Abstract
Behçet's disease is a chronic inflammatory disease of unknown aetiology, characterized by recurrent oral and genital aphthous ulcerations, uveitis, skin lesions and other multisystem affections associated with vasculitis. Different types of vessels, predominantly veins, can be affected in Behçet's disease. The frequency of vascular lesions in Behçet's disease, such as superficial and deep venous thromboses, arterial aneurysms and occlusions, ranges between 7-29%. Budd-Chiari syndrome is a rare and serious complication of Behçet's disease and implies thrombosis of the hepatic veins and/or the intrahepatic or suprahepatic inferior vena cava. We report a case of a 25-year-old man with Behçet's disease that developed Budd-Chiari syndrome. The correlation of dermatological, pathological and imaging studies confirmed the diagnosis.
Keywords: Behcet disease, Budd-Chiari Syndrome, Thrombosis
Abstract
Doença de Behçet é uma doença inflamatória crônica de etiologia desconhecida, caracterizada clinicamente por ulcerações aftosas orais e genitais recorrentes, uveíte, lesões cutâneas e outras afecções multissistêmicas associadas à vasculite. Diferentes tipos de vasos, predominantemente veias, podem ser afetados na doença de Behçet, causando tromboses venosas superficiais e profundas, aneurismas arteriais e oclusões, com uma frequência em torno de 7 a 29%. Síndrome de Budd-Chiari é uma rara e grave complicação da SB e implica trombose das veias hepáticas e/ou da veia cava inferior intra ou suprahepática. Nós reportamos um caso de paciente masculino com Doença de Behçet que apresentou Síndrome de Budd-Chiari e tromboses múltiplas, cujo diagnóstico foi favorecido pela correlação entre aspectos dermatológicos, histopatológicos, radiológicos e laboratoriais.
INTRODUCTION
Behçet's disease (BD) is an multisystem inflammatory disorder with unknown etiology, characterized by recurrent oral and genital ulcers, uveitis and skin lesions.1 Clinical presentation of this disorder includes articular, central nervous system, gastrointestinal, renal, urogenital, pulmonary and cardiovascular manifestations, all of which are associated with systemic vasculitis, a pivotal pathophysiological feature of BS. Blindness is frequent, resulting from repeated attacks of uveitis. Genetic susceptibility and environmental factors can be associated with this syndrome. International diagnostic criteria were established in 1990.2 Budd-Chiari syndrome (BCS) is a rare and serious complication of BS and implies thrombosis of hepatic veins and/or intrahepatic or suprahepatic inferior vena cava. Severe vascular complications of BCS associated with BS seem to affect mainly young men.3,4
CASE REPORT
A 25 year-old man was hospitalized in a public hospital with the following complaints: ascites, prominent venous collaterals on the abdominal wall, swelling in the legs and cutaneous lesions. Two years earlier, he had developed asymmetric recurrent migratory arthritis, aseptic meningitis, moderate and intermittent fever, recurrent lesions in the oral cavity and unilateral blindness. He denied smoking and alcoholism. Physical examination showed jaundice, acneiform eruptions on the abdomen, oral ulcers, reduced vesicular murmur at right lung base, ascites with varicose veins in the abdomen near the skin surface, an enlarged and tender liver and edema of legs (++/4) (Figures 1 and 2). Laboratory tests detected hypochromic and microcytic anemia; nonreactive viral hepatitis serology, HIV and syphilis infection serology; negative autoantibodies; normal rheumatoid factor and serum complement; low levels of protein C and S, and normal levels of antithrombin III; high hemosedimentation velocity and C reactive protein; serum ascites albumin gradient greater than 1.1; and a negative skin pathergy test. Histopathology of papulopustular lesion showed show perifollicular and perivascular mononuclear and neutrophilic infiltration (Figure 3). Endoscopy showed oesophageal varices. Doppler ultrasound examination and computed tomography showed ascites and absence of flow in the suprahepatic and cava veins (Figures 4 and 5). Doppler ultrasound of lower limbs showed thrombosis. The correlation of dermatological, pathological and imaging studies confirmed the diagnosis of BD in association with BCS. Symptomatic treatment was established with diuretics, oral corticosteroids, azathioprine, colchicine and anticoagulants. After such treatment was begun the patient had significant improvement, but died five months later due to haemorrhage complications.
FIGURE 1.

Ascites, colateral circulation and acneiform lesions on abdomen
FIGURE 2.

Oral aphthous lesions
FIGURE 3.
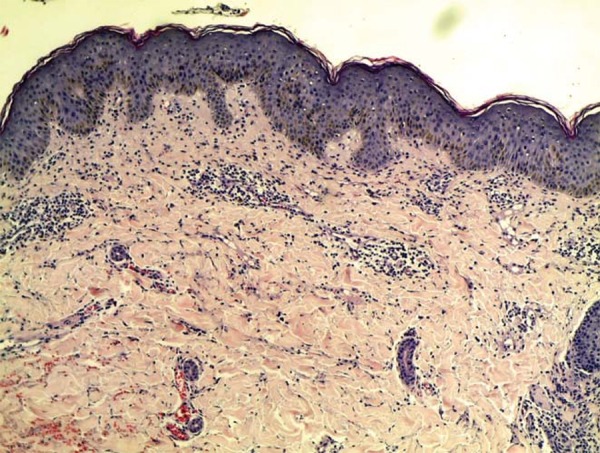
Perivascular and interstitial neutrophilic infiltrate.
FIGURE 4.
Absence of flow into inferior vena cava
FIGURE 5.
Absence of flow into suprahepatic veins
DISCUSSION
BD is named after Hulusi Behçet, a Turkish dermatologist, who described three patients with a triple symptom complex of aphthae, genital ulcers, and hypopyon uveitis in 1937. Oral ulcerations are frequently the first as well as the most frequent symptoms. Minor aphthous ulcers (<10mm in diameter) are the most common type. Aphthae are usually multiple and it is difficult to distinguish them from those of recurrent oral ulcers due to other causes.5 Spontaneous papulopustular, follicular, pseudofollicular, or acneiform lesions are among the elements of the ISG criteria having a sensitivity and specificity of 70% and 76% respectively.2 They are seen as small, usually follicular, pustules, with an erythematous base, and tend to localize in the upper and lower limbs. The pathergy reaction is a nonspecific hyperreactivity of the skin to trauma such as a needle prick. A papule or pustule typically forms in 24-48 hours after a skin puncture with a needle. While the positivity reaches 60-70% of patients in Turkey and Japan, it is rarely observed in BD patients from Northern Europe and North America.6 Extragenital ulcers, Sweet's syndrome, pyoderma gangrenosum, leucocytoclastic vasculitis and true arterial lesions are other less common skin lesions.5
Chronic, relapsing bilateral uveitis involving both anterior and posterior chambers is seen in half of all patients but is more frequent and more severe among the male and the young. Anterior uveitis with intense inflammation (hypopyon) observed in only a small fraction of patients indicates a bad outcome and is generally associated with severe retinal vasculitis. Posterior uveal inflammation with involvement of the retina can cause retinal exudates, haemorrhages, venous thrombosis, papilloedema and macular disease. Recurrent attacks of eye disease result in structural changes leading to loss of vision if left untreated.5
The frequency of vascular involvement in BD (superficial and deep venous thromboses, arterial aneurysms, occlusions) ranges between 7-29%.7 Budd-Chiari syndrome (BCS) caused by occlusion of the major hepatic veins, the adjacent inferior vena cava or both, is a rare and serious complication of BD, with high mortality rate and prevalence of 3,2%.4 Evidence in countries where BS is prevalent suggests that this disease should be included among the diagnostic possibilities in cases of BCS.8 Endothelial dysfunction resulting from vascular inflammation is considered to be an important factor of thrombosis, although the endothelial injury itself cannot completely explain the hypercoagulable state of the disease, because other vasculitis syndromes do not increase the risk of thrombosis.9 Other alterations, such as deficiencies of protein C, protein S and antithrombin III, the presence of antiphospholipid antibodies, factor V Leiden and prothrombin 20210A mutations have been considered. Some studies found an association between these abnormalities and thrombosis in Behçet's disease.10
The hepatic venous outflow obstruction in BS is often associated with other venous thrombosis. We believe that the multiple venous thrombosis and BCS of our patient are due to the concomitant presence of BS and protein C and S deficiency, since both provoke hypercoagulable state. The prognosis may be favorable with medical interventions, including anticoagulation, treatment for vasculitis and the use of diuretics, when required. Some authors treat these patients only with immunosuppressive agents, sugesting monthly pulses of cyclophosphamide combined with 1mg/kg of prednisolone and tapering the prednisolone dose to <10 mg/day after three months. Anticoagulation is contraindicated for these authors, because of the risk of bleeding4. Our patient showed initial response with anticoagulants and azathioprine, but died five months later because of excessive bleeding, confirming this risk. In summary, dermatologists should be aware of skin manifestations and complications of patients with BS.
Footnotes
Study carried out at the Dermatology Service of the Federal University of Pará (Serviço de Dermatologia da Universidade Federal do Pará - UFPA) - Belém (PA), Brazil.
Conflict of interest: None
Financial funding: None
REFERENCES
- 1.Bonamigo RR, Razera F, Olm GS. Neutrophilic dermatoses: part I. An Bras Dermatol. 2011;86:11–25. doi: 10.1590/s0365-05962011000100002. [DOI] [PubMed] [Google Scholar]
- 2.International Study Group for Behçet's Disease Criteria for diagnosis of Behçet's disease. Lancet. 1990;335:1078–1080. [PubMed] [Google Scholar]
- 3.La Regina M, Gasparyan AY, Orlandini F, Prisco D. Behçet's disease as a model of venous thrombosis. Open Cardiovasc Med J. 2010;4:71–77. doi: 10.2174/1874192401004020071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ben Ghorbel I, Ennaifer R, Lamloum M, Khanfir M, Miled M, Houman MH. Budd-Chiari syndrome associated with Behçet's disease. Gastroenterol Clin Biol. 2008;32:316–320. doi: 10.1016/j.gcb.2007.12.022. [DOI] [PubMed] [Google Scholar]
- 5.Seyahi E, Yurdakul S. Behçet's Syndrome and Thrombosis. Mediterr J Hematol Infect Dis. 2011;3:e2011026. doi: 10.4084/MJHID.2011.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yazici H, Chamberlain MA, Tüzün Y, Yurdakul S, Müftüoglu A. A comparative study of the pathergy among Turkish and British patients with Behçet's disease. Ann Rheum Dis. 1984;43:74–75. doi: 10.1136/ard.43.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kuzu MA, Ozaslan C, Köksoy C, Gürler A, Tüzüner A. Vascular involvement in Behçet's disease: 8-year audit. World J Surg. 1994;18:948–953. doi: 10.1007/BF00299119. [DOI] [PubMed] [Google Scholar]
- 8.Uskudar O, Akdogan M, Sasmaz N, Yilmaz S, Tola M, Sahin B. Etiology and portal vein thrombosis in Budd-Chiari syndrome. World J Gastroenterol. 2008;14:2858–2862. doi: 10.3748/wjg.14.2858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lee YJ, Kang SW, Yang JI, Choi YM, Sheen D, Lee EB, et al. Coagulation parameters and plasma total homocysteine levels in Behçet's disease. Thromb Res. 2002;106:19–24. doi: 10.1016/s0049-3848(02)00085-3. [DOI] [PubMed] [Google Scholar]
- 10.Mader R, Ziv M, Adawi M, Mader R, Lavi I. Thrombophilic factors and their relation to thromboembolic and other clinical manifestations in Behçet's disease. J Rheumatol. 1999;26:2404–2408. [PubMed] [Google Scholar]




