Abstract
We compared carbapenemase detection among 271 Gram-negative bacilli (of which 131 were carbapenemase producers) using a novel chromogenic rapid test—the Carba NP test (CNP)—and the modified Hodge test (MHT). Sensitivities were comparable (CNP, 100%, versus MHT, 98%; P = 0.08), but CNP was more specific (100% versus 80%; P < 0.0001) and faster.
TEXT
Gram-negative bacilli (GNB) with acquired carbapenemases have disseminated worldwide, rendering them a global threat. The therapeutic armamentarium for infections caused by carbapenem-resistant Enterobacteriaceae (CRE) is limited, and CRE infections have been associated with significant mortality (1). Enterobacteriaceae harboring Klebsiella pneumoniae carbapenemase (KPC) are now endemic in some regions of the United States (2, 3), and although still sporadic, GNB harboring New Delhi metallo-β-lactamase (NDM) have been reported for nine states (4). Timely detection of these plasmid-borne and easily transmissible carbapenemases (along with emerging carbapenemases like OXA-48 and VIM) is important given implications for appropriate therapy and infection control. Detection is challenging, since isolates may have only borderline reductions in susceptibility to carbapenems (5), and resistance may be mediated by mechanisms other than carbapenemase production (e.g., AmpC or extended-spectrum β-lactamase [ESBL] with decreased membrane permeability). While molecular methods are confirmatory, testing may not be immediately available and may be limited by the number of targets assayed. The modified Hodge test (MHT), a CLSI-recommended confirmatory test for carbapenemase production, suffers from lack of specificity, a long turnaround time, and poor sensitivity for metallo-β-lactamase detection (6, 7). A rapid phenotypic test to screen for carbapenemases is highly desirable. Recently, Nordmann et al. described a rapid chromogenic carbapenemase detection assay based on hydrolysis of the β-lactam ring of imipenem, the Carba NP test (CNP) (8–10). Herein, we compared the CNP to the MHT for detection of carbapenemase-producing GNB.
(This study was presented in part at the 113th General Meeting of the American Society of Microbiology, Denver, CO, 18 to 21 May 2013.)
Two hundred seventy-one GNB, including 39 characterized reference isolates (5 derepressed AmpC mutants and 5 plasmid-mediated AmpC producers with or without porin loss, 18 ESBL producers with or without porin loss, and 8 KPC, 1 NDM-1, 1 OXA-48, and 1 VIM-2 isolate) and 232 clinical isolates (including 111 KPC, 3 NDM, 1 SME-1, and 5 VIM isolates), were studied (Table 1). The 271 isolates included 201 Enterobacteriaceae and 70 nonfermenting GNB. Clinical isolates included those submitted to the clinical microbiology laboratory, Mayo Clinic, Rochester, MN, from October 2012 to January 2013 for modified Hodge testing (n = 40) and rectal swab surveillance isolates (n = 192). The latter were recovered using the Centers for Disease Control and Prevention (CDC)-recommended method for CRE screening (11) and/or on HardyCHROM ESBL medium (Hardy Diagnostics, Santa Maria, CA) from 47 rectal surveillance swabs collected between September and November 2012, as part of a CRE colonization study performed in long-term acute-care facilities in Chicago, IL (12). The MHT was performed using Mueller-Hinton Agar (BD BBL, Franklin Lakes, NJ) with 10 μg meropenem and ertapenem disks (BD BBL). The CNP, with slight modification from the originally described protocol (modifications based on personal communication from Patrice Nordmann), was performed as follows. Each isolate was tested in paired tubes. Two 1.5-ml low-bind protein microcentrifuge tubes (Eppendorf NA, Hauppauge, NY), each containing 100 μl of a 20 mM tris-HCl lysis buffer, SoluLyse (Thermo Fisher Scientific, Waltham, MA), were individually inoculated with a 1-μl loopful of bacterial colony (18 to 24 h old, loop swept through pure culture), and bacterial suspensions were vortexed for 5 s. To the first tube, 100 μl of 0.5% (wt/vol) phenol red solution (Sigma-Aldrich, St. Louis, MO) with 10 mM zinc sulfate (Sigma-Aldrich) (solution A, buffered to pH 7.8 by adding 0.1 N NaOH) was then added, and the tube was vortexed. To the second tube, 100 μl of solution A with imipenem (USP) dissolved directly in solution A to a final concentration of 6 mg/ml was added and then vortexed. Imipenem was reconstituted in solution A on each day of testing. K. pneumoniae ATCC BAA1705 (KPC positive) and BAA1706 (KPC negative) and a pair of “blank” tubes without bacteria were used as controls with each CNP run. Tubes were visually read at 15, 30, 45, 60, and 120 min. A color change from red to yellow/orange indicated carbapenemase production (i.e., as a result of the pH change induced by imipenem hydrolysis), while tubes remaining red/reddish-orange were considered negative (Fig. 1). Clinical isolates were tested in a blinded fashion. Interobserver accuracy was assessed by three blinded operators who performed the CNP in triplicate using four isolates (1 NDM Escherichia coli isolate, 1 VIM-2 Pseudomonas aeruginosa isolate, 1 KPC isolate [ATCC BAA-1705], and one non-carbapenemase-producing isolate [ATCC BAA-1706]) on different days. A duplex PCR for blaKPC and blaNDM was performed with clinical/surveillance isolates (13). If negative for blaKPC and blaNDM, CRE were further evaluated for SME (14), VIM (15), IMP (16), GES (17), and OXA-48 (18), AmpC (19), and OmpK35/36 porin loss (20) using conventional PCR. Nonfermenting GNB which yielded a positive CNP result were also subjected to the aforementioned conventional PCRs. PCR was considered the gold standard for carbapenemase characterization. Antimicrobial susceptibility testing was performed by agar dilution, and identification of clinical isolates was by matrix-assisted laser desorption ionization-time of flight mass spectrometry (Bruker Daltonics, Billerica, MA).
Table 1.
Breakdown of reference and clinical isolates tested
| Description | Species (no) | Genotype(s) (no) | MIC of drug |
Test result(s) (np) |
||
|---|---|---|---|---|---|---|
| Ertapenem | Meropenem | Carba NP | Modified Hodge | |||
| Reference isolates | ||||||
| Derepressed AmpC mutanta | E. coli (3) | ampC promoter/attenuator mutation (3) | ≤0.25 | ≤1 | Negative (3) | Negative (2), positive (1)d |
| Derepressed AmpC mutant with porin lossa | E. coli (1) | ampC attenuator mutation and OmpF | 1 | ≤1 | Negative (1) | Equivocale |
| E. coli (1) | ampC promoter/attenuator mutation and OmpC | ≤0.25 | ≤1 | Negative (1) | Positived | |
| AmpCa | E. coli (3) | CMY-2 | ≤0.25–0.5 | ≤1 | Negative (3) | Negative (2), positive (1)d |
| E. coli (1) | FOX-5 | ≤0.25 | ≤1 | Negative | Equivocald | |
| AmpC with porin lossa | E. coli (1) | CMY-2 and OmpF | ≤0.25 | ≤1 | Negative | Equivocale |
| ESBLb | E. coli (1) | TEM-1 + SHV-43 | ≤0.25 | ≤1 | Negative | Negative |
| K. pneumoniae (6) | CTX-M-12, SHV-43, TEM-10, TEM-10 + TEM-1, SHV-12, TEM-9 | ≤0.25 | ≤1 | Negative (6) | Negative (6) | |
| ESBL with porin loss | E. coli (7) | CTX-M-15, TEM-1 + OmpFa (2); CTX-M-15, OXA-1 + OmpCa (2); CTX-M-14, TEM-1 + OmpFa (2), TEM-12 + OmpC/Fb (1) | ≤0.25–1 | ≤1 | Negative (7) | Negative (6), equivocal (1)e |
| K. pneumoniae (4)a | CTX-M-2, SHV-11 + OmpK35 (1); CTX-M-15, SHV-11, TEM-1, OXA-1 + OmpK36 (1); CTX-M-15, OXA-1 + OmpK35/36 (1); CTX-M-15, SHV-1 + OmpK35 (1) | ≤0.25–0.5 | ≤1 | Negative (4) | Negative (4) | |
| Acquired carbapenemases | Citrobacter spp. (1) | KPC | >4 | 8 | Positive | Positive |
| E. aerogenes (1) | KPC | >4 | >8 | Positive | Positive | |
| E. cloacae complex (1) | KPC | >4 | 8 | Positive | Positive | |
| E. coli (1) | KPC | 4 | 2 | Positive | Positive | |
| P. aeruginosa (1) | KPC | >4 | >8 | Positive | Positive | |
| P. mirabilis (1) | KPC | >4 | 8 | Positive | Positive | |
| P. stuartii (1) | KPC | ≤0.25 | ≤1 | Positive | Positive | |
| S. marcescens (1) | KPC | >4 | >8 | Positive | Positive | |
| E. coli (1)c | NDM-1 | >4 | >8 | Positive | Positive | |
| K. pneumoniae NCTC 13442 (1) | OXA-48 | 1 | ≤1 | Positive | Positive | |
| P. aeruginosa (1)b | VIM-2 | >4 | >8 | Positive | Positive | |
| Clinical isolates | ||||||
| Carbapenem-resistant Enterobacteriaceae (carbapenemase producing) | K. pneumoniae (98) | KPC | >4/>4 | 8/>8 | Positive (111) | Positive (111) |
| Klebsiella spp. (3) | KPC | |||||
| E. coli (4) | KPC | |||||
| Citrobacter spp. (2) | KPC | |||||
| E. cloacae complex (1) | KPC | |||||
| E. aerogenes (1) | KPC | |||||
| P. stuartii (1) | KPC | |||||
| S. marcescens (1) | KPC | |||||
| K. pneumoniae (2), E. coli (1) | NDM | >4/>4 | >8/>8 | Positive (3) | Positive (1), Negative (2) | |
| S. marcescens (1) | SME-1 | 4 | 8 | Positive | Positive | |
| Carbapenem-resistant Enterobacteriaceae (non- carbapenemase producing) | E. aerogenes (1) | ampC + ompK36 | >4 | 4 | Negative | Negative |
| E. cloacae complex (2) | Undefined (ESBL phenotype; likely hyperproducer) (1); ampC (1) | 1 | <1 | Negative | Positivef | |
| E. coli (6) | ampC (4); Undefined (ESBL phenotype; likely hyperproducer) (2) | >4/>4 | 4/>8 | Negative (6) | Negative (4), positive (1)g, inhibited (1)h | |
| K. pneumoniae (2) | ompK35/36 (1); ampC+ompK35 (1) | 2–>4 | ≤1–2 | Negative (2) | Negative (2) | |
| P. agglomerans (1) | ampC | >4 | 4 | Negative | Negative | |
| Enterobacteriaceae resistant to expanded-spectrum cephalosporins | E. coli (4) | Not done | ≤0.25/≤0.25 | ≤1/≤1 | Negative (17) | Negative (15), positive (2)i |
| K. pneumoniae (4) | Not done | |||||
| P. mirabilis (3) | Not done | |||||
| P. stuartii (3) | Not done | |||||
| M. morganii (2) | Not done | |||||
| E. cloacae complex (1) | Not done | |||||
| Expanded-spectrum cephalosporin/carbapenem- susceptible Enterobacteriaceae | P. stuartii (4) | Not done | ≤0.25/≤0.25 | ≤1/≤1 | Negative (20) | Negative (16), positive (2)j, inhibited (2)k |
| P. mirabilis (5) | Not done | |||||
| E. coli (5) | Not done | |||||
| K. pneumoniae (2) | Not done | |||||
| E. aerogenes (2) | Not done | |||||
| M. morganii (1) | Not done | |||||
| Serratia liquefaciens/S. grimesii (1) | Not done | |||||
| Carbapenem-resistant nonfermenting Gram-negative bacilli | P. aeruginosa (51) | VIM (5)l; not done (62) | >4/>4 | >8/>8 | Positive(5)l | Positive (18)m |
| Acinetobacter spp. (16) | >8/>8 | >8/>8 | Negative (62) | Negative (36), inhibited (13)n | ||
| Carbapenem-susceptible nonfermenting Gram-negative bacilli | Alcaligenes faecalis (1) | Not done (1) | ≤0.25 | ≤1 | Negative | Negative |
Gift of George Zhanel and Daryl Hoban.
Gift of John Quinn.
Gift of Paul Schreckenberger.
Ertapenem disk.
Meropenem disk.
Ertapenem disk Modified Hodge Test (MHT) positive, meropenem disk MHT weak positive.
One isolate with ampC.
One isolate with ampC.
One Proteus mirabilis and one Providencia stuartii isolate.
Two P. stuartii isolates.
Two P. mirabilis isolates.
Conventional PCR was done for five Pseudomonas aeruginosa isolates positive for the Carba NP test, and these were found to be positive for VIM.
Six P. aeruginosa and 12 Acinetobacter isolates.
Twelve P. aeruginosa isolates and one Acinetobacter isolate.
n, no. of isolates.
n, no. of results.
Fig 1.
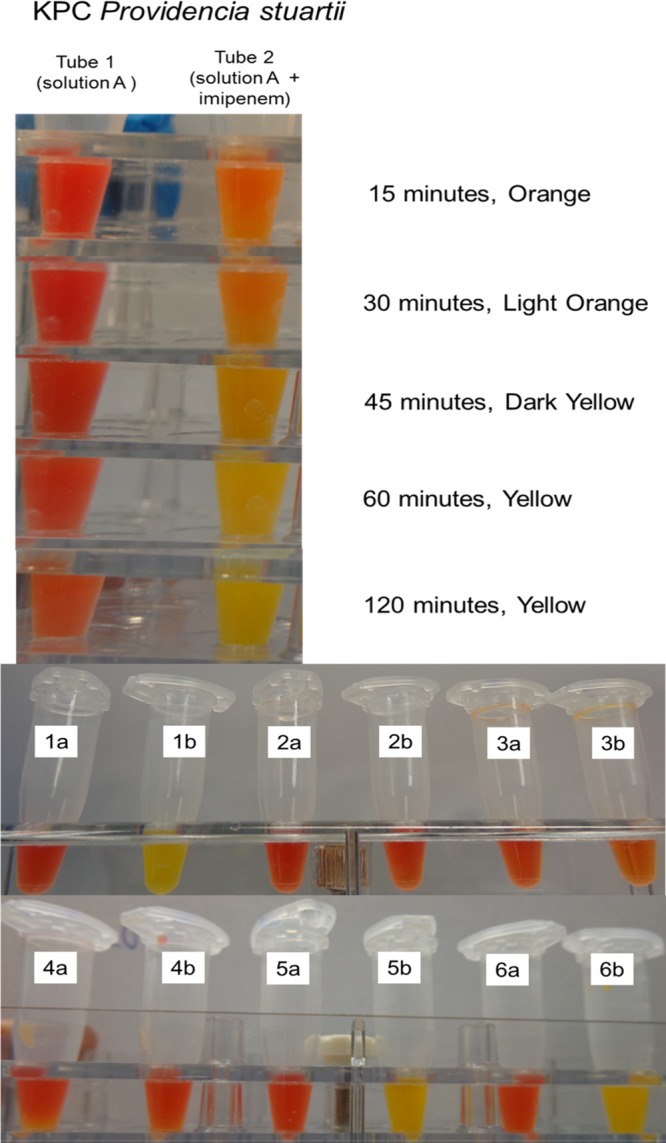
Carba NP test: example of assay and interpretation of results. (a) KPC Providencia stuartii (ertapenem MIC ≤ 0.25 μg/ml; meropenem MIC ≤ 1 μg/ml) Carba NP test run; note relative slower color changes. The majority of KPC-positive isolates in this study turned a definitive yellow within 15 min. (b) Carba NP read at 2 h. Isolates were tested in paired tubes; those labeled “a” contain solution A, and tubes labeled “b” contain solution A plus imipenem. Tubes 1, KPC-positive Klebsiella pneumoniae control (BAA-1705); tubes 2, KPC K. pneumoniae-negative control (BAA-1706); tubes 3, blank control; tubes 4, extended-spectrum-beta-lactamase-producing Escherichia coli (TEM-12); tubes 5, NDM-1-positive E. coli; tubes 6, OXA-48-positive K. pneumoniae (NCTC 13442).
The CNP detected all carbapenemase-producing positive GNB (n = 131), while the MHT detected 128/131 (97.7%). Two NDM isolates were negative by the MHT. The two tests had comparable overall sensitivities (P = 0.08), but the CNP had superior specificity overall and with the subset of Enterobacteriaceae (both P < 0.0001) (Table 2). Besides inferior specificity, the MHT yielded 20 (7.4%) equivocal/nonreadable results (i.e., growth inhibition of the Escherichia coli lawn around the test streak or swarming of Proteus species). All positive CNP reactions yielded a distinct color change to yellow on initial testing except for two VIM-positive Pseudomonas aeruginosa isolates (one reference and one clinical isolate), which yielded orange and light orange colors, respectively. These reactions were considered positive but were repeated by a second operator for confirmation. Both isolates yielded a yellow reaction on repeat testing. Overall, of the CNP-positive isolates (n = 131), 123/131 (93.9%) and 129/131 (98.5%) turned distinctly yellow (positive) at 15 and 60 min, respectively. Eight isolates took more than 15 min to achieve a distinct yellow reaction: these comprised 5 VIM P. aeruginosa (range, 30 min to 2 h), 1 OXA-48 Klebsiella pneumoniae (1 h), 1 KPC K. pneumoniae (30 min), and 1 Providencia stuartii (45 min) isolate. There was 100% accuracy and agreement in the interobserver CNP assessment.
Table 2.
Performance characteristics of the Carba NP and modified Hodge tests
| Performance characteristic (compared to presence of carbapenemase gene) | Value for isolate group and test (ne)a |
|||
|---|---|---|---|---|
| All isolates (Enterobacteriaceae and nonfermenting Gram-negative bacilli) |
Enterobacteriaceae |
|||
| Carba NP (269)b | Modified Hodge (251)b | Carba NP (200)c | Modified Hodge (194)c | |
| Sensitivity, % (95% CId) | 100 (96.4–100) | 97.7 (92.9–99.4) | 100 (96.3–100) | 98.4 (93.7–99.7) |
| Specificity, % (95% CI) | 100 (96.7–100) | 80.0 (71.5–86.5) | 100 (94.1–100) | 85.7 (74.8–92.6) |
| Positive predictive value, % (95% CI) | 100 (96.4–100) | 84.2 (77.2–89.4) | 100 (96.3–100) | 92.4 (86.1–96.1) |
| Negative predictive value, % (95% CI) | 100 (96.7–100) | 97.0 (90.8–99.2) | 100 (94.1–100) | 96.8 (87.8–99.4) |
Excluding equivocal/nonreadable results for the MHT.
McNemar's test for sensitivity, P = 0.08; specificity, P < 0.0001.
McNemar's test for sensitivity, P = 0.16; specificity, P < 0.0001.
CI, confidence interval.
n, no. of isolates.
The CDC and Public Health England (formerly the Health Protection Agency) recommended active surveillance for CRE in certain high-risk settings or for certain patient groups (e.g., patients transferred from long-term-care facilities) (21, 22). Although the CDC recommends testing CRE isolates from patients with a history of hospitalization outside the United States for blaKPC and blaNDM (23), molecular testing is largely limited to public health and reference laboratories. The MHT, while a useful screen for carbapenemases, suffers from lack of specificity, poor sensitivity for metallo-β-lactamase detection, and a long turnaround time, findings corroborated by our study. Although we studied a limited number of NDM isolates, the CNP detected all four, compared to two of four detected by the MHT. This is likely due to zinc supplementation of the CNP (7). While the CNP detected all carbapenemase-producing GNB in our study, we noticed that color changes were slower for VIM-positive isolates and isolates with low carbapenem MICs (the KPC P. stuartii and OXA-48 K. pneumoniae reference isolates), possibly secondary to inherent differences in hydrolytic activities of VIM and OXA-48 versus KPC and NDM carbapenemases (24–26) and/or lower expression of carbapenemases in the KPC P. stuartii isolate with low carbapenem MICs (27). The blank tubes included in each run were helpful in this respect; true-positive isolates should exhibit a yellow/orange color, which is more obvious in comparison to the blank. A limitation of our study is that the majority of carbapenemase-producing Enterobacteriaceae studied were KPC-positive isolates; specificity would have been more rigorously assessed had we studied more carbapenemase-negative, carbapenem-nonsusceptible Enterobacteriaceae. However, a strength of our study was that the CNP was assessed with clinical isolates cultured from surveillance swabs and not just on reference isolates alone, thus decreasing selection bias.
Our findings are consistent with previously published data by Nordmann and colleagues (8–10), although in this study we utilized whole bacterial cells (instead of supernatant after bacterial lysis) and an increased concentration of imipenem (6 instead of 3 mg/ml) based on personal communication with Nordmann. This approach enabled detection of a KPC P. stuartii isolate, 6 VIM P. aeruginosa isolates (1 reference, and 5 clinical), and 1 KPC P. aeruginosa isolate which were initially negative when tested with 3 mg/ml of imipenem and supernatant obtained after bacterial lysis (8; also data not shown). Overall, we found that the CNP was easily performed, displayed excellent sensitivity, and had superior specificity and a faster turnaround time than the MHT. These features allow easy implementation in the clinical laboratory and translate to timely and actionable clinical results.
ACKNOWLEDGMENTS
We thank the technologists in the antimicrobial susceptibility section of the Mayo Clinic Bacteriology laboratory for their invaluable help with this project, John Quinn, Paul Schreckenberger, George Zhanel, and Daryl Hoban for providing reference isolates, and Patrice Nordmann for answering technical questions about the Carba NP test.
Footnotes
Published ahead of print 3 July 2013
REFERENCES
- 1.Patel G, Huprikar S, Factor SH, Jenkins SG, Calfee DP. 2008. Outcomes of carbapenem-resistant Klebsiella pneumoniae infection and the impact of antimicrobial and adjunctive therapies. Infect. Control Hosp. Epidemiol. 29:1099–1106 [DOI] [PubMed] [Google Scholar]
- 2.Landman D, Babu E, Shah N, Kelly P, Olawole O, Bäcker M, Bratu S, Quale J. 2012. Transmission of carbapenem-resistant pathogens in New York City hospitals: progress and frustration. J. Antimicrob. Chemother. 67:1427–1431 [DOI] [PubMed] [Google Scholar]
- 3.Won SY, Munoz-Price LS, Lolans K, Hota B, Weinstein RA, Hayden MK, Centers for Disease Control and Prevention Epicenter Program 2011. Emergence and rapid regional spread of Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae. Clin. Infect. Dis. 53:532–540 [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention 2013. Healthcare-associated infections: tracking CRE. Centers for Disease Control and Prevention, Atlanta, GA: http://www.cdc.gov/hai/organisms/cre/TrackingCRE.html Accessed 19 February 2013 [Google Scholar]
- 5.Kitchel B, Rasheed JK, Endimiani A, Hujer AM, Anderson KF, Bonomo RA, Patel JB. 2010. Genetic factors associated with elevated carbapenem resistance in KPC-producing Klebsiella pneumoniae. Antimicrob. Agents Chemother. 54:4201–4207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carvalhaes CG, Picao RC, Nicoletti AG, Xavier DE, Gales AC. 2010. Cloverleaf test (modified Hodge test) for detecting carbapenemase production in Klebsiella pneumoniae: be aware of false positive results. J. Antimicrob. Chemother. 65:249–251 [DOI] [PubMed] [Google Scholar]
- 7.Girlich D, Poirel L, Nordmann P. 2012. Value of the modified Hodge test for detection of emerging carbapenemases in Enterobacteriaceae. J. Clin. Microbiol. 50:477–479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nordmann P, Poirel L, Dortet L. 2012. Rapid detection of carbapenemase-producing Enterobacteriaceae. Emerg. Infect. Dis. 18:1503–1507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dortet L, Poirel L, Nordmann P. 2012. Rapid detection of carbapenemase-producing Pseudomonas spp. J. Clin. Microbiol. 50:3773–3776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dortet L, Poirel L, Nordmann P. 2012. Rapid identification of carbapenemase types in Enterobacteriaceae and Pseudomonas spp. by using a biochemical test. Antimicrob. Agents Chemother. 56:6437–6440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention 2008. Laboratory protocol for detection of carbapenem-resistant or carbapenemase-producing, Klebsiella spp. and E. coli from rectal swabs. Centers for Disease Control and Prevention, Atlanta, GA: http://www.cdc.gov/HAI/pdfs/labSettings/Klebsiella_or_Ecoli.pdf Accessed 6 March 2013 [Google Scholar]
- 12.Thurlow CJ, Prabaker K, Lin MY, Lolans K, Weinstein RA, Hayden MK, Centers for Disease Control and Prevention Epicenters Program 2013. Anatomic sites of patient colonization and environmental contamination with Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae at long-term acute care hospitals. Infect. Control Hosp. Epidemiol. 34:56–61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cunningham SA, Noorie T, Meunier D, Woodford N, Patel R. 23 January 2013. Rapid and simultaneous detection of genes encoding Klebsiella pneumoniae carbapenemase (blaKPC) and New Delhi metallo-beta-lactamase (blaNDM) in Gram-negative bacilli. J. Clin. Microbiol. 10.1128/JCM.03062-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hong SS, Kim K, Huh JY, Jung B, Kang MS, Hong SG. 2012. Multiplex PCR for rapid detection of genes encoding class A carbapenemases. Ann. Lab. Med. 32:359–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Poirel L, Naas T, Nicolas D, Collet L, Bellais S, Cavallo JD, Nordmann P. 2000. Characterization of VIM-2, a carbapenem-hydrolyzing metallo-beta-lactamase and its plasmid- and integron-borne gene from a Pseudomonas aeruginosa clinical isolate in France. Antimicrob. Agents Chemother. 44:891–897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Senda K, Arakawa Y, Ichiyama S, Nakashima K, Ito H, Ohsuka S, Shimokata K, Kato N, Ohta M. 1996. PCR detection of metallo-β-lactamase gene (blaIMP) in Gram-negative rods resistant to broad-spectrum β-lactams. J. Clin. Microbiol. 34:2909–2913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Poirel L, Le Thomas I, Naas T, Karim A, Nordmann P. 2000. Biochemical sequence analyses of GES-1, a novel class A extended-spectrum beta-lactamase, and the class 1 integron In52 from Klebsiella pneumoniae. Antimicrob. Agents Chemother. 44:622–632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Poirel L, Heritier C, Tolun V, Nordmann P. 2004. Emergence of oxacillinase-mediated resistance to imipenem in Klebsiella pneumoniae. Antimicrob. Agents Chemother. 48:15–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perez-Perez FJ, Hanson ND. 2002. Detection of plasmid-mediated AmpC beta-lactamase genes in clinical isolates by using multiplex PCR. J. Clin. Microbiol. 40:2153–2162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaczmarek FM, Dib-Hajj F, Shang W, Gootz TD. 2006. High-level carbapenem resistance in a Klebsiella pneumoniae clinical isolate is due to the combination of blaACT-1 beta-lactamase production, porin OmpK35/36 insertional inactivation, and down-regulation of the phosphate transport porin phoe. Antimicrob. Agents Chemother. 50:3396–3406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention 2012. 2012 CRE toolkit—guidance for control of carbapenem-resistant Enterobacteriaceae (CRE). Centers for Disease Control and Prevention, Atlanta, GA: http://www.cdc.gov/hai/organisms/cre/cre-toolkit/index.html Accessed 6 March 2013 [Google Scholar]
- 22.Health Protection Agency (UK)/Advisory Committee on Antimicrobial Resistance and Healthcare Associated Infections (ARHAI) 2011. Advice on carbapenemase producers: recognition, infection control and treatment. Health Protection Agency, London, United Kingdom: http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_c/1294740725984 Accessed 6 March 2013 [Google Scholar]
- 23.Centers for Disease Control and Prevention HAN 2013. CDC Health Advisory: new carbapenem-resistant Enterobacteriaceae warrant additional action by healthcare providers. http://www.bt.cdc.gov/HAN/han00341.asp Accessed 6 March 2013
- 24.Walther-Rasmussen J, Hoiby N. 2006. OXA-type carbapenemases. J. Antimicrob. Chemother. 57:373–383 [DOI] [PubMed] [Google Scholar]
- 25.Walther-Rasmussen J, Hoiby N. 2007. Class A carbapenemases. J. Antimicrob. Chemother. 60:470–482 [DOI] [PubMed] [Google Scholar]
- 26.Yong D, Toleman MA, Giske CG, Cho HS, Sundman K, Lee K, Walsh TR. 2009. Characterization of a new metallo-beta-lactamase gene, blaNDM-1, and a novel erythromycin esterase gene carried on a unique genetic structure in Klebsiella pneumoniae sequence type 14 from India. Antimicrob. Agents Chemother. 53:5046–5054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Naas T, Cuzon G, Truong HV, Nordmann P. 2012. Role of ISKpn7 and deletions in blaKPC gene expression. Antimicrob. Agents Chemother. 56:4753–4759 [DOI] [PMC free article] [PubMed] [Google Scholar]


