Abstract
Malakoplakia is a rare acquired disease that can affect many systems but is more common in the urogenital tract. Cutaneous malakoplakia is even rarer. It is far more frequent in immunodeficient patients. We report a case of cutaneous malakoplakia in a kidney transplant patient who had recently stopped receiving immunosuppressive therapy to illustrate a review of the relevant recent literature.
Keywords: Kidney Transplantation, Malacoplakia, Review, Skin
Abstract
Malacoplaquia é uma doença adquirida rara que pode afetar diversos órgãos e sistemas, mas é mais comum no trato urogenital. O acometimento cutâneo é ainda menos frequente. Atinge principalmente imunodeficientes. Relatamos caso de malacoplaquia cutânea em um paciente transplantado renal que havia recentemente deixado de receber a terapia imunossupressora, a fim de ilustrar uma revisão da literatura recente relevante.
INTRODUCTION
Malakoplakia is a term derived from the Greek, meaning "soft plaque".1,2 The disease was first described in 1902 by Michaelis and Gutman.3 It describes a granulomatous process of infectious etiol ogy triggered by bacteria that occurs preferentially in subjects affected by primary or secondary immunodeficiency.4,5 The pathogenesis of malakoplakia remains poorly understood, and it is thought to represent an acquired bactericidal defect of macrophages associat ed with infection, immunosuppression, and/or immunosuppressive agentes.4.6,7
The most common site of occurrence is the urogenital tract, although the condition has also been found to affect the gastrointestinal and respiratory tracts, retroperitoneum, thyroid gland, lymph nodes, bones/joints, middle ear, eyes and brain.4-9 The condition has been considered rare, and cutaneous malako plakia is even rarer; the first case was reported by Leclerc and Bernier in 1972.10
We report a case of cutaneous malakoplakia in a kidney transplant recipient and proceed with a review of the topic.
CASE REPORT
A 51-year-old white man from Brazil, suffering from idiopathic chronic renal failure, presented with a immunosuppressive agentes.4.6,7 2-year history of asymptomatic cutaneous lesion on the left groin, noticed by his nephrologist during hospitalization due to sepsis caused by catheter infection.
The patient was frequently catheterized at this site since an unsuccessful kidney transplantation 2 years before.
The lesion was a yellow-erythematous-purple plaque measuring around 1 cm in diameter, on the left groin, near a femoral vein catheter (Figure 1).
FIGURE 1.

Malakoplakia: Picture of the yellow-erythematous- purple plaque measuring little more than 1 cm in diameter on the left groin of the patient near a femoral vein cateter
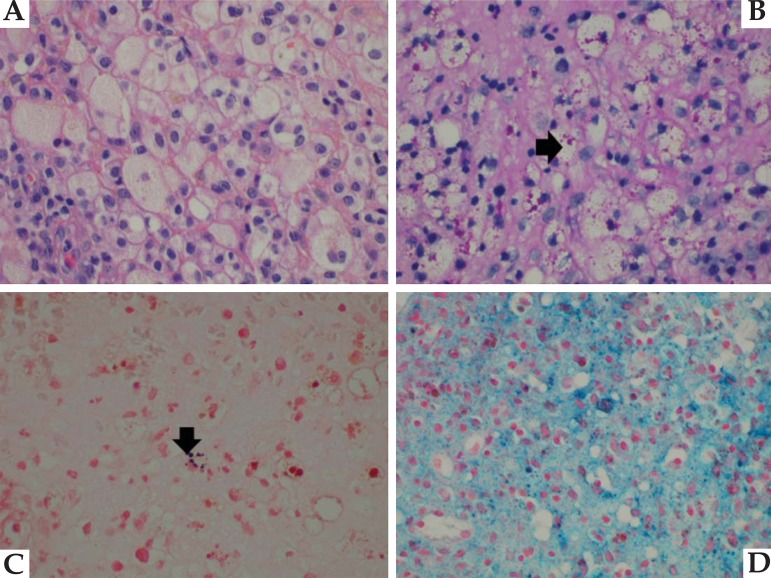
The lesion was sampled for histopathologic and culture studies. The culture results revealed the growth of Providentia spp and Candida albicans. Histopathologic analysis revealed a chronic inflammatory process characterized by sheets of closely packed macrophages containing PAS-positive inclusions (von Hansemann cells) and calcospherites known as Michaelis-Gutmann bodies, as demonstrated by Von Kossa stain, which shows the homogeneous bodies in black (Figures 2A, 2B e 2C). Prussian blue staining demonstrated the presence of hemosiderin inside macrophages, which may explain the purple color of the lesion (Figure 2D).
FIGURE 2.
Malakoplakia: A-hematoxylin-eosin (400 X) stain showing the sheets of macrophages. B-von Hansemann cells in PAS stain (400 X)(black arrow). C-Michaelis- Gutmann bodies, shown in black after Von Kossa staining (400 X)(black arrow). D-Prussian blue demonstrates hemosiderin inside macrophages (400 X)
The patient was treated with surgical excision in association with sulfametoxazol-trimetoprin antibiotic therapy. No evidence of recurrence was detected on 3-year follow-up, as shown in figure 3.
FIGURE 3.

Malakoplakia: Left groin picture of the same patient after treatment and 3-year follow-up
DISCUSSION
Malakoplakia is a rare granulomatous disease in which a defect of the killing capacity of macrophages after endocytosis is considered to be the central event. Disturbed phagosome-lysosome fusion was suggested, but it is still not clear how and why this disorder happens, and the hypothesis is not fully accepted.11-13 We reviewed published articles in indexed periodicals that appeared in a PubMed search performed using the term "cutaneous malakoplakia". Based on Kohl et al. 2008, we added cases of cutaneous malakoplakia published from January 2006 until January 2012, as demonstrated in chart 1. 14
CHART 1.
Reported cases of cutaneous Malakoplakia
| Reported Cases of Cutaneous Malakoplakia in the Literature* | |||||
| Case No. | Reference No. | Age/Sex | Location | Gross | Medical History |
| 1 | 5 | 51 y/M | Perianal, inguinal, scrotum | Nodules and ulcerations | Kidney Tx |
| 2 | 5 | 67 y/M | Right temple | Nodule | Kidney Tx |
| 3 | 33 | 69 y/F | Right axilla | Ulceration and mass | RA, breast carcinoma |
| 4 | 34 | 40 y/F | Inguinal, broad ligament | Ulceration | N/A |
| 5 | 10 | 64 y/M | Perianal | Indurated mass | RA |
| 6 | 35 | 35 y/M | Left eyelid | Nodule | Kidney Tx |
| 7 | 1 | 64 y/M | Perianal | Ulceration | Lymphoma |
| 8 | 36 | 75 y/F | Vulva | Ulceration | RA |
| 9 | 37 | 50 y/F | Abdominal wound | Polypoid mass | N/A |
| 10 | 38 | 31 y/M | Right axilla | Mass | HIV |
| 11 | 9 | 32 y/M | Abdomen | Abdomen Abscess | Kidney Tx |
| 12 | 9 | 44 y/M | Perianal and left lung | Abscess | Kidney Tx |
| 13 | 9 | 42 y/M | Right axilla | Chronic abscess | SLE |
| 14 | 39 | 70 y/M | Buttock | Nodule | Chronic hepatitis C |
| 15 | 40 | 75 y/M | Right hand and wrist | Abscess | N/A |
| 16 | 41 | 41 y/M | Peritoneal, supraclavicular | Cystic mass and firm nodule | DM |
| 17 | 42 | 74 y/M | Perianal | Nonhealing lesion | MPD |
| 18 | 43 | 55 y/M | Gluteal cleft | Ulcers | HIV |
| 19 | 44 | 67 y/M | Left neck | Mass | No significant PMH |
| 20 | 45 | 81 y/F | Frontal mass | Irregular plaque | DM |
| 21 | 46 | 56 y/M | Internal canthus of eye | Nodule | Sarcoidosis |
| 22 | 32 | 44 y/F | Buttock | Nodule | Kidney Tx |
| 23 | 47 | 60 y/F | Nasolabial sulcus | Ulceration | N/A |
| 24 | 14 | 2 mo/M | Colorectal and perianal | Polypoid masses | Immunodeficiency |
| 25 | 2 | 68 y/M | Left inguinal region | Papules | N/A |
| 26 | 2 | 66 y/M | Right axilla | Nodule | RA, DM |
| 27 | 48 | 53 y/F | Perineum | Papules | Kidney Tx |
| 28 | 49 | 42 y/M | Inguinal region | Mass with ulceration | Lymphoma |
| 29 | 50 | 41 y/M | Frontal scalp, right lung | Abscess, pulmonary lesions | HIV, Hepatitis B |
| 30 | 51 | 64 y/F | Left neck mass | Mass with cavitation | Thyroidectomy |
| 31 | 52 | 60 y/M | Gluteal fold | Cutaneous fistula | DM |
| 32 | 53 | 62 y/M | Chest | Ulceration | N/A |
| 33 | 54 | 65 y/M | Ureterocutaneous fistula | Abdominal fistula | N/A |
| 34 | 19 | 51 y/M | Perianal | Nodule | Heart Tx |
| 35 | 55 | 69 y/M | Left arm and flank | Ulceration, mass | Escherichia coli sepsis |
| 36 | 56 | 55 y/F | Abdominal wall | Papules | N/A |
| 37 | 57 | 22 y/F | Arm | Fluctuating mass | N/A |
| 38 | 58 | 52 y/F | Inferior abdomen | Fistula with abscess | Kidney Tx |
| 39 | 59 | 30 y/M | Perianal | Abscesses | Dermatomyositis |
| 40 | 60 | 51 y/M | Left thigh | Mass with draining abscess | HIV, DM |
| 41 | 16 | 60 y/F | Abdominal fold | Pink-yellow plaques | Healthy |
| 42 | 17 | 23 y/M | Perianal | Pink nodules | Healthy |
| 43 | 18 | 14 Y/M | Gluteal fold | Papule | Healthy |
| 44 | 20 | 55 y/F | Right Labia | "Boil" (nodule + abscess) | Heart Tx |
| 45 | 27 | 58 y/M | Perianal | Erosive plaque | Psoriasis |
| 46 | 61 | 63 y/F | Abdominal wall | Fistula | Pulmonary sarcoidosis |
| 47 | 62 | 83 y/F | Neck | Goma (nodule + fistula) | SLE, RA, Sjogren |
| 48 | 63 | 45 y/F | Perigenital | Papules, nodules and sinuses | HIV |
| 49 | 64 | 24 y/M | Abdominal wall | Fistula | Psoas abscess (Tuberculosis?) |
| 50 | 65 | 87 y/M | Buttock | Scaly plaques and polypoid nodules | No significant PMH |
| 51 | 66 | 66 y/M | Lower abdomen | Abscesses, nodules and fistula | Poor overall health |
| 52 | current article case | 51 y/M | Left groin | Plaque | Kidney Tx |
While the majority of subjects are immunodeficient patients, including HIV-infected patients, patients with neoplasia, transplanted patients and others, more recently cases involving previously healthy patients have been reported.15-17 Almost all transplanted patient cases refer to kidney recipients, as the one in this article, but two were reported in heart transplant recipients.18,19 There are few reports in which prevalence among women is higher (2:1).20,21 The age peak occurs between the sixth and seventh decades, being even rarer in children.17,22
Approximately 90% of patients have coliform bacteria detected in urine, blood, or tissue, suggesting an infectious cause.4 The most commonly found bacterium is Escherichia coli, but Klebsiella, Proteus, Pseudomonas, Mycobacterium avium, Mycobacterium tuberculosis, Shigella, Staphylococcus aureus and Enterococcus spp were also found.23,24 Rhodococcus equi is the most commonly implicated microbe in HIV-infected patients.25 In 75% of cases, the disease affects the genitourinary tract, but other systems have been implicated, including the skin.26
No typical clinical presentation is described, skin presentation varies from papules, plaques, nodules, abscesses with or without fluctuation, and fistula to ulcers, cystic and polypoid masses.14 Therefore, the diagnosis is predominantly confirmed by anatomopathologic and culture studies. Vanbrabant et al.2004 recently described the possibility of using 18fluoro-deoxyglucose positron emission tomography for diagnosis and follow-up.27
Histopathologically, the pathognomonic finding of Michaelis-Gutmann bodies, which represent partially degraded bacterial organisms, can establish the diagnosis. Michaelis-Gutmann bodies are intracytoplasmic, round-ovoid, basophilic, concentric laminated inclusions in macrophages that are typically enlarged and display foamy cytoplasm and eccentric, hyperchromatic, round nuclei, denoted as Hansemann cells.
Differential diagnosis is possible with other infectious diseases or neoplastic and reactive/reparative processes. Infections to consider include tuberculosis, Whipple's disease, lepromatous leprosy, fungus (Cryptococcus), and parasites (leishmaniasis). Special stains for microorganisms and tissue culture are necessary. Reactive and neoplastic processes include Langerhans cell histiocytosis, fibrous histiocytoma, lymphoma, granular cell tumor, xanthoma, foreign-body granuloma, hemophagocytic syndromes, and sarcoidosis.14 Although generally presenting benign self-limited evolution, a fatal outcome is possible, but none was described in cutaneous malakoplakia.28 Pseudomalakoplakia was once described as a proliferation of histiocytes at a previous surgical site, but only as an abstract. No other publications on this theme are found.29
Our observation that the disease developed on a site of recognized trauma and contamination, in accordance with other related cases, highlights the importance of direct inoculation of bacteria in the pathophysiology, since the presence of immunosuppression is necessary, but not sufficient for its development.
There are no prospective comparative studies, probably due to the limited incidence, so approaches to management vary from surgical excision, with or without antibiotics, to the use of antibiotics alone.8 Van der Voort et al. 1996 compared treatments and concluded that surgical excision achieved the higher cure rate (90%), and that, when comparing antibiotics, quinolones seemed to be superior.7 The discontinuation of immunosuppressives and treatment of HIV could also be helpful.7,9 Sulfamethoxazole-trimethoprim is also cited as effective.30 It was selected by us due to considerations such as cost, access and drug interaction.
We illustrated this article reporting a case of cutaneous malakoplakia synchronous to previous immunosuppressive therapy, in a subject with no current immunosuppressive treatment. The option for surgical plus antibiotic treatment resulted in cure with no recurrence to date. We also reviewed the literature and counted the reported cases of cutaneous malakoplakia described on chart 1 (including this one).31-66
Footnotes
Syudy carried out at the Dermatology Department of Paulista Medical School (Departamento de Dermatologia da Escola Paulista de Medicina - UNIFESP) - São Paulo (SP) Brazil.
Financial funding: None
Conflict of interest: None
REFERENCES
- 1.Almagro UA, Choi H, Caya JG, Norback DH. Cutaneous malakoplakia: report of a case and review of the literature. Am J Dermatopathol. 1981;3:295–301. [PubMed] [Google Scholar]
- 2.Mehregan DR, Mehregan AH, Mehregan DA. Cutaneous malakoplakia: areport of two cases with the use of anti-BCG for the detection for micro-organisms. J Am Acad Dermatol. 2000;43:351–354. doi: 10.1067/mjd.2000.100538. [DOI] [PubMed] [Google Scholar]
- 3.Michaelis L, Gutman C. Uber Einschlusse in Blasentumoren. ZKlin Med. 1902;47:208–215. [Google Scholar]
- 4.Stanton MJ, Maxted W. Malacoplakia: a study of the literature and currentconcepts of pathogenesis, diagnosis and treatment. J Urol. 1981;125:139–146. doi: 10.1016/s0022-5347(17)54940-x. [DOI] [PubMed] [Google Scholar]
- 5.Biggar WD, Keating A, Brear RA. Malakoplakia: evidence for an acquired disease secondary to immunosuppression. Transplantation. 1981;31:109–112. [PubMed] [Google Scholar]
- 6.Rémond B, Dompmartin A, Moreau A, Esnault P, Thomas A, Mandard JC, et al. Cutaneous malacoplakia. Int J Dermatol. 1994;33:538–542. doi: 10.1111/j.1365-4362.1994.tb02888.x. [DOI] [PubMed] [Google Scholar]
- 7.van der Voort HJ, ten Velden JA, Wassenaar RP, Silberbusch J. Malacoplakia: two case reports and a comparison of treatment modalities based on a literature review. Arch Intern Med. 1996;156:577–583. doi: 10.1001/archinte.156.5.577. [DOI] [PubMed] [Google Scholar]
- 8.Lowitt MH, Kariniemi AL, Niemi KM, Kao GF. Cutaneous malacoplakia: a report of two cases and review of the literature. J Am Acad Dermatol. 1996;34:325–332. doi: 10.1016/s0190-9622(07)80002-8. [DOI] [PubMed] [Google Scholar]
- 9.Biggar WD, Crawford L, Cardella C, Bear RA, Gladman D, Reynolds WJ. Malakoplakia and immunosuppressive therapy: reversal of clinical and leukocyte abnormalities after withdrawal of prednisone and azathioprine. Am J Pathol. 1985;199:5–11. [PMC free article] [PubMed] [Google Scholar]
- 10.Leclerc JC, Bernier L. Malacoplasie cutanee. Union Med Can. 1972;101:471–473. [PubMed] [Google Scholar]
- 11.Abdou NI, NaPombejara C, Sagawa A, Ragland C, Stechschulte DJ, Nilsson U, et al. Malakoplakia: evidence for monocyte lysosomal abnormality correctable by cholinergic agonist in vitro and in vivo. NEJM. 1977;297:1413–1419. doi: 10.1056/NEJM197712292972601. [DOI] [PubMed] [Google Scholar]
- 12.Lou TY, Teplitz C. Malakoplakia: pathogenesis and ultrastructural morphogenesis. A problem of altered macrophage (phagolysosomal) response. Hum Pathol. 1974;5:191–207. doi: 10.1016/s0046-8177(74)80066-3. [DOI] [PubMed] [Google Scholar]
- 13.van Crevel R, Curfs J, van der Ven AJ, Assmann K, Meis JF, van der Meer JW. Functional and morphological monocyte abnormalities in a patient with malakoplakia. Am J Med. 1998;105:74–77. doi: 10.1016/s0002-9343(98)00130-2. [DOI] [PubMed] [Google Scholar]
- 14.Kohl SK, Hans CP. Cutaneous malakoplakia. Arch Pathol Lab Med. 2008;132:113–117. doi: 10.5858/2008-132-113-CM. [DOI] [PubMed] [Google Scholar]
- 15.Flann S, Norton J, Pembroke AC. Cutaneous malakoplakia in an abdominal skin fold. J Am Acad Dermatol. 2010;62:896–897. doi: 10.1016/j.jaad.2008.10.044. [DOI] [PubMed] [Google Scholar]
- 16.Shawaf AZ, Boushi LA, Douri TH. Perianal cutaneous malakoplakia in an immunocompetent patient. Dermatol Online J. 2010;16:10–10. [PubMed] [Google Scholar]
- 17.Patrizi A, Giacomini F, Bianchi F, Misciali C, Neri I. Recurrent calcified cutaneous nodule of the perianal region. Arch Dermatol. 2007;143:1441–1446. doi: 10.1001/archderm.143.11.1441-c. [DOI] [PubMed] [Google Scholar]
- 18.Rémond B, Dompmartin A, De Pontville M, Moreau A, Mandard JC, Leroy D. Cutaneous malacoplakia in heart transplanted patient. Ann Dermatol Venereol. 1993;120:805–808. [PubMed] [Google Scholar]
- 19.Teeters JC, Betts R, Ryan C, Huether J, Elias K, Hartmann D, et al. Rectal and cutaneous malakoplakia in an orthotopic cardiac transplant recipient. J Heart Lung Transplant. 2007;26:411–413. doi: 10.1016/j.healun.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 20.Long JP Jr, Althausen AF. Malacoplakia: a 25-year experience with a review of the literature. J Urol. 1989;141:1328–1331. doi: 10.1016/s0022-5347(17)41297-3. [DOI] [PubMed] [Google Scholar]
- 21.Ben Amna M, Hajri M, Oumaya C, Anis J, Bacha K, Ben Hassine L, et al. Genito-urinary malakoplakia. Report of 10 cases and review of the literature. Ann Urol (Paris) 2002;36:388–391. doi: 10.1016/s0003-4401(02)00137-7. [DOI] [PubMed] [Google Scholar]
- 22.Debie B, Cosyns JP, Feyaerts A, Opsomer RJ, Tombal B, Van Cangh PJ, et al. Malacoplakia in children. Prog Urol. 2005;15:511–513. [PubMed] [Google Scholar]
- 23.Rull R, Grande L, García-Valdecasas JC, Bombi JA, Alós LL, Fuster J, et al. Malakoplakia in the gastrointestinal tract of a liver transplant recipient. Transplantation. 1995;59:1492–1494. doi: 10.1097/00007890-199505270-00026. [DOI] [PubMed] [Google Scholar]
- 24.Minor L, Lindgren BW. Malakoplakia of the bladder in a 16-year-old girl. J Urol. 2003;170:568–569. doi: 10.1097/01.ju.0000071475.79104.98. [DOI] [PubMed] [Google Scholar]
- 25.Yuoh G, Hove MG, Wen J, Haque AK. Pulmonary malakoplakia in acquired immunodeficiency syndrome: an ultrastructural study of morphogenesis of Michaelis-Gutmann bodies. Mod Pathol. 1996;9:476–483. [PubMed] [Google Scholar]
- 26.McClure J. Malakoplakia. J Pathol. 1983;140:275–330. doi: 10.1002/path.1711400402. [DOI] [PubMed] [Google Scholar]
- 27.Vanbrabant P, Drieskens O, Blockmans D. 18-fluoro-deoxyglucose positron emission tomography may contribute to the diagnosis and follow-up of malakoplakia. Acta Clin Belg. 2004;59:138–142. doi: 10.1179/acb.2004.020. [DOI] [PubMed] [Google Scholar]
- 28.Dervan PA, Teeling M, Dempsey J, Drury IM, O'Malley E, O'Connell D. Lymphadenopathy due to fatal histiocytic proliferative disorder containing Michaelis Gutmann bodies. Cancer. 1986;57:1337–1340. doi: 10.1002/1097-0142(19860401)57:7<1337::aid-cncr2820570715>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 29.Sina B, Kauffman L. Pseudomalakoplakia [abstract] J Cutan Pathol. 1998;25(513) [Google Scholar]
- 30.Herrero C, Torras H, Palou J, Mascaro JM. Successful treatment of a patient with cutaneous malacoplakia with clofazimine and trimethoprim-sulfamethoxazole. J Am Acad Dermatol. 1990;23:947–948. doi: 10.1016/s0190-9622(08)80708-6. [DOI] [PubMed] [Google Scholar]
- 31.Von Hansemann D. Uber Malakoplakie der Hernblase. Virchows Arch. 1903;173:302–308. (Ger). [Google Scholar]
- 32.Schaller J, Metz K, Schmidt U, Kunze J. Cutaneous malacoplakia in a patient with psoriasis vulgaris. Hautarzt. 1996;47:763–766. doi: 10.1007/s001050050505. [DOI] [PubMed] [Google Scholar]
- 33.Moore WM, Stokes TL, Cabanas VY. Malakoplakia of the skin: report of a case. Am J Clin Pathol. 1973;60:218–221. doi: 10.1093/ajcp/60.2.218. [DOI] [PubMed] [Google Scholar]
- 34.Rao NR. Malacoplakia of broad ligament, inguinal region, and endometrium. Arch Pathol. 1969;88:85–88. [PubMed] [Google Scholar]
- 35.Addison DJ. Malakoplakia of the eyelid. Ophthalmology. 1986;93:1064–1067. doi: 10.1016/s0161-6420(86)33633-9. [DOI] [PubMed] [Google Scholar]
- 36.Arul KJ, Emmerson RW. Malacoplakia of the skin. Clin Exp Dermatol. 1977;2:131–135. doi: 10.1111/j.1365-2230.1977.tb01556.x. [DOI] [PubMed] [Google Scholar]
- 37.Baez-Giangreco A, Afzal M, Chattopadhyay SK. Malacoplakia: extensive female genital tract and skin involvement. Int J Gynecol Obstet. 1994;45:159–160. doi: 10.1016/0020-7292(94)90124-4. [DOI] [PubMed] [Google Scholar]
- 38.Barnard M, Chalvardjian A. Cutaneous malakoplakia in a patient with acquired immunodeficiency syndrome (AIDS) Am J Dermatopathol. 1998;20:185–188. doi: 10.1097/00000372-199804000-00015. [DOI] [PubMed] [Google Scholar]
- 39.Bodokh I, Lacour JP, Perrin C, Rainero C, Lebreton E, Grosshan E, et al. Malacoplakie cutanee associee a une hepatite chronique due au virus de l'hepatite C. Ann Dermatol Venereol. 1993;120:808–810. (Fre). [PubMed] [Google Scholar]
- 40.Carloz B, Bioulac-Sage P, Domercq B, Royer P, Beylot C. Malacoplasie cutanee: a propos d'un cas. Rev Eur Dermatol Mst. 1991;3:259–263. (Fre). [Google Scholar]
- 41.Chaudhry AP, Satchidanand SK, Anthone R, Baumler RA, Gaeta JF. An unusual case of supraclavicular and colonic malakoplakia-a light and ultrastructural study. J Pathol. 1980;131:193–208. doi: 10.1002/path.1711310302. [DOI] [PubMed] [Google Scholar]
- 42.Colby TV. Malakoplakia: two unusual cases which presented diagnostic problems. Am J Surg Pathol. 1978;2:377–382. [PubMed] [Google Scholar]
- 43.Davis D, Bigler L, Shimazu C, Omura E. Cutaneous malakoplakia. J Cutan Pathol. 1997;24:93–93. [Google Scholar]
- 44.Douglas-Jones AG, Rodd C, James EM, Mills RG. Prediagnostic malakoplakia presenting as a chronic inflammatory mass in the soft tissues of the neck. J Laryngol Otol. 1992;106:173–177. doi: 10.1017/s0022215100119012. [DOI] [PubMed] [Google Scholar]
- 45.Feldmann R, Breier F, Duschet P, Low-Weiser H, Gschnait F. Cutaneous malakoplakia on the forehead. Dermatology. 1997;194:358–360. doi: 10.1159/000246136. [DOI] [PubMed] [Google Scholar]
- 46.Font RL, Bersani TA, Eagle RC Jr. Malakoplakia of the eyelid: clinical, histopathologic, and ultrastructural characteristics. Ophthalmology. 1988;95:61–68. doi: 10.1016/s0161-6420(88)33232-x. [DOI] [PubMed] [Google Scholar]
- 47.Kumar PV, Tabei SZ. Cutaneous malacoplakia diagnosed by scraping cytology. Acta Cytol. 1988;32:125–127. [PubMed] [Google Scholar]
- 48.Neiland ML, Silverman AR, Borochovitz D, Saferstein HL. Cutaneous malakoplakia. Am J Dermatopathol. 1981;3:287–294. [PubMed] [Google Scholar]
- 49.Palazzo JP, Ellison DJ, Garcia IE, Langer C, Scher RM, Hoffman JP, et al. Cutaneous malakoplakia simulating relapsing malignant lymphoma. J Cutan Pathol. 1990;17:171–175. doi: 10.1111/j.1600-0560.1990.tb00077.x. [DOI] [PubMed] [Google Scholar]
- 50.Toubes-Klingler E, Prabhu VC, Bernal K, Poage D, Swindells S. Malacoplakia of the cranium and cerebrum in a human immunodeficiency virus-infected man: case report. J Neurosurg. 2006;104:432–435. doi: 10.3171/jns.2006.104.3.432. [DOI] [PubMed] [Google Scholar]
- 51.Pang LC. Malacoplakia manifesting as a chronic inflammatory mass at the site of a nonhealing surgical wound. Ear Nose Throat J. 2003;82:876–880. [PubMed] [Google Scholar]
- 52.Porrazzi LC, De Gregorio A, Ferraraccio F, Maiello FM, Onufrio A. A case of fistulizated pelvic malacoplakia: cytohistologic, immunohistochemical and electron-microscopic study. Appl Pathol. 1989;7:249–255. [PubMed] [Google Scholar]
- 53.Price HM, Hanrahan JB, Florida RG. Morphogenesis of calcium laden cytoplasmic bodies in malakoplakia of the skin: an electron microscopic study. Hum Pathol. 1973;4:381–394. doi: 10.1016/s0046-8177(73)80100-5. [DOI] [PubMed] [Google Scholar]
- 54.Reiner RJ, Conway GF, Goodman PA. Retroperitoneal malakoplakia. Urology. 1977;X:276–277. [Google Scholar]
- 55.Sarkell B, Dannenberg M, Blaylock WK, Patterson JW. Cutaneous malacoplakia. J Am Acad Dermatol. 1994;30:834–836. doi: 10.1016/s0190-9622(94)70091-5. [DOI] [PubMed] [Google Scholar]
- 56.Scullin DR, Hardy R. Malacoplakia of the urinary tract with spread to the abdominal wall. J Urol. 1972;107:908–910. doi: 10.1016/s0022-5347(17)61169-8. [DOI] [PubMed] [Google Scholar]
- 57.Sencer O, Sencer H, Uluoğlu O, Torunoğlu M, Tatlicioğlu E. Malakoplakia of the skin. Ultrastructure and quantitative x-ray microanalysis of Michaelis-Gutmann bodies. Arch Pathol Lab Med. 1979;103:446–450. [PubMed] [Google Scholar]
- 58.Sian CS, McCabe RE, Lattes CG. Malacoplakia of skin and subcutaneous tissue in a renal transplant recipient. Arch Dermatol. 1981;117:654–655. [PubMed] [Google Scholar]
- 59.Singh M, Kaur S, Vajpayee BK, Banerjee AK. Cutaneous malakoplakia with dermatomyositis. Int J Dermatol. 1987;26:190–191. doi: 10.1111/j.1365-4362.1987.tb00890.x. [DOI] [PubMed] [Google Scholar]
- 60.Wittenberg GP, Douglass MC, Azam M, Lee MW, al-Ujayli B, Lowe L. Cutaneous malacoplakia in a patient with the acquired immunodeficiency syndrome. Arch Dermatol. 1998;134:244–245. doi: 10.1001/archderm.134.2.244. [DOI] [PubMed] [Google Scholar]
- 61.Knausz J, Lipták J, Andrásovszky Z, Baranyay F. Vesico-cutaneous fistula revealing abdominal wall malakoplakia accompanied by Boeck's sarcoidosis. Orv Hetil. 2010;151:220–223. doi: 10.1556/OH.2010.28785. [DOI] [PubMed] [Google Scholar]
- 62.Garg M, Eley KA, Bond SE, Shah KA, Browning L, Watt-Smith SR. Malakoplakia presenting as an enlarging neck mass: Case presentation and review of the literature. Head Neck. 2010;32:1269–1272. doi: 10.1002/hed.21183. [DOI] [PubMed] [Google Scholar]
- 63.Savant SR, Amladi ST, Kangle SD, Wadhwa SL, Nayak CS. Cutaneous malakoplakia in an HIV-positive patient. Int J STD AIDS. 2007;18:435–436. doi: 10.1258/095646207781024801. [DOI] [PubMed] [Google Scholar]
- 64.Sinha SK, Sethy PK, Kaman L, Vaiphei K, Nagi B, Dutta U, et al. Multiple spontaneous enterocutaneous fistulae in malakoplakia. Indian J Gastroenterol. 2003;22:234–235. [PubMed] [Google Scholar]
- 65.Verma SB. Cutaneous malakoplakia: a rare diagnosis of chronic nodules over the buttocks. Int J Dermatol. 2011;50:184–186. doi: 10.1111/j.1365-4632.2010.04709.x. [DOI] [PubMed] [Google Scholar]
- 66.Sormes M, Siemann-Harms U, Brandner JM, Moll I. Cutaneous malakoplakia. J Dtsch Dermatol Ges. 2011;9:914–915. doi: 10.1111/j.1610-0387.2011.07758.x. [DOI] [PubMed] [Google Scholar]