H, Gebhart W. Classification of peripheral nerve sheath tumor. Arch Dermatol Res. 1977;258:100–100. [Google Scholar]
- 25.Gholam AP, Sanders DR, Goldberg ME. Albert DM, Jacobiec FA. Principles and practice of ophthalmology. Philadelphia: WB Saunders Company; 1980. The Phakomatosis; pp. 1197–1201. [Google Scholar]
- 26.Riccardi VM. Neurofibromatosis: clinical heterogeneity. Curr Probl Cancer. 1982;8:1–34. doi: 10.1016/s0147-0272(82)80016-0. [DOI] [PubMed] [Google Scholar]
- 27.Carey JC, Baty BJ, Johnson JP, Morrison T, Skolnik M, Kivlin J. The genetic aspects of neurofibromatosis. Ann NY Acad Sci. 1986;486:45–46. doi: 10.1111/j.1749-6632.1986.tb48061.x. [DOI] [PubMed] [Google Scholar]
- 28.Riccardi VM. Mast-cell stabilization to decrease neurofibroma growth. Preliminary experience with ketotifen. Arch Dermatol. 1987;123:1011–1016. [PubMed] [Google Scholar]
- 29.Barker DE, Wright K, Nguien K, Cannon L, Fain P, Goldgar D, et al. Gene for Von Recklinghausen neurofibromatosis is in the pericentric region of chromosome 17. Science. 1987;236:1100–1102. doi: 10.1126/science.3107130. [DOI] [PubMed] [Google Scholar]
- 30.Seizinger BR, Martuza RL, Gusella JF. Loss of genes on chromosome 22 in tumorigenesis of human acoustic neuroma. Nature. 1986;322:664–667. doi: 10.1038/322644a0. [DOI] [PubMed] [Google Scholar]
- 31.Neurofibromatosis. Conference statement. National Institutes of Health Consensus Development Conference. Arch Neurol. 1988;45:575–578. [PubMed] [Google Scholar]
- 32.Collins FS, O'connell P, Ponder BAJ, Seizinger BR. Progress towards identifying the neurofibromatosis (NF1) gene. Hum Genet Dis. 1989;5:217–221. doi: 10.1016/0168-9525(89)90085-1. [DOI] [PubMed] [Google Scholar]
- 33.Diehl SR, Boehnke M, Erickson RP, Ploughman LM, Seiler KA, Lieberman JL, et al. A refinated genetic maps of the region of chromosome 17 surrounding the von Recklinghausen neurofibromatosis (NF1) gene. Am J Human Genet. 1989;44:33–37. [PMC free article] [PubMed] [Google Scholar]
- 34.Fountain JW, Wallace MR, Bruce MA, Seizinger BR, Menon AG, Gusella JF, et al. Physical mapping of a translocation breakpoint in neurofibromatosis. Science. 1989;224:1085–1087. doi: 10.1126/science.2543076. [DOI] [PubMed] [Google Scholar]
- 35.O'Connel P, Leach RJ, Ledbetter DH, Cawthon RM, Culter M, Eldridge JR, et al. Fine structure DNA mapping studies of the chromosomal region harboring the genetic defect in neurofibromatosis type I. Am J Hum Genet. 1989;44:51–57. [PMC free article] [PubMed] [Google Scholar]
- 36.Stephens K, Green P, Riccardi VM, Ng S, Rising M, Barker D, Darby JK, et al. Genetic analysis of eight loci tightly linked to neurofibromatosis 1. Am J Hum Genet. 1989;44:13–19. [PMC free article] [PubMed] [Google Scholar]
- 37.Cawthon RM, Weiss R, Xu GF, Viskochil D, Culver M, Stevens J, et al. A major neurofibromatosis type-1 gene: cDNA sequence, genomic structure, and point mutations. Cell. 1990;62:193–201. doi: 10.1016/0092-8674(90)90253-b. [DOI] [PubMed] [Google Scholar]
- 38.Viskochil D, Buchberg AM, Xu G, Cawthon RM, Stevens J, Wolff RK, et al. Deletion and a translocation interrupt a cloned gene at the neurofibromatosis type 1 locus. Cell. 1990;62:187–192. doi: 10.1016/0092-8674(90)90252-a. [DOI] [PubMed] [Google Scholar]
- 39.Wallace MR, Marchuk DA, Andersen LB, Letcher R, Odeh HM, Saulino AM, et al. Type-1 neurofibromatosis gene: identification of a large transcript desrupted in three NF1 patients. Science. 1990;249:181–186. doi: 10.1126/science.2134734. [DOI] [PubMed] [Google Scholar]
- 40.Rouleau GA, Seizinger BR, Wertelecki W, Haines JL, Supermeau DW, Martuza RL, et al. Flanking markers bracket the neurofibromatosis type 2 (NF2) gene on chromosome 22. Am J Hum Genet. 1990;46:323–328. [PMC free article] [PubMed] [Google Scholar]
- 41.Wolf RK, Frazer KA, Jacker RK, Lanser MJ, Pitts LH, Cox DR. Analysis of chromosome22 deletions in neurofibromatosis type 2-related tumors. Am J Hum Genet. 1992;51:478–485. [PMC free article] [PubMed] [Google Scholar]
- 42.Rouleau GA, Merel P, Lutchman M, Sanson M, Zucman J, Marineuau C, et al. Alteration a new gene encoding a putative membrane-organizing protein causes neuro-fibromatosis type 2. Nature. 1993;363:515–521. doi: 10.1038/363515a0. [DOI] [PubMed] [Google Scholar]
- 43.Trofatter JA, MacCollin MM, Rutter JL, Murrell JR, Duyao MP, Parry DM, et al. A novel moesin-, ezrin-, radixin-like gene is a candidate for the neurofibromatosis 2 tumor suppressor. Cell. 1993;72:791–800. doi: 10.1016/0092-8674(93)90406-g. [DOI] [PubMed] [Google Scholar]
- 44.Legius E, Descheemaeker MJ, Steyaert J, Spaepen A, Vlietinck R, Casaer P, et al. Neurofibromatosis type 1 in childhood: correlation of MRI findings with intelligence. J Neurol Neurosurg Psychiatry. 1995;59:638–640. doi: 10.1136/jnnp.59.6.638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Andersen LB, Fountain JW, Gutmann DH, Tarlé SA, Glover TW, Dracopoli NC, et al. Mutation in the neurofibromatosis 1 gene in sporadic malignant melanoma cell lines. Nat Genet. 1993;3:118–121. doi: 10.1038/ng0293-118. [DOI] [PubMed] [Google Scholar]
- 46.Collins FS, O'connell P, Ponder BAJ, Seizinger BR. Progress towards identifying the neurofibromatosis (NF1) gene. Hum Genet Dis. 1989;5:217–221. doi: 10.1016/0168-9525(89)90085-1. [DOI] [PubMed] [Google Scholar]
- 47.Goloni-Bertollo EM, Antônio JR, Varella-Garcia M. Avaliação genético-clínico em neurofibromatose. An Bras Dermatol. 1994;69:311–322. [Google Scholar]
- 48.Goloni-Bertollo EM. Estudo genético-clínico e citogenético em neurofibromatose. São Paulo, SP: Universidade Estadual Paulista Júlio de Mesquita Filho; 1994. [Google Scholar]
- 49.Huson SM. Huson SM, Hughes RAC. The neurofibromatoses. A pathogenetic and clinical overview. Preface. London: Chapman & Hall; 1994. Neurofibromatosis: histological perspective, classification and diagnostic criteria. 7. Neurofibromatosis 1: a clinical and genetic overview. [Google Scholar]
- 50.Valerio NI. Neurofibromatose: gravidade da doença do ponto de vista de observadores e estratégias de enfrentamento. São José do Rio Preto, SP: Faculdade de Medicina de São José do Rio Preto; 1996. [Google Scholar]
- 51.Cnossen MH, Moons KG, Garssen MP, Pasmans NM, de Goede-Bolder A, Niermeijer MF, et al. Minor disease features in neurofibromatosis type 1 (NF1) and their possible value in diagnosis of NF1 in children < or = 6 years and clinically suspected of having NF1. J Med Genet. 1998;35:624–627. doi: 10.1136/jmg.35.8.624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Cnossen MH, de Goede-Bolder A, van den Broek KM, Waasdorp CM, Oranje AP, Stroink H, et al. A prospective 10 year follow up study of patients with neurofibromatosis type 1. Arch Dis Child. 1998;78:408–412. doi: 10.1136/adc.78.5.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kaste SC, Pivnick EK. Bony orbital morphology in neurofibromatosis type 1 (NF1) J Med Genet. 1998;35:628–631. doi: 10.1136/jmg.35.8.628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Howell SJ, Wilton P, Lindberg A, Shalet SM. Growth hormone replacement and the risk of malignancy in children with neurofibromatosis. J Pediatr. 1998;133:201–205. doi: 10.1016/s0022-3476(98)70245-8. [DOI] [PubMed] [Google Scholar]
- 55.Machado LA. Avaliação clínica, citogenética e molecular em pacientes portadores de NF. São Paulo, SP: Universidade Estadual Paulista Júlio de Mesquita Filho; 1998. [Google Scholar]
- 56.Nielsen GP, Stemmer-Rachamimov AO, Ino Y, Moller MB, Rosenberg AE, Louis DN. Malignant transformation of neurofibromas in neurofibromatosis 1 is associated with CDKN2A/p16 inactivation. Am J Pathol. 1999;155:1879–1884. doi: 10.1016/S0002-9440(10)65507-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Teixeira MF. Alterações oculares em Neurofibromatose Tipo 1 (NF1) São José do Rio Preto, SP: Faculdade de Medicina de São José do Rio Preto; 1999. [Google Scholar]
- 58.John AM, Ruggieri M, Ferner R, Upadhyaya M. A search for evidence of somatic mutations in the NF1 gene. J Med Genet. 2000;37:44–49. doi: 10.1136/jmg.37.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Szudek J, Birch P, Friedman JM. Growth in North American white children with neurofibromatosis 1 (NF1) J Med Genet. 2000;37:933–938. doi: 10.1136/jmg.37.12.933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ferner RE, Lucas JD, O'Doherty MJ, Hughes RA, Smith MA, Cronin BF, et al. Evaluation of fluorodeoxyglucose positron emission tomography (FDG PET) in the detection of malignant peripheral nerve sheath tumours arising from within plexiform neurofibromas in neurofibromatosis 1. J Neurol Neurosurg Psychiatry. 2000;68:353–357. doi: 10.1136/jnnp.68.3.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.DeBella K, Szudek J, Friedman JM. Use of the national institutes of health criteria for diagnosis of neurofibromatosis 1 in children. Pediatrics. 2000;105:608–614. doi: 10.1542/peds.105.3.608. [DOI] [PubMed] [Google Scholar]
- 62.Rasmussen SA, Yang Q, Friedman JM. Mortality in neurofibromatosis 1: an analysis using U.S. death certificates. Am J Hum Genet. 2001;68:1110–1118. doi: 10.1086/320121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Illés T, Halmai V, de Jonge T. Dubousset J.Decreased bone mineral density in neurofibromatosis-1 patients with spinal deformities. Osteoporos Int. 2001;12:823–827. doi: 10.1007/s001980170032. [DOI] [PubMed] [Google Scholar]
- 64.Antonio JR. Neurofibromatose: estudo genético-clínico, avaliação quantitativa dos mastócitos e dos componentes da matriz extracelular em neurofibromas. São José do Rio Preto, SP: Faculdade de Medicina de São José do Rio Preto; 2001. [Google Scholar]
- 65.Mautner VF, Kluwe L, Thakker SD, Leark RA. Treatment of ADHD in neurofibromatosis type 1. Dev Med Child Neurol. 2002;44:164–170. doi: 10.1017/s0012162201001876. [DOI] [PubMed] [Google Scholar]
- 66.Guillamo JS, Créange A, Kalifa C, Grill J, Rodriguez D, Doz F, et al. Prognostic factors of CNS tumours in Neurofibromatosis 1 (NF1): a retrospective study of 104 patients. Brain. 2003;126:152–160. doi: 10.1093/brain/awg016. [DOI] [PubMed] [Google Scholar]
- 67.Evans DG, Baser ME, McGaughran J, Sharif S, Howard E, Moran A. Malignant peripheral nerve sheath tumours in neurofibromatosis 1. J Med Genet. 2002;39:311–314. doi: 10.1136/jmg.39.5.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Singhal S, Birch JM, Kerr B, Lashford L, Evans DGR. Neurofibromatosis type 1 and sporadic optic gliomas. Arch Dis Child. 2002;87:65–70. doi: 10.1136/adc.87.1.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Ars E, Kruyer H, Morell M, Pros E, Serra E, Ravella A, et al. Recurrent mutations in the NF1 gene are common among neurofibromatosis type 1 patients. J Med Genet. 2003;40:e82. doi: 10.1136/jmg.40.6.e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.De Raedt T, Brems H, Wolkenstein P, Vidaud D, Pilotti S, Perrone F, et al. Elevated risk for MPNST in NF1 microdeletion patients. Am J Hum Genet. 2003;72:1288–1292. doi: 10.1086/374821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Cunha KSG, Barboza EP, Da Fonseca EC. Identification of growth hormone receptor in localised neurofibromas of patients with neurofibromatosis type 1. J Clin Pathol. 2003;56:758–763. doi: 10.1136/jcp.56.10.758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ozerdem U. Targeting Neovascular Pericytes in Neurofibromatosis type 1. Angiogenesis. 2004;7:307–311. doi: 10.1007/s10456-004-6643-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kuorilehto T, Pöyhönen M, Bloigu R, Heikkinen J, Väänänen K, Peltonen J. Decreased bone mineral density and content in neurofibromatosis type 1: lowest local values are located in the load-carrying parts of the body. Osteoporos Int. 2005;16:928–936. doi: 10.1007/s00198-004-1801-4. [DOI] [PubMed] [Google Scholar]
- 74.Mattocks C, Baralle D, Tarpey P, ffrench-Constant C, Bobrow M, Whittaker J. Automated comparative sequence analysis identifies mutations in 89% of NF1 patients and confirms a mutation cluster in exons 11-17 distinct from the GAP related domain. J Med Genet. 2004;41:e48. doi: 10.1136/jmg.2003.011890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Yang G, Khalaf W, van de Locht L, Jansen JH, Gao M, Thompson MA, et al. Transcriptional repression of the Neurofibromatosis-1 tumor suppressor by the t(8;21) fusion protein. Mol Cell Biol. 2005;25:5869–5879. doi: 10.1128/MCB.25.14.5869-5879.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Venturin M, Guarnieri P, Natacci F, Stabile M, Tenconi R, Clementi M, et al. Mental retardation and cardiovascular malformations in NF1 microdeleted patients point to candidate genes in 17q11.2. J Med Genet. 2004;41:35–41. doi: 10.1136/jmg.2003.014761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ferner RE, Hughes RA, Hall SM, Upadhyaya M, Johnson MR. Neurofibromatous neuropathy in neurofibromatosis 1 (NF1) J Med Genet. 2004;41:837–841. doi: 10.1136/jmg.2004.021683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Muniz MP. Lesões ósseas no diagnóstico de neurofibromatose. São José do Rio Preto, SP: Faculdade de Medicina de São José do Rio Preto; 2004. [Google Scholar]
- 79.Tucker T, Wolkenstein P, Revuz J, Zeller J, Friedman JM. Association between benign and malignant peripheral nerve sheath tumors in NF1. Neurology. 2005;65:205–211. doi: 10.1212/01.wnl.0000168830.79997.13. [DOI] [PubMed] [Google Scholar]
- 80.Johannessen CM, Reczek EE, James MF, Brems H, Legius E, Cichowski K. The NF1 tumor suppressor critically regulates TSC2 and mTOR. Proc Natl Acad Sci U S A. 2005;102:8573–8578. doi: 10.1073/pnas.0503224102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.De Schepper S, Boucneau J, Vander Haeghen Y, Messiaen L, Naeyaert JM, Lambert J. Cafe-au-lait spots in neurofibromatosis type 1 and in healthy control individuals: hyperpigmentation of a different kind? Arch Dermatol Res. 2006;297:439–449. doi: 10.1007/s00403-006-0644-6. [DOI] [PubMed] [Google Scholar]
- 82.Page PZ, Page GP, Ecosse E, Korf BR, Leplege A, Wolkenstein P. Impact of neurofibromatosis 1 on Quality of Life: a cross-sectional study of 176 American cases. Am J Med Genet A. 2006;140:1893–1898. doi: 10.1002/ajmg.a.31422. [DOI] [PubMed] [Google Scholar]
- 83.Levine TM, Materek A, Abel J, O'Donnell M, Cutting LE. Cognitive profile of neurofibromatosis type 1. Semin Pediatr Neurol. 2006;13:8–20. doi: 10.1016/j.spen.2006.01.006. [DOI] [PubMed] [Google Scholar]
- 84.Rübben A, Bausch B, and Nikkels A. Somatic deletion of the NF1 gene in a neurofibromatosis type 1-associated malignant melanoma demonstrated by digital PCR. Mol Cancer. 2006;5:36–36. doi: 10.1186/1476-4598-5-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Lim R, Jaramillo D, Poussaint TY, Chang Y, Korf B. Superficial neurofibroma: a lesion with unique MRI characteristics in patients with neurofibromatosis type 1. AJR Am J Roentgenol. 2005;184:962–968. doi: 10.2214/ajr.184.3.01840962. [DOI] [PubMed] [Google Scholar]
- 86.Muniz MP, Ferraz F, Lopes JR, Souza AS, Zanusso SH, Bertelli ECP, Bertollo EMGi. Neurofibromatosis type 1: clinical and radiological aspects. Rev Imagem. 2006;28:87–96. [Google Scholar]
- 87.Yoshida Y, Sato N, Furumura M, Nakayama J. Treatment of pigmented lesions of neurofibromatosis 1 with intense pulsed-radio frequency in combination with topical application of vitamin D3 ointment. J Dermatol. 2007;34:227–230. doi: 10.1111/j.1346-8138.2007.00258.x. [DOI] [PubMed] [Google Scholar]
- 88.Hanemann CO, Hayward C, Hilton DA. Neurofibromatosis type 1 with involvement of the enteric nerves. J Neurol Neurosurg Psychiatry. 2007;78:1163–1164. doi: 10.1136/jnnp.2007.120451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Stevenson DA, Moyer-Mileur LJ, Murray M, Slater H, Sheng X, Carey JC, et al. Bone Mineral Density in Children and Adolescents with Neurofibromatosis Type 1. J Pediatr. 2007;150:83–88. doi: 10.1016/j.jpeds.2006.10.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Brems H, Chmara M, Sahbatou M, Denayer E, Taniguchi K, Kato R, et al. Germline loss-of-function mutations in SPRED1 cause a neurofibromatosis 1-like phenotype. Nat Genet. 2007;39:1120–1126. doi: 10.1038/ng2113. [DOI] [PubMed] [Google Scholar]
- 91.Brunetti-Pierri N, Doty SB, Hicks J, Phan K, Mendoza-Londono R, Blazo M, et al. Generalized metabolic bone disease in Neurofibromatosis type I. Molecular Genetics and Metabolism. 2008;94:105–111. doi: 10.1016/j.ymgme.2007.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Carroll, Ratner Nancy. How Does the Schwann Cell Lineage Form Tumors in NF1? Glia. 2008;56:1590–1605. doi: 10.1002/glia.20776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.McKeever K, Shepherd CH, Crawford H, Morrison PJ. An epidemiological, clinical and genetic survey of Neurofibromatosis type 1 in children under sixteen years of age. Ulster Med J. 2008;77:160–163. [PMC free article] [PubMed] [Google Scholar]
- 94.Krab LC, de Goede-Bolder A, Aarsen FK, Pluijm SM, Bouman MJ, van der Geest JN, et al. Effect of simvastatin on cognitive functioning in children with neurofibromatosis type 1: a randomized controlled trial. JAMA. 2008;300:287–294. doi: 10.1001/jama.300.3.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Stevenson DA, Schwarz EL, Viskochil DH, Moyer-Mileur LJ, Murray M, Firth SD, et al. Evidence of Increased Bone Resorption in Neurofibromatosis Type 1 Using Urinary Pyridinium Crosslink Analysis. Pediatr Res. 2008;63:697–701. doi: 10.1203/PDR.0b013e31816fee45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Boley S, Sloan JL, Pemov A, Stewart DR. A Quantitative assessment of the burden and distribution of Lisch nodules in adults with neurofibromatosis type 1. Invest Ophthalmol Vis Sci. 2009;50:5035–5043. doi: 10.1167/iovs.09-3650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Brems H, Park C, Maertens O, Pemov A, Messiaen L, Upadhyaya M, et al. Glomus tumors in neurofibromatosis type 1: genetic, functional, and clinical evidence of a novel association. Cancer Res. 2009;69:7393–7401. doi: 10.1158/0008-5472.CAN-09-1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Boyd KP, Gao L, Feng R, Beasley M, Messiaen L, Korf BR, et al. Phenotypic variability among café-au-lait macules in neurofibromatosis type 1. J Am Acad Dermatol. 2010;63:440–447. doi: 10.1016/j.jaad.2009.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Turbyville TJ, Gürsel DB, Tuskan RG, Walrath JC, Lipschultz CA, Lockett SJ, et al. Schweinfurthin A selectively inhibits proliferation and Rho signaling in glioma and neurofibromatosis type 1 tumor cells in a NF1-GRD-dependent manner. Mol Cancer Ther. 2010;9:1234–1243. doi: 10.1158/1535-7163.MCT-09-0834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Johnson BA, MacWilliams BA, Carey JC, Viskochil DH, D'Astous JL, Stevenson DA. Motor Proficiency in Children with Neurofibromatosis Type 1. Pediatr Phys Ther. 2010;22:344–348. doi: 10.1097/PEP.0b013e3181f9dbc8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Kolanczyk M, Mautner V, Kossler N, Nguyen R, Kühnisch J, Zemojtel T, et al. MIA is a potential biomarker for tumour load in neurofibromatosis type 1. BMC Med. 2011;9:82–82. doi: 10.1186/1741-7015-9-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Duong TA, Sbidian E, Valeyrie-Allanore L, Vialette C, Ferkal S, Hadj-Rabia S, et al. Mortality associated with neurofibromatosis 1: a cohort study of 1895 patients in 1980-2006 in France. Orphanet J Rare Dis. 2011;6:18. doi: 10.1186/1750-1172-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Sbidian E, Bastuji-Garin S, Valeyrie-Allanore L, Ferkal S, Lefaucheur JP, Drouet A, et al. At-risk phenotype of neurofibromatose-1 patients: a multicentre case-control study. Orphanet J Rare Dis. 2011;6:51–51. doi: 10.1186/1750-1172-6-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Pasmant E, Masliah-Planchon J, Lévy P, Laurendeau I, Ortonne N, Parfait B, et al. Identification of genes potentially involved in the increased risk of malignancy in NF1-microdeleted patients. Mol Med. 2011;17:79–87. doi: 10.2119/molmed.2010.00079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Upadhyaya M, Spurlock G, Thomas L, Thomas NS, Richards M, Mautner VF, et al. Microarray-based copy number analysis of neurofibromatosis type-1 (NF1)-associated malignant peripheral nerve sheath tumors reveals a role for Rho-GTPase pathway genes in NF1 tumorigenesis. Hum Mutat. 2012;33:763–776. doi: 10.1002/humu.22044. [DOI] [PubMed] [Google Scholar]
- 106.Kantaputra PN, van den Ouweland A, Sangruchi T, Limwongse C. Severe plexiform facial neurofibromatosis, type 1 with underdeveloped eyes and a novel NF1 mutation. Am J Med Genet A. 2012;158A:1750–1753. doi: 10.1002/ajmg.a.35422. [DOI] [PubMed] [Google Scholar]
- 107.Chaudhary N, Borker A. Metronomic therapy for malignant peripheral nerve sheath tumor in neurofibromatosis type 1. Pediatr Blood Cancer. 2012;59:1317–1319. doi: 10.1002/pbc.24245. [DOI] [PubMed] [Google Scholar]
- 108.Gong M, Ma J, Li M, Zhou M, Hock JM, Yu X. MicroRNA-204 critically regulates carcinogenesis in malignant peripheral nerve sheath tumors. Neuro Oncol. 2012;14:1007–1017. doi: 10.1093/neuonc/nos124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Jett K, Friedman JM. Clinical and genetic aspects of neurofibromatosis 1. Genet Med. 2010;12:1–11. doi: 10.1097/GIM.0b013e3181bf15e3. [DOI] [PubMed] [Google Scholar]
- 110.Williams VC, Lucas J, Babcock MA, Gutmann DH, Korf B, Maria BL. Neurofibromatosis Type 1 Revisited. Pediatrics. 2009;123:124–133. doi: 10.1542/peds.2007-3204. [DOI] [PubMed] [Google Scholar]
- 111.Pulst SM. Prenatal diagnosis of the neurofibromatosis. Clin Perinatol. 1990;17:829–844. [PubMed] [Google Scholar]
- 112.Ross KL. The neurofibromatosis. ENT J. 1992;71:512–518. [Google Scholar]
- 113.Valero MC, Martín Y, Hernández-Imaz E, Marina Hernández A, Meleán G, Valero AM, et al. A hightly sensitive genetic protocol to detect NF1 mutations. J Mol Diagn. 2011;13:113–122. doi: 10.1016/j.jmoldx.2010.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Declue JE, Cohen BD, Lowy DR. Identification and characterization of the neurofibromatosis type 1 protein product. Proc natl Acad Sc USA. 1991;88:9914–9918. doi: 10.1073/pnas.88.22.9914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Daston MM, Scrable H, Nordlund M, Sturbaum AK, Nissen LM, Ratner N. The protein product of neurofibromatosis type 1 gene is expressed at highest abundance in neurons, Scwann cells, and oligodendrocytes. Neuron. 1992;8:415–428. doi: 10.1016/0896-6273(92)90270-n. [DOI] [PubMed] [Google Scholar]
- 116.Norduland M, Gu X, Shipley MT, Ratner N. neurofibrin is enriched in the endoplasmic reticulum of CNS neurons. J Neurosci. 1993;13:1588–1600. doi: 10.1523/JNEUROSCI.13-04-01588.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Martin GA, Viskochil D, Bollag G, McCabe PC, Crosier WJ, Haubruck H, et al. The GAP-related domain of the neurofibromatosis type 1 gene product interacts with ras p21. Cell. 1990;63:843–849. doi: 10.1016/0092-8674(90)90150-d. [DOI] [PubMed] [Google Scholar]
- 118.Boguski MS, McCormick F. Proteins regulating Ras and its relatives. Nature. 1993;366:643–654. doi: 10.1038/366643a0. [DOI] [PubMed] [Google Scholar]
- 119.Trovó-Marqui AB, Tajara EH. Neurofibromin: a general Outlook. Clin Genet. 2006;70:1–13. doi: 10.1111/j.1399-0004.2006.00639.x. [DOI] [PubMed] [Google Scholar]
- 120.Rasmussen SA, Friedman JM. NF1 Gene and neurofibromatosis 1. Am J Epidemiol. 2000;151:33–40. doi: 10.1093/oxfordjournals.aje.a010118. [DOI] [PubMed] [Google Scholar]
- 121.Tonsgard JH. Clinical manifestations and management of neurofibromatosis type 1. Semin Pediatr Neurol. 2006;13:2–7. doi: 10.1016/j.spen.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 122.Ferner RE. Neurofibromatosis 1. Eur J Hum Genet. 2007;15:131–138. doi: 10.1038/sj.ejhg.5201676. [DOI] [PubMed] [Google Scholar]
- 123.Williams VC, Lucas J, Babcock MA, Gutmann DH, Korf B, Maria BL. Neurofibromatosis type 1 revisited. Pediatrics. 2009;123:124–133. doi: 10.1542/peds.2007-3204. [DOI] [PubMed] [Google Scholar]
- 124.Crowe FW, Schull WJ. Diagnostic importance of café-au-lait spot in neurofibromatoses. Arch Intern Med. 1953;91:758–766. doi: 10.1001/archinte.1953.00240180067008. [DOI] [PubMed] [Google Scholar]
- 125.Riccardi VM. Pathophyology of neurofibromatosis. Dermatological insights into heterogeneity and pathogenesis. J Am Acad Dermatol. 1980;3:157–166. [PubMed] [Google Scholar]
- 126.Zhu Y, Ghosh P, Charnay P, Burns DK, Parada LF. Neurofibromas in NF1: Schwann cell origin and role of tumor environment. Science. 2002;296:920–922. doi: 10.1126/science.1068452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Aloi F, Massobrio R. Solitary plexiform neurofibroma. Dermatologica. 1989;179:84–86. doi: 10.1159/000248318. [DOI] [PubMed] [Google Scholar]
- 128.Lubs MLE, Bauer M.J, Formas ME, Djokic B. Lisch nodules in neurofibromatosis type 1. N Engl J Med. 1991;324:1264–1266. doi: 10.1056/NEJM199105023241807. [DOI] [PubMed] [Google Scholar]
- 129.Gordon RRS. Measurement of cranial capacity in children. Br J Radiol. 1966;39:377–377. [Google Scholar]
- 130.Holt JF, Kuhns LR. Macrocranium and macroencephaly in neurofibromatosis. Skeletal Radiol. 1976;1:25–28. [Google Scholar]
- 131.Sengpiel GW, Ruzicka FF, Lodnnel EA. Lateral intra thoracic meningocele. Radiology. 1968;50:515–520. doi: 10.1148/50.4.515. [DOI] [PubMed] [Google Scholar]
- 132.Handa J, Kayama T, Shimizy Y, Yoneda S. Skull defect involving the lambdoid suture in neurofibromatosis. Surg Neurol. 1975;3:119–121. [PubMed] [Google Scholar]
- 133.Pitt MJ, Mosher JF, Edeiken J. Periosteum and abnormal bone in neurofibromatosis. Radiology. 1972;103:143–146. doi: 10.1148/103.1.143. [DOI] [PubMed] [Google Scholar]
- 134.Korf BR. Malignancy in neurofibromatosis type 1. Oncologist. 2000;5:477–485. doi: 10.1634/theoncologist.5-6-477. [DOI] [PubMed] [Google Scholar]
- 135.Souza JF, Toledo LL, Ferreira MC, Rodrigues LO, Rezende NA. Neurofibromatosis type 1: more frequent and severe then usually thought. Rev Assoc Med Bras. 2009;55:394–399. doi: 10.1590/s0104-42302009000400012. [DOI] [PubMed] [Google Scholar]
- 136.Niimura M. Neurofibromatoses: in Dermatology Progress and Perspective; The proceedings of the 18th World Congress of Dermatology; New York. The Parthenon Publishing Group Inc.; 1993. pp. 767–768. [Google Scholar]