Abstract
Besides being the most widely used vaccine directed against tuberculosis (TB) worldwide, Mycobacterium bovis BCG is also the most controversial vaccine in current use. Its protective efficacy varies widely in different parts of the world. One approach to improving the current BCG vaccine might be to produce recombinant BCG strains that express major antigens encoded by genes that are present in the M. tuberculosis-specific region of difference 1 (RD1), such as pe35, cfp10, and esat6. In this study, pe35, cfp10, and esat6 genes were cloned into shuttle plasmid pDE22 to generate the recombinant plasmids PDE22-PE35, PDE22-CFP10, and PDE22-ESAT6, which were electroporated into BCG to generate recombinant BCGs (rBCGs). The cellular immune responses (antigen-induced proliferation and secretion of selected T helper 1 [Th1], Th2, and anti-inflammatory cytokines, i.e., gamma interferon [IFN-γ], interleukin 5 [IL-5], and IL-10, respectively) that are specific to the proteins of cloned genes were studied by using spleen cells from mice immunized with native BCGs and rBCGs and synthetic peptides covering the protein sequence of the cloned genes. The results showed that the spleen cells did not secrete IL-5, whereas IL-10 was secreted in response to peptides of all three proteins from mice immunized with rBCGs only, suggesting expression of the cloned genes and in vivo priming of spleen cells to the expressed proteins. However, in Th1 cell assays that correlate with protective cellular immune responses, i.e., antigen-induced proliferation and IFN-γ secretion, only mice immunized with rBCG-pDE22-PE35 yielded positive responses to the peptides of PE35. These results suggest that rBCG-PDE22-PE35 is the only one of the three vaccines used in this work that is worthy of consideration as a new vaccine candidate against TB.
INTRODUCTION
Tuberculosis (TB) is a major infectious disease problem of global concern. Estimates from the World Health Organization (WHO) suggest that about 9.3 million new cases of TB occur annually (1). Furthermore, tuberculosis is the highest single cause of mortality due to bacterial infections, leading to about 1.7 million deaths worldwide per year (1). Vaccination has long been recognized as an optimal strategy for controlling TB (2). The live attenuated vaccine against TB, Mycobacterium bovis bacillus Calmette-Guérin (BCG), has been given to neonates or young children around the world since the 1950s. It is known to prevent severe manifestations of the disease, such as meningeal and miliary TB. Furthermore, the BCG vaccine has many advantages, including a long-standing safety profile, the need for only a single inoculum, superb adjuvant activity, low cost, easy production, and convenient storage (3, 4). Despite all of these advantages and its wide use, BCG vaccination remains controversial (3). Its protective efficacy varies widely in different parts of the world and its impact on the global problem of tuberculosis remains unclear (3). One approach to improving the current BCG vaccine is to express major Mycobacterium tuberculosis-specific region of difference 1 (RD1) antigens. To identify the individual open reading frames (ORFs) of the RD1-encoding proteins that are potent for Th1-cell reactivity, peptide pools of 12 ORFs present in the RD1 were tested individually with human peripheral blood mononuclear cells (PBMCs). The results showed that PE35, CFP10, and ESAT6 were among the important antigens that stimulated human PBMCs in the protective Th1 cell assays, i.e., antigen-induced proliferation and gamma interferon (IFN-γ) secretion (5, 6). In addition, when tested with PBMCs in a cattle model of TB, PE35, CFP10, and ESAT6 were also found to be moderate-to-major stimulators of Th1 cells that are present in the peripheral blood of M. bovis-infected cattle (7). Moreover, the vaccination of animals, such as guinea pigs and mice, with ESAT6 and CFP10 has been shown to provide protection against challenge with M. tuberculosis (8). According to these indications, the pe35, cfp10, and esat-6 genes were selected in this study to be cloned into shuttle plasmid pDE22 and used to transform BCG in anticipation of improving its immunogenicity relevant to protection against tuberculosis. The shuttle vector pDE22 was developed by O'Gaora et al. in 1997 (9), and it contains a hygromycin-resistant gene marker in addition to a heat shock protein 60 (hsp60) transcription signal and the secretion signal of M. tuberculosis alpha antigen to export the expressed proteins into the extracellular milieu (9).
To study the expression and immunogenicity of the cloned genes in recombinant BCGs (rBCGs), mice were immunized with the live recombinants, and spleen cells were used to study the induction of antigen-specific cellular immune responses, i.e., antigen-induced proliferation and secretion of Th1 (IFN-γ), Th2 (IL-5), and anti-inflammatory (IL-10) cytokines in response to the peptides of proteins expressed by cloned genes.
MATERIALS AND METHODS
Bacterial strains and media.
M. tuberculosis (strain H37Rv) and M. bovis BCG were obtained from the American Type Culture Collection (ATCC), Manassas, VA. Mycobacteria were grown on Middlebrook 7H9 medium (Difco Laboratories, Detroit, MI) supplemented with 0.2% glycerol, 0.05% Tween 80, 10 μg/ml amphotericin B (Fungizone; Gibco), and 10% albumin-dextrose-catalase (ADC) (5% albumin, 2% glucose, 0.004% catalase, and 0.85% sodium chloride) (Gibco-BRL), or on solid Middlebrook 7H11 medium (Difco Laboratories) supplemented with 10% oleic acid-albumin-dextrose-catalase (OADC) (0.05% oleic acid, 5% albumin, 2% d-glucose, 0.85% sodium chloride, and 0.004% catalase) (Gibco-BRL). Plasmids were maintained in rBCG by the addition of 50 μg/ml hygromycin to the growth medium. Escherichia coli strain DH5α was grown in Luria broth (LB) (Difco) medium according to standard procedures and used for the propagation of native and recombinant plasmids.
Mitogen, antigens, and synthetic peptides.
The mitogen concanavalin A (ConA) was purchased from Sigma Chemicals, St. Louis, MO. The complex mycobacterial antigens included BCG sonicates and M. tuberculosis culture filtrate (MT-CF) enriched for secreted antigens. MT-CF was produced under NIH contract no. HHSN266200400091C/ADB, contract no. AI40092, Tuberculosis Vaccine Testing and Research Materials contract, and was kindly provided by J. T. Belisle (Colorado State University, Fort Collins, CO) (10). A total of 18 peptides (25-mer overlapping with neighboring peptides by 10 residues) covering the sequence of PE35, CFP10, and ESAT6 were commercially synthesized by Thermo Electron Corporation, Germany, using fluorenylmethoxycarbonyl chemistry, as described previously (6), and were provided as powders. The powders were dissolved in sterile phosphate-buffered saline (PBS) (pH 7.0) by vigorously vortexing and were frozen at −20°C in aliquots (1 mg/ml) until used. All antigens, mitogens, and peptides were added to a final concentration of 5 μg/ml in cell culture experiments (11).
Cloning of pe35, cfp10, and esat6 genes in the shuttle plasmid pDE22.
The genes of M. tuberculosis RD1 proteins PE35, CFP10, and ESAT6 were amplified by PCR using the genomic DNA of M. tuberculosis H37Rv and gene-specific primers according to standard procedures (12). The amplified DNA was cloned into pGEM-T Easy (Promega Corp., Madison, WI) and subcloned subsequently into the pGES-TH-1 plasmid for expression in E. coli, as described previously (13). After confirming the appropriateness of the inserts in pGES-TH-1, they were excised using the restriction enzymes BamHI and HindIII and subcloned into pDE22 shuttle vector, predigested with the same restriction enzymes, to generate recombinant pDE22-PE35, pDE22-CFP10, and pDE22-ESAT6.
Preparation of recombinant BCG.
Native BCG cells were transformed with the recombinant plasmids by electroporation using the Gene Pulser II electroporation system (Bio-Rad, CA) by using procedures described previously (14). The electroporated BCG cells were plated on Middlebrook 7H11 Bacto agar (Difco) supplemented with 10% OADC and 50 μg/ml hygromycin. After 3 to 4 weeks of incubation at 37°C, the individual colonies of growing cells were picked up from agar plates and inoculated further in the liquid 7H9 medium supplemented with 10% ADC and hygromycin (50 μg/ml), according to standard procedures (14). PCR, using gene-specific primers, was performed to check the presence of pe35, cfp10, and esat6 genes in the rBCGs, as described previously (15, 16).
DNA sequencing.
Forward (F) and reverse (R) oligonucleotide primers to determine the DNA sequence of transcriptional and translational signals around the multiple cloning site (MCS) and the cloned gene in recombinant pDE22 were designed, and they were synthesized commercially by Interactiva Biotechnologies GmbH, Ulm, Germany. The sequences of these primers were as follows: pDE22F, 5′-AGCGTAAGTAGCGGGGTTG-3′ , and pDE22R, 5′-TGGCTTGTCCAAGGGTGTAT-3′ .
DNA plasmids were isolated from rBCG strains and used as a template for PCR, according to standard procedures (17). The amplified DNA plasmids were purified using the High Pure PCR product purification kit (Roche Diagnostics), according to the manufacturer's protocol. The purified DNA plasmids were sequenced using the BigDye Terminator v1.1 cycle sequencing kit (3130xl genetic analyzer; Applied Biosystems) and the sequencer (3130xl genetic analyzer; Applied Biosystems), as described by the manufacturer. The obtained sequences were compared with reference sequences covering transcriptional and translational signals, as well as the cloned genes, using the Clustal W2 website (http://www.ebi.ac.uk/Tools/msa/clustalw2/).
Immunization of mice.
Mice were immunized and handled according to established Institutional Animal Care and Use Committee (IACUC)-approved protocols at Kuwait University, Kuwait. Groups of 6- to 8-week-old female BALB/c mice (5 mice in each group) were immunized intraperitoneally with 5 × 107 CFU of viable native BCG and rBCGs in 100 μl PBS plus 0.05% Tween 80 (PBS-Tween). Four weeks later, all mice immunized with native BCG and two mice from each group immunized with rBCGs were euthanized to collect spleen samples. The remaining three mice from each group immunized with rBCGs were boosted with the same administration route, dose, and rBCGs as in the first immunization. The boosted mice were euthanized 4 weeks later to collect spleen cells. The splenocytes from the euthanized mice were isolated and used in antigen-induced proliferation and secretion of Th1 (IFN-γ), Th2 (IL-5), and anti-inflammatory (IL-10) cytokine assays.
Antigen- and peptide-induced proliferation of mouse splenocytes.
Antigen- and peptide-induced proliferation of mouse splenocytes was performed according to standard procedures (18–20). In brief, spleen cells (2 × 105 cells/well) suspended in 50 μl of complete tissue culture medium were seeded into 96-well tissue culture plates (Nunc, Roskilde, Denmark). The plates were incubated at 37°C in a humidified atmosphere of 5% CO2 and 95% air. The cultures were pulsed for 24 h on day 3 with 1 μCi of [3H]thymidine (Amersham Life Sciences, Little Chalfont, United Kingdom) and harvested on filter mats with a Skatron harvester (Skatron Instruments AS, Oslo, Norway). The radioactivity incorporated was measured by liquid scintillation counting (21, 22) as counts per minute (cpm). Average cpm was calculated from duplicate cultures stimulated with each antigen or peptide. Cellular proliferation results are presented as the stimulation index (SI), which is defined as follows: SI = average cpm in antigen-stimulated cultures/average cpm in cultures without antigen. SI values of ≥2 were considered to be positive proliferative responses against complex mycobacterial antigens and peptides (21–23).
IFN-γ, IL-10, and IL-5 assays.
Supernatants (100 μl) were collected from cultures of mouse splenocytes in 96-well plates before they were pulsed with [3H]thymidine. The supernatants were kept frozen at −70°C until assayed for IFN-γ, IL-10, and IL-5 activity. The amount of cytokines in the supernatants was quantified by enzyme-linked immunosorbent assay (ELISA) using kits purchased from Bender MedSystems, Vienna, Austria, as specified by the manufacturer. The minimum detectable concentrations of IFN-γ, IL-10, and IL-5 by using the kits were 5.3, 5.0, and 3.3 pg/ml, respectively. The secretion of a cytokine in response to a given antigen or peptide was considered positive when the concentration in antigen-stimulated cultures was >100 pg/ml and >2 times the concentration in control cultures without antigen (24).
RESULTS
Construction of recombinant BCG.
The recombinant shuttle vectors pDE22-PE35, pDE22-CFP10, and pDE22-ESAT6 were introduced into BCG by electroporation. Hygromycin-resistant colonies were grown in 7H9 medium containing the selective antibiotic. The growing colonies were confirmed for being recombinant using primers that were specific for each RD1 gene in PCR. The results showed that DNA of an expected size was amplified from each tested colony (Fig. 1).
Fig 1.
Agarose gel electrophoresis of DNA amplified from rBCGs, transformed with pDE22 shuttle vectors, using gene-specific primers. Lane a, 100-bp DNA ladder (marker); lane b, DNA amplified from rBCG-pDE22-PE35 using PE35-specific primers (297-bp product, corresponding to PE35); lane c, DNA amplified from rBCG-pDE22-CFP10 using CFP10-specific primers (300-bp product, corresponding to CFP10); lane d, DNA amplified from rBCG-pDE22-ESAT6 using ESAT6-specific primers (285-bp product, corresponding to ESAT6); lane e, DNA amplified from M. tuberculosis using PE35-specific primers; lane f, DNA amplified from M. tuberculosis using CFP10-specific primers; lane g, DNA amplified from M. tuberculosis using ESAT6-specific primers; lane h, negative control (water).
Sequencing of recombinant plasmids isolated from rBCG.
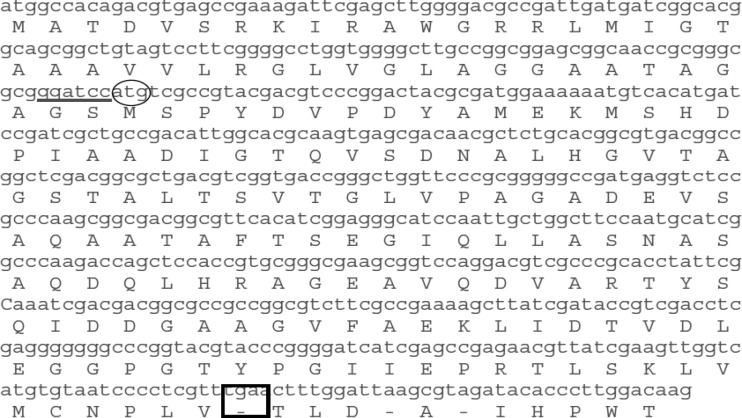
The recombinant plasmids pDE22-PE35, pDE22-CFP10, and pDE22-ESAT6 were isolated from transformed BCG colonies and sequenced to check whether they were subjected to any change when incorporated in their final host. Recombinant plasmid DNA was prepared and amplified using primers flanking the cloning sites of the shuttle vectors. The amplified products included the hsp65 promoter, the alpha antigen secretion signal (alpha-SS), and the DNA insert sequences. The results showed that all of the cloned genes were intact and in frame for expression in pDE22 (Fig. 2, data shown for PDE22-PE35).
Fig 2.
DNA sequence of recombinant plasmid pDE22-PE35, covering alpha-SS and cloned gene. Restriction enzyme (BamHI) sites for gene cloning (underlined), the PE35 ORF start codon (circled), and the stop codon (boxed) are marked. Plasmid DNA was isolated and sequenced by the 3130xl genetic analyzer (Applied Biosystems), as described by the manufacturer. The obtained sequences were compared with reference sequences covering transcriptional and translational signals, as well as the cloned gene, using the ClustalW2 website.
Antigen-induced proliferation of splenocytes isolated from immunized mice.
The spleen cells from all groups of mice showed positive proliferation (SI ≥ 2) in response to ConA, BCG sonicate, and MT-CF (Tables 1, 2, and 3). Furthermore, all of the mice immunized once with native BCGs and rBCGs had negative proliferation responses (SI < 2) to peptide pools of PE35, CFP10, and ESAT6 and their individual peptides (Tables 1, 2, and 3, respectively). Moreover, spleen cells from mice immunized and boosted with recombinant BCG-pDE22-PE35 showed positive responses to the pool of PE35 peptides and the individual peptides P1 and P3 (Table 1).
Table 1.
Antigen/mitogen-induced proliferation of spleen cells from mice immunized with native BCG and recombinant BCG-pDE22-PE35
| Spleen cell stimulanta | No. of mice positive/no. tested, by immunization typeb |
||
|---|---|---|---|
| Native BCG | rBCG-pDE22-ORF3 | rBCG-pDE22-ORF3 (boosted) | |
| ConA | 5/5 | 2/2 | 3/3 |
| BCG sonicate | 5/5 | 2/2 | 3/3 |
| MT-CF | 5/5 | 2/2 | 3/3 |
| PE35 peptide pool | 0/5 | 0/2 | 2/3 |
| P1 | 0/5 | 0/2 | 2/3 |
| P2 | 0/5 | 0/2 | 0/3 |
| P3 | 0/5 | 0/2 | 2/3 |
| P4 | 0/5 | 0/2 | 0/3 |
| P5 | 0/5 | 0/2 | 0/3 |
| P6 | 0/5 | 0/2 | 0/3 |
ConA, concanavalin A; MT-CF, M. tuberculosis culture filtrate.
The proliferation response was considered positive with a stimulation index (SI) of ≥2.
Table 2.
Antigen/mitogen-induced proliferation of spleen cells from mice immunized with native BCG and recombinant BCG-pDE22-CFP10
| Spleen cell stimulanta | No. of mice positive/no. tested, by immunization typeb |
||
|---|---|---|---|
| Native BCG | rBCG-pDE22-CFP10 | rBCG-pDE22-CFP10 (boosted) | |
| ConA | 5/5 | 2/2 | 3/3 |
| BCG sonicate | 5/5 | 2/2 | 3/3 |
| MT-CF | 5/5 | 2/2 | 3/3 |
| CFP10 peptide pool | 0/5 | 0/2 | 1/3 |
| P1 | 0/5 | 0/2 | 1/3 |
| P2 | 0/5 | 0/2 | 1/3 |
| P3 | 0/5 | 0/2 | 0/3 |
| P4 | 0/5 | 0/2 | 1/3 |
| P5 | 0/5 | 0/2 | 2/3 |
| P6 | 0/5 | 0/2 | 1/3 |
ConA, concanavalin A; MT-CF, M. tuberculosis culture filtrate.
The proliferation response was considered positive with a stimulation index (SI) of ≥2.
Table 3.
Antigen/mitogen-induced proliferation of spleen cells from mice immunized with native BCG and recombinant BCG-pDE22-ESAT6
| Spleen cell stimulanta | No. of mice positive/no. tested, by immunization typeb |
||
|---|---|---|---|
| Native BCG | rBCG-pDE22-ESAT6 | rBCG-pDE22-ESAT6 (boosted) | |
| ConA | 5/5 | 2/2 | 3/3 |
| BCG sonicate | 5/5 | 2/2 | 3/3 |
| MT-CF | 5/5 | 2/2 | 3/3 |
| ESAT6 peptide pool | 0/5 | 0/2 | 0/3 |
| P1 | 0/5 | 0/2 | 0/3 |
| P2 | 0/5 | 0/2 | 0/3 |
| P3 | 0/5 | 0/2 | 0/3 |
| P4 | 0/5 | 0/2 | 0/3 |
| P5 | 0/5 | 0/2 | 0/3 |
| P6 | 0/5 | 0/2 | 0/3 |
ConA, concanavalin A; MT-CF, M. tuberculosis culture filtrate.
The proliferation response was considered positive with a stimulation index (SI) of ≥2.
Spleen cells from mice that were immunized and boosted with rBCG-pDE22-CFP10 showed positive proliferation (SI > 2) in response to the pool of CFP10 peptides and the individual peptides P1, P2, P4, P5, and P6 (Table 2). Furthermore, the splenocytes of mice immunized and boosted with rBCG-pDE22-ESAT6 did not show antigen-induced proliferation in response to the pool of peptides and the individual peptides of ESAT6 (Table 3). The positive proliferation responses in most of the positive animals were weak (SI = 2 to 4).
Antigen-induced secretion of cytokines by splenocytes of immunized mice.
IL-5 secretion was detected only in culture supernatants of splenocytes from all groups of mice in response to ConA but to none of the antigens (data not shown). The cytokines IL-10 and IFN-γ were secreted by splenocytes from all groups of animals in response to BCG sonicate, MT-CF (Fig. 3A and B, respectively), and ConA (data not shown). Furthermore, IL-10 was secreted by splenocytes from mice that were immunized and boosted with rBCG-pDE22-PE35, rBCG-pDE22-CFP10, and rBCG-pDE22-ESAT6 in response to the pool of peptides of PE35, CFP10, and ESAT6, respectively (Fig. 3A). However, splenocytes from mice immunized and boosted with rBCG-pDE22-PE35 secreted only IFN-γ in response to the PE35 peptide pool (Fig. 3B) and the individual peptides P1, P3, P4, and P5 (Fig. 4).
Fig 3.
Antigen-induced secretion of cytokines from spleen cells obtained from nonimmunized mice and mice immunized and boosted with rBCG-pDE22-PE35 stimulated with the PE35 peptide pool, rBCG-pDE22-CFP10 stimulated with the CFP10 peptide pool, and rBCG-pDE22-ESAT6 stimulated with the ESAT6 peptide pool for IL-10 (A) and for IFN-γ (B). BCG son., BCG sonicate; MT-CF, M. tuberculosis culture filtrate. Supernatants from antigen-stimulated and nonstimulated cultures of splenocytes from various groups of immunized mice were collected and assayed for Th1 (IFN-γ), Th2 (IL-5), and anti-inflammatory (IL-10) cytokines by ELISA. Concentrations in antigen-stimulated cultures were considered positive when there was >100 pg/ml and >2 times the concentration in cultures with no antigen, indicated by a solid line. Error bars represent the standard errors of the mean.
Fig 4.
Antigen-induced secretion of IFN-γ from spleen cells obtained from mice immunized and boosted with rBCG-pDE22-PE35 and stimulated with single peptides of PE35 (P1 to P6) (n = 2). Supernatants from antigen-stimulated and nonstimulated cultures of splenocytes from immunized mice were collected and assayed for IFN-γ by ELISA. Concentrations in antigen-stimulated cultures were considered positive when there was >100 pg/ml and >2 times the concentration in cultures with no antigen (indicated by a solid line). Error bars represent the standard errors of the mean.
DISCUSSION
The focus of this study was to improve BCG by complementation with genes of the RD1 locus, which encode major antigenic proteins of M. tuberculosis. Among the regions deleted during the attenuation of M. bovis to BCG by Calmette and Guérin, the RD1 locus is considered the first deletion and therefore is important for the loss of protective immunity (25). This argument is supported by a previous study, which showed that restoration of the RD1 locus improved the protective efficacy of BCG in animal models of tuberculosis (26). However, the RD1 locus as a whole is also suggested to have a role in the pathogenesis of M. tuberculosis, and the BCG strains complemented with RD1 have shown increased persistence in mice and guinea pigs (27). The RD1 locus contains 9.5 kb DNA and is predicted to encode a total of 14 M. tuberculosis-specific proteins (28). To avoid pathogenicity while retaining the immunogenicity of the RD1, it has been argued that BCG should be complemented with genes encoding individual antigenic proteins of the RD1 (26). In previous studies, using overlapping synthetic peptides corresponding to putative proteins encoded by genes predicted in the RD1 locus, PE35, CFP10, and ESAT6 were identified as stimulating protective Th1 cells from mice, cattle, and humans (6, 29, 30). Therefore, in this study, to improve BCG, we complemented BCG with the pe35, cfp10, and esat6 genes of the RD1. All of these genes, which code for secreted proteins in native M. tuberculosis, were cloned into the pDE22 shuttle vector, and BCG cells were transformed with recombinant pDE22 shuttle vector in an attempt to direct the expression of these proteins to the extracellular milieu. The presence of each gene in the rBCGs was confirmed by PCR using gene-specific primers (Fig. 1).
To confirm that cloned inserts were in frame for expression in BCG, the DNA of recombinant plasmids pDE22-PE35, pDE22-CFP10, and pDE22-ESAT6 was isolated from BCG cultures and processed for DNA sequence analyses of the appropriate regions of each plasmid. The results show that all sequences of the cloned genes were complete and in frame for expression in pDE22 (Fig. 2) and thus suitable for further experiments to determine in vivo expression and immunogenicity. The recombinant constructs (rBCG-pDE22-PE35, rBCG-pDE22-CFP10, and rBCG-pDE22-ESAT6) were evaluated for in vivo expression of ORF proteins by immunizing BALB/c mice and performing cellular responses (antigen-induced proliferation and cytokine assays) using splenocytes from immunized mice. The results show that splenocytes from all groups of mice proliferated and produced cytokines in response to the mitogen ConA and various complex antigens, i.e., sonicates of BCG and the culture filtrate of M. tuberculosis. These results suggest that the procedures used to assess antigen-induced proliferation of splenocytes were working. Therefore, the same procedures were used to determine the proliferation of splenocytes in response to overlapping synthetic peptides of the RD1 ORFs.
Ideally, full-length proteins of the RD1 ORFs should have been used in the cellular assays. However, obtaining full-length purified RD1 proteins that are free of contaminants, either from cultures of M. tuberculosis or using recombinant expression and purification technologies, is technically demanding and quite cumbersome (31–33). Therefore, to overcome the problems associated with obtaining full-length proteins, pools of synthetic peptides corresponding to each RD1 ORF were used in this study. One of the obvious advantages of this approach is the speed with which peptides can be synthesized and standardized to be tested for stimulating cellular reactivity. Furthermore, immunodominant single peptides can be identified and exact T-cell epitopes defined by subsequent testing of the individual peptides of each ORF, as reported previously (23, 34–36). Each synthetic peptide was 25 amino acids (aa) in length and overlapped with the neighboring peptides by 10 residues. The reason for the 10-residue overlap was to greatly reduce the probability of missing T-cell epitopes, which are usually ≤10 aa in length (37).
In general, immune responses and cytokine secretion levels were lower in mice that were immunized only once with native and recombinant BCG constructs compared to those immunized and boosted with similar constructs. Furthermore, splenocytes from mice that were immunized and boosted with the homologous rBCGs failed to secrete detectable concentrations of Th2 cytokine IL-5, but they could induce secretion of detectable levels of the anti-inflammatory cytokine IL-10, which was secreted in response to the peptide pools of PE35, CFP10, and ESAT6, from splenocytes immunized with the corresponding rBCG. These results confirm those of a previous study by Hanif et al. (18) using DNA vaccine constructs of RD1 ORFs (PE35, CFP10, and ESAT6), which showed that IL-5 was not secreted by the splenocytes of immunized mice in response to peptides of the immunizing ORFs, but that study also failed to detect secretion of IL-10. However, the discrepancy between this study and the study of Hanif et al. for IL-10 results might be due to differences in the vehicles used, i.e., live BCG versus DNA.
The results of Th1-cell assays, i.e., antigen-induced proliferation and IFN-γ secretion, with the splenocytes of mice that were immunized and boosted with homologous rBCGs show that splenocytes proliferated in response to the peptide pools of PE35 and CFP10, but IFN-γ was secreted in response to PE35 only. These results suggest that PE35 is a stronger inducer of Th1 cells when delivered in the context of BCG. In line with these results, the RD1 PE35 has also been reported to induce the strongest IFN-γ responses in mice immunized with the DNA vaccine constructs of PE35, CFP10, and ESAT6 (18).
Both antigen-induced proliferation and IFN-γ secretion have been correlated with protective immunity against tuberculosis. In particular, Th1 immune responses mediated by IFN-γ are a prerequisite for mounting efficient protection against M. tuberculosis challenge in mice (38). Humans with mutated IFN-γ receptor genes are highly susceptible to infection by atypical mycobacteria (39), and mice with a disrupted IFN-γ gene neither produce reactive nitrogen intermediates nor restrict the growth of tubercle bacilli, although they do develop granulomas (40). Furthermore, the models, in which the host is unable to produce any IFN-γ necessary for the generation of antimicrobial activity, demonstrate that IFN-γ is essential for the containment of mycobacterial infection (41). Since rBCG-PDE22-PE35 induces both antigen-induced proliferation and IFN-γ secretion, it may be a better vaccine candidate against tuberculosis than are the other two rBCGs.
In addition to strong Th1 cell reactivity, a candidate vaccine against tuberculosis should be able to induce Th1 cell responses against multiple and HLA-promiscuous epitopes of the immunizing antigen (42). This requirement is essential to overcome the limitations imposed by the highly polymorphic nature of HLA class II molecules in human populations, which are required for the presentation of antigenic epitopes by antigen-presenting cells to Th1 cells (37). The results in this study, by testing the individual peptides of PE35 using splenocytes from mice that were immunized and boosted with rBCG-PDE22-PE35, demonstrate that five of the six peptides of PE35, except peptide 6, induced antigen-induced proliferation and/or IFN-γ secretion. Thus, multiple Th1 cell epitopes scattered throughout the sequence of this protein are present. Furthermore, the analysis of the PE35 sequence for peptide sequences that are capable of binding to HLA class II molecules, using a computer-based prediction program (ProPred) (43), suggests that the RD1 PE35 has multiple and HLA-promiscuous T-cell epitopes (Table 4). These observations support the notion that rBCG-PDE22-PE35 deserves to be considered a new candidate vaccine against tuberculosis.
Table 4.
HLA-DR binding prediction by ProPred analysis for the sequences of complete protein and synthetic peptides (P1 to P6) of RD1 PE35
| Peptide sequence (aa) | No. of alleles predicted to bind/no. of alleles included in ProPred for HLA-DRB allele: |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1.1 | 1.3 | 1.4 | 1.7 | 1.8 | 1.11 | 1.13 | 1.15 | 5.1 | All alleles | |
| PE35 (1–99) | 2/2 | 6/7 | 9/9 | 0/2 | 3/6 | 9/9 | 10/11 | 2/3 | 2/2 | 43/51 |
| P1 (1–25) | 0/2 | 0/7 | 0/9 | 0/2 | 0/6 | 0/9 | 0/11 | 0/3 | 0/2 | 0/51 |
| P2 (16–40) | 0/2 | 0/7 | 0/9 | 0/2 | 0/6 | 0/9 | 0/11 | 0/3 | 0/2 | 0/51 |
| P3 (31–55) | 1/2 | 0/7 | 0/9 | 0/2 | 0/6 | 0/9 | 1/11 | 0/3 | 0/2 | 2/51 |
| P4 (46–70) | 2/2 | 6/7 | 9/9 | 0/2 | 3/6 | 9/9 | 10/11 | 2/3 | 2/2 | 43/51 |
| P5 (61–85) | 0/2 | 0/7 | 0/9 | 0/2 | 0/6 | 1/9 | 0/11 | 0/3 | 0/2 | 1/51 |
| P6 (76–99) | 0/2 | 0/7 | 0/9 | 0/2 | 0/6 | 0/9 | 0/11 | 0/3 | 0/2 | 0/51 |
The overall results of this study suggest the potential of rBCG-PE35 as a candidate vaccine against TB. This should be confirmed by demonstrating the protective ability of rBCG-PE35 in challenge experiments with live M. tuberculosis in animal models of TB. However, supportive evidence is available by using other rBCGs that overexpress cross-reactive antigens (antigens common to M. tuberculosis and BCG), i.e., the antigen 85 (Ag85) complex and 38-kDa antigen (44, 45), which show stronger protective efficacy than native BCG in experimental animal models of tuberculosis. Among these, rBCG-30 (rBCG overexpressing Ag85B) has been tested in phase I clinical trials in humans to establish its safety (46). rBCG will retain the attributes of BCG as a vaccine, including a long-standing safety profile, the need for only a single inoculum, superb adjuvant activity, low expense, easy production, and convenient storage. Hence, in spite of the controversies surrounding its use, BCG cannot easily be replaced by another vaccine candidate. Therefore, the improvements to BCG in the form of rBCG expressing M. tuberculosis-specific antigens remain among the best choices for the rational design of a vaccine for tuberculosis, and the results reported in this work suggest that rBCG-PE35 may be one of them.
ACKNOWLEDGMENTS
This work was supported by Kuwait University research grant no. YM04/18 and GM01/01.
We thank Fatma Shaban for technical support.
Footnotes
Published ahead of print 12 June 2013
REFERENCES
- 1. World Health Organization 2010. Global tuberculosis control. WHO report WHO/HTM/2010.7. World Health Organization, Geneva, Switzerland: [Google Scholar]
- 2. Young D, Dye C. 2006. The development and impact of tuberculosis vaccines. Cell 4: 683– 687 [DOI] [PubMed] [Google Scholar]
- 3. Haile M, Källenius G. 2005. Recent developments in tuberculosis vaccines. Curr. Opin. Infect. Dis. 18: 211– 215 [DOI] [PubMed] [Google Scholar]
- 4. Wang LM, Shi CH, Fan XL, Xue Y, Bai YL, Xu ZK. 2007. Expression and immunogenicity of recombinant Mycobacterium bovis bacillus Calmette-Guérin strains secreting the antigen ESAT-6 from Mycobacterium tuberculosis in mice. Chin. Med. J. (Engl.) 120: 1220– 1225 [PubMed] [Google Scholar]
- 5. Mustafa AS, Al-Attiyah R. 2009. Identification of Mycobacterium tuberculosis-specific genomic regions encoding antigens induced protective cellular immune responses. Indian J. Exp. Biol. 47: 498– 504 [PubMed] [Google Scholar]
- 6. Mustafa AS, Al-Attiyah R, Hanif SN, Shaban FA. 2008. Efficient testing of large pools of Mycobacterium tuberculosis RD1 peptides and identification of major antigens and immunodominant peptides recognized by human Th1 cells. Clin. Vaccine Immunol. 15: 916– 924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mustafa AS, Cockle PJ, Shaban F, Hewinson RG, Vordermeier HM. 2002. Immunogenicity of Mycobacterium tuberculosis RD1 region gene products in infected cattle. Clin. Exp. Immunol. 130: 37– 42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zhang H, Shi CH, Xue Y, Bai YL, Wang LM, Xu ZK. 2006. Immune response and protective efficacy induced by fusion protein ESAT6-CFP10 of M. tuberculosis in mice. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi 22: 443– 446 (In Chinese.) [PubMed] [Google Scholar]
- 9. O'Gaora P, Barnini S, Hayward C, Filley E, Rook G, Young D, Thole J. 1997. Mycobacteria as immunogens: development of expression vectors for use in multiple mycobacterial species. Med. Princ. Pract. 6: 91– 96 [Google Scholar]
- 10. Al-Attiyah R, Mustafa AS. 2008. Characterization of human cellular immune responses to novel Mycobacterium tuberculosis antigens encoded by genomic regions absent in Mycobacterium bovis BCG. Infect. Immun. 76: 4190– 4198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Andersen P, Askgaard D, Gottschau A, Bennedsen J, Nagai S, Heron I. 1992. Identification of immunodominant antigens during infection with Mycobacterium tuberculosis. Scand. J. Immunol. 36: 823– 831 [DOI] [PubMed] [Google Scholar]
- 12. Ahmad S, Ali MM, Mustafa AS. 2003. Construction of a modified vector for efficient purification of recombinant Mycobacterium tuberculosis proteins expressed in Escherichia coli. Protein Expr. Purif. 29: 167– 175 [DOI] [PubMed] [Google Scholar]
- 13. Ahmad S, El-Shazly S, Mustafa AS, Al-Attiyah R. 2004. Mammalian cell-entry proteins encoded by the mce3 operon of Mycobacterium tuberculosis are expressed during natural infection in humans. Scand. J. Immunol. 60: 382– 391 [DOI] [PubMed] [Google Scholar]
- 14. Parish T, Stoker NG. (ed). 1998. Mycobacteria protocols. Humana Press, Totowa, NJ [Google Scholar]
- 15. Hanif SN, Al-Attiyah R, Mustafa AS. 2010. Molecular cloning, expression, purification and immunological characterization of three low-molecular weight proteins encoded by genes in genomic regions of difference of Mycobacterium tuberculosis. Scand. J. Immunol. 71: 353– 361 [DOI] [PubMed] [Google Scholar]
- 16. Hanif SN, Al-Attiyah R, Mustafa AS. 2010. DNA vaccine constructs expressing Mycobacterium tuberculosis-specific genes induce immune responses. Scand. J. Immunol. 72: 408– 415 [DOI] [PubMed] [Google Scholar]
- 17. Mustafa AS, Das Chugh T, Abal AT. 1999. Polymerase chain reaction targeting of single- and multiple-copy genes of mycobacteria in the diagnosis of tuberculosis. Nutrition 11(Suppl 5): 665–669 [PubMed] [Google Scholar]
- 18. Hanif SN, Al-Attiyah R, Mustafa AS. 2011. Cellular immune responses in mice induced by M. tuberculosis PE35-DNA vaccine construct. Scand. J. Immunol. 74: 554– 560 [DOI] [PubMed] [Google Scholar]
- 19. Mustafa AS, Deggerdal A, Lundin KE, Meloen RM, Shinnick TM, Oftung F. 1994. An HLA-DRw53-restricted T-cell epitope from a novel Mycobacterium leprae protein antigen important to the human memory T-cell repertoire against M. leprae. Infect. Immun. 62: 5595– 5602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Oftung F, Geluk A, Lundin KE, Meloen RH, Thole JE, Mustafa AS, Ottenhoff TH. 1994. Mapping of multiple HLA class II-restricted T-cell epitopes of the mycobacterial 70-kilodalton heat shock protein. Infect. Immun. 62: 5411– 5418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Al-Attiyah R, Mustafa AS, Abal AT, El-Shamy AS, Dalemans W, Skeiky YA. 2004. In vitro cellular immune responses to complex and newly defined recombinant antigens of Mycobacterium tuberculosis. Clin. Exp. Immunol. 138: 139– 144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mustafa AS, Abal AT, Shaban F, El-Shamy AM, Amoudy HA. 2005. HLA-DR binding prediction and experimental evaluation of T-cell epitopes of mycolyl transferase 85B (Ag85B), a major secreted antigen of Mycobacterium tuberculosis. Med. Princ. Pract. 14: 140– 146 [DOI] [PubMed] [Google Scholar]
- 23. Mustafa AS, Shaban FA, Abal AT, Al-Attiyah R, Wiker HG, Lundin KE, Oftung F, Huygen K. 2000. Identification and HLA restriction of naturally derived Th1-cell epitopes from the secreted Mycobacterium tuberculosis antigen 85B recognized by antigen-specific human CD4+ T-cell lines. Infect. Immun. 68: 3933– 3940 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Al-Attiyah R, Mustafa AS. 2010. Characterization of human cellular immune responses to Mycobacterium tuberculosis proteins encoded by genes predicted in RD15 genomic region that is absent in Mycobacterium bovis BCG. FEMS Immunol. Med. Microbiol. 59: 177– 187 [DOI] [PubMed] [Google Scholar]
- 25. Behr MA, Wilson MA, Gill WP, Salamon H, Schoolnik GK, Rane S, Small PM. 1999. Comparative genomics of BCG vaccines by whole-genome DNA microarray. Science 284: 1520– 1523 [DOI] [PubMed] [Google Scholar]
- 26. Pym AS, Brodin P, Majlessi L, Brosch R, Demangel C, Williams A, Griffiths KE, Marchal G, Leclerc C, Cole ST. 2003. Recombinant BCG exporting ESAT-6 confers enhanced protection against tuberculosis. Nat. Med. 9: 533– 539 [DOI] [PubMed] [Google Scholar]
- 27. Pym AS, Brodin P, Brosch R, Huerre M, Cole ST. 2002. Loss of RD1 contributed to the attenuation of the live tuberculosis vaccines Mycobacterium bovis BCG and Mycobacterium microti. Mol. Microbiol. 46: 709– 717 [DOI] [PubMed] [Google Scholar]
- 28. Amoudy HA, Al-Turab MB, Mustafa AS. 2006. Identification of transcriptionally active open reading frames within the RD1 genomic segment of Mycobacterium tuberculosis. Med. Princ. Pract. 15: 137– 144 [DOI] [PubMed] [Google Scholar]
- 29. Hanif SN, Al-Attiyah R, Mustafa AS. 2010. Species-specific antigenic Mycobacterium tuberculosis proteins tested by delayed-type hypersensitivity response. Int. J. Tuberc. Lung Dis. 14: 489– 494 [PubMed] [Google Scholar]
- 30. Mustafa AS. 2002. Development of new vaccines and diagnostic reagents against tuberculosis. Mol. Immunol. 39: 113– 119 [DOI] [PubMed] [Google Scholar]
- 31. Ahmad S, Amoudy HA, Thole JE, Young DB, Mustafa AS. 1999. Identification of a novel protein antigen encoded by a Mycobacterium tuberculosis-specific RD1 region gene. Scand. J. Immunol. 49: 515– 522 [DOI] [PubMed] [Google Scholar]
- 32. Amoudy HA, Ahmad S, Thole JE, Mustafa AS. 2007. Demonstration of in vivo expression of a hypothetical open reading frame (ORF-14) encoded by the RD1 region of Mycobacterium tuberculosis. Scand. J. Immunol. 66: 422– 425 [DOI] [PubMed] [Google Scholar]
- 33. Daugelat S, Kowall J, Mattow J, Bumann D, Winter R, Hurwits R, Kaufmann SH. 2003. The RD1 proteins of Mycobacterium tuberculosis: expression in Mycobacterium smegmatis and biochemical characterization. Microbes Infect. 5: 1082– 1095 [DOI] [PubMed] [Google Scholar]
- 34. Al-Attiyah R, Shaban FA, Wiker HG, Oftung F, Mustafa AS. 2003. Synthetic peptides identify promiscuous human Th1 cell epitopes of the secreted mycobacterial antigen MPB70. Infect. Immun. 71: 1953– 1960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mustafa AS, Shaban FA. 2006. ProPred analysis and experimental evaluation of promiscuous T-cell epitopes of three major secreted antigens of Mycobacterium tuberculosis. Tuberculosis (Edinb.) 86: 115– 124 [DOI] [PubMed] [Google Scholar]
- 36. Mustafa AS, Shaban FA, Al-Attiyah R, Abal AT, El-Shamy AM, Andersen P, Oftung F. 2003. Human Th1 cell lines recognize the Mycobacterium tuberculosis ESAT-6 antigen and its peptides in association with frequently expressed HLA class II molecules. Scand. J. Immunol. 57: 125– 134 [DOI] [PubMed] [Google Scholar]
- 37. Mustafa AS. 2000. HLA-restricted immune response to mycobacterial antigens: relevance to vaccine design. Hum. Immunol. 61: 166– 171 [DOI] [PubMed] [Google Scholar]
- 38. Tascon RE, Stavropoulos E, Lukacs KV, Colston MJ. 1998. Protection against Mycobacterium tuberculosis infection by CD8+ T cells requires the production of gamma interferon. Infect. Immun. 66: 830– 834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Newport MJ, Huxley CM, Huston S, Hawrylowicz CM, Oostra BA, Williamson R, Levin M. 1996. A mutation in the interferon-gamma-receptor gene and susceptibility to mycobacterial infection. N. Engl. J. Med. 335: 1941– 1949 [DOI] [PubMed] [Google Scholar]
- 40. Flynn JL, Chan J, Triebold KJ, Dalton DK, Stewart TA, Bloom BR. 1993. An essential role for interferon gamma in resistance to Mycobacterium tuberculosis infection. J. Exp. Med. 178: 2249– 2254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Boussiotis VA, Tsai EY, Yunis EJ, Thim S, Delgado JC, Dascher CC, Berezovskaya A, Rousset D, Reynes J, Goldfeld AE. 2000. IL-10-producing T cells suppress immune responses in anergic tuberculosis patients. J. Clin. Invest. 105: 1317– 1325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mustafa AS. 2010. Cell mediated immunity assays identify proteins of diagnosis and vaccine potential from genomic regions of difference of Mycobacterium tuberculosis. Kuwait Med. J. 42: 98– 105 [Google Scholar]
- 43. Singh H, Raghava GP. 2001. ProPred: prediction of HLA-DR binding sites. Bioinformatics 17: 1236– 1237 [DOI] [PubMed] [Google Scholar]
- 44. Castañon-Arreola M, López-Vidal Y, Espitia-Pinzón C, Hernández-Pando R. 2005. A new vaccine against tuberculosis shows greater protection in a mouse model with progressive pulmonary tuberculosis. Tuberculosis (Edinb.) 85: 115– 126 [DOI] [PubMed] [Google Scholar]
- 45. Horwitz MA, Harth G, Dillon BJ, Maslesa-Galic S. 2000. Recombinant bacillus Calmette-Guérin (BCG) vaccines expressing the Mycobacterium tuberculosis 30-kDa major secretory protein induce greater protective immunity against tuberculosis than conventional BCG vaccines in a highly susceptible animal model. Proc. Natl. Acad. Sci. U. S. A. 97: 13853– 13858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hoft DF, Blazevic A, Abate G, Hanekom WE, Kaplan G, Soler JH, Weichold F, Geiter L, Sadoff JC, Horwitz MA. 2008. A new recombinant bacille Calmette-Guérin vaccine safely induces significantly enhanced tuberculosis-specific immunity in human volunteers. J. Infect. Dis. 198: 1491– 1501 [DOI] [PMC free article] [PubMed] [Google Scholar]